CASE REPORT
Management of a Mutilated Dentition with a Palatally Impacted Canine, Hypoplastic Lower First Premolars, and Missing Lower First Molars
Because each tooth plays a distinct role in the arch, its absence will cause particular effects. For example, the first permanent molars are essential to occlusal function and arch stability; their premature loss may cause mesial tipping or drifting of adjacent teeth or overeruption of opposing teeth, potentially resulting in marked dental asymmetry and poor interproximal contact.1-3 Absence of the upper canines, which are the cornerstones of the maxillary arch, will affect both esthetics and function.
In a mutilated dentition with multiple missing teeth, treatment becomes more challenging and is often prolonged.2 Patients with mutilated dentitions can present with additional concerns such as impactions, enamel hypoplasia, periodontal lesions, and TMJ disorders.4 Considering the difficulty of managing such complex cases, an accurate diagnosis and comprehensive treatment plan are essential. This case report documents the successful treatment of a patient with missing lower first molars, a palatally impacted upper left canine, enamel hypoplasia, and crossbite.
Diagnosis and Treatment Plan
A 20-year-old female presented with the chief complaints of misaligned and protrusive anterior teeth and gaps in the lower posterior regions, where both lower first molars had been extracted during childhood due to extensive decay. Clinical examination found a mesoprosopic facial form and straight profile, with an incompetent and short upper lip (Fig. 1A). The canines were in an edge-to-edge relationship on the right side, but the relationship on the left could not be assessed due to the absence of the upper left canine. An anterior crossbite involving both upper lateral incisors was evident. Both lower first molars were absent, and both lower first premolars showed signs of grade IV enamel hypoplasia. An overjet of 3.5mm and overbite of 2.5mm were noted.
Similar articles from the archive:
- CASE REPORT A Multidisciplinary Approach to Treatment of Multiple-Tooth Agenesis, Retention, and Impaction December 2023
- Controlled Slicing for Space Closure in Cases with Congenitally Missing Second Premolars April 2023
- CASE REPORT Treatment of a Patient with a Missing Lower Incisor and Three Impacted Teeth August 2021

Fig. 1 20-year-old female patient with palatally impacted upper left canine, enamel hypoplasia on lower first premolars, missing lower first permanent molars, anterior crossbite, and crowding before treatment (continued in next page).
The maxillary midline was shifted 1mm to the right of the facial midline, and the mandibular midline was shifted 2mm to the left of the maxillary dental midline. Occlusal caries were observed in both the upper first and lower second permanent molars. The anterior Bolton ratio was 62.3% (norm = 77.2% ± 1.6%), and the overall Bolton ratio was 81.1% (norm = 91.3% ± 1.9%). Severe crowding was found in the upper arch, with a space discrepancy of 14mm, while mild crowding (3mm discrepancy) was present in the lower arch (Fig. 1B).
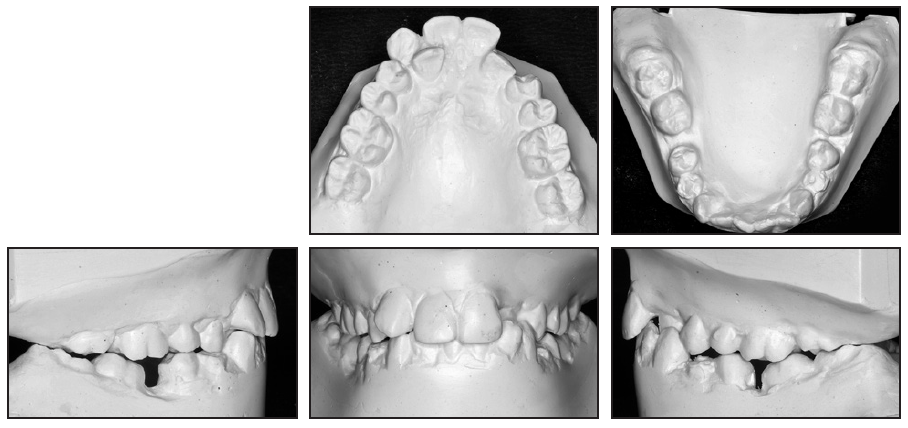
Fig. 1 (cont.) 20-year-old female patient with palatally impacted upper left canine, enamel hypoplasia on lower first premolars, missing lower first permanent molars, anterior crossbite, and crowding before treatment.
