ALIGNER CORNER
This JCO column is compiled by Contributing Editor William V. Gierie, DDS, MS. Every few months, Dr. Gierie will introduce a pertinent article related to clear aligner therapy. Your suggestions for future topics or authors are welcome.
In this installment of the Aligner Corner, the author presents three cases treated with the Invisalign First* system. The patients provide a good representation of Phase I therapeutic needs, including an anterior crossbite. The cases are all well documented and well treated, and the author offers numerous tips and techniques gleaned from her experience with some of the earliest Invisalign First cases. One particularly helpful idea was to employ smartphone reminders to help patients remember to replace their aligners after eating—another great example of leveraging technology to assist us in our ever-busier lives.
Phase I treatment is an exciting area of expansion for clear aligner therapy and will only continue to grow.
WVG
Phase I Orthodontic Treatment Using Invisalign First
Few authors have reported the use of sequential clear aligners in the mixed dentition. Long and colleagues described a 100-patient prospective study of such patients, with clear aligners used to treat anterior crossbite, posterior crossbite, deep bite, crowding, and spacing.1,2
Similar articles from the archive:
A few individual case reports have demonstrated the application of clear aligners in the correction of a midline diastema,3 mesial molar drift,4 or anterior crossbite.5 One of the greatest challenges encountered in using clear aligners for Phase I treatment seems to be the maintenance of adequate appliance fit while teeth are exfoliating and erupting.
I had a unique opportunity to offer Invisalign First* clear aligners to my patients in 2017 and early 2018 through a limited market-release program, in which Align Technology gave invited clinicians early access to new aligner features specific to Phase I therapy. Recent advances now make the use of clear aligners much more feasible in early mixed-dentition treatment. The turnaround time from the lab is more predictable, helping to avoid fit problems caused by tooth eruption. Appliance retention can be significantly improved using custom-shaped composite attachments. Pontic spaces and interproximal leeway space can be built into the appliances to compensate for erupting permanent teeth, so that treatment disruption is minimized. Additional features such as elastic hooks and bite ramps can be integrated into the aligners as desired. These developments enable clinicians to prescribe clear aligners in the early mixed dentition for arch development; treatment of crowding, protrusion, and rotations; or personal considerations, as when growing patients are self-conscious about their smiles.
A successful Phase I sets up an optimal environment for the remaining dental development and makes Phase II relatively straightforward. The first phase also establishes a baseline for patient expectations of the second-phase experience. Compared with traditional fixed appliances, Invisalign First clear aligners have fewer dietary restrictions, provide the convenience of weekly aligner changes (and therefore less risk of appliance damage during treatment), and permit better oral hygiene, making compliance easier to manage among 6- to 10-year-olds.
The following patients treated with Invisalign First clear aligners in the early mixed dentition demonstrate the range of initial results achieved in our practice.
Case 1
A 9-year-old male in the early mixed dentition presented with severe mandibular crowding, mid-arch narrowing, a deep overbite that was impinging on the palate, a lingually positioned upper right permanent lateral incisor, and an ectopic lower left permanent canine (Fig. 1).

Fig. 1 Case 1. 9-year-old male patient with Class I dental and skeletal relationships, severe mandibular crowding, and ectopic lower left permanent canine before treatment.
The diagnosis was a Class I dental and skeletal relationship (Table 1).
The patient had previously consulted with another orthodontist, who had suggested primary tooth extractions and a maxillary expander, but the parents sought a less invasive treatment. Invisalign First was prescribed for Phase I, with the objectives of dentoalveolar expansion and arch development, resolution of crowding, and observation of the impacted lower left canine. Sequential molar expansion was prescribed to address lower crowding, and SmartForce* extrusion attachments were added on the upper lateral incisors (Fig. 2).
