Treatment of Skeletal Class III Malocclusion in Adolescents Using Miniscrew-Supported Orthopedic and Fixed Orthodontic Appliances
Skeletal Class III malocclusion is characterized by maxillary retrusion, mandibular protrusion, or a combination of the two.1,2 This type of malocclusion is among the most challenging for orthodontists to treat, since unfavorable growth will compromise any clinical improvements in 20-25% of patients.3 Factors affecting the success of treatment include the patient’s age and sex, a family history of Class III malocclusion, and the severity of the sagittal discrepancy.
Early intervention is advised, particularly in cases of maxillary retrusion, since this malocclusion is associated with reduced self-esteem and avoidance of social interaction.4 The greatest biological response to maxillary protraction is seen at ages 4-7.5,6 A short term of treatment can improve facial esthetics and thus have a positive effect on psychological well-being during childhood.7 Some evidence indicates that early treatment may reduce the amount of of surgical correction required, with more stable and predictable results.8,9
Traditionally, early treatment involves a combination of an RPE and a facemask.5 This strategy produces the skeletal effects of forward dislocation and counterclockwise rotation of the maxilla, along with backward movement and clockwise rotation of the mandible.2,10 Dentoalveolar side effects such as extrusion and mesialization of the maxillary molars, proclination of the maxillary incisors, and retroclination of the mandibular incisors must be avoided to maximize the orthopedic effects.10-12
In the past decade, several skeletal-anchorage strategies have been proposed to improve the efficiency of maxillary protraction.7,13,14 De Clerck and colleagues introduced a bone-anchored method in which Class III elastics are attached to miniplates in the maxillary infrazygomatic region and the anterior portion of the mandible.7 Although effective, their protocol entails surgical procedures of mild to moderate complexity, usually under general sedation, to position and remove the miniplates.
To address those limitations, de Souza and colleagues developed a modified bone-anchored maxillary protraction protocol using Class III elastics attached to orthodontic miniscrews, rather than miniplates, in both jaws.15 They cautioned, however, that the technique should not be used in patients requiring skeletal maxillary expansion.
In cases involving both maxillary constriction and retrusion, an h-RPE has been proposed in conjunction with alternating rapid maxillary expansion and constriction (Alt-RAMEC) and facemask therapy.13,14,16 This protocol is known as skeletal Alt-RAMEC for Class III malocclusion (SKAR III). The Alt-RAMEC technique weakens skeletal resistance, facilitating maxillary protraction in early or late adolescence.2,10,17-21 While the skeletal expansion effectively disarticulates the circummaxillary sutures,6,21,22 any sagittal correction obtained at a prepubertal stage is largely canceled out by residual growth, indicating that a conventional RPE-facemask approach would be just as effective at this age.8 The SKAR III protocol should therefore be reserved for late-adolescent patients with advanced skeletal maturity and little remaining growth. The h-RPE has the further advantages of limiting stress on the anchor teeth and minimizing the dentoalveolar effects of facemask therapy, especially in late adolescence.16,23
Similar articles from the archive:
- Skeletal Anchorage for Strategic Treatment of Hyperdivergent Class III Malocclusion in Adult Patients September 2023
- Nonsurgical Camouflage Treatment of Skeletal Class III Malocclusion Using the Biocreative Reverse-Curve Technique July 2022
- Tandem Skeletal Expander and MAPA Protocol for Palatal Expansion in Adults November 2020
The use of a three-dimensionally printed surgical guide, according to the MAPA protocol, can ensure adequate depth and angulation of the anchoring miniscrews by matching cone-beam computed tomography (CBCT) scans of the maxilla to the digital model.24,25
This article describes the treatment of a 14-year-old female patient with skeletal Class III malocclusion, open bite, and secondary atypical swallowing. Forward displacement of the maxilla was achieved in an orthopedic phase using an h-RPE and protraction facemask, followed by clockwise rotation of the mandible with subsequent extrusion of the anterior teeth in an orthodontic phase of fixed appliances and Class III elastics.
