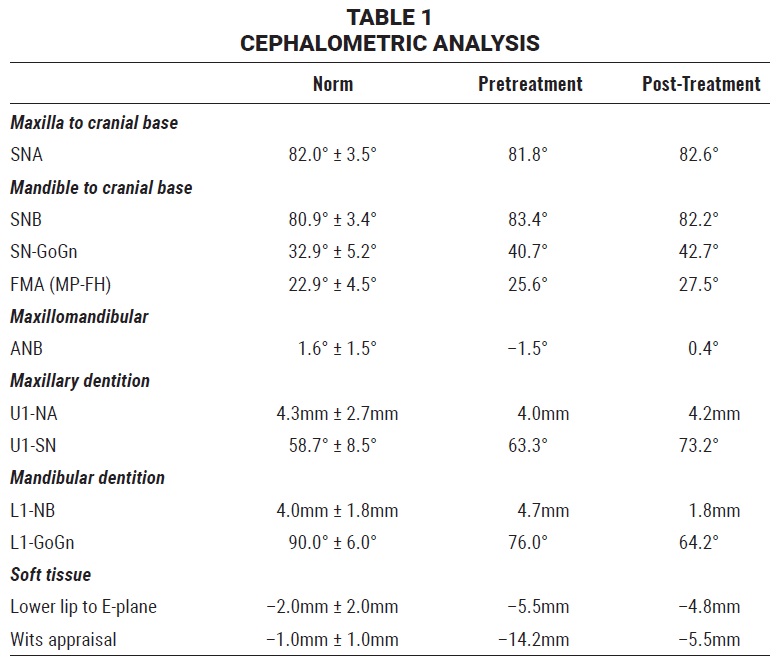
CASE REPORT
Nonsurgical Correction of a Severe Class III Open-Bite Patient with Long-Face Syndrome
An adult patient with a complex Class III malocclusion involving extreme sagittal and vertical disharmony generally requires surgical resolution of the skeletal discrepancy before the orthodontic issues can be resolved.1-4 If the patient refuses surgery, however, an orthodontic camouflage alternative may be needed.
The functional occlusal plane is represented by a line traced through the midpoint between the mesial cusps of the first molars and the cusps of the canines (or, in the case of ectopic lower canines, the cusps of the first premolars). Any change in the cant of the functional occlusal plane will directly affect the sagittal relationship of the maxilla and mandible. Counterclockwise rotation of the occlusal plane can restore proper molar mastication by establishing a Class I posterior platform early in treatment.4-7
The Class III Carriere Motion 3D is a one-piece device that positions the dentition in a Class I platform from molars to canines (Fig. 1).2,8,9 The anterior pad is bonded to the lower canine and incorporates a hook for attachment of Class III elastics. The central arm passes over the two lower premolars with a slight curve following the contour of the dental arch. This segment is oval in its vertical cross-section to add rigidity while maintaining axial control of the lower canines and molars. Between the second premolar and molar, the arm flattens transversely to provide greater lateral flexibility; an offset bayonet bend and toe-in angulation produce a small, 10° distal rotation of the lower posterior pad, which is bonded to the molar.6,9-11 A Class II Carriere Motion Appliance can be substituted in a Class III patient with missing lower molars.