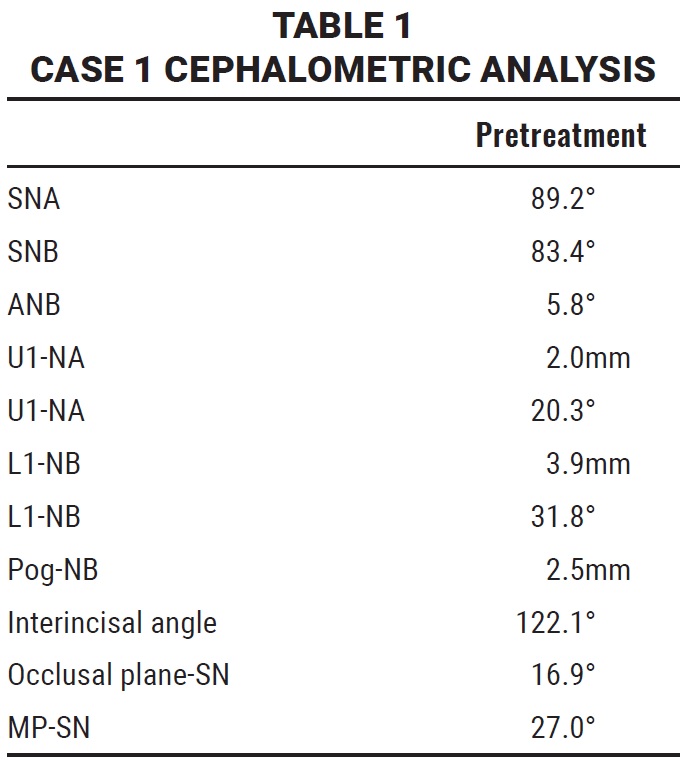
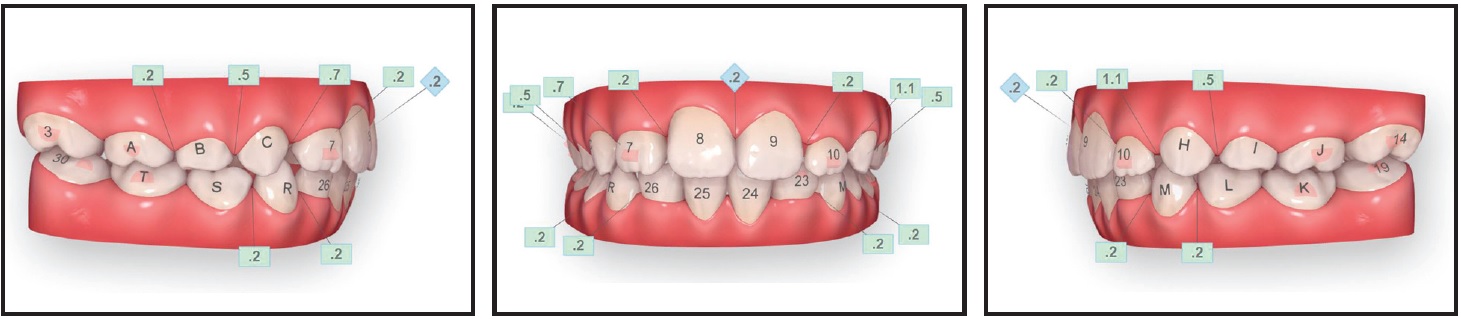
Fig. 2 Case 1. ClinCheck* plan (numbers in green boxes represent interproximal spaces specified for wider permanent teeth).
The aligners tracked perfectly over the course of the Phase I treatment, which lasted about nine months (Fig. 3).
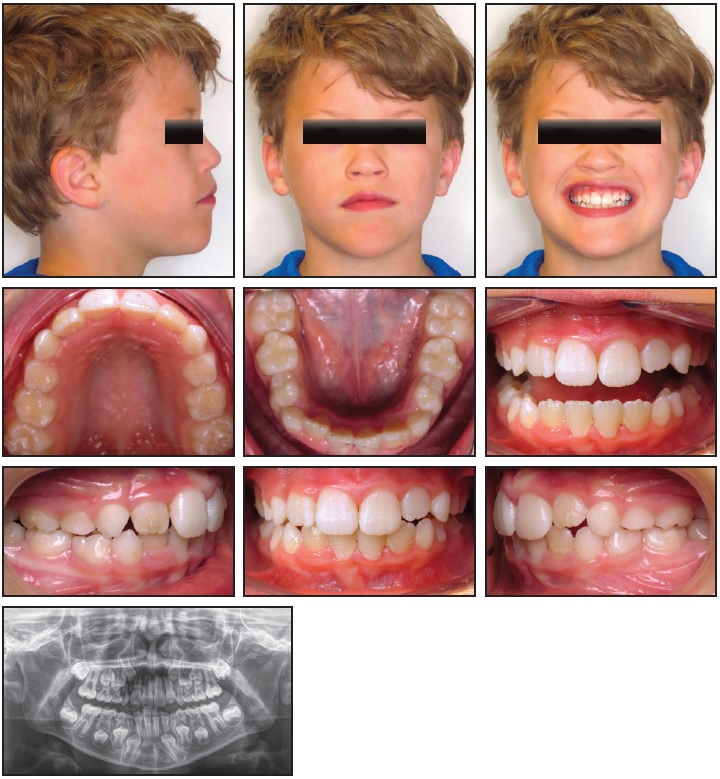
Fig. 3 Case 1. Patient after nine months of Phase I treatment with 40 upper and 37 lower aligners.
Forty upper and 37 lower aligner trays were used, with no refinement needed. Three passive aligners were worn in the lower arch while the upper arch was finishing. The patient changed aligners every seven days, and his compliance was excellent.
Aligner treatment is also anticipated for Phase II. In the interim, the plan is to extract the lower left first deciduous molar to gain space for the lower left canine (which remains impacted), and to use the final aligner as a lower holding arch to prevent mesial drift of the lower left first and second molars. The eruption of the lower left canine and first and second premolars will be closely monitored. If the canine does not drift spontaneously into proper position, the patient may need surgical exposure and placement of a bracket and chain to distalize the canine with elastic traction from the upper left first molar. Another alternative would be to extract the lower left permanent lateral incisor.
Case 2
A 9-year-old female presented with an extreme overjet, a deep overbite, and moderate to severe mandibular crowding. All four permanent canines were blocked out due to early loss of the deciduous canines, which were extracted before the patient’s first visit to our office (Fig. 4).
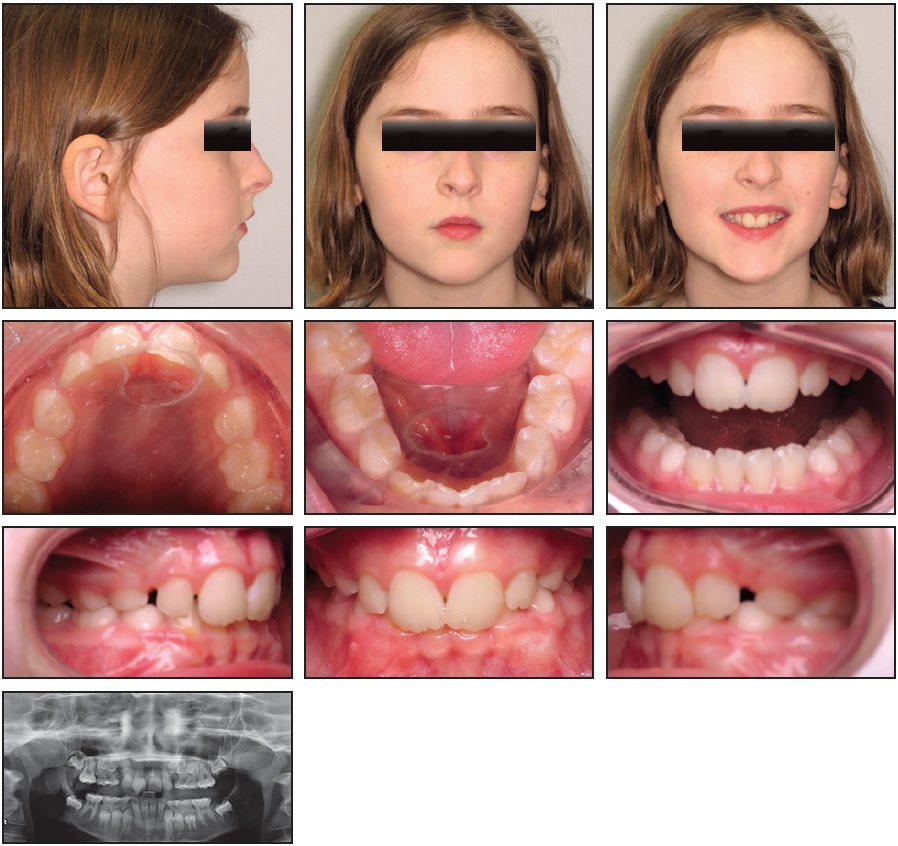
Fig. 4 Case 2. 9-year-old female patient with Class II, division 1 malocclusion, deep overbite, mandibular crowding, and impacted permanent canines before treatment.
Evaluation found a Class II, division 1 malocclusion in the early mixed dentition. No cephalograms were taken because the family wished to keep the number of x-rays to a minimum.
Instead of trying to recapture the lost space of the deciduous canines, a previous orthodontist had recommended serial extractions and a maxillary expander. The family therefore requested less invasive alternatives. Our treatment aims included arch development, dentoalveolar expansion, and growth modification (Fig. 5).
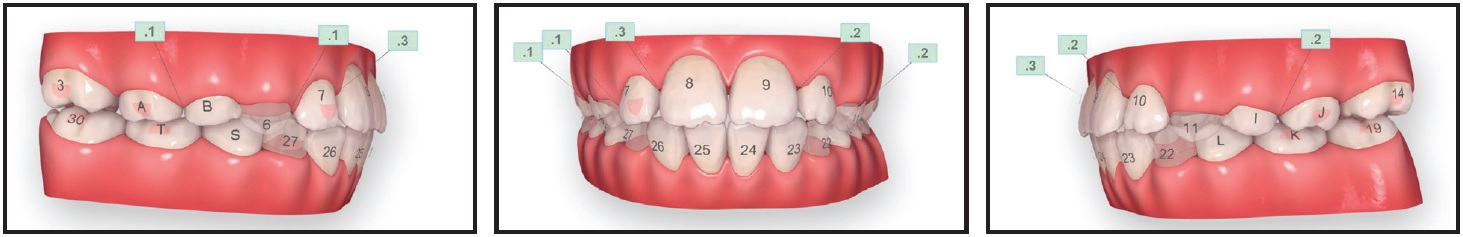
Fig. 5 Case 2. ClinCheck plan, with Power Ridges* (not shown in final aligner stage) used for torque control of upper central incisors and all four lower incisors in stages 1-40.
The crowding and deep bite would be addressed through upper first-molar rotation and incisor proclination, respectively. Mesial root tip of the lateral incisors and interproximal leeway space were built into the ClinCheck* plan to accommodate the erupting permanent teeth.
Phase I treatment lasted nine months (Fig. 6).

Fig. 6 Case 2. Patient after nine months of Phase I treatment with 40 upper and 44 lower aligners (photos taken three months later).
Forty upper and 44 lower aligners were required, with no refinement stage. Four passive upper aligners were worn to account for the difference in treatment duration between the arches. The patient changed her aligners every three to five days. Compliance was excellent, and the aligners tracked well with the prescribed treatment plan. After a transitional holding phase, Phase II treatment will involve the use of clear aligners to guide the remaining dental eruption and detail the occlusion.
Case 3
An 8-year-old female in the early mixed dentition presented with a Class III relationship, a narrow mandible, mild anterior crowding, and a crossbite of the permanent central and left lateral incisors (Fig. 7, Table 2). The lower midline was deviated 1mm to the left; a 3mm anterior functional shift indicated that the Class III malocclusion would be less severe after resolution of the crossbite.
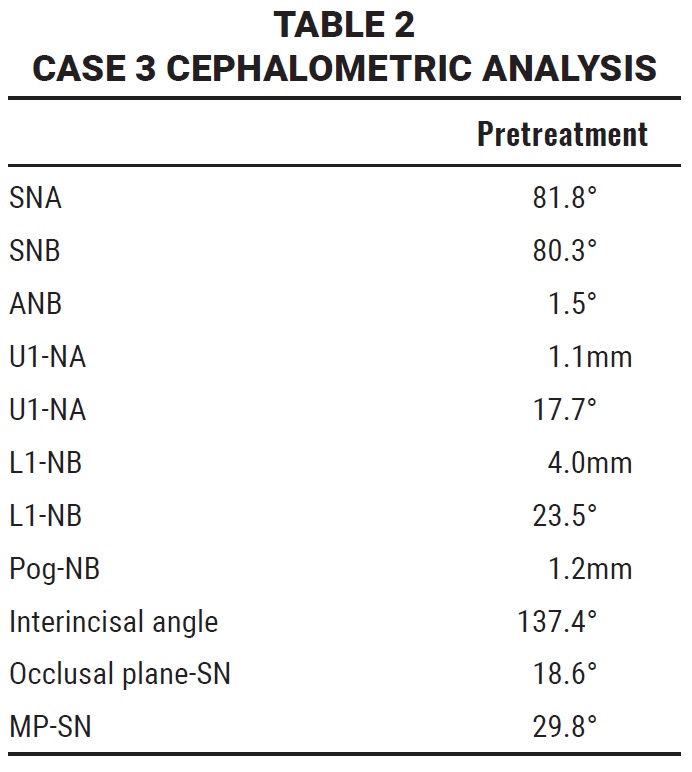
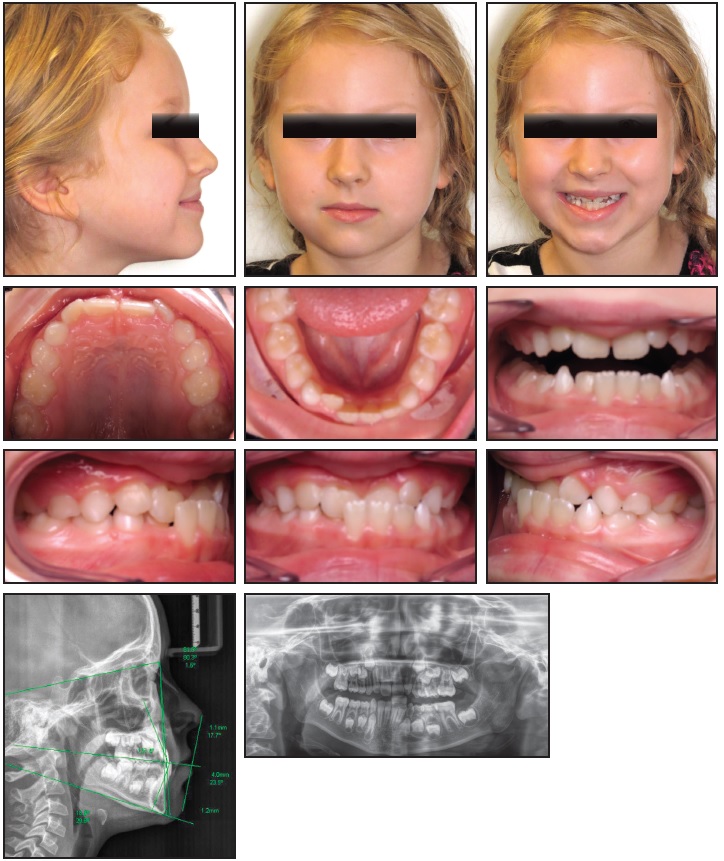
Fig. 7 Case 3. 8-year-old female patient in early mixed dentition with Class III malocclusion, mandibular crowding, and crossbite before treatment.
Phase I treatment was designed to correct the anterior crossbite and enable arch development and growth modification, using Invisalign First clear aligners and interarch elastics for Class III correction (Fig. 8).
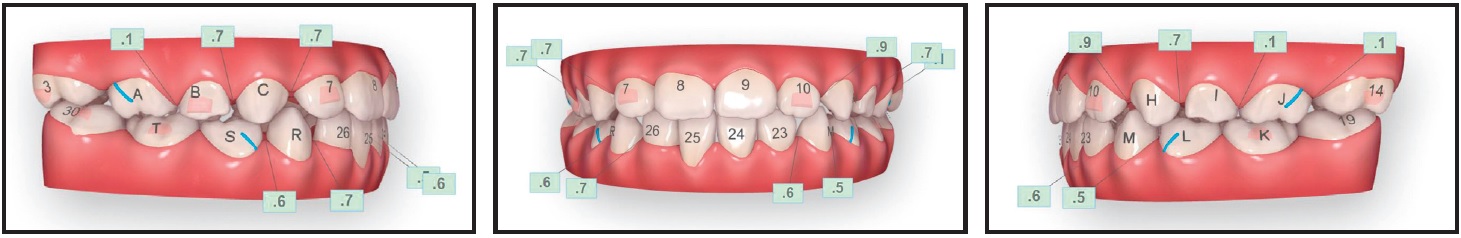
Fig. 8 Case 3. ClinCheck plan (blue lines represent precision cuts for Class III elastics).
In the ClinCheck plan, precision cuts for Class III elastics were added near the upper first permanent molars and lower first deciduous molars. The protocol involved 2oz, ³⁄16" Ormco Quail** elastics, worn after school and while sleeping, during aligner stages 10-26. Composite attachments were added to ensure appliance retention. To open the bite temporarily and make the anterior crossbite easier to correct, lingual bite ramps were built into the aligners on the lower permanent central and left lateral incisors for the first 23 stages (until the crossbite was jumped). Occlusal bite ramps were added to the upper first deciduous molars and the upper and lower second deciduous molars. Interproximal leeway spaces were built into the plan to accommodate the erupting permanent teeth.
Phase I treatment lasted nine months (Fig. 9).

Fig. 9 Case 3. Patient after nine months of Phase I treatment with 29 upper and 25 lower aligners.
The patient was prescribed 29 upper and 25 lower aligners, plus four passive lower trays. No refinement was needed. Aligners were changed weekly, and compliance was generally very good. Some minor tracking issues were experienced when the second and third sets of aligners did not seat correctly, but the problem was resolved by moving the patient forward to stage 4. Because this tray fit well, a new intraoral scan was not needed. The anterior crossbite was corrected, the Class III malocclusion was resolved, the midline was centered, and leeway spaces were created for the remaining unerupted permanent dentition. Plans for Phase II include eruption guidance and detailing with clear aligners. In the meantime, eruption of the upper permanent canines will be monitored every three months.
Discussion
As an early investigator for Invisalign First, I observed several positive factors. Because the clear aligners are removable, the children’s oral hygiene was exceptional, and the level of patient comfort was much higher than what we typically experience with fixed-appliance treatment. Additionally, because the trays are made of plastic and changed weekly, almost no emergency appointments were needed. The most common problem was the loss of an aligner, which was usually addressed by having the patient advance to the next set of trays without an office visit. I was pleasantly surprised by the level of compliance, especially compared with my adult patients. I attribute this both to the comfort of Invisalign First and to parental oversight. I did see issues arise when patients forgot to put their aligners back in after meals—which is one downside to the lack of dietary restrictions with removable appliances. An effective strategy implemented by some parents was to set post-mealtime cellphone alerts reminding them to have their children put the aligners back in.
I found it was ideal to start Phase I treatment with Invisalign First at a stage when the deciduous teeth, particularly the first and second molars, would be stable for eight to 12 months. Nevertheless, the loss of the first deciduous molars during treatment did not seem to have a dramatic effect on results. The most predictable treatment outcomes involved Class II malocclusions in which the molars needed to be rotated and slightly distalized, as well as cases with mild maxillary or mandibular constriction in which I felt comfortable expanding the arch by as much as 5mm. Class III patients with functional shifts requiring light elastics also responded well to aligner treatment.
The biggest learning curve I encountered was the turnaround time in receiving aligners from the lab. Tooth movement can occur while waiting for trays to arrive at the office, requiring a new scan to account for possible changes. During treatment, it was crucial to monitor erupting teeth that might hit the edge of an aligner, which could be adjusted by trimming the tray with an acrylic bur.
Our early use of Invisalign First has already produced several benefits. For the practice, it offers a competitive advantage. We now have parents requesting clear aligners for their children after hearing about them from other patients and parents. Treating preteens and teens with Invisalign has brought consistent 35% annual growth of our entire practice over the past four years. Time studies have demonstrated that expected profits are about 30% higher with Invisalign than with fixed appliances.
Finally, we have embraced Align’s digital platform throughout our practice. Because we use iTero Element* scanners to demonstrate every patient’s smile simulation and occlusal analysis, we keep at least two scanners in every office. Showing the family the early dentition and explaining how we monitor growth and development through digital imaging has been an added value, helping us educate patients and their families about what high-quality orthodontic treatment with Invisalign might look like. We have also had all the orthodontists in our practice engage in Invisalign Pro* to become comfortable with the ClinCheck software. This has allowed us to continually enhance our learning, so that we can treat more patients with clear aligners.
My chief recommendation to all orthodontists is to dive in and learn what Align Technology has to offer. If you are not ready for Invisalign First, I would advise starting with Invisalign for full-dentition teenagers. While the market is changing rapidly, staying current on technology allows our practices to thrive and provides our patients with high-quality, state-of-the-art treatment.
FOOTNOTES
- *Registered trademark of Align Technology, Inc., San Jose, CA; www.aligntech.com.
- **Ormco Corporation, Orange, CA; www.ormco.com.
REFERENCES
- 1. Long, B.; Chisari, J.; Dolce, C.; McGorray, S.; Aoisa, L.; Ossi, A.; Tapley, P.; Pappas, J.; Reed, J.; and Wheeler, T.T.: A prospective trial on Invisalign therapy for crossbite, deepbite, crowding, and spacing in the mixed dentition, poster presentation, AAO annual session, Boston, 2009.
- 2. Long, B.T.: Safety and efficiency of Invisalign in mixed dentition, thesis, University of Florida, Gainesville, FL, 2009.
- 3. Womack, W.R.: Invisalign for a special needs child, Orthotown, November:34, 36, 37 passim, 2010.
- 4. Neumann, I.; Schupp, W.; and Heine, G.: Distal movement of upper first molars with the Invisalign system: A patient report [in German], Kieferorthop. 18:133-137, 2004.
- 5. Abraham, K.K.; James, A.R.; Thenumkal, E.; and Emmatty, T.: Correction of anterior crossbite using modified transparent aligners: An esthetic approach, Contemp. Clin. Dent. 7:394-397, 2016.




COMMENTS
.