Tandem Skeletal Expander and MAPA Protocol for Palatal Expansion in Adults
Transverse maxillary deficiency, which is frequently seen among adolescent and adult patients seeking orthodontic care, can create clinical, esthetic, and functional problems in both arches. The cause is multifactorial, attributable to both genetic and functional factors. The most common clinical finding is a unilateral or bilateral posterior crossbite.1,2 As many as 30% of adult patients may develop transverse maxillary deficiencies and posterior crossbites because their malocclusions have been left untreated during growth.3
Rapid maxillary expansion (RME) is effective in growing patients, both for correcting maxillary arch constriction and a posterior crossbite and for expanding the arch perimeter to help resolve dental crowding.4 Traditional RME may be inadequate, however, in adult patients. To avoid side effects such as dentoalveolar tipping and bony dehiscence, alternative solutions must be considered. Surgically assisted rapid palatal expansion (SARPE) is a common therapeutic option for overcoming the increased resistance of the midpalatal suture.5,6 Although it does provide significant transverse skeletal correction, it has been associated with a considerable degree of relapse and patient discomfort.7,8
Another alternative is to use miniscrew-assisted boneborne and toothborne RME. Evidence suggests it is possible to avoid surgery and still achieve successful expansion of the midpalatal suture, with minimal buccal tipping or undesirable periodontal effects, by inserting palatal miniscrews to anchor the expander.9,10 Miniscrews placed in the paramedian anterior palate have a low failure rate and are therefore suitable for supporting orthodontic appliances.11,12 To safely insert the device in the correct position, we use a three-dimensional surgical guide designed specifically for palatal application: the MAPA System.*13,14 By enabling accurate preoperative planning based on volumetric tomography and customized software, the template ensures proper bicortical anchorage and parallelism of the implants.
In some adult cases, a single expansion screw may not provide optimal results. The Tandem Skeletal Expander** (TSE) comprises two expansion screws, which are mounted on four miniscrews inserted in the palate with the MAPA System (Fig. 1). The expansion screws are activated simultaneously to obtain parallel opening of the median suture, resulting in equivalent anterior and posterior increases in the transverse dimension.
This article describes the TSE and illustrates its use in two adult patients whose transverse maxillary deficiencies and crossbites were successfully treated using a skeletally anchored maxillary expansion protocol.
Case 1
A 25-year-old male presented with a transverse maxillary deficiency, left lateral crossbite, and agenesis of the upper lateral incisors (Fig. 2A). Although he was highly motivated to resolve his malocclusion and obtain a pleasant smile, he refused surgery and demanded esthetic, noninvasive treatment.
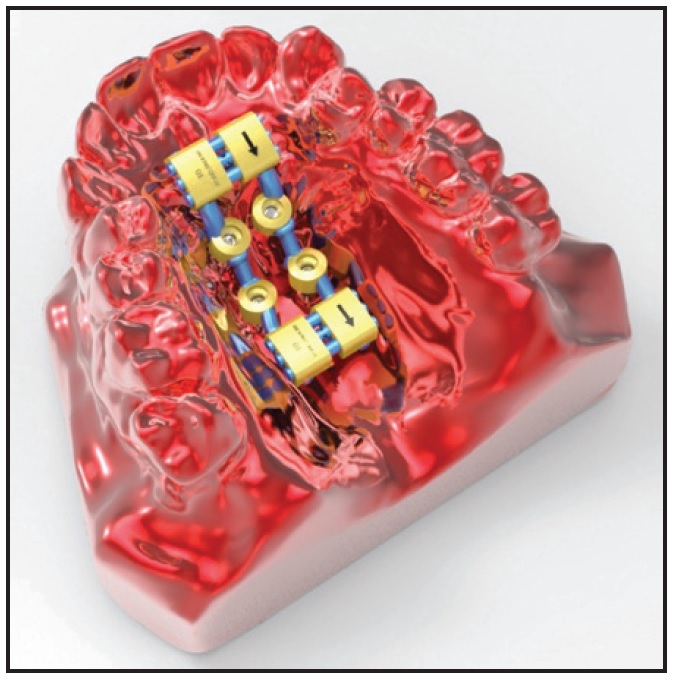
Fig. 1 Tandem Skeletal Expander** (TSE).
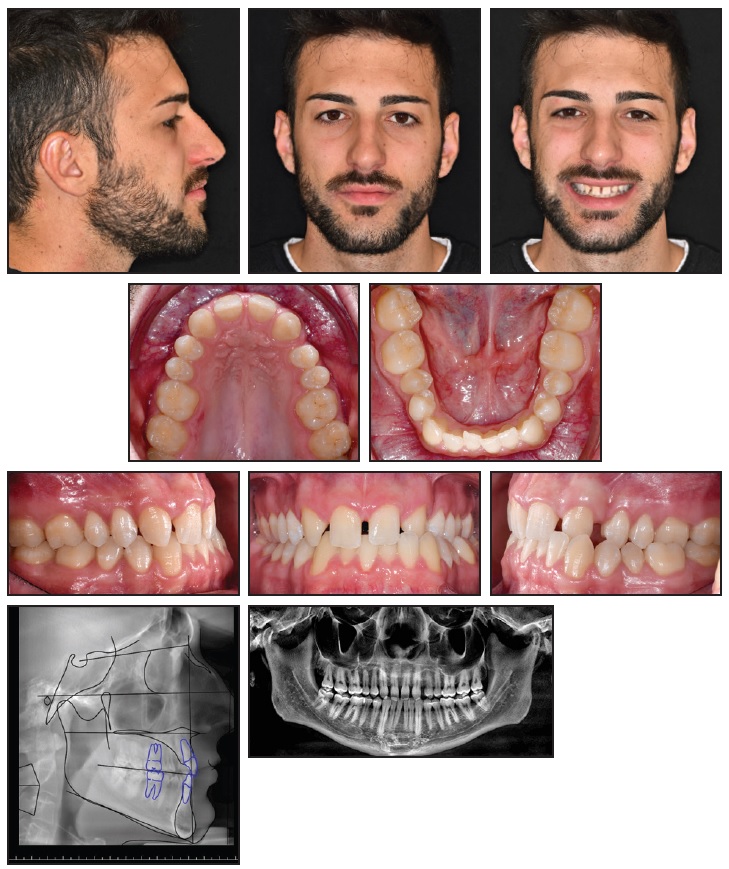
Fig. 2 Case 1. 25-year-old male patient with transverse maxillary deficiency and left lateral crossbite before treatment (continued in next image).
From a frontal view, the patient’s face appeared harmonious, with the lower third proportional to the middle and the upper thirds. The mandibular symphysis was deviated to the left. He had a straight profile, a proper nasolabial angle, and a good maxillary bone relationship. Except for the missing upper lateral incisors, all teeth were present, including normally erupted third molars. Bilateral Class I molar relationships were observed, with a Class I canine relationship on the right side and Class II on the left. The lower arch was slightly crowded, and the midline was deviated to the left. The upper arch presented a central diastema and dental asymmetry because of the more distal position of the upper left quadrant. The adjacent teeth had not entirely migrated into the space of the missing lateral incisors, leaving diastemas, especially on the left side. A maxillary transverse deficiency had directly caused the left lateral crossbite (Fig. 2B.
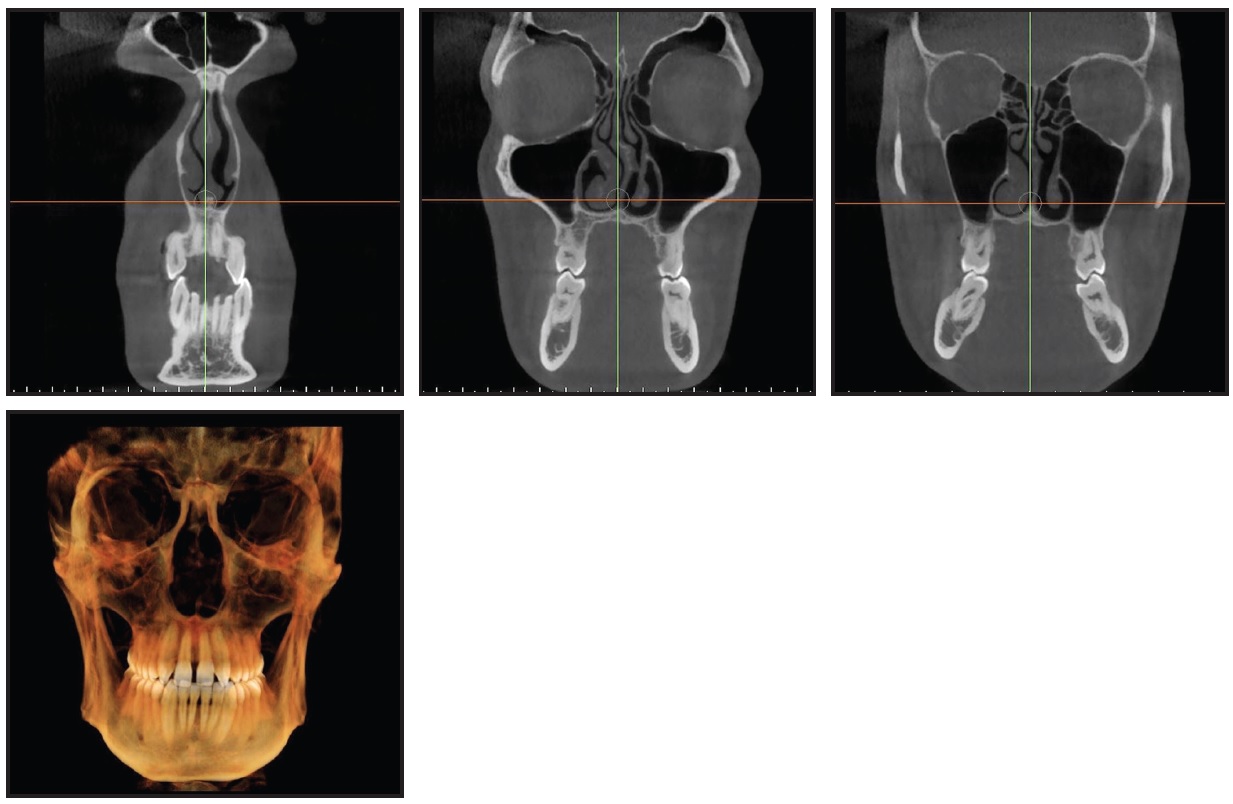
Fig. 2 (cont.) Case 1. 25-year-old male patient with transverse maxillary deficiency and left lateral crossbite before treatment.
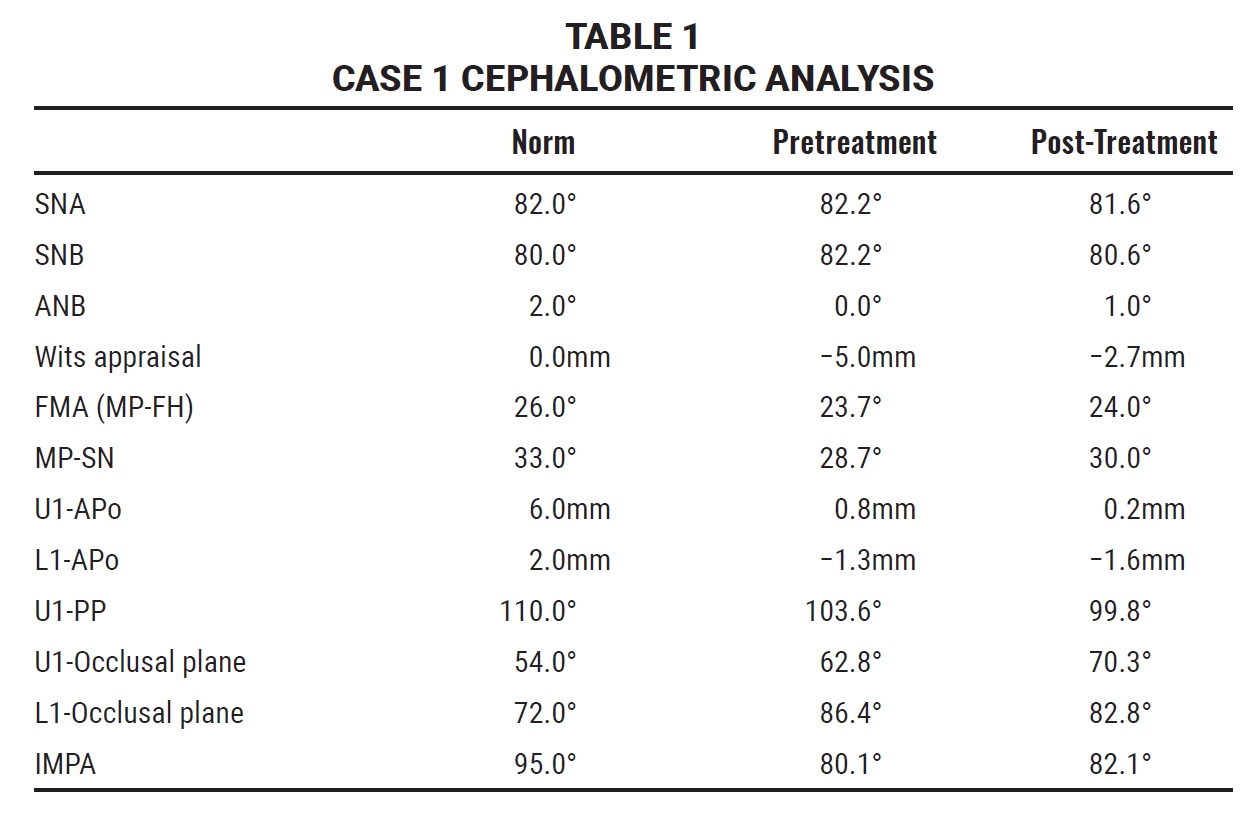
Axial cone-beam computed tomography (CBCT) slices at the upper canines and premolars and at the furcation of the first molars confirmed the maxillary transverse deficiency, the left lateral crossbite, and an accentuated curve of Wilson. Cephalometric analysis (Table 1) indicated a Class III relationship (ANB = 0°, Wits appraisal = −5mm). The skeletal growth pattern was normodivergent (FMA = 23.7°). The upper incisors were normally inclined with respect to the palatal plane (U1-PP = 103.6°), and the lower incisors were retroclined relative to the mandibular plane (IMPA = 80.1°).
A two-phase treatment was planned using skeletal maxillary expansion to obtain orthopedic correction of the transverse deficiency, followed by dental alignment. The optimal site for miniscrew insertion was identified on the CBCT scan and superimposed onto the stereolithographic (STL) image of the digital model (Fig. 3). The anteroposterior insertion sites were selected based on the thickness and width of the palatal vault. A 3D surgical guide, properly fitting the morphology of the palate, was then printed using the MAPA System.
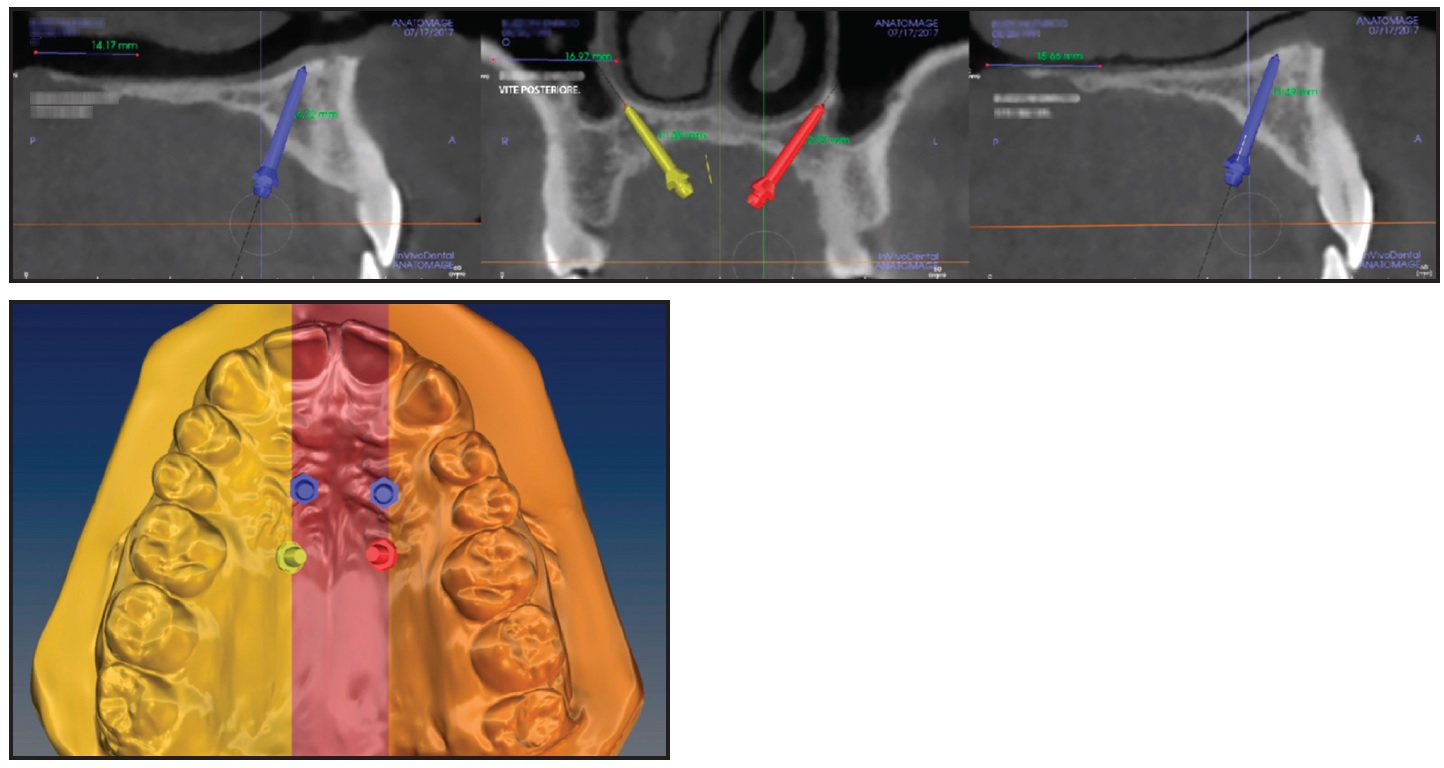
Fig. 3 Case 1. Virtual planning of miniscrew insertion sites based on Digital Imaging and Communication in Medicine (DICOM) and stereolithographic (STL) files.
A TSE was fabricated from a polyvinyl siloxane impression of the upper arch and a digital design (Fig. 4).