Similar articles from the archive:
- Nonsurgical Camouflage Treatment of Skeletal Class III Malocclusion Using the Biocreative Reverse-Curve Technique July 2022
- CASE REPORT Nonsurgical Treatment of an Adult Skeletal Class III Patient with Compensated Dentition November 2021
- CASE REPORT Nonsurgical Correction of Class III Malocclusion and Anterior Open Bite with Mini-Implant Anchorage November 2018
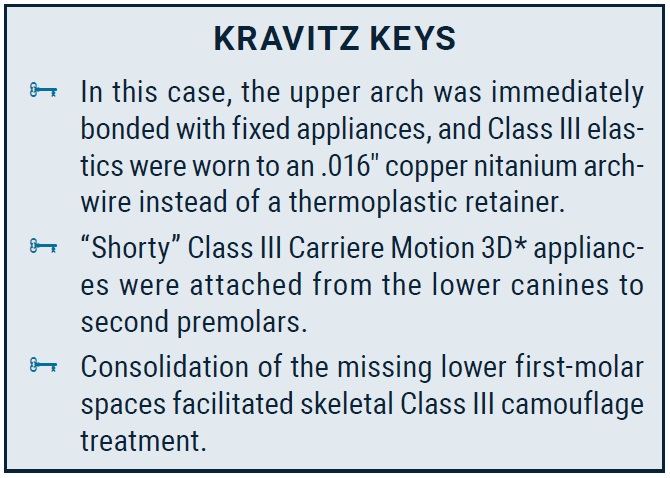
Diagnosis and Treatment Planning
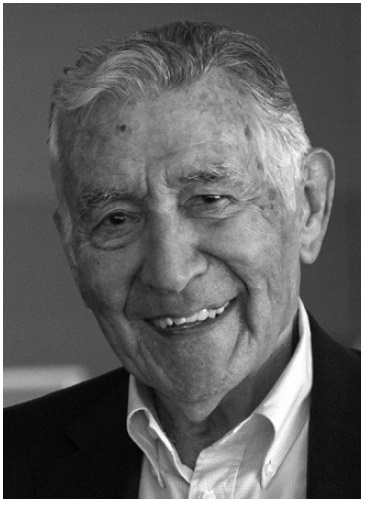
A 21-year-old male had visited several orthodontic offices looking for an orthodontic-only correction with an esthetic result. He was apprehensive about undergoing surgery, and he wanted to preserve his intrinsic familial facial characteristics. His goals were to improve the obvious prognathism; recover a normal masticatory function; and correct the dental-arch alignment, crossbite, open bite, high upper canines, and crooked anterior teeth.
The morphological diagnosis was a skeletal Class III malocclusion with a hyperdivergent long face, maxillary hypoplasia, transverse constriction, and hyperplastic mandible (Fig. 2A).
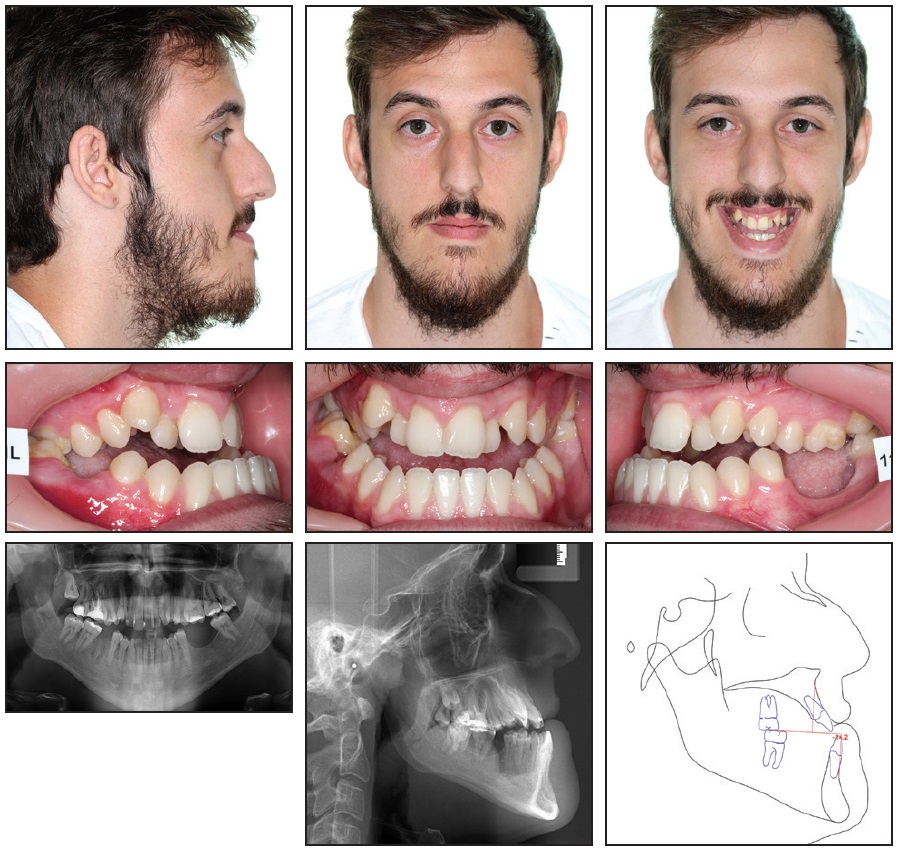
Fig. 2 21-year-old male patient with skeletal Class III malocclusion, hyperdivergent long face, maxillary hypoplasia, transverse constriction, and hyperplastic mandible before treatment (continued in next image).
The dental arches increased in divergence from the first permanent molars to a 5mm anterior open bite, resulting in a negative overjet and a full crossbite—a challenging condition with a high risk of root resorption over a long period of treatment. The lower right first molar and left first and second molars were missing, and the upper arch had two high canines (Fig. 2B).
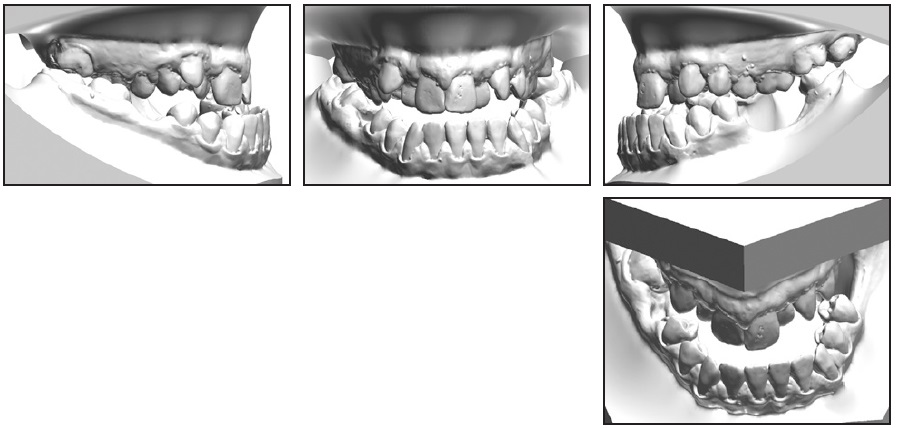
Fig. 2 (cont.) 21-year-old male patient with skeletal Class III malocclusion, hyperdivergent long face, maxillary hypoplasia, transverse constriction, and hyperplastic mandible before treatment.
The neuromuscular pattern was hypotonic; the patient’s leptosomic body type was reflected in a poor masticatory stroke in the masseter and temporalis muscles. The tongue and its elevating musculature were hypertrophic, with improper function at rest and when chewing and swallowing.
We wanted to treat the case step by step, in an order determined by the degree of relevance of each problem to the overall malocclusion. These problems included the Class III dolichofacial pattern; extreme anterior open bite; premaxillary hypoplasia with severe upper crowding; transverse discrepancy with bilateral posterior crossbite; severe anterior crossbite, negative overjet, retroclined lower incisors, and lower crowding; retrusive upper lip, protrusive lower lip, flat mentolabial groove, protrusive chin point, and concave profile; and missing lower molars.
When the patient rejected the proposed surgical-orthodontic treatment, we applied the “sagittal first” principle in planning nonsurgical orthodontic treatment with a sequence of movements from distal to mesial.1,2,7,9 Treatment goals were to correct the Class III malocclusion, close the anterior open bite, correct the posterior crossbite, protract the maxillary teeth, retract the mandibular teeth, and effect a counterclockwise rotation of the posterior functional occlusal plane to balance the Wits appraisal7 (Table 1). The soft-tissue Class III relationship would be improved by mesializing the lower right second and third molars into the space of the missing first molar, thus avoiding the need for a future implant.
Myofunctional Therapy
In any open-bite case, we prioritize myofunctional therapy. This patient’s tongue and skeletal condition would have interfered with tooth movement, lengthening treatment and increasing the risk of severe root resorption and future relapse. To correct a tongue dysfunction, we use an in-office rehabilitation program involving three tongue positions: at rest, when chewing, and when swallowing (Fig. 3).
A hypertrophic tongue rests between the dental arches, with the lips sealed and in strong contraction. The tongue protrudes between the teeth to produce a third point of contact with the lips. A negative pressure is thus produced inside the mouth relative to the outside atmospheric pressure. The exercise for this position involves the following steps:
- The lips are parted to balance the oral-cavity pressure with the pressure outside the mouth.
- After relaxing the tip of the tongue, the patient directs it to contact a point on the palatal rugae. The tongue should not move beyond this point when at rest.
- The base of the tongue is then directed back and down to the rear of the oral cavity.
If the dental arches are inefficient in chewing, the tongue compensates by pushing the food bolus against the hard palate and the lingual aspects of the teeth, acting as an alternative masticatory organ. These forces cause hypertrophy of the striated muscular fibers and an increase in tongue volume, aggravating the open bite and interfering with orthodontic treatment. We use chewing gum in the exercise for this position:
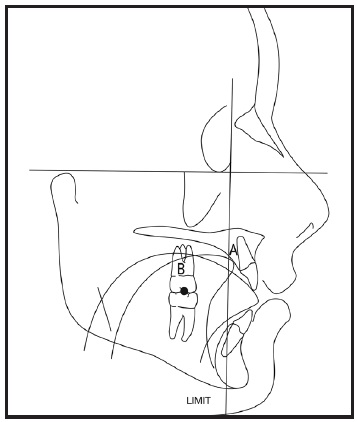
Fig. 3 Tongue rehabilitation exercises for open-bite patient A: Point to place tip of tongue at rest and as starting point for deglutition. B: Specific zone for molar mastication and for clenching contact when swallowing. Limit: Line not to be crossed by tip of tongue.
- The lips are parted to prevent the tip of the tongue from protruding between the teeth to contact the lips.
- While chewing gum, the patient uses the tongue to direct the gum to the molar regions, thus stimulating the masseter and temporalis muscles to retrain molar chewing function.
- After the patient learns exclusively molar mastication, this exercise can be generalized to chewing during regular meals.
In swallowing, a hypertrophic tongue is projected between the anterior teeth, actively contributing to the open bite and the risk of root resorption, interfering with tooth movement, and compromising long-term stability. The patient therefore needs to practice synchronizing these three positions:
- The lips are parted to prevent protrusion of the tip of the tongue.
- The posterior bite is clenched so that the molars make contact at a specific point.
- The tip of the tongue is placed against the palatal rugae, and the deglutition wave begins from this point backward.
Treatment Progress
Although a vacuformed maxillary retainer can be used for attachment of Class III elastics, we decided to start with upper leveling in this case to help develop the maxillary arch and maximize soft-tissue support in the upper lip. After MBT**-prescription .022" Carriere SLX passive self-ligating brackets were bonded, a maxillary .014" round copper nitanium (27°C) archwire was used for four weeks (Fig. 4).

The maxillary archwire was then changed to .016" round copper nitanium (27°C), and “shorty” Class III Carriere Motion 3D appliances were placed from the lower canines to second premolars to begin distalizing the lower posterior segments with Class III elastics and thus correct the negative overjet (Fig. 5). Lower posterior build-ups were bonded to avoid occlusal interference with the upper molar tubes. This temporarily increased the anterior open bite but enabled us to work on the transverse dimension while simultaneously beginning the sagittal correction.

Fig. 5 After four weeks of treatment, upper .016" round copper nitanium (27°C) archwire inserted; “shorty” Class III Carriere Motion 3D appliance placed from lower canines to second premolars to distalize lower posterior segments and correct negative overjet.
Four weeks later, the maxillary archwire was changed to .014" × .025" copper nitanium (27°C) to finish the sagittal correction (Fig. 6). A positive overjet was achieved in eight weeks. At this point, we noted a slight increase in the open bite caused by a premature occlusal contact of the lower third molars and the upper second and third molars, which were undergoing transverse correction.

Fig. 6 Four weeks later, upper archwire changed to .014" × .025" copper nitanium (27°C) to complete sagittal correction.
After the Carriere Motion 3D appliances were removed, the mandibular arch was bonded with .022" Carriere SLX passive self-ligating brackets, and an .014" round copper nitanium (27°C) archwire was inserted (Fig. 7). Four tongue tamers were also bonded to the lingual surfaces of the lower incisors, and the maxillary archwire was changed to .017" × .025" copper nitanium (35°C).

Fig. 7 After 16 weeks of treatment, Carriere Motion 3D appliances removed, upper archwire changed to .017" × .025" copper nitanium (35°C), .022" Carriere SLX passive self-ligating brackets and .014" round copper nitanium (27°C) archwire placed in lower arch, and four tongue tamers bonded to lower incisors.
Four weeks later, we placed maxillary .019" × .025" copper nitanium (35°C) and mandibular .016" round copper nitanium (27°C) archwires, along with power chain to begin moving the lower right second molar into the space of the first molar and the third molar into the space of the second molar (Fig. 8).

Fig. 8 Four weeks later, upper .019" × .025" copper nitanium (35°C) and lower .016" round copper nitanium (27°C) archwires inserted, along with power chain to move lower right second molar into space of first molar and third molar into space of second molar.
In another four weeks, the archwires were changed to maxillary .019" × .025" copper nitanium (35°C) and mandibular .014" × .025" copper nitanium (27°C), and the lower right second molar tube was rebonded more mesiogingivally for molar uprighting. A nickel titanium closed-coil spring and ligature were applied to move the lower right second molar mesially into the space of the first molar.
Four weeks later, we inserted maxillary .019" × .025" copper nitanium (35°C) and mandibular .017" × .025" copper nitanium (35°C) archwires, which were again worn for four weeks. Maxillary .019" × .025" beta titanium and mandibular .019" × .025" copper nitanium (35°C) archwires were applied for the next eight months (Fig. 9).
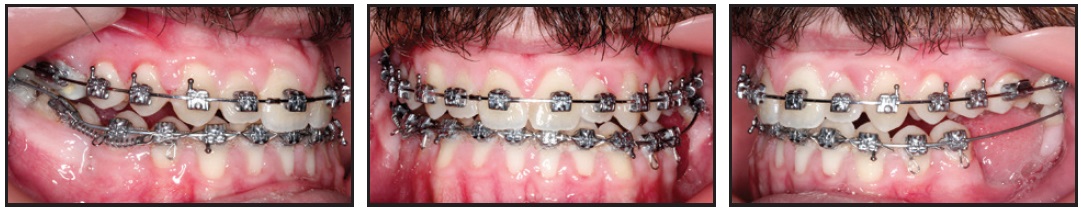
Fig. 9 After 32 weeks of treatment, archwires changed to upper .019" × .025" beta titanium and lower .019" × .025" copper nitanium (35°C).
The mandibular archwire was then changed to .019" × .025" beta titanium for five additional months.
Maxillary .021" × .027" nickel titanium and mandibular .019" × .025" beta titanium archwires were used, along with finishing intermaxillary vertical elastics, during the final four weeks of treatment (Fig. 10).

Fig. 10 Upper .021" × .027" nickel titanium and lower .019" × .025" beta titanium archwires used for four weeks of finishing at end of treatment.
Treatment Results
Total treatment time was 22 months (Fig. 11).
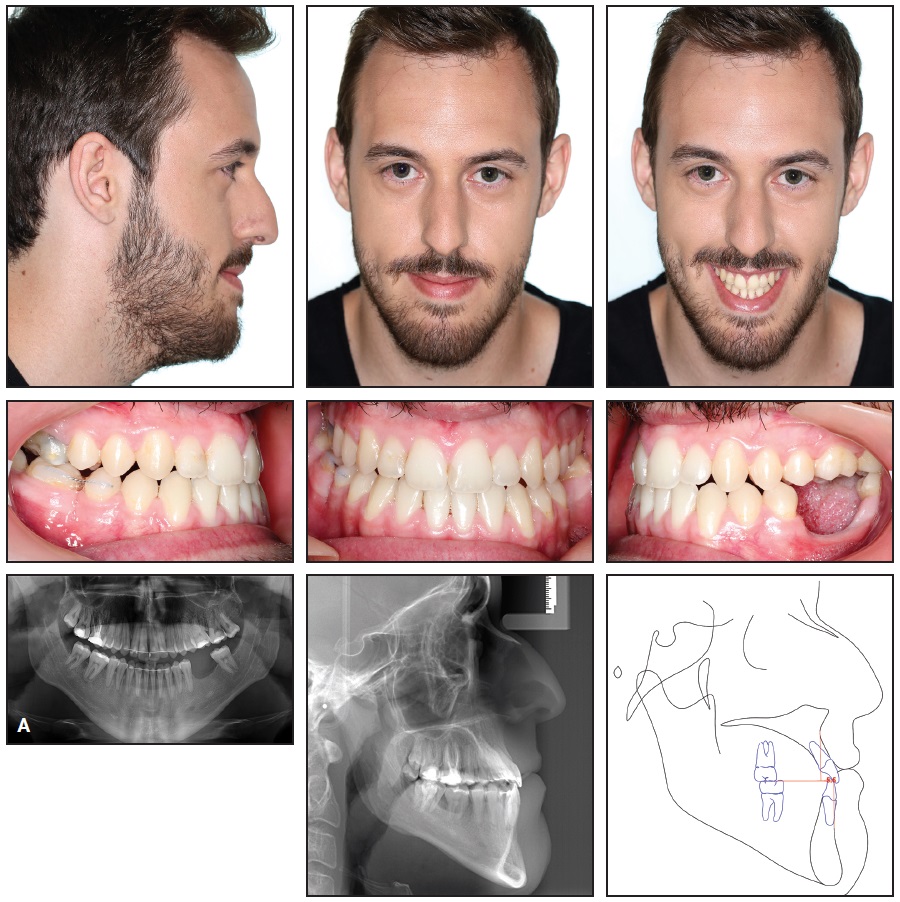
Fig. 11 A. Patient after 22 months of treatment (continued in next image).
The patient showed an improvement in the sagittal spatial geometry of the intermaxillary relationship, with a consequent improvement in his facial esthetics12 (Table 1). A minor distal movement of the mandible was seen, with no change in the size of the maxilla or mandible, and proper molar mastication was recovered (Fig. 11B).
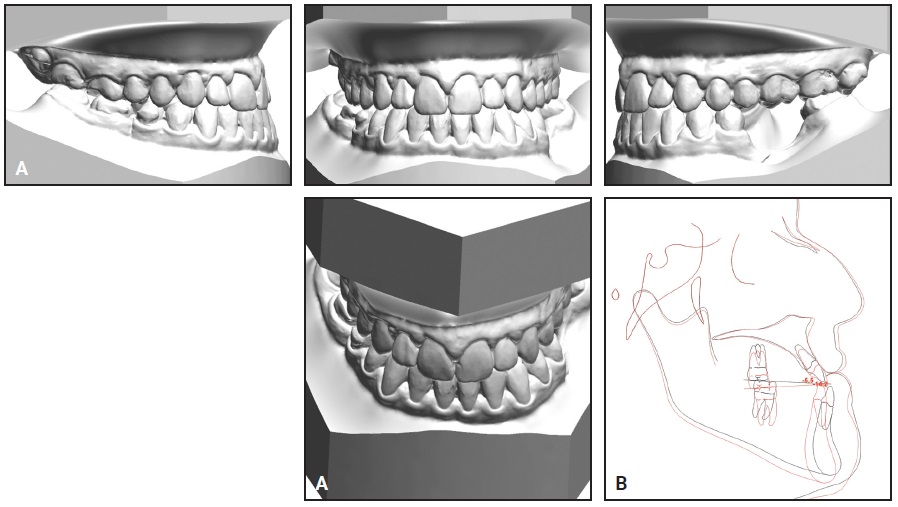
Fig. 11 (cont.) A. Patient after 22 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
Fixed upper and lower lingual retainer wires and nighttime vacuformed retainers were prescribed; in addition, a small segment of wire was bonded buccally to stabilize the lower right second molar by interproximal connection with the lower second premolar (Fig. 12).

Fig. 12 Patient 18 months after treatment.
After 18 months of retention, only the buccally bonded wire was continued (Fig. 13).

Fig. 13 Patient five years after treatment, with no retention after 18 months other than buccal interproximal connector between lower right second molar and second premolar.
Discussion
The complexity of this case required us to prioritize the various problems contributing to the skeletal Class III malocclusion. The most urgent issue was to recover a proper tongue function. Along with the use of light force, that made it possible to avoid the occurrence of root resorption during treatment.
Since the patient refused surgery, we took advantage of the many beneficial effects offered by the Class III Carriere Motion 3D appliance, in addition to mandibular distalization. The cant of the functional occlusal plane was tipped back, producing a direct improvement in the Wits appraisal. The elastic traction on the appliance enabled a counterclockwise rotation of the functional occlusal plane, improving the intermaxillary relationship and the prognathic appearance of the patient̓s face.
This nonsurgical treatment enhanced the patient’s facial esthetics without changing his intrinsic family traits, thus addressing his primary concern. His psychosocial relationships, self-esteem, and confidence had improved by the end of treatment.4-6,9
FOOTNOTES
- *Registered trademark of Henry Schein Orthodontics, Melville, NY; www.henryscheinortho.com.
- **Trademark of 3M, Monrovia, CA; www.3M.com.
REFERENCES
- 1. Carrière, L.: Hippocratic philosophy: Biominimalism and new technologies: Innovation in a new orthodontic treatment method and optimization of the facial icon, lecture, Royal Academy of Doctors induction ceremony, Barcelona, Spain, 2015.
- 2. Carrière, J.: Inverse Anchorage Technique in Fixed Orthodontic Treatment, Quintessence Publishing Co., Inc., Batavia, IL, 1991.
- 3. Proffit, W.R. and Ackerman, J.L.: A systematic approach to orthodontic diagnosis and treatment planning, in Current Orthodontic Concepts and Techniques, 3rd ed., ed. T.M. Graber and B.F. Swain, C.V. Mosby, St. Louis, 1985.
- 4. Burstone, C.J. and Marcotte, M.: Problem Solving in Orthodontics: Goal-Oriented Treatment Strategies, Quintessence Publishing Co., Inc., Chicago, 2000.
- 5. Jacobson, A.: The “Wits” appraisal of jaw disharmony, Am. J. Orthod. 67:125-138, 1975.
- 6. Jacobson, A.: Update on the Wits appraisal, Angle Orthod. 58:205-219, 1988.
- 7. McNamara, J.A.; Franchi, L.; McClatchey, L.M.; Kowalski, S.E.; and Cheeseman, C.C.: Evaluation of adolescent and adult patients treated with the Carriere Motion Class III appliance followed by fixed appliances, Angle Orthod. 91:149-156, 2021.
- 8. Benyus, J.M.: Biomimicry: Innovation Inspired by Nature, HarperCollins Publishers, Inc., New York, 2002.
- 9. Carrière, L.: Nonsurgical correction of severe skeletal Class III malocclusion, J. Clin. Orthod. 50:216-230, 2016.
- 10. Cetlin, N.M. and Ten Hoeve, A.: Nonextraction treatment, J. Clin. Orthod. 17:396-413, 1983.
- 11. Melsen, B.: Current Controversies in Orthodontics, Quintessence Publishing Co., Inc., Chicago, 1991.
- 12. Cussó i Anglés, J.: Gaudi’s Sagrada Familia: A Monument to Nature, Editorial Milenio, Barcelona, Spain, 2013.





COMMENTS
.