Case Report
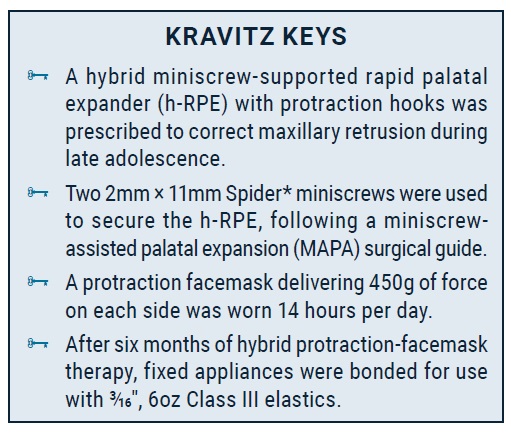
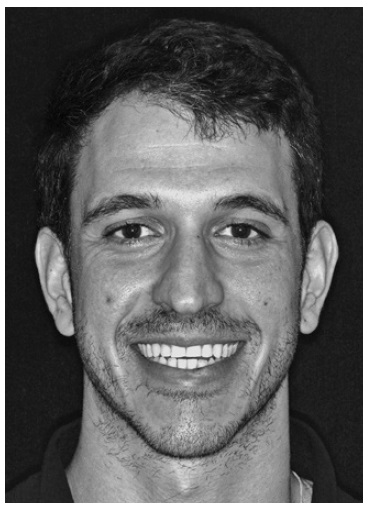
A 14-year-old female presented with the chief complaint of an unpleasant smile with crooked anterior teeth (Fig. 1). The patient exhibited a triangular face with a mildly excessive lower third and a slight deviation of the nose to the right. The facial profile was straight, and the nasolabial angle was slightly open. Incisor exposure in smiling was acceptable, but there were wide lateral black corridors. The maxillary dental midline was deviated 1mm to the right with respect to the mandibular dental midline, but the latter was coincident with the facial midline in smiling. The patient showed a slight bilateral Class III molar relationship (–1.5mm) and a bilateral Class I canine relationship, with a lateral open bite on both sides. The overbite was reduced (.4mm), but the overjet was normal (1mm). Transversely, the patient had a maxillary deficiency, with a V-shaped upper arch and a unilateral crossbite between the upper right first and second premolars. The upper incisors were tipped toward the upper right canine, which was ectopic and high in the vestibule, contributing to a cant of the maxillary occlusal plane. The upper arch was severely crowded, but the lower arch was only mildly crowded, with excessive curves of Spee and Wilson.
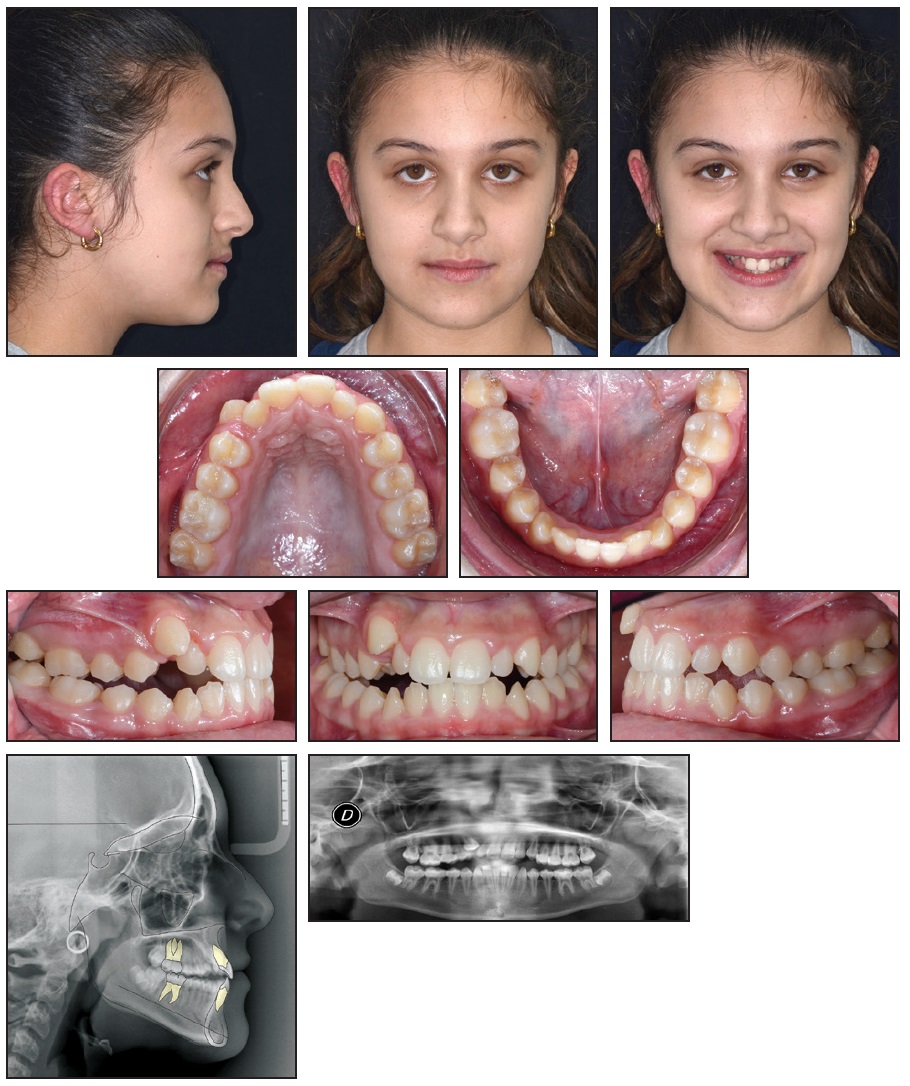
Fig. 1 14-year-old female patient with skeletal Class III malocclusion, lateral open bite, ectopic upper right canine, canted maxillary plane, severe crowding in upper arch, and secondary atypical swallowing before treatment.
Functional tests found secondary atypical swallowing, with tongue interposition between the arches and constriction of the perioral mimic muscles, especially the orbicular muscle.
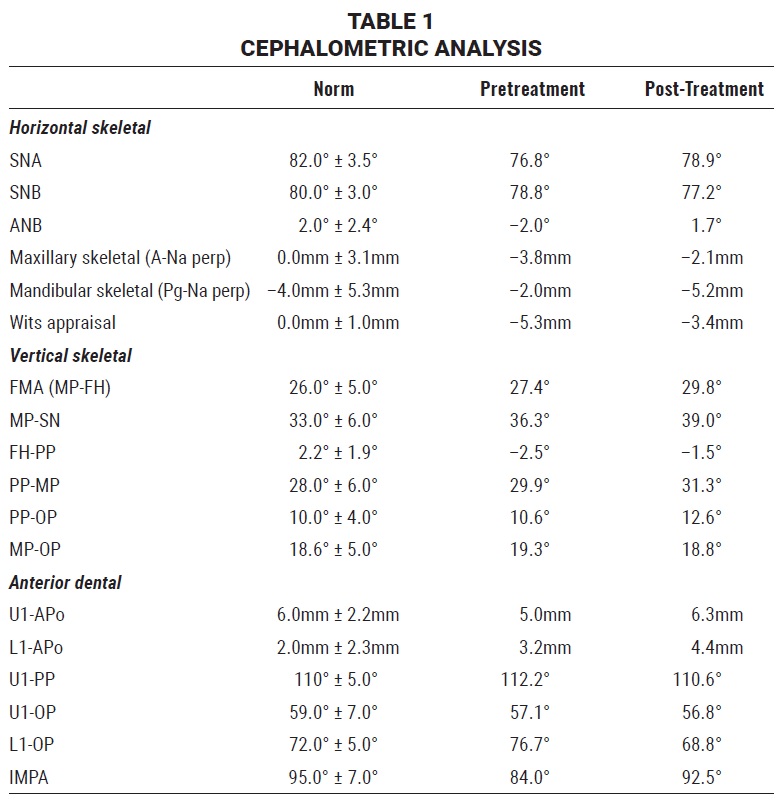
A panoramic radiograph revealed the presence of all teeth except for the upper third molars, with no signs of apical resorption or interdental bone defects. Cephalometric analysis (Table 1) indicated a skeletal Class III relationship (ANB = –2°, Wits appraisal = –5.3mm), with the maxilla in a retrusive position (SNA = 76.8°, A-Na perp = –3.8mm). The facial pattern was normodivergent (FMA = 27.4°), although a general tendency toward a hyperdivergent pattern could be seen (MP-SN = 36.3°). The upper incisors were normally inclined, with a slight tendency toward proclination (U1-PP = 112.2°), while the lower incisors were retroclined (IMPA = 84°).
The primary objective was an orthopedic correction of the transverse and anteroposterior maxillary deficiencies to produce a good intermaxillary relationship. Other goals were to obtain Class I molar and canine relationships; normalize the overbite; and achieve leveling, alignment, and coordination of the arches after erupting the ectopic upper right canine. A further objective was to increase the incisor display in smiling. From a functional standpoint, the atypical swallowing needed to be resolved.
The parents noted that the patient had reached menarche two and one-half years earlier. Given the patient̓'s skeletal maturity and moderate degree of sagittal discrepancy, several treatment options were presented. One was to delay surgical-orthodontic therapy until the end of growth to increase the likelihood of a successful facial and occlusal outcome. A similar option was to begin treatment with only maxillary expansion, postponing any surgery until the end of growth with the expectation that the procedure would be less invasive and complex. When the parents rejected any kind of orthognathic surgery, various orthodontic-only treatment plans were considered. One possibility involved a Class III extraction pattern (lower first premolars and upper second premolars), followed by fixed appliance treatment with Class III elastics. This would allow recovery of the ectopic upper right canine and correction of the sagittal deficiency, but would produce minimal changes in the facial profile. The parents expressed a preference for an even less invasive procedure that would improve the profile. Therefore, we proposed an initial miniscrew-supported orthopedic phase, using an h-RPE and a facemask, followed by a phase of orthodontic correction with fixed appliances. This option was accepted by the patient and her parents.
Digital intraoral scans were stored in STL format. When the lateral cephalogram was taken, a thermoplastic glycol-modified polyethylene terephthalate maxillary appliance with radiopaque markers positioned along the palatine raphe was used to identify the palatal mucosa and maxillary bone (Fig. 2A). According to Kim and colleagues, the accuracy of a lateral headfilm is comparable to that of a CBCT scan in determining the palatal thickness within 5mm of the median sagittal plane.26 After accurate matching of the lateral cephalogram with the digital models, the ideal direction of insertion, position, and length of two palatal miniscrews were determined (Fig. 2B).
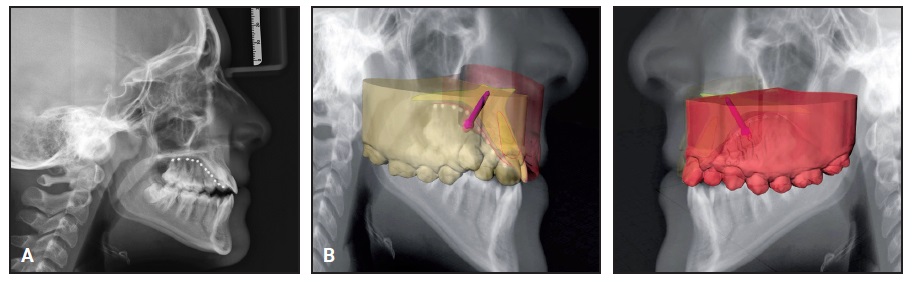
Fig. 2 A. Fit of thermoplastic appliance. B. Accurate matching of lateral cephalogram with digital models for planning of miniscrew insertion.
A MAPA surgical guide was digitally designed and 3D-printed to aid in the insertion of 2mm × 11mm Spider Screw K2 Konic miniscrews (Fig. 3).24,25
Next, an h-RPE was fabricated, with buccal arms welded to the first-molar bands for attachment of the facemask (Fig. 4). The anterior palatal arms of the RPE were welded to two metal abutments designed to fit over the miniscrew heads, each affixed with a microscrew. After bonding, the h-RPE was activated until the transverse deficiency was corrected (32 days at one quarter-turn per day).
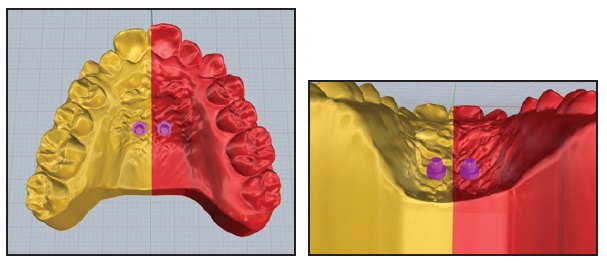
Fig. 3 Miniscrew placement in palatal vault on three-dimensional digital model.
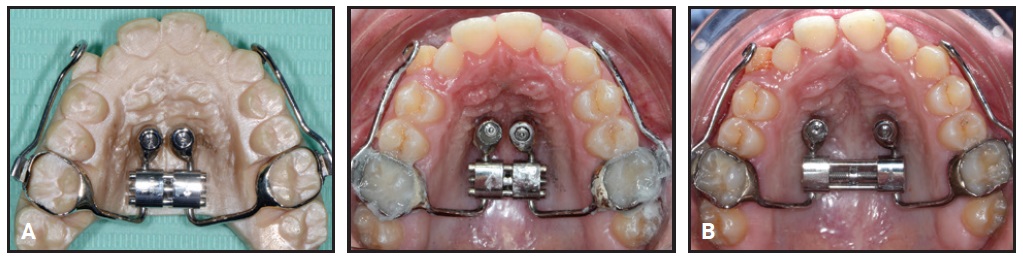
Fig. 4 A. Hybrid rapid palatal expander (h-RPE) with anterior palatal arms welded to metal abutments over miniscrew heads. B. Skeletal maxillary expansion after 32 days (one quarter-turn per day).
The patient was instructed to wear a protraction facemask 14 hours per day (Fig. 5). A 450g orthopedic force was applied on each side in a downward and forward direction, at an inclination of about 30° to the occlusal plane, until the sagittal dimension had been slightly overcorrected.
After six months of orthopedic treatment, the buccal and posterior arms of the h-RPE were removed, and the facemask was discontinued (Fig. 6).
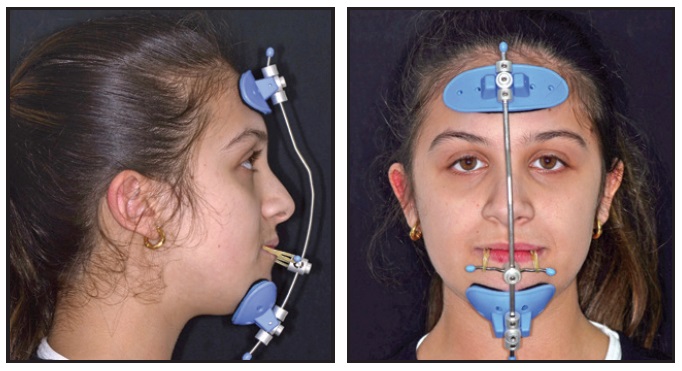
Fig. 5 Protraction facemask with 450g of orthopedic force applied on each side in downward and forward direction, at about 30° to occlusal plane.
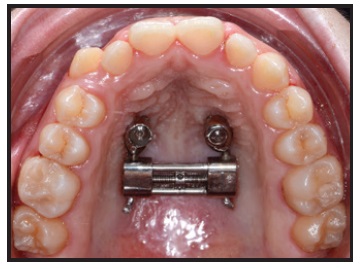
Fig. 6 Buccal and posterior arms of h-RPE removed after six months of orthopedic treatment.
Primo** .022" labial brackets were bonded indirectly, and .014" nickel titanium archwires were inserted in both arches (Fig. 7). An open-coil spring was placed between the upper right lateral incisor and first premolar to provide space for eruption of the ectopic canine and to help center the upper dental midline.

Fig. 7 Primo** .022" labial brackets bonded and .014" nickel titanium archwires inserted in both arches; open-coil spring placed between upper right lateral incisor and first premolar to provide space for canine eruption and to center upper dental midline.
Two months later, when enough space had been created for the upper right canine, its eruption was initiated by tying an elastic module to its mesial bracket wings and to the archwire27 (Fig. 8).
After four months of canine alignment, an .019" × .025" nickel titanium archwire was inserted in the upper arch to continue leveling (Fig. 9). An .019" × .025" stainless steel archwire was inserted in the lower arch, with elastomeric chain added to close existing spaces and to prevent unwanted spaces from opening between the lower canines and lateral incisors. For sagittal and anterior vertical correction, the patient was asked to wear ³⁄16", 6oz Class III elastics*** 22 hours per day in a triangular configuration from hooks on the upper and lower canines to hooks on the upper first molars.
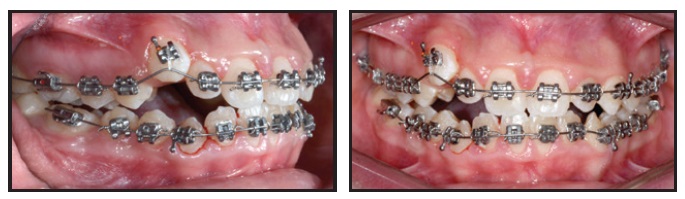
Fig. 8 Two months later, with sufficient space gained for upper right canine, eruption initiated with elastic module tied to mesial bracket wings and archwire.
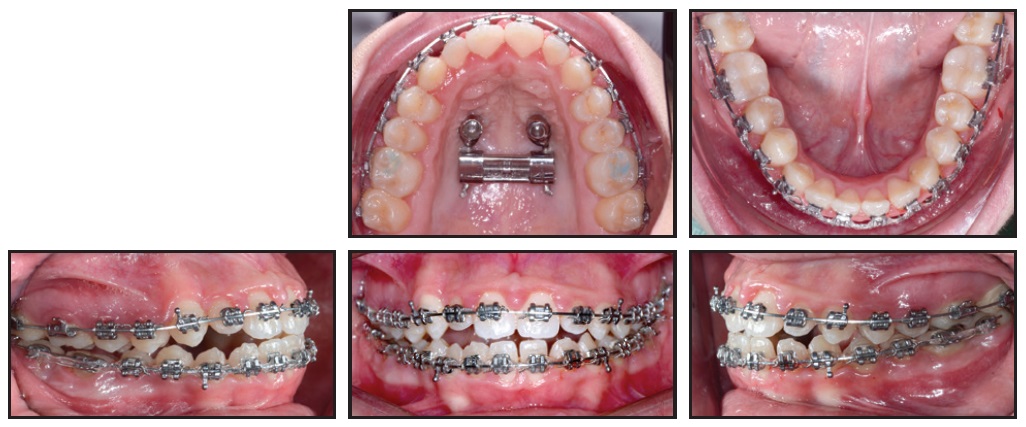
Fig. 9 After four months of canine alignment, upper .019" × .025" nickel titanium and lower .019" × .025" stainless steel archwires inserted, with elastomeric chain added in lower arch for space closure.
Two months later, the brackets on the upper right central incisor and lower right first premolar were repositioned for finishing and detailing, and Class III elastics were applied asymmetrically to center the upper and lower dental midlines (Fig. 10).
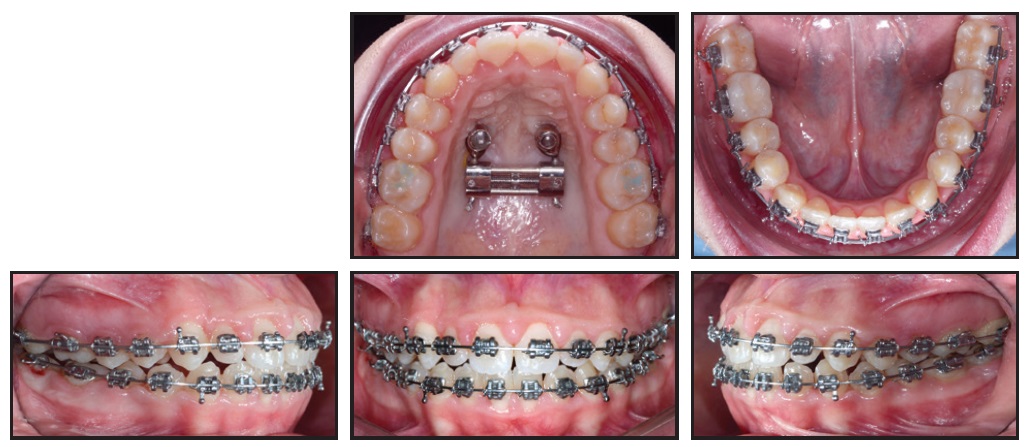
Fig. 10 Two months later, brackets repositioned on upper right central incisor and lower right first premolar for finishing and detailing.
Total treatment time was 22 months (Fig. 11). The patient’s facial profile was more convex and esthetically pleasant. The dental midlines appeared centered in smiling, the black corridors were significantly reduced, and the smile arc was consonant. The incisor display was improved, although a slight asymmetry in gingival exposure could be observed in smiling. Bilateral Class I canine and molar relationships were obtained and the open bite was corrected, with ideal overbite and optimal alignment in both arches. A slightly uneven gingival margin at the upper right canine was attributable both to the initial cant of the maxillary occlusal plane and to a need for further bracket repositioning or wirebending in the finishing phase.
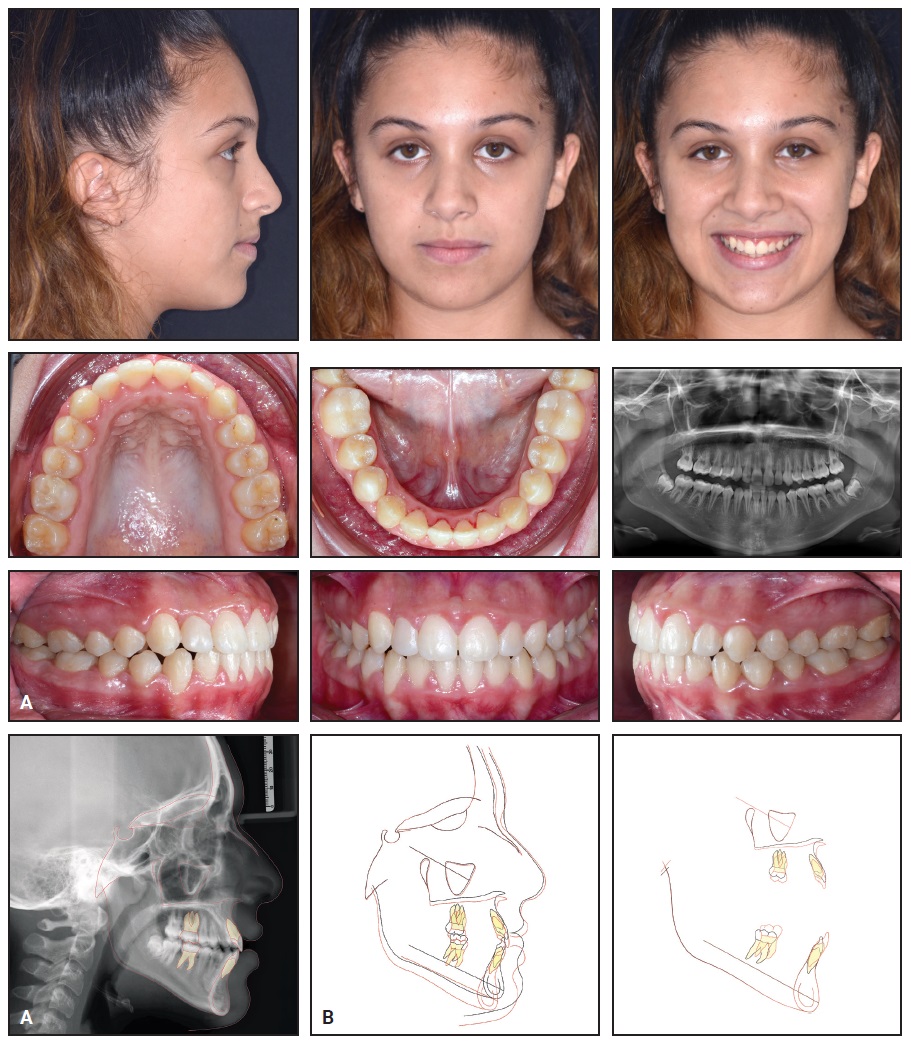
Fig. 11 A. Patient after 22 months of treatment. B. Superimposition of pretreatment (black) and post-treatment (red) cephalometric tracings.
The final panoramic radiograph showed good root parallelism and proper leveling of the interdental bone peaks, with no signs of root resorption. Cephalometric analysis (Table 1) confirmed an improvement in the skeletal sagittal discrepancy (ANB = 1.7°, Wits appraisal = –3.4mm), with an increased SNA angle (78.9°) and normalized lower-incisor inclination (IMPA = 92.5°). The vertical dimension was slightly increased (FMA = 29.8°, MP-SN = 39°), owing to clockwise rotation of the mandible. Regional superimpositions showed extrusion of the upper and lower molars and incisors, but the upper-molar extrusion was more limited than the upper-incisor extrusion, indicating that a clockwise rotation of the maxillary plane had compensated for the clockwise rotation of the mandible.
After debonding, vacuformed maxillary and mandibular retainers were delivered for six months of full-time wear, followed by nighttime-only wear. To further improve vertical stability and tongue function, the patient was referred for speech therapy.
Discussion
Maxillary hypoplasia is characterized not only by a retrusive maxilla in the sagittal plane, but also by skeletal deficiency in the transverse plane. Therefore, maxillary transverse deficiency is a common finding in patients with skeletal Class III malocclusions.28
Treatment planning will depend on both the patient’s age and the severity of the malocclusion.29,30 Although skeletal maturity will limit the potential to resolve a skeletal Class III relationship orthodontically,5,6 an optimal solution often requires waiting until the end of skeletal growth to perform orthognathic surgery.30
In situations where late-adolescent patients and their parents reject surgery and request a more immediate improvement in facial appearance, skeletal anchorage has become a useful alternative to the conventional RPE-facemask protocol, enabling forward displacement of the maxilla despite advanced skeletal maturity.31 Facemask therapy causes clockwise rotation of the mandible and thus retracts the skeletal pogonion, making the facial profile more esthetically convex and improving the occlusal relationships.32 This approach should therefore be considered for patients with mild to moderate skeletal Class III malocclusions and meso- or hypodivergent facial patterns.33
In girls, the adolescent spurt in mandibular growth begins between ages 10 and 12, while in boys it begins between ages 12 and 15.34 The growth spurt lasts longer in males, usually continuing until after age 18, and the amount of mandibular growth is also greater in males than in females.34,35 Hence, adolescent females generally have a better prognosis than males in Class III treatment.
In our 14-year-old female patient, we decided to use an h-RPE with only a single phase of expansion (32 days) and concurrent facemask protraction. Stable skeletal anchorage, ensured by accurate miniscrew-insertion planning, allowed us to limit dentoalveolar effects such as mesialization of the upper first molars while maximizing the skeletal effect. Without the use of an Alt-RAMEC protocol to enhance the responsiveness of the maxilla, the orthopedic phase produced forward and downward maxillary displacement (SNA +2.1°, A-Na perp +1.7mm). Subsequent advancement of point A and retraction of pogonion (Pg-Na perp –3.2mm) were attributable primarily to clockwise rotation of the mandible (FMA +2.4°). This facemask-induced rotation could be identified as mandibular backward rotation type 2, as described by Björk, considering that a slight backward and upward growth of the condyles was observed.36 The increased vertical dimension and reduced chin projection improved the patient’s Class III facial profile. An orthodontic phase of fixed appliances and Class III elastics compensated for the mandibular rotation by extruding the anterior teeth, thus preventing the development of anterior open bite.
ACKNOWLEDGMENT: Special thanks to Prof. Giuliano Maino and Mr. Emanuele Paoletto, inventors of the MAPA protocol, and to Mr. Paoletto for planning digital insertion of the palatal miniscrews.
FOOTNOTES
- *Trademark of HDC Italy, Thiene, Italy; www.hdc-italy.com.
- **Registered trademark of Sweden & Martina, Due Carrare, Padova, Italy; www.sweden-martina.com.
- ***Impala, trademark of Ormco Corporation, Brea, CA; www.ormco.com.
REFERENCES
- 1. Ellis, E. III and McNamara, J.A. Jr.: Components of adult Class III malocclusion, J. Oral Maxillofac. Surg. 42:295-305, 1984.
- 2. Foersch, M.; Jacobs, C.; Wriedt, S.; Hechtner, M.; and Wehrbein, M.: Effectiveness of maxillary protraction using facemask with or without maxillary expansion: A systematic review and meta-analysis, Clin. Oral Invest. 19:1181-1192, 2015.
- 3. Masucci, C.; Franchi, L.; Defraia, E.; Mucedero, M.; Cozza, P.; and Baccetti, T.: Stability of rapid maxillary expansion and facemask therapy: A long-term controlled study, Am. J. Orthod. 140:493-500, 2011.
- 4. Bernabé, E.; Sheiham, A.; and de Oliveira, C.M.: Condition-specific impacts on quality of life attributed to malocclusion by adolescents with normal occlusion and Class I, II and III malocclusion, Angle Orthod. 78:977-982, 2008.
- 5. Baccetti, T.; McGill, J.S.; Franchi, L.; McNamara, J.A. Jr.; and Tollaro, I.: Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy, Am. J. Orthod. 113:333-343, 1998.
- 6. Melsen, B. and Melsen, F.: The postnatal development of the palatomaxillary region studied on human autopsy material, Am. J. Orthod. 82:329-342, 1982.
- 7. De Clerck, H.J.; Cornelis, M.A.; Cevidanes, L.H.; Heymann, G.C.; and Tulloch, C.J.: Orthopedic traction of the maxilla with miniplates: A new perspective for treatment of midface deficiency, J. Oral Maxillofac. Surg. 67:2123-2129, 2009.
- 8. Masucci, C.; Franchi, L.; Franceschi, D.; Pierleoni, F.; and Giuntini, V.: Post-pubertal effects of the Alt-RAMEC/FM and RME/FM protocols for the early treatment of Class III malocclusion: A retrospective controlled study, Eur. J. Orthod. 44:292-310, 2022.
- 9. Mucedero, M.; Coviello, A.; Baccetti, T.; Franchi, L.; and Cozza, P.: Stability factors after double-jaw surgery in Class III malocclusion: A systematic review, Angle Orthod. 78:1141-1152, 2008.
- 10. Cordasco, G.; Matarese, G.; Rustico, L.; Fastuca, S.; Caprioglio, A.; Lindauer, S.J.; and Nucera, R.: Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: A systematic review and meta-analysis, Orthod. Craniofac. Res. 17:133-143, 2014.
- 11. Jäger, A.; Braumann, B.; Kim, C.; and Wahner, S.: Skeletal and dental effects of maxillary protraction in patients with Angle Class III malocclusion: A meta-analysis, J. Orofac. Orthop. 62:275-284, 2001.
- 12. Da Silva Filho, O.G.; Magro, A.C.; and Capelozza, F.L.: Early treatment of the Class III malocclusion with rapid maxillary expansion and maxillary protraction, Am. J. Orthod. 113:196-203, 1998.
- 13. Wilmes, B.; Ngan, P.; Liou, E.J.; Franchi, L.; and Drescher, D.: Early Class III facemask treatment with the Hybrid Hyrax and Alt-RAMEC protocol, J. Clin. Orthod. 48:84-93, 2014.
- 14. Kircelli, B.H. and Pektas, Z.O.: Midfacial protraction with skeletally anchored face mask therapy: A novel approach and preliminary results, Am. J. Orthod. 133:440-449, 2008.
- 15. De Souza, R.A.; Rino Neto, J.; and de Paiva, J.B.: Maxillary protraction with rapid maxillary expansion and facemask versus skeletal anchorage with mini-implants in Class III patients: A non-randomized clinical trial, Prog. Orthod. 20:35, 2019.
- 16. Maino, G.; Turci, Y.; Arreghini, A.; Paoletto, E.; Siciliani, G.; and Lombardo, L.: Skeletal and dentoalveolar effects of and facemask treatment in growing skeletal Class III patients, Am. J. Orthod. 153:262-268, 2018.
- 17. Tortop, T.; Keykubat, A.; and Yuksel, S.: Facemask therapy with and without expansion, Am. J. Orthod. 132:467-474, 2007.
- 18. Masucci, C.; Franchi, L.; Giuntini, V.; and Defraia, E.: Short-term effects of a modified Alt-RAMEC protocol for early treatment of Class III malocclusion: A controlled study, Orthod. Craniofac. Res. 17:259-269, 2014.
- 19. Akbulut, S.; Yilmaz, S.; and Yagci, A.: Comparison of the short-term effects of facemask therapy preceded by conventional rapid maxillary expansion or by an alternate rapid maxillary expansions and constrictions protocol: A retrospective study, J. Orofac. Orthop. 84:278-286, 2023.
- 20. Isci, D.; Turk, T.; and Elekdag-Turk, S.: Activation-deactivation rapid palatal expansion and reverse headgear in Class III cases, Eur. J. Orthod. 32:706-715, 2010.
- 21. Liou, E.J.: Effective maxillary orthopedic protraction for growing Class III patients: A clinical application simulates distraction osteogenesis, Prog. Orthod. 6:154-171, 2005.
- 22. Moon, W.: Class III treatment by combining facemask (FM) and maxillary skeletal expander (MSE), Semin. Orthod. 24:95-107, 2018.
- 23. Özbilen, E.Ö.; Yılmaz, H.N.; and Acar, Y.B.: Does Alt-RAMEC protocol and facemask treatment affect dentoalveolar structures, Angle Orthod. 91:626-633, 2021.
- 24. Maino, G.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: MAPA: A new high precision 3D method of palatal mini-screw placement, Eur. J. Clin. Orthod. 3:41-47, 2015.
- 25. Maino, B.G.; Paoletto, E.; Lombardo, L. III; and Siciliani, G.: A three-dimensional digital insertion guide for palatal miniscrew placement, J. Clin. Orthod. 50:12-22, 2016.
- 26. Kim, Y.J.; Lim, S.H.; and Gang, S.N.: Comparison of cephalometric measurements and cone-beam computed tomography-based measurements of palatal bone thickness, Am. J. Orthod. 145:165-172, 2014.
- 27. Valverde Montalva, S.H.: Minimizing side effects during canine extrusion with twin brackets, J. Clin. Orthod. 55:559-560, 2021.
- 28. McNamara, J.A. Jr.: An orthopedic approach to the treatment of Class III malocclusion in young patients, J. Clin. Orthod. 21:598-608, 1987.
- 29. Choi, Y.J.; Chang, J.E.; Chung, C.J.; Tahk, J.H.; and Kim, K.H.: Prediction of long-term success of orthopedic treatment in skeletal Class III malocclusions, Am. J. Orthod. 152:193-203, 2017.
- 30. Stellzig-Eisenhauer, A.; Lux, C.J.; and Schuster, G.: Treatment decision in adult patients with Class III malocclusion: Orthodontic therapy or orthognathic surgery? Am. J. Orthod. 122:27-38, 2002.
- 31. Miranda, F.; Cunha Bastos, J.C.D.; Magno dos Santos, A.; Janson, G.; Pereira Lauris, J.R.; and Garib, D.: Dentoskeletal comparison of miniscrew-anchored maxillary protraction with hybrid and conventional hyrax expanders: A randomized clinical trial, Am. J. Orthod. 160:774-783, 2021.
- 32. Burns, N.R.; Musich, D.R.; Martin, C.; Razmus, T.; Gunel, E.; and Ngan, P.: Class III camouflage treatment: What are the limits? Am. J. Orthod. 137:9-11, 2010.
- 33. De Clerck, H.J. and Proffit, W.R.: Growth modification of the face: A current perspective with emphasis on Class III treatment, Am. J. Orthod. 148:37-46, 2015.
- 34. Alexander, A.E.; McNamara, J.A. Jr.; Franchi, L.; and Baccetti, T.: Semilongitudinal cephalometric study of craniofacial growth in untreated Class III malocclusion, Am. J. Orthod. 135:700-701, 2009.
- 35. Reyes, B.C.; Baccetti, T.; and McNamara, J.A. Jr.: An estimate of craniofacial growth in Class III malocclusion, Angle Orthod. 76:577-584, 2006.
- 36. Björk, A.: Prediction of mandibular growth rotation, Am. J. Orthod. 55:585-599, 1969.







COMMENTS
.