CASE REPORT
A Multidisciplinary Approach to Treatment of Multiple-Tooth Agenesis, Retention, and Impaction
The etiology of maxillary canine impaction has two main explanations.1-5 According to the genetic theory, the initial displacement of the tooth bud is entirely inherited. Guidance theory, on the other hand, suggests that any lateral-incisor anomaly (such as a missing or peg-shaped lateral incisor) could interfere with development of the adjacent canine, causing its displacement.1,6-8
Clinical diagnosis can be made by visual examination of an absent permanent canine, inability to palpate the canine‘s prominence, or retention of the deciduous canine. Radiographic diagnosis can be made by cone-beam computed tomography (CBCT) or panoramic, lateral cephalometric, occlusal, and periapical radiographs. In recent years, CBCT has become the gold standard for visualization of the canine’s three-dimensional position in planning orthodontic and surgical treatments.9,10
There are three traditional options for managing impacted maxillary canines: no treatment (with deciduous-canine extraction), interceptive treatment (space maintenance and palatal expansion), and orthodontic alignment after surgical exposure.11 Given that active orthodontic traction of an impacted maxillary canine takes an average 8.4 ± 3.26 months,12 however, extraction of the tooth should be considered as a fourth option, especially if the canine is causing root resorption of the adjacent teeth.
One of the most common developmental defects seen in dentistry is tooth agenesis, which affects the maxillary lateral incisors more than any other teeth except for the third molars.13 Even after more than 50 years of debate, the best orthodontic approach to treating patients with maxillary lateral-incisor agenesis is still at issue.14 Canine guidance is favored by those who support prosthetic restoration of the missing tooth as the best option for a long-lasting, healthy occlusion.15,16 Proponents of orthodontic space closure, on the other hand, contend that the periodontal conditions of these patients are superior to those of patients with fixed or removable prostheses.17-19
Similar articles from the archive:
- Space Closure with Single Miniscrews in Patients with Upper Lateral-Incisor Agenesis February 2023
- A Sliding Jig for Movement of a Central Incisor Across the Midline in a Class II Patient with Agenesis and Multiple Impactions October 2022
- CASE REPORT Treatment of Mandibular Canine Agenesis with Bone-Anchored Protraction of Posterior Teeth July 2020
The present report describes multidisciplinary treatment of a complex case involving multiple-tooth agenesis, retention, and impaction.
Diagnosis and Treatment Planning
A 16-year-old female presented to the orthodontic department at St. Joseph University of Beirut with the chief complaints of a rotated upper right canine, lower spacing, and a crooked smile that made her feel unconfident around her friends (Fig. 1A). Clinical examination showed a Class I molar relationship, an upper midline shifted 2mm to the left, and a lower midline shifted 2mm to the right. The patient had a straight lower profile with lower-lip protrusion. The upper left canine, lower right canine, and upper left lateral incisor were missing, and there was a retained lower right second premolar with its cusp tip pointing lingually (Fig. 1B).
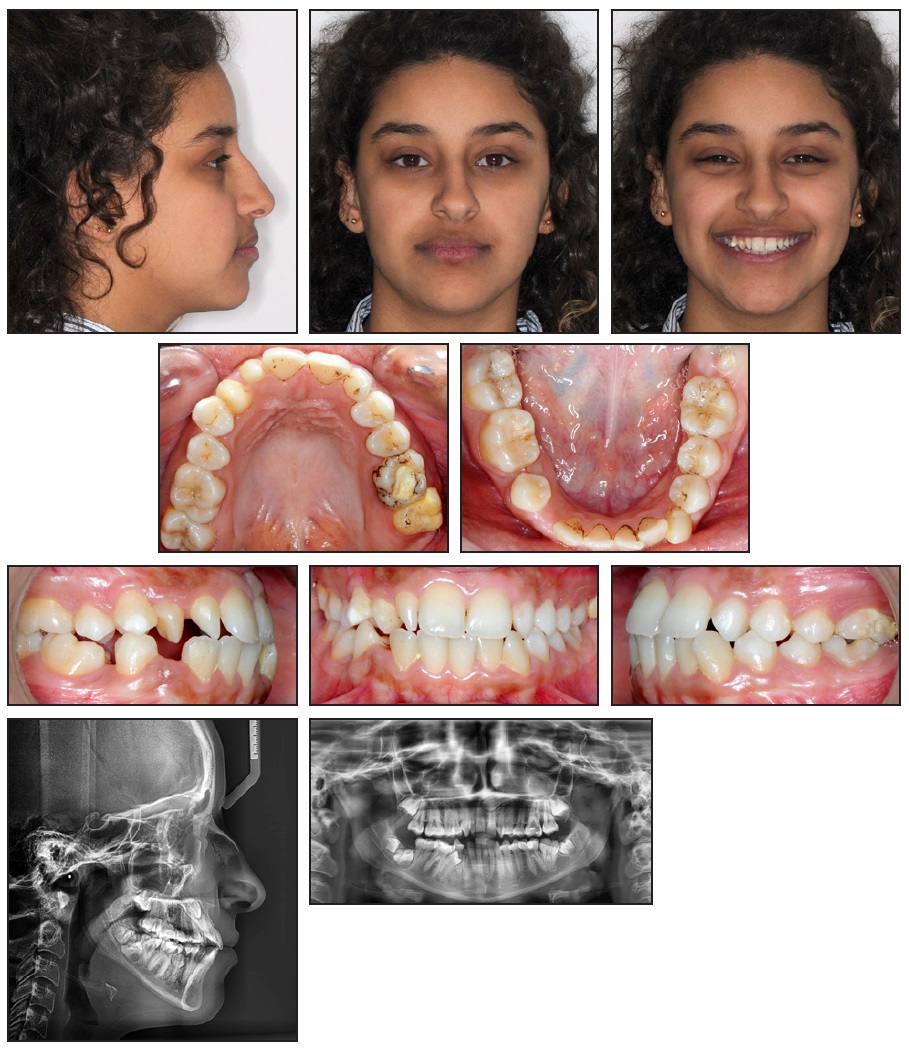
Fig. 1 16-year-old female patient with noncoincident midlines, agenesis of upper left lateral incisor and lower right canine, impacted upper left canine and lower right second premolar, retained lower right second premolar, and supernumerary lower right third molar with “kissing molar” syndrome before treatment (continued in next image).
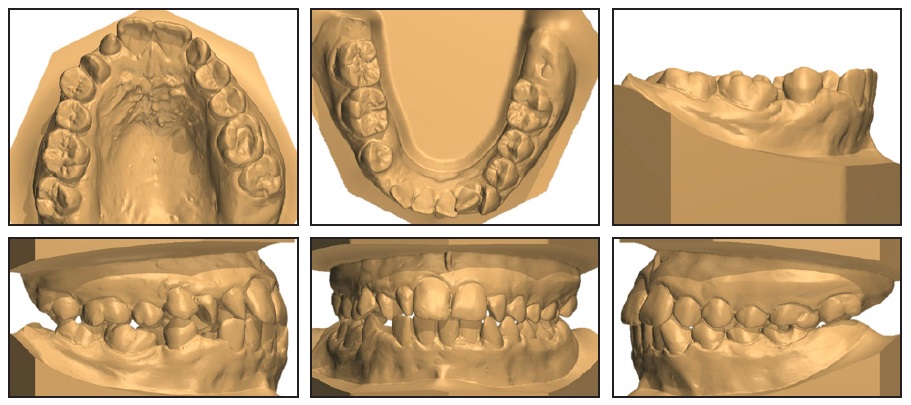
Fig. 1 (cont.) 16-year-old female patient with noncoincident midlines, agenesis of upper left lateral incisor and lower right canine, impacted upper left canine and lower right second premolar, retained lower right second premolar, and supernumerary lower right third molar with “kissing molar” syndrome before treatment.
The panoramic radiograph indicated agenesis of the upper left lateral incisor and lower right canine, as well as impaction of the upper left canine and lower right second premolar. The canine impaction was complicated, according to the classification of Ericsson and colleagues20: horizontally displaced, with the crown past the maxillary left central-incisor root. We also noticed a supernumerary lower right third molar with “kissing molar” syndrome. No TMD symptoms were detected.
Treatment objectives were to achieve Class I molar and canine relationships, a proper overjet and overbite, symmetrical and coordinated arches, improved facial esthetics (primarily the smile arc), coincident midlines, and normal masticatory and articulatory occlusal functions.
Three treatment options were presented. The first was to extract the upper left deciduous canine, the impacted upper left canine, and the upper left first molar (which evidenced deep caries) and to replace those teeth with two implants. The lower left canine and the root of the lower right deciduous canine would also be extracted. The second alternative was to extract the upper left deciduous canine and first molar and to attempt orthodontic eruption of the impacted canine. The third treatment option involved extraction of the peg-shaped upper right lateral incisor, impacted upper left canine, and upper left first molar, substitution of the upper left deciduous canine for the left lateral incisor and the upper right canine for the right lateral incisor, and mesialization of the upper left second and third molars into the extraction space of the first molar (Fig. 2). A mobility test of the upper left deciduous canine was positive, confirming that the tooth was not ankylosed. In the mandibular arch, extractions would include the left canine and third molar, the root of the right deciduous canine, and the right third molar and its supernumerary. The lower first premolars would then be substituted for the canines. This third treatment option was selected with informed consent by the patient and her mother.
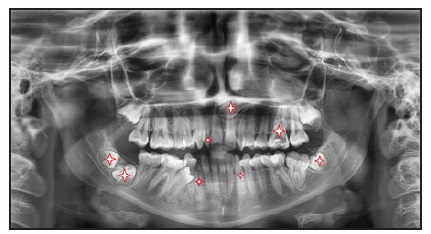
Fig. 2 Treatment plan involving extraction of peg-shaped upper right lateral incisor, impacted upper left canine, upper left first molar, lower left canine, lower left third molar, root of lower right deciduous canine, and lower right third molar with its supernumerary (starred teeth).
Treatment Progress
Periodontal cleaning and scaling were performed before orthodontic treatment began. Based on the orthodontic treatment plan, three stages of oral surgery were scheduled, with a two-week healing period between each. Stage 1 called for extraction of the impacted upper left canine through a palatal approach, along with the peg-shaped upper right lateral incisor. Stage 2 involved extraction of the upper left first molar and lower left canine and a germectomy of the lower left third-molar bud, with a minimal removal of gingival tissue blocking the second molar. Stage 3 was a germectomy of the kissing lower right third molars, followed by removal of the lower right deciduous-canine root.
Active orthodontic treatment was initiated during the second stage, using .022" × .028" MBT*-prescription RMO FLI** mini-twin brackets. Leveling and alignment were carried out over 24 weeks with a sequence of .014", .016", and .016" × .022" nickel titanium archwires.
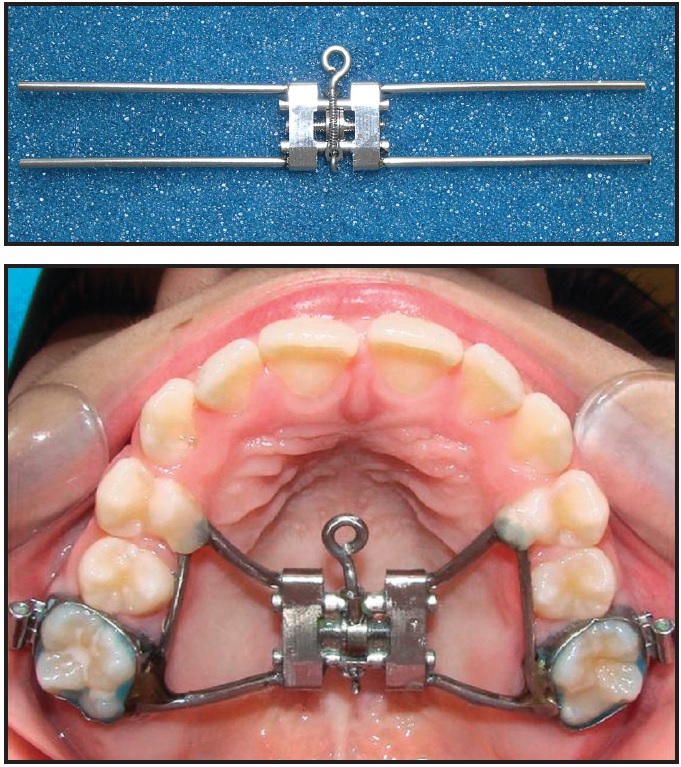
Active tooth movement was then initiated on .017" × .025" stainless steel archwires. The extraction spaces of the lower right deciduous canine and lower left canine were used to center the lower midline, and an RMO 302** open-coil spring was placed between the lower right first molar and first premolar to mesialize the first premolar and obtain enough space for traction of the impacted second premolar.
After 36 weeks of treatment, once the second premolar was in the arch and fully engaged in the stainless steel archwire, retraction of the mandibular incisors was started using sliding mechanics and differential anchorage. On the left side, maximum anchorage was gained by using 3⁄16", 6oz Impala* Class III elastics to center the lower midline and to help mesialize the upper left second and third molars without affecting the anterior teeth. Minimal anchorage was established on the right side by using Class II elastics. In the upper arch, the extraction space of the upper left first molar was used for mesialization of the second and third molars. Open-coil springs were attached mesial and distal to the upper left deciduous canine to provide .5mm of space on each side for cosmetic recontouring into the shape of a lateral incisor. The upper midline was corrected by using Class II elastics on the right side.
After another 12 months, the midline was centered and incisor retraction was initiated with sliding mechanics. In the final stage, .019" × .025" stainless steel archwires were placed to improve arch coordination and finishing, while triangular 3⁄16", 6oz Impala seating elastics were worn.
Immediately after debonding, both upper canines were prepared for composite adhesion by applying a chamfer diamond bur*** to their buccal surfaces. To avoid a bulky appearance of the new lateral incisors, the labial surfaces were flattened and the mesial and distal contours were narrowed using KUT† flame-shaped diamond burs. Composite facings were made with Ceram.x Spectra ST HV‡ universal composite in shade A2, and the anatomy was sculpted to mimic the natural anatomy of upper lateral incisors. Finishing and polishing were performed using contouring and polishing discs†† and polishing wheels.††
An upper wraparound retainer was delivered for the patient to wear full-time, except when eating, for six months. A lower 3-3 retainer made of Respond* dead-soft straight wire was bonded.
Treatment Results
Satisfactory facial esthetics and dental results were achieved in 30 months of treatment (Fig. 3A). The patient finished with Class I relationships, good intercuspal contacts, a positive overlap of the anterior teeth (overjet = 2mm, overbite = 2mm), acceptable dental alignment, harmonious arch widths, and symmetrical arches (Fig. 3B).
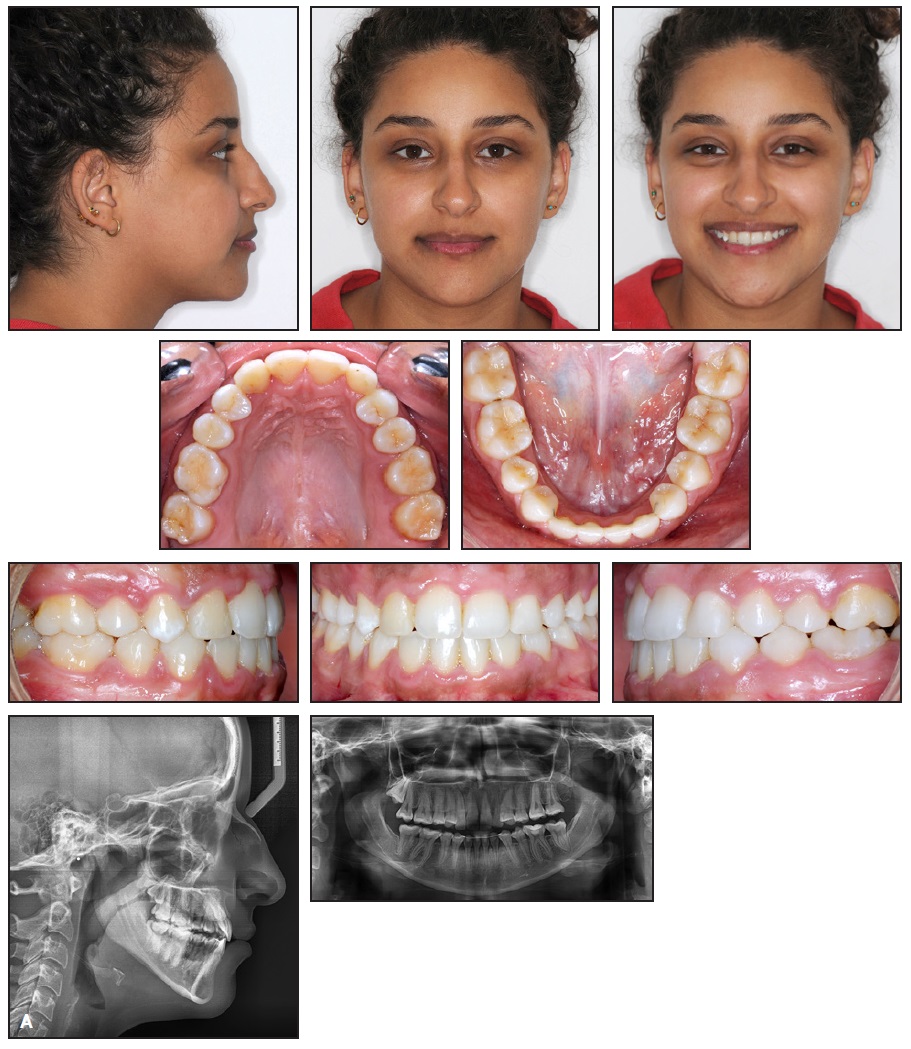
Fig. 3 A. Patient after 30 months of treatment (continued in next image).
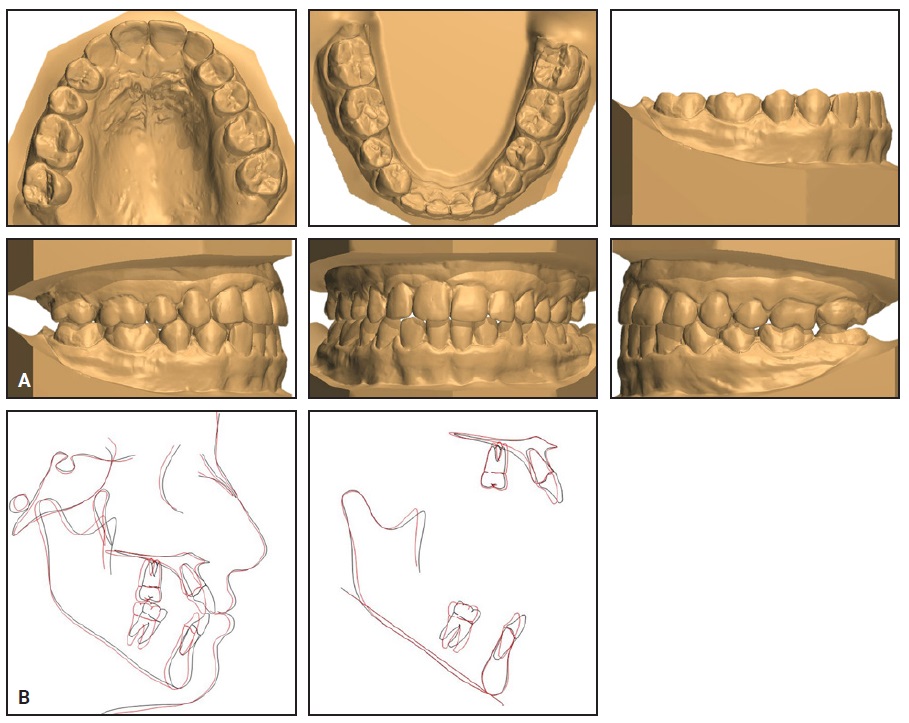
Fig. 3 (cont.) A. Patient after 30 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
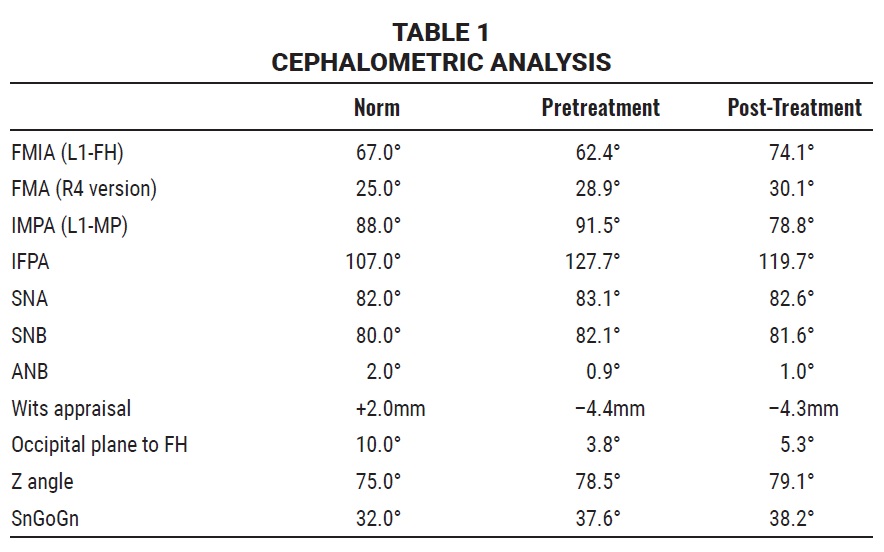
The panoramic radiograph confirmed good root parallelism, with all extraction sites closed and no signs of root resorption. The most significant cephalometric change (Table 1) involved palatal and lingual crown repositioning of the upper and lower incisors, respectively (IMPA –12.7°, IFPA –8°). The vertical dimension was controlled, with only a slight increase in SnGoGn. Socially, the patient displayed a more upbeat and outgoing attitude.
Discussion
In 2006, Pitt and colleagues developed a difficulty index to better assess the complexity of unerupted maxillary canines.21 Our patient’s upper left canine had a score of 20, which is considered high on that scale. The tooth also exhibited an inclination of more than 45°, overlapping the sagittal midline, with a high cusp tip and an apex positioned between the upper left second premolar and first molar. Several studies have found that if an impacted canine is angulated at more than 31° to the midline, the likelihood of successful eruption after extraction of the deciduous predecessor is reduced.20,22-24 Taken together, these factors indicated a difficult impaction.
Root resorption is the most frequent sequela of ectopic maxillary canines. Compared to buccally displaced canines, palatally displaced canines are more frequently responsible for root resorption of the maxillary anterior teeth.25 In a recent study using panoramic radiographs, the root apices of palatally impacted canines approximated the apices of the upper first premolars, whereas the apices of buccally impacted canines approximated the apices of the upper lateral incisors.26 In any case, physical proximity of 1mm or less must be regarded as a risk factor for root resorption. That issue pointed toward surgical extraction of our patient’s palatally impacted upper left canine.5
According to Arriola-Guillén and colleagues, the duration of active orthodontic traction of an impacted maxillary canine can range from four to 16 months, depending on the patient’s age, the horizontal and vertical position of the canine, and its angulation.12 This concern also led us to favor extraction of the tooth, considering the patient’s desire for the “shortest possible” orthodontic treatment.
Agenesis is a congenital dental anomaly that can lead to esthetic problems, displacement of adjacent teeth, and a shortage of alveolar bone, sometimes resulting in malocclusion.27 Dental anomalies such as agenesis, microformation, delayed development, palatal displacement of canines, hypo-occlusion of deciduous molars, and distoangulation of lower second premolars have been found to co-occur much more frequently than would be expected by chance alone28-31; Peck referred to these as “dental anomaly patterns.”32
Debates among orthodontists regarding the relative merits of space opening and space closure in treating patients with upper lateral-incisor agenesis have been ongoing for decades.33,34 A recent systematic review concluded that tooth-supported dental prostheses perform worse than orthodontic space closure in terms of periodontal indices, and that tooth- or implant-supported dental prostheses are considered less attractive by laypeople, patients, and dentists.14 A prospective study by Amm and colleagues demonstrated that space closure can produce satisfactory results in patients with both Class I and Class III skeletal patterns.35
Since our patient had a limited budget, and given the problems associated with implant-supported prostheses in the long term, we decided to take advantage of the retained upper left deciduous canine (which had a long root) and substitute it for a lateral incisor. Studies have found that if the clinician effectively manages the canine’s lingual root torque during space closure and correctly performs the subsequent enameloplasty (recontouring), the esthetic result will look more natural than a prosthetic replacement.16,34 Gingival recontouring to reduce the difference between the upper central and lateral incisors might have given our patient even better smile esthetics, according to the checklist of Magne and colleagues.36 Nevertheless, we believe our multidisciplinary therapy matched the patient’s demands and needs in this case.
FOOTNOTES
- *Registered trademark of Ormco Corporation, Brea, CA; www.ormco.com.
- **Registered trademark of RMO, Franklin, IN; www.rmortho.com.
- ***Brasseler USA, Savannah, GA; www.brasselerusa.com.
- †iM3 Pty Ltd, Sydney, Australia; www.im3vet.com.au.
- ‡Registered trademark of Dentsply Sirona, York, PA; www.dentsplysirona.com.
- ††3M Sof-Lex Discs, trademark of 3M, Monrovia, CA; www.3M.com.
REFERENCES
- 1. Becker, A. and Chaushu, S.: Etiology of maxillary canine impaction: A review, Am. J. Orthod. 148:557-567, 2015.
- 2. Schindel, R.H. and Duffy, S.L.: Maxillary transverse discrepancies and potentially impacted maxillary canines in mixed-dentition patients, Angle Orthod. 77:430-435, 2007.
- 3. Faber, J.; Berto, P.M.; and Quaresma, M.: Rapid prototyping as a tool for diagnosis and treatment planning for maxillary canine impaction, Am. J. Orthod. 129:583-589, 2006.
- 4. Bishara, S.E.: Clinical management of impacted maxillary canines, Semin. Orthod. 4:87-98, 1998.
- 5. Crincoli, V.; Tettamanti, L.; Lucchina, A.G.; Dedola, A.; Cazzolla, A.P.; Lacaita, M.G.; and Mastrangelo, F.: Correlation between maxillary canine impaction and facial biotype, J. Craniofac. Surg. 30:1044-1048, 2019.
- 6. Alqerban, A.; Storms, A.S.; Voet, M.; Fieuws, S.; and Willems, G.: Early prediction of maxillary canine impaction, Dentomaxillofac. Radiol. 45:20150232, 2016.
- 7. Bishara, S.E.; Kommer, D.D.; McNeil, M.H.; Montagano, L.N.; Oesterle, L.J.; and Youngquist, H.W.: Management of impacted canines, Am. J. Orthod. 69:371-387, 1976.
- 8. Manne, R.; Gandikota, C.; Juvvadi, S.R.; Rama, H.R.; and Anche, S.: Impacted canines: Etiology, diagnosis, and orthodontic management, J. Pharm. Bioallied Sci. 4:234-238, 2012.
- 9. Bedoya, M.M. and Park, J.H.: A review of the diagnosis and management of impacted maxillary canines, J. Am. Dent. Assoc. 140:1485-1493, 2009.
- 10. De Grauwe, A.; Ayaz, I.; Shujaat, S.; Dimitrov, S.; Gbadegbegnon, L.; Vande Vannet, B.; and Jacobs, R.: CBCT in orthodontics: A systematic review on justification of CBCT in a paediatric population prior to orthodontic treatment, Eur. J. Orthod. 41:381-389, 2019.
- 11. Counihan, K.; Al-Awadhi, E.A.; and Butler, J.: Guidelines for the assessment of the impacted maxillary canine, Dent. Update 40:770-777, 2013.
- 12. Arriola-Guillén, L.E.; Aliaga-Del Castillo, A.; Ruíz-Mora, G.A.; Rodríguez-Cárdenas, Y.A.; and Dias-da Silveira, H.L.: Influence of maxillary canine impaction characteristics and factors associated with orthodontic treatment on the duration of active orthodontic traction, Am. J. Orthod. 156:391-400, 2019.
- 13. Polder, B.J.; Van’t Hof, M.A.; Van der Linden, F.P.; and KuijpersJagtman, A.M.: A meta-analysis of the prevalence of dental agenesis of permanent teeth, Comm. Dent. Oral Epidemiol. 32:217-226, 2004.
- 14. Silveira, G.S.; de Almeida, N.V.; Pereira, D.M.; Mattos, C.T.; and Mucha, J.N.: Prosthetic replacement vs space closure for maxillary lateral incisor agenesis: A systematic review, Am. J. Orthod. 150:228-237, 2016.
- 15. Roth, R.H.: The maintenance system and occlusal dynamics, Dent. Clin. N. Am. 20:761-788, 1976.
- 16. D’Amica, A.: Canine teeth: Normal functional relation of the natural teeth of man, J. S. Calif. Dent. Assoc. 26:239-241, 1958.
- 17. Rosa, M. and Zachrisson, B.U.: Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors, J. Clin. Orthod. 35:221-234, 2001.
- 18. Nordquist, G.G. and McNeill, R.W.: Orthodontic vs. restorative treatment of the congenitally absent lateral incisor: Long term periodontal and occlusal evaluation, J. Periodontol. 46:139-143, 1975.
- 19. Robertsson, S. and Mohlin, B.: The congenitally missing upper lateral incisor: A retrospective study of orthodontic space closure versus restorative treatment, Eur. J. Orthod. 22:697-710, 2000.
- 20. Ericson, S. and Kurol, J.: Early treatment of palatally erupting maxillary canines by extraction of the primary canines, Eur. J. Orthod. 10:283-295, 1988.
- 21. Pitt, S.; Hamdan, A.; and Rock, P.: A treatment difficulty index for unerupted maxillary canines, Eur. J. Orthod. 28:141-144, 2006.
- 22. Jacoby, H.: The etiology of maxillary canine impactions, Am. J. Orthod. 84:125-132, 1983.
- 23. Stellzig, A.; Basdra, E.K.; and Komposch, G.: The etiology of canine tooth impaction: A space analysis [in German], Fortschr. Kieferorthop. 55:97-103, 1994.
- 24. Mercuri, E.; Cassetta, M.; Cavallini, C.; Vicari, D.; Leonardi, R.; and Barbato, E.: Dental anomalies and clinical features in patients with maxillary canine impaction, Angle Orthod. 83:22-28, 2013.
- 25. Rafflenbeul, F.; Gros, C.I.; Lefebvre, F.; Bahi-Gross, S.; Maizeray, R.; and Bolender, Y.: Prevalence and risk factors of root resorption of adjacent teeth in maxillary canine impaction, among untreated children and adolescents, Eur. J. Orthod. 41:447-453, 2019.
- 26. Kim, S.H.; Son, W.S.; Yamaguchi, T.; Maki, K.; Kim, S.S.; Park, S.B.; and Kim, Y.I.: Assessment of the root apex position of impacted maxillary canines on panoramic films, Am. J. Orthod. 152:489-493, 2017.
- 27. Choi, S.J.; Lee, J.W.; and Song, J.H.: Dental anomaly patterns associated with tooth agenesis, Acta Odontol. Scand. 75:161-165, 2017.
- 28. Baccetti, T.: A controlled study of associated dental anomalies, Angle Orthod. 68:267-274, 1998.
- 29. Langberg, B.J. and Peck, S.: Tooth-size reduction associated with occurrence of palatal displacement of canines, Angle Orthod. 70:126-128, 2000.
- 30. Peck, S.; Peck, L.; and Kataja, M.: Prevalence of tooth agenesis and peg-shaped maxillary lateral incisor associated with palatally isplaced canine (PDC) anomaly, Am. J. Orthod. 110:441-443, 1996.
- 31. Peck, S.; Peck, L.; and Kataja, M.: Concomitant occurrence of canine malposition and tooth agenesis: Evidence of orofacial genetic fields, Am. J. Orthod. 122:657-660, 2002.
- 32. Peck, S.: Dental anomaly patterns (DAP): A new way to look at malocclusion, Angle Orthod. 79:1015-1016, 2009.
- 33. Kokich, V.G. and Spear, F.M.: Guidelines for managing the orthodontic-restorative patient, Semin. Orthod. 3:3-20, 1997.
- 34. Zachrisson, B.U.; Rosa, M.; and Toreskog, S.: Congenitally missing maxillary lateral incisors: Canine substitution, Am. J. Orthod. 139:440, 2011.
- 35. Amm, E.W.; Antoszewska-Smith, J.; and Boley, J.: Canine substitution of congenitally missing maxillary lateral incisors in Class I and Class III malocclusions by using skeletal anchorage, Am. J. Orthod. 156:512-521, 2019.
- 36. Magne, P.; Salem, P.; and Magne, M.: Influence of symmetry and balance on visual perception of a white female smile, J. Prosth. Dent. 120:573-582, 2018.










COMMENTS
.