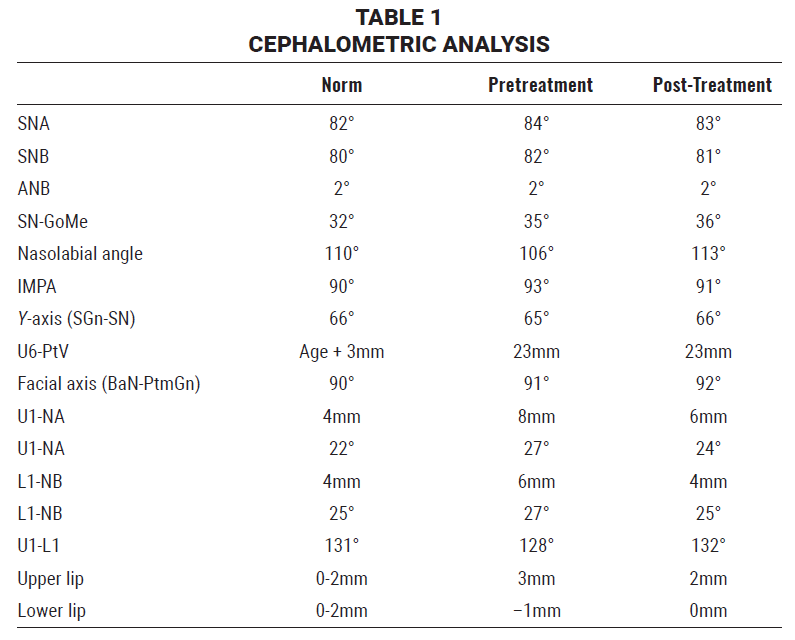
The panoramic radiograph revealed that the upper left canine was palatally impacted and that the lower second molars had tipped mesially into the extraction spaces of the lower first molars, but with no indication of bone loss in the edentulous regions. All third molars except for the upper left were present. Cephalometric analysis (Table 1) indicated a skeletal Class I relationship (ANB = 2°) with a hyperdivergent growth pattern (SN-GoMe = 35°) and a deficient interincisal angle (128°).
Treatment goals were to alleviate the crowding, incorporate the impacted upper left canine into the arch, close the spaces left by extraction of the lower first molars, and achieve a satisfactory occlusion. Additional objectives were to align both arches and to achieve coincident midlines and an ideal overjet and overbite, while preserving the profile and optimizing facial esthetics.
Following recommendations in the literature, the position of the canine was analyzed to determine its prognosis (Fig. 2).5-8 The canine cusp tip was in sector II, according to Ericson and Kurol’s system,5 close to the midline and overlapping the adjacent lateral incisor but not the central incisor. Although this position suggested a fair prognosis, the crown was above the halfway point of the central-incisor root, and the horizontal position of the canine root apex was higher than normal, both indicating a better prognosis. Finally, the canine had a mesial angulation of 30° in relation to the midline, which suggested a fair prognosis. Based on the overall favorable prognosis for the impacted left canine, a guided orthodontic eruption after surgical exposure was determined to be the most suitable approach.
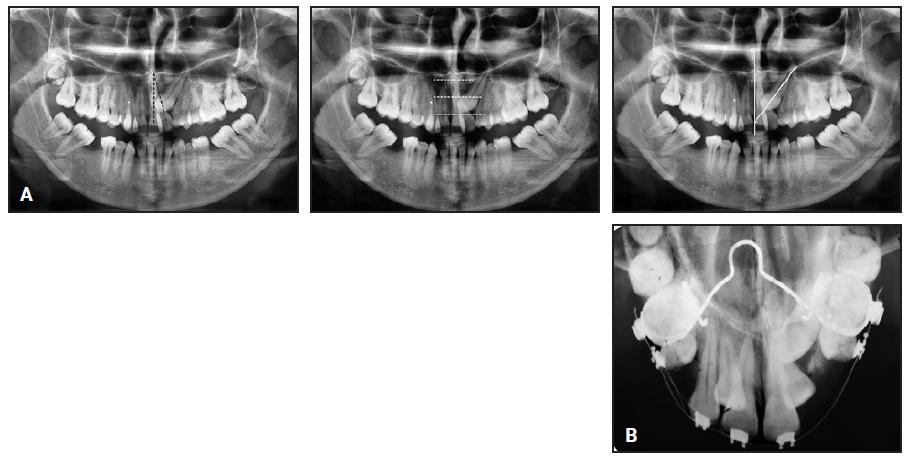
Fig. 2 A. Radiographic assessment of impacted upper left canine to determine prognosis. B. After 10 weeks of treatment, new radiograph taken to plan surgical procedure.
Since the impacted canine was positioned high in the palate, well above the mucogingival junction, a closed-eruption surgical technique was deemed appropriate.9 To address the remaining concerns, one treatment option would involve extracting all four first premolars and using prosthetic implants to replace the missing lower first permanent molars, resulting in a Class I molar relationship. The second option would be to extract the upper first premolars and upright the lower second permanent molars, resulting in a Class II molar relationship. After an explanation of the prolonged treatment time either course would require, the patient chose the second option to avoid the need for prosthetic implants.
Treatment Progress
The upper first premolars were extracted to alleviate the upper crowding. Two weeks later, the upper arch was banded and bonded with MBT*-prescription .022" x .028" preadjusted edgewise brackets, except for the blocked-in upper lateral incisors. Leveling and alignment were performed using a series of progressively larger nickel titanium wires (.012", .014", .016", and .016" × .022"), changed every five weeks.
After five months of treatment, an open-coil spring was inserted between the upper right central incisor and canine on an .017" × .025" stainless steel archwire to open space for the blocked-in upper right lateral incisor (Fig. 3A). To align the left lateral incisor, an .012" “piggyback” nickel titanium archwire was inserted. Posterior bite blocks were cemented to the lower arch to prevent interference and facilitate tooth movement. At the same time, the closed-eruption technique was used to surgically expose the impacted upper left canine (Fig. 3B). A lingual button was bonded to the canine for attachment of an .011" ligature wire, with its ends emerging from the sutured flap of gingival tissue. To preserve the extraction space and prevent tipping of the neighboring teeth during traction, a sleeve was placed between the upper left lateral incisor and second premolar.
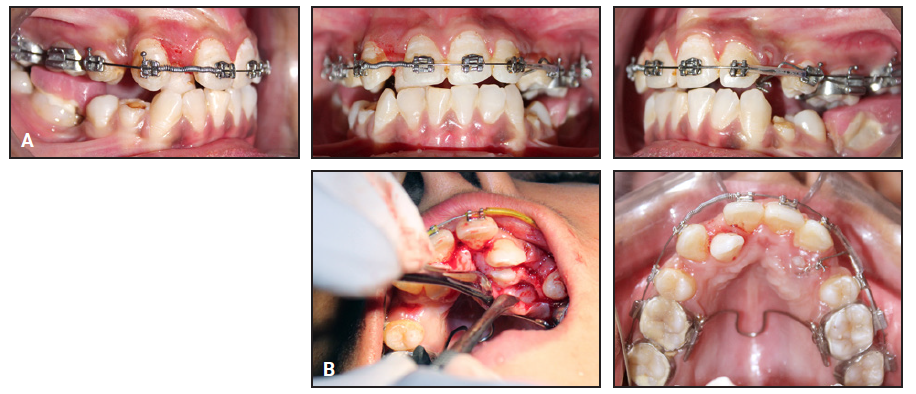
Fig. 3 A. After five months of treatment, open-coil spring inserted between upper right central incisor and canine. B. Closed-eruption surgical technique performed on impacted upper left canine, and K-9 spring placed.
Since immediate traction is generally beneficial after surgical exposure of palatally impacted canines in late adolescents and young adults, orthodontic eruption was initiated as soon as inflammation from the surgery had subsided. A K-9 extrusion spring was bent from .017" × .025" TMA** wire to guide the impacted canine into the extraction space.10 The spring was engaged in the auxiliary slot of a buccal tube on the upper left first molar and activated by bending its vertical arm upward and attaching it to the button on the impacted canine, thus applying a light extrusive force. With a pattern of alternating activation and deactivation, the spring also exerted the buccal component of force needed to bring the canine into the arch. While the reactive force of activation with the vertical arm of a K-9 spring applies an intrusive force and a clockwise moment to the molars and premolars, any side effects are generally minor.10,11 Movement of the canine was facilitated by cinching the spring back about 2mm.
Over the next eight months, the progress of canine eruption was monitored with monthly appointments. No complications were observed at the surgical site, and the gingiva remained healthy. After the crown of the impacted canine had erupted, it was bonded and engaged in the archwire. For another eight months, progressively larger stainless steel wires (.016", .017" × .025", and .019" × .025") were securely tied for leveling and alignment.
After the upper arch was aligned, the bite blocks were removed (Fig. 4), and leveling and alignment of the lower arch were initiated with an .012" nickel titanium archwire. The wires were changed three times, every four weeks, progressing up to .016" × .022" nickel titanium.

Fig. 4 After 21 months of treatment, leveling and alignment of maxillary arch completed and posterior bite blocks removed.
Four months later, bilateral helical uprighting springs were fabricated from 15-20mm lengths of .017" × .025" TMA wire on an .017" x .025" stainless steel base (Fig. 5). The springs were passed through buccal tubes on the lower second molars, with the helices distal to the tubes. Hooks were added at the mesial ends of the springs for attachment to the archwire between the lower canines and lower first premolars, so that each uprighting spring applied 50g of force. The force exerted on the anchor units was assessed every four weeks using a Dontrix gauge, and the springs were reactivated if necessary. After four months of treatment with the springs, uprighting of the lower second molars was complete.

Fig. 5 After 25 months of treatment, helical uprighting springs inserted bilaterally for uprighting of lower second molars.
Another month later, a 1.5mm x 8mm mini-implant was inserted between the upper right first molar and second premolar to provide skeletal anchorage for Class III elastics (3⁄16", 4.5oz); at the same time, to close the remaining space and correct the midline shift, Class II elastics (3⁄16", 4.5oz) were worn between a hook distal to the upper left lateral incisor and a hook on the lower left second-molar tube (Fig. 6).
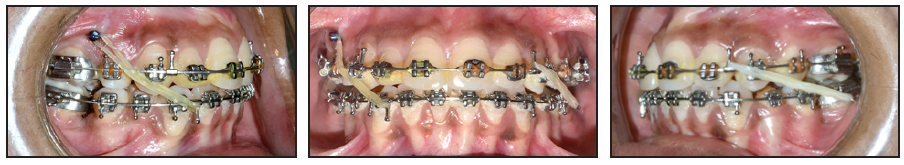
Fig. 6 After 30 months of treatment, mini-implant inserted between upper right first molar and second premolar for attachment of Class III elastics on right side, and Class II elastics worn on left side.
Two months later, after complete closure of the extraction space, final settling was performed on an .014" nickel titanium archwire, and zirconia crowns were cemented on the hypoplastic lower first premolars.
After a total 32 months of treatment, the fixed appliances were removed, and upper 4-4 and lower 3-3 lingual retainer wires were bonded.
Treatment Results
All treatment objectives were accomplished. An acceptable occlusion was achieved, with Class II molar relationships and Class I canine relationships on both sides, good intercuspation, coincident dental and facial midlines, and appropriate overjet and overbite (Fig. 7A).
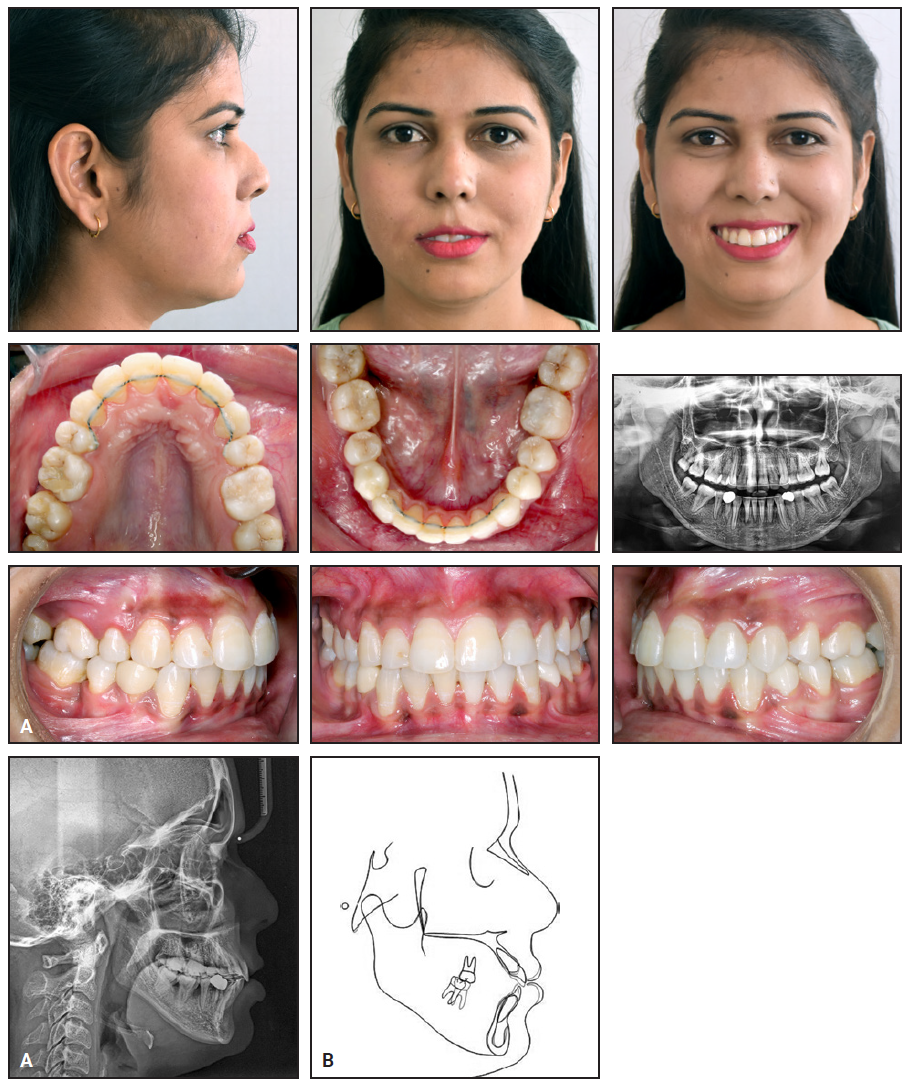
Fig. 7 A. Patient after 32 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings (continued in next image).
The crowding was relieved in both arches, and the crossbite was corrected. The impacted upper left canine was successfully integrated into the arch. Post-treatment panoramic radiographs revealed satisfactory root parallelism without significant resorption. Cephalometric analysis (Table 1) indicated an improved incisor inclination (U1-NA = 6mm, 24°; L1-NB = 4mm, 25°; SN-GoMe = 36°; IMPA = 91°). To prevent further complications, the patient was advised to have the upper right third molar extracted,12 but she expressed satisfaction with the treatment results and declined any further surgical procedures (Fig. 7B).
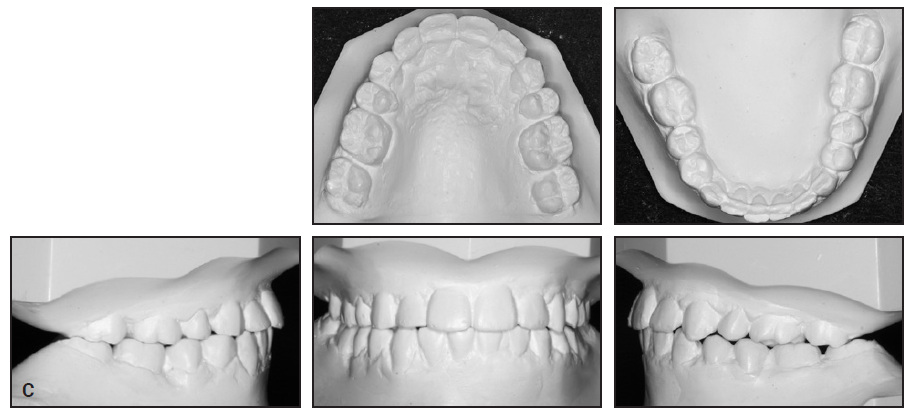
Fig. 7 (cont.) C. Post-treatment casts.
Discussion
It is unusual to encounter a mutilated dentition in which an impacted canine, missing molars, enamel hypoplasia, crowding, and crossbite occur together. Management of such a complex case must consider space creation for the impacted canine, restoration of the hypoplastic teeth, and options for replacement of the absent molars, among other factors.
Impaction of an upper canine occurs twice as often in females as in males; after the third molars, the canines are the most frequently impacted teeth. Palatal canine impaction is more common than labial impaction13 and is associated with abnormalities such as infraocclusion of the deciduous molars, enamel hypoplasia, aplasia of the second premolars, and underdeveloped upper lateral incisors14; if left untreated, the impacted canine can cause displacement or root resorption of adjacent teeth or the formation of cystic lesions.15 Several treatment options have been proposed, including observation, an interceptive approach, autotransplantation, extraction followed by movement of the premolar into the extraction space, and, for severe impactions, surgical intervention.10,16,17
Our patient presented with grade IV enamel hypoplasia on both lower first premolars, with an unknown etiology.18 To preserve the functional occlusion and improve the esthetic appearance, we chose to restore the teeth with prosthetic crowns.
Missing lower first permanent molars can be treated with either orthodontic space closure or prosthetic replacement. Fixed prostheses are relatively expensive and carry risks such as partial abrasion of fundamental tooth structures, mechanical errors during placement, and the potential for additional decay. Orthodontic space closure avoids surgical trauma and reduces the financial burden on the patient.19,20
After early loss of the lower first molars, the second molars often tip into the extraction spaces, increasing the risk of root resorption and bone dehiscence and causing adverse effects in both the vertical and sagittal planes.21 Uprighting of the second molars, which is essential to restoring optimal function and periodontal health, can be achieved with various orthodontic approaches, including cantilever springs, helical uprighting springs, nickel titanium coil springs, and traction from removable appliances.22 Among these options, helical springs are commonly used because they provide comprehensive control over uprighting and adequate extrusion while minimizing the need for patient cooperation.23 This method saves time, avoids the requirement for additional anchorage, and better mimics spontaneous eruption, since the force is applied in the direction of the normal eruption path.
In the case shown here, despite the complexity of the tooth movements required to treat a mutilated dentition, the use of a multidisciplinary approach, personalized to the patient’s specific needs, allowed us to achieve our treatment objectives without any notable adverse effects on the teeth or periodontium.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
- **Registered trademark of Ormco Corporation, Brea, CA; www.ormco.com.
REFERENCES
- 1. Stoica, S.N.; Nimigean, V.; Vîrlan, M.J.R.; and Nimigean, V.R.: The pathology of the first permanent molar during the mixed dentition stage: Review, Appl. Sci. 13:483, 2023.
- 2. Mavani, K.J.; Jain, M.J.; Pai, V.; and Naik, V.: Orthodontic treatment of a case with palatally impacted canine and missing molars: A case report, Cureus 14:24741, 2022.
- 3. Rezaie, M.; Ghapanchi, J.; Haghnegahdar, A.; Khojastehpour, L.; Khorshidi, H.; and Heidari, H.: A radiographic evaluation of missing of permanent first molars in a group of Iranian children and adults: A retrospective study, Int. J. Dent. 2018:5253965, 2018.
- 4. Hanlin, S.M.: The mutilated dentition: Management of the debilitated dentition, Ann R. Australas Coll. Dent. Surg. 21:49-50, 2012.
- 5. Ericson, S. and Kurol, J.: Radiographic examination of ectopically erupting maxillary canines, Am. J. Orthod. 91:483-492, 1987.
- 6. McSherry, P.: The assessment of and treatment options for the buried maxillary canine, Dent. Update 23: 7-10:1996.
- 7. Pitt, S.; Hamdan, A.; and Rock, P.: A treatment difficulty index for unerupted maxillary canines, Eur. J. Orthod. 28:141-144:2006.
- 8. Counihan, K.; Al-Awadhi, E.A.; and Butler, J.: Guidelines for the assessment of the impacted maxillary canine, Dent. Update 40:770-777, 2013.
- 9. Manne, R.; Gandikota, C.; Juvvadi, S.R.; Rama, H.R.M.; and Anche, S.: Impacted canines: Etiology, diagnosis, and orthodontic management, J. Pharm. Bioallied Sci. 4:S234-S238, 2012.
- 10. Kalra, V.: The K-9 spring for alignment of impacted canines, J. Clin. Orthod. 34:606-610, 2000.
- 11. Schroeder, M.A.; Schroeder, D.K.; Capelli Júnior, J.; and Santos, D.J.D.S.: Orthodontic traction of impacted maxillary canines using segmented arch mechanics, Dent. Press J. Orthod. 24:79-89, 2019.
- 12. Normando, D.: Third molars: To extract or not to extract, Dent. Press J. Orthod. 20:17-18, 2015.
- 13. Kumar, S.; Mehrotra, P.; Bhagchandani, J.; Singh, A.; Garg, A.; Kumar, S.; Sharma, A.; and Yadav, H.: Localization of impacted canines, J. Clin. Diag. Res. 9:11-14, 2015.
- 14. Baccetti, T.: A controlled study of associated dental anomalies, Angle Orthod. 68:267-74, 1998.
- 15. Guarnieri, R.; Cavallini, C.; Vernucci, R.; Vichi, M.; Leonardi, R.; and Barbato, E.: Impacted maxillary canines and root resorption of adjacent teeth: A retrospective observational study, Med. Oral Patol. Oral Cir. Bucal. 21:743-750, 2016.
- 16. Frank, C.A.: Treatment options for impacted teeth, J. Am. Dent. Assoc. 131:623-632, 2000.
- 17. Charles, A.; Duraiswamy, S.; Krishnaraj, R.; and Jacob, S.: Surgical and orthodontic management of impacted maxillary canines, SRM J. Res. Dent. Sci. 3:198-203, 2012.
- 18. Sandhu, M.; Gulia, S.; Nagpal, M.; and Sachdev, V.: Circular enamel hypoplasia: A rare enamel developmental disturbance in permanent teeth, J. Clin. Diag. Res. 8:ZD39-ZD40, 2014.
- 19. Al-Quran, F.A.; Al-Ghalayini, R.F.; and Al-Zu’bi, B.N.: Single-tooth replacement: Factors affecting different prosthetic treatment modalities, BMC Oral Health 11:34, 2011.
- 20. Raveli, T.B.; Shintcovsk, R.L.; Knop, L.A.H.; Sampaio, L.P., and Raveli, D.B.: Orthodontic replacement of lost permanent molar with neighbor molar: A six-year follow-up, Case Rep. Dent. 2017:4206435, 2017.
- 21. Raveli, T.B.; Raveli, D.B.; de Mathias Almeida, K.C.; and Pinto, A.D.S.: Molar uprighting: A considerable and safe decision to avoid prosthetic treatment, Open Dent. J. 11:466-475, 2017.
- 22. Magkavali-Trikka, P.; Emmanouilidis, G.; and Papadopoulos, M.A.: Mandibular molar uprighting using orthodontic miniscrew implants: A systematic review, Prog. Orthod. 19:1, 2018.
- 23. Shellhart, W.C. and Oesterle, L.J.: Uprighting molars without extrusion, J. Am. Dent. Assoc. 130:381-385, 1999.







COMMENTS
.