CASE REPORT
Nonsurgical Management of an Anterior Open Bite in a Young Adult
Treatment of an anterior open bite can be challenging due to the relatively high risk of relapse and a multifactorial etiology that may include skeletal and dentoalveolar components,1,2 as well as parafunctional habits such as bruxism involving splint treatment.3,4 While skeletal open bites in adult patients have traditionally been treated surgically, recent advances in biomechanics and the use of temporary anchorage devices5,6 have expanded the range of nonsurgical options for patients with moderate open bites of primarily dental origin.7 The risks, costs, and recovery time associated with orthognathic surgery can be avoided with carefully planned orthodontic treatment, including the strategic use of elastics and selective extractions.8,9
This case report details such an approach to the nonsurgical management of an anterior open bite, potentially caused by an occlusal splint.
Diagnosis and Treatment Plan
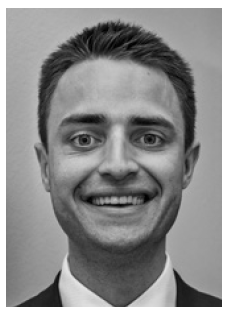
A 23-year-old male presented with the chief complaint of an open bite that created difficulty in chewing (Fig. 1). The patient reported that his anterior teeth had made contact before he began wearing an occlusal splint to treat bruxism in 2019. After noticing changes to his occlusion in 2020, he discontinued use of the splint.
The profile was slightly convex, with balanced facial thirds, an obtuse nasolabial angle (115°), a retrusive lower lip relative to the E-line, a shallow mentolabial fold, and normal chin projection. At rest, 3mm of incisal display was noted; in smiling, the patient showed 100% incisal display and 3mm of gingival display. The lower midline was shifted 2mm to the right of the facial midline.
Similar articles from the archive:
- CASE REPORT Nonsurgical Correction of a Severe Class III Open-Bite Patient with Long-Face Syndrome September 2022
- CASE REPORT Nonsurgical Correction of Class III Malocclusion and Anterior Open Bite with Mini-Implant Anchorage November 2018
- CASE REPORT Nonsurgical Treatment of a Severe Skeletal Anterior Open Bite February 2017
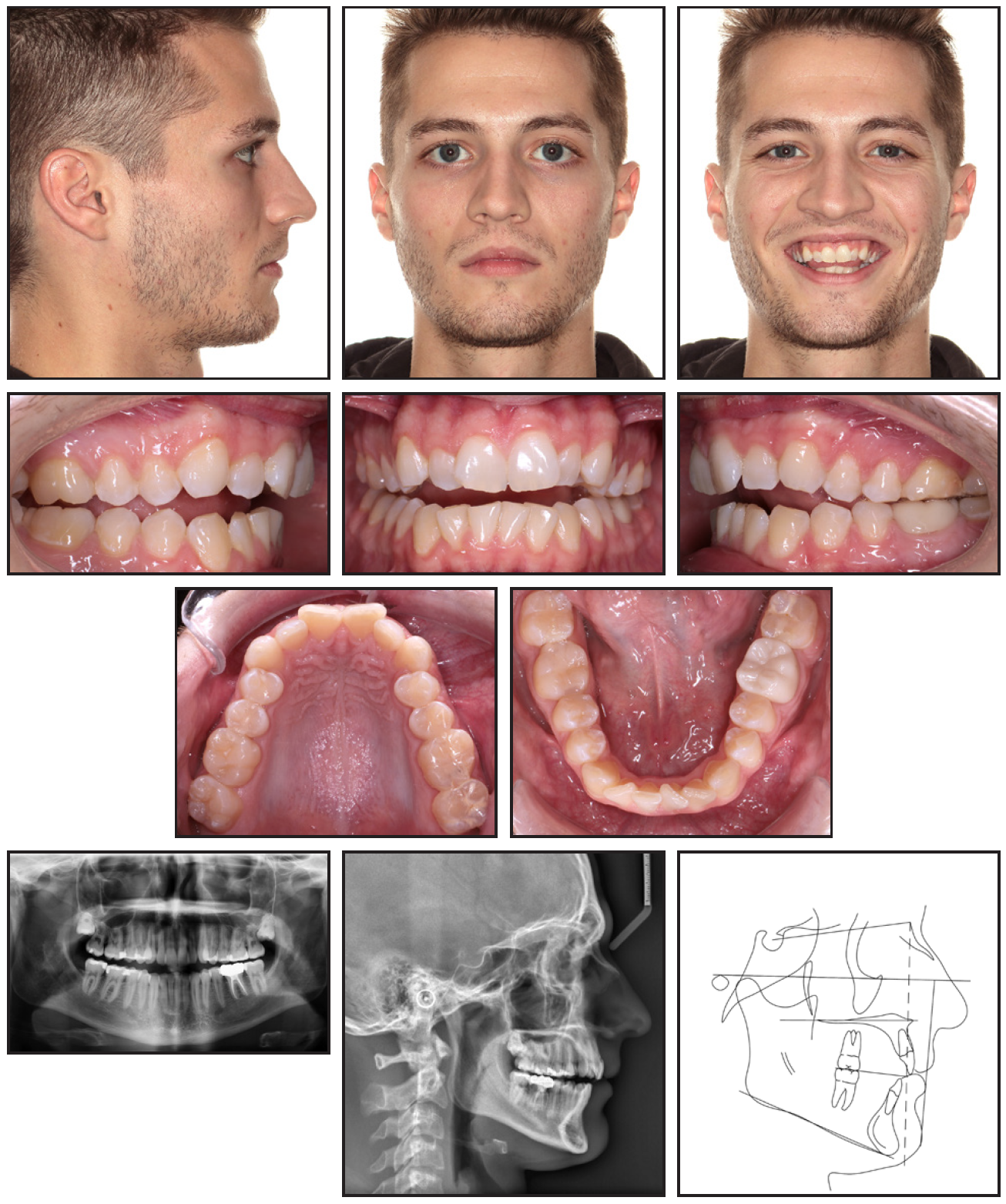
Fig. 1 23-year-old male patient with anterior and posterior open bites, retroclined upper and lower incisors, moderate lower crowding, and mild facial convexity before treatment.
The patient had a Class II, division 1 malocclusion with Class II canine relationships, an end-on Class II molar relationship on the right, and a tendency toward a Class II molar relationship on the left, with moderate crowding in the lower arch. The overjet was excessive (4mm), the upper incisors were retroclined (U1-SN = 94°), and the lower incisors were normally inclined (IMPA = 87°). A 3mm anterior open bite was present from canine to canine, along with a 1mm posterior open bite from the upper right first premolar to first molar and at the upper left first premolar. A mild upper curve of Spee and moderate lower reverse curve of Spee were present. The transpalatal width was diminished (32mm), with a 1mm transverse discrepancy at the first molars.
Cephalometric analysis (Table 1) indicated a skeletal Class I relationship (ANB = 3.5°, Wits appraisal = +.6mm) with an orthognathic maxilla (SNA = 81°) and a slightly retrognathic mandible (SNB = 77°). The mandibular plane angle (FMA = 22°) and facial height (N-ANS = 55mm, ANSMe = 76mm) were normal.
The treatment objectives were to improve mastication and smile esthetics by correcting the anterior and posterior open bites, establishing Class I molar and canine relationships, resolving the lower crowding, and coordinating the arches. We planned a nonsurgical, nonextraction approach for the initial treatment. If necessary, selective extractions would be performed at a later stage. We planned to procline the upper incisors 10-15° and the lower incisors about 5°. In addition, the upper incisors would be extruded 1-2mm, and the lower incisors 2-3mm, to level the curves of Spee. The upper intermolar width would be expanded by about 1mm.
Treatment Progress
After the patient received a periodontal evaluation and his dentist’s approval for treatment, .018" full fixed appliances* were placed. The upper and lower first molars were banded, and brackets were bonded from second premolar to second premolar in both arches.
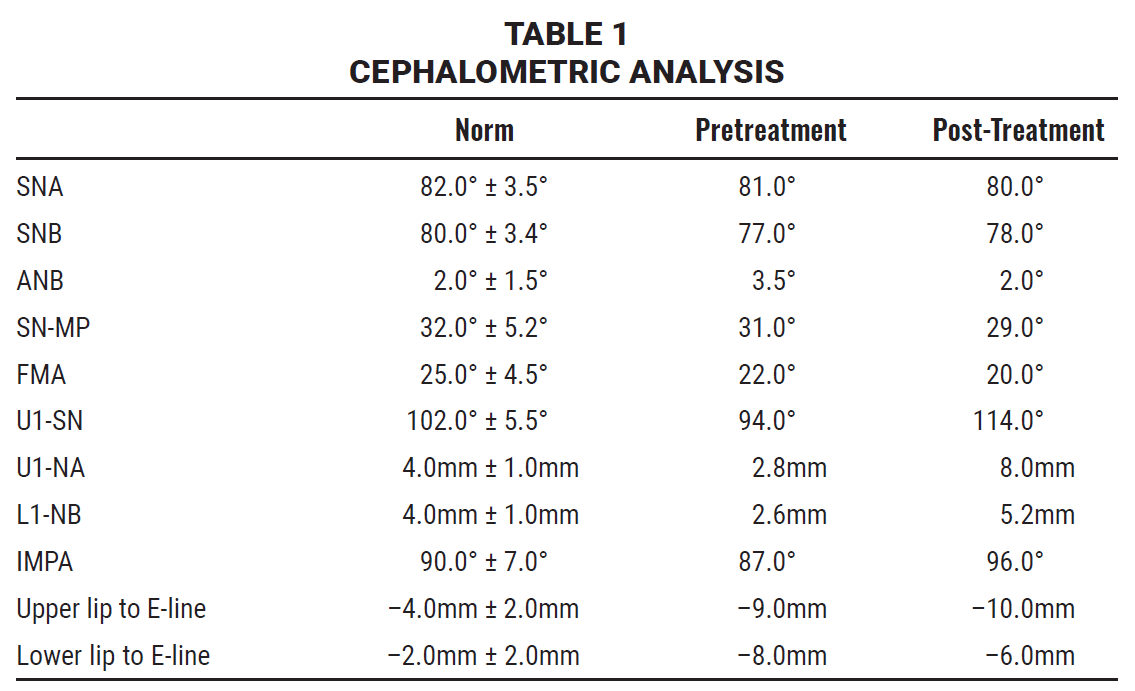
Initial leveling and alignment were performed over three months with a sequence of .016" nickel titanium, .016" stainless steel, and .016" × .016" stainless steel archwires. During this phase, the patient wore bilateral ¼", 3.5oz anterior vertical elastics full-time from the upper to lower canines. The –3mm anterior open bite was corrected to a 2mm overbite while both arches were leveled (Fig. 2).
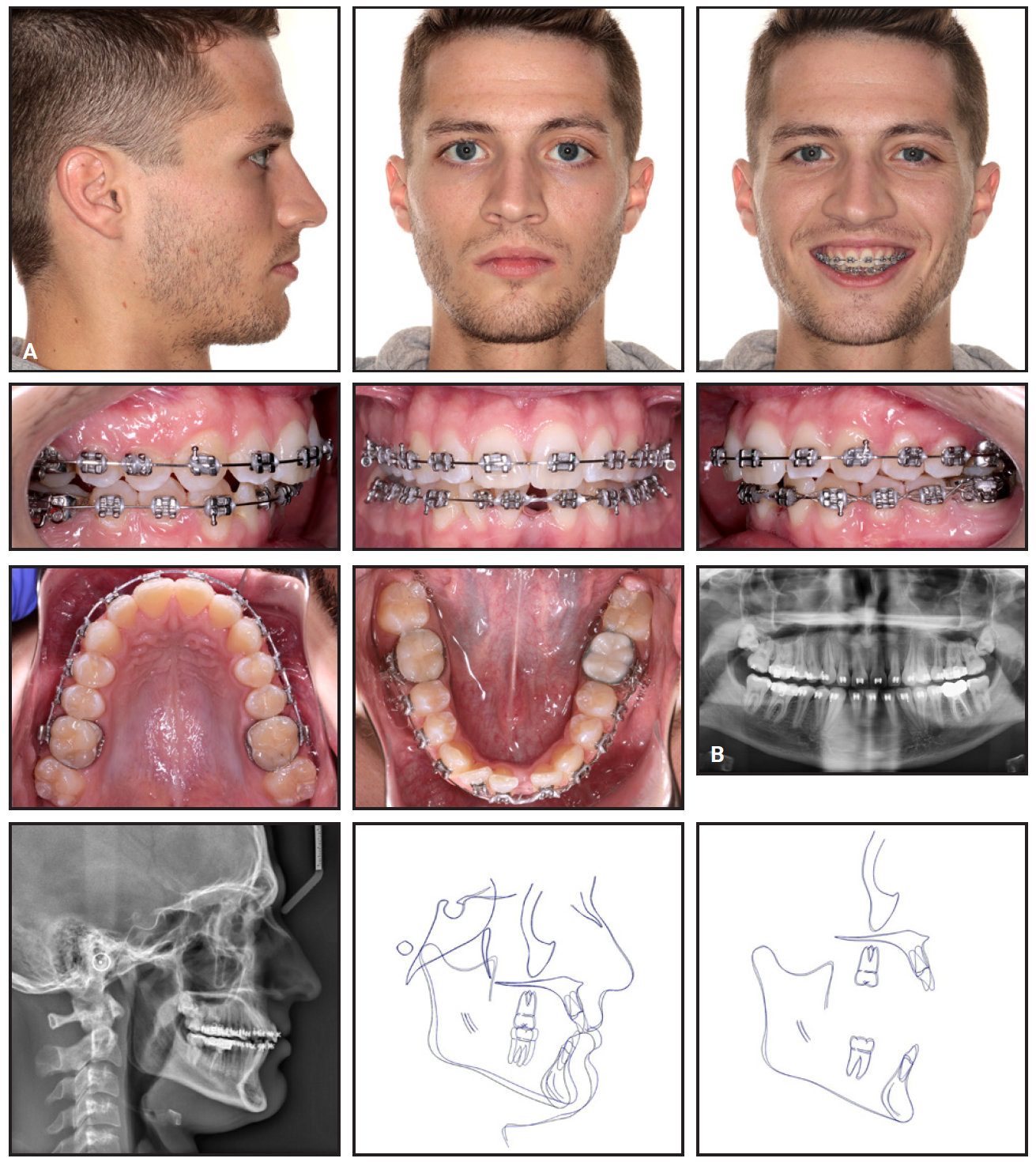
Fig. 2 A. After five months of treatment, showing improvement in overbite after initial alignment and anterior vertical elastic wear. B. Incisor proclination and mandibular autorotation visible on lateral cephalogram and superimposition (black = pretreatment, blue = progress) after 14 months of treatment.
Three options for further treatment were then presented to the patient: extraction of the upper first premolars and lower second premolars; extraction of the lower left central incisor; or interproximal reduction at the lower incisors, leaving some residual crowding. After discussion of the advantages and limitations of each approach, the patient opted for extraction of the lower left central incisor.
Following the incisor extraction, space closure was conducted with power chains on .016" × .022" stainless steel archwires. Class II elastics (¼", 6oz) were worn for about four months to produce the Class II correction. The final phase of treatment involved finishing bends for detailing and arch coordination.
The total active treatment time was 25 months (Fig. 3). After debonding, two sets of upper and lower active clear retainers were delivered. The first set, worn full-time for two weeks, was designed to manage a small amount of residual lower incisor crowding and remaining spaces from the molar bands. The second set, designed for long-term retention, was worn full-time for six months, then at night indefinitely. The patient planned to address the impacted upper third molars with his general dentist.
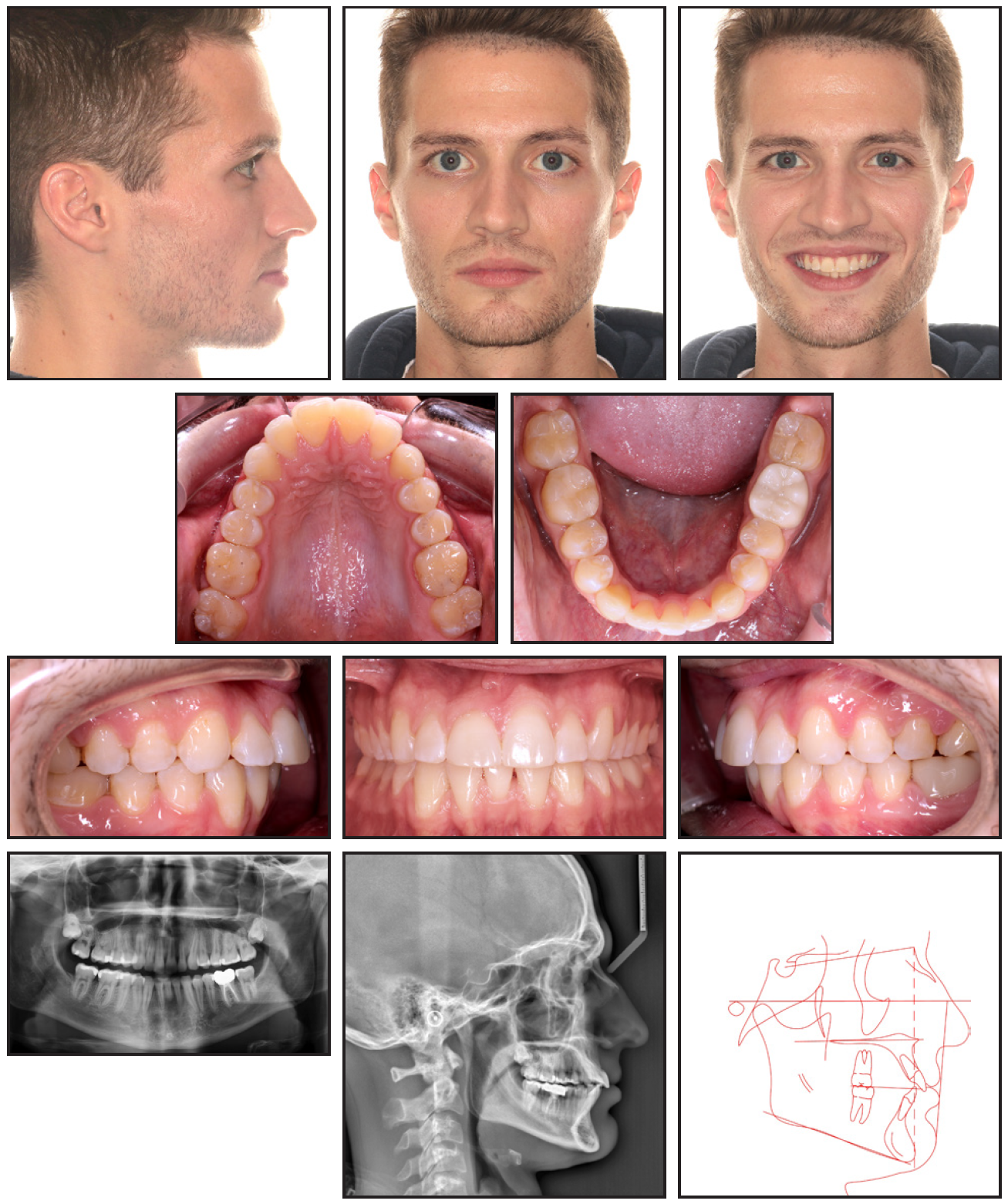
Fig. 3 After total 25 months of treatment, demonstrating closure of anterior and posterior open bites, improved incisor inclination, and enhanced facial esthetics.
Treatment Results
The anterior and posterior open bites were closed, resolving the patient’s chief complaint of difficulty chewing. Class I molar and canine relationships were established bilaterally. A positive overbite of about 2mm was achieved, although a 3-4mm overjet remained because of the lower incisor extraction and resulting Bolton discrepancy.
Cephalometric analysis showed minimal skeletal changes, with SNA decreasing 1°, SNB increasing 1°, and ANB decreasing 2° (Table 1). A 2° reduction in FMA was attributable to counterclockwise rotation of the mandible induced by a slight intrusion of the lower molars and the use of anterior vertical elastics. The upper incisors were proclined 20° (U1-SN = 114°) and protruded 5.2mm (U1-NA = 8mm), while the lower incisors were proclined 9° (L1-MP = 98.3°) and protruded 2.6mm (L1-NB = 5.2mm). The upper intermolar width increased 2mm, while the mandibular intercanine and intermolar widths remained unchanged. The reduction in profile convexity could be ascribed to incisor proclination, Class II correction, and a slight forward and upward rotation of the mandible. The upper lip was also slightly retruded (about 1mm) relative to the E-line, while the lower lip was protruded (about 2mm).
Mild gingival recession was noted on the lower right lateral incisor and canine, which is a well-documented side effect of incisor proclination.10,11 The patient was referred to a periodontist for evaluation.
Discussion
In this case, the combination of full fixed appliances with the strategic use of vertical and Class II elastics effectively closed an anterior open bite through both incisor extrusion and counterclockwise mandibular rotation, as previously reported.5,6,12 Anterior vertical elastics have been shown to successfully treat open-bite malocclusions through dentoalveolar rather than skeletal modifications12; the slight counterclockwise rotation of the mandible observed in this case also agrees with previous observations.6 Although recent studies have demonstrated acceptable stability for open-bite closure through incisor extrusion, there are still some concerns about long-term relapse.1,12,13
Premolar extractions can be used in conjunction with maximum anchorage mechanics to treat anterior open bites,12 but the required incisor retraction can negatively affect the soft-tissue profile.14 Extracting a lower incisor rather than a premolar can resolve moderate to severe mandibular crowding in Class II patients15,16 with minimal adverse effects on the facial profile,17 which is particularly beneficial in cases with mandibular Bolton discrepancies.
While treatment was largely successful in the present case, several modifications could have enhanced efficiency and improved the results. Extracting the lower left central incisor at the outset could have reduced the duration of treatment, although the delay did allow the patient to make an informed decision in light of initial progress. In addition, bonding the second molars for comprehensive arch control would have improved posterior torque and reduced the overjet.18 Additional detailing and correction of the slightly excessive overjet could have further refined the outcome, but we elected not to continue treatment because of the patient’s personal circumstances and satisfaction with the results already achieved.
As this case demonstrates, a comprehensive approach to orthodontic treatment can successfully manage complex dentoalveolar issues without surgical intervention, even in adult patients with established open bites.1,9,12 Nevertheless, the long-term stability of the anterior open-bite correction and the potential development of gingival recession after incisor proclination warrant close monitoring.10,11
FOOTNOTES
- *American Orthodontics, Sheboygan, WI; www.americanortho.com.
REFERENCES
- 1. Greenlee, G.M.; Huang, G.J.; Chen, S.S.; Chen, J.; Koepsell, T.; and Hujoel, P.: Stability of treatment for anterior open-bite malocclusion: A meta-analysis, Am. J. Orthod. 139:154-169, 2011.
- 2. Proffit, W.R.; Fields, H.W.; and Sarver, D.M.: Contemporary Orthodontics, 5th ed., Mosby Elsevier, St. Louis, 2012.
- 3. Todd, M.A. and Freer, T.J.: Case report—Anterior open bite as a complication of splint therapy, Aust. Orthod. J. 13:164-167, 1994.
- 4. Bereznicki, T.; Barry, E.; and Wilson, N.H.F.: Unintended changes to the occlusion following the provision of night guards, Br. Dent. J. 225:715-722, 2018.
- 5. Park, H.S.; Kwon, O.W.; and Sung, J.H.: Nonextraction treatment of an open bite with microscrew implant anchorage, Am. J. Orthod. 130:391-402, 2006.
- 6. Kim, Y.H.: Anterior openbite and its treatment with multiloop edgewise archwire, Angle Orthod. 57:290-321, 1987.
- 7. Baek, M.S.; Choi, Y.J.; Yu, H.S.; Lee, K.J.; Kwak, J.; and Park, Y.C.: Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth, Am. J. Orthod. 138:396. e1-396.e9, 2010.
- 8. Lee, J.; Choi, Y.J.; Park, J.H.; Chung, C.J.; Lee, J.H.; and Kim, K.H.: Surgical vs. nonsurgical treatments in patients with anterior open-bite have similar effects in occlusal function: A 2-year follow-up study, Am. J. Orthod. 165:38-45, 2024.
- 9. Cambiano, A.O.; Janson, G.; Lorenzoni, D.C.; Garib, D.G.; and Davalos, D.T.: Nonsurgical treatment and stability of an adult with a severe anterior open-bite malocclusion, J. Orthod. Sci. 7:2, 2018.
- 10. Joss-Vassalli, I.; Grebenstein, C.; Topouzelis, N.; Sculean, A.; and Katsaros, C.: Orthodontic therapy and gingival recession: A systematic review, Orthod. Craniofac. Res. 13:127-141, 2010.
- 11. Renkema, A.M.; Fudalej, P.S.; Renkema, A.; Kiekens, R.; and Katsaros, C.: Development of labial gingival recessions in orthodontically treated patients, Am. J. Orthod. 143:206-212, 2013.
- 12. Janson, G.; Valarelli, F.P.; Beltrao, R.T.; de Freitas, M.R.; and Henriques, J.F.: Stability of anterior open-bite extraction and nonextraction treatment in the permanent dentition, Am. J. Orthod. 129:768-774, 2006.
- 13. Lopez-Gavito, G.; Wallen, T.R.; Little, R.M.; and Joondeph, D.R.: Anterior open-bite malocclusion: A longitudinal 10-year postretention evaluation of orthodontically treated patients, Am. J. Orthod. 87:175-186, 1985.
- 14. Kocadereli, İ.: Changes in soft tissue profile after orthodontic treatment with and without extractions, Am. J. Orthod. 122:67-72, 2002.
- 15. Bahreman, A.A.: Lower incisor extraction in orthodontic treatment, Am. J. Orthod. 72:560-567, 1977.
- 16. Kokich, V.G. and Shapiro, P.A.: Lower incisor extraction in orthodontic treatment: Four clinical reports, Angle Orthod. 54:139-153, 1984.
- 17. Zhylich, D. and Suri, S.: Mandibular incisor extraction: A systematic review of an uncommon extraction choice in orthodontic treatment, J. Orthod. 38:185-195, 2011.
- 18. Dritsas, K.; Alharbi, M.; Kouvelis, G.; Kloukos, D.; and Gkantidis, N.: Effect of the timing of second molar bonding on the duration of the mandibular arch levelling: A randomized clinical trial, Eur. J. Orthod. 44:203-209, 2022.


COMMENTS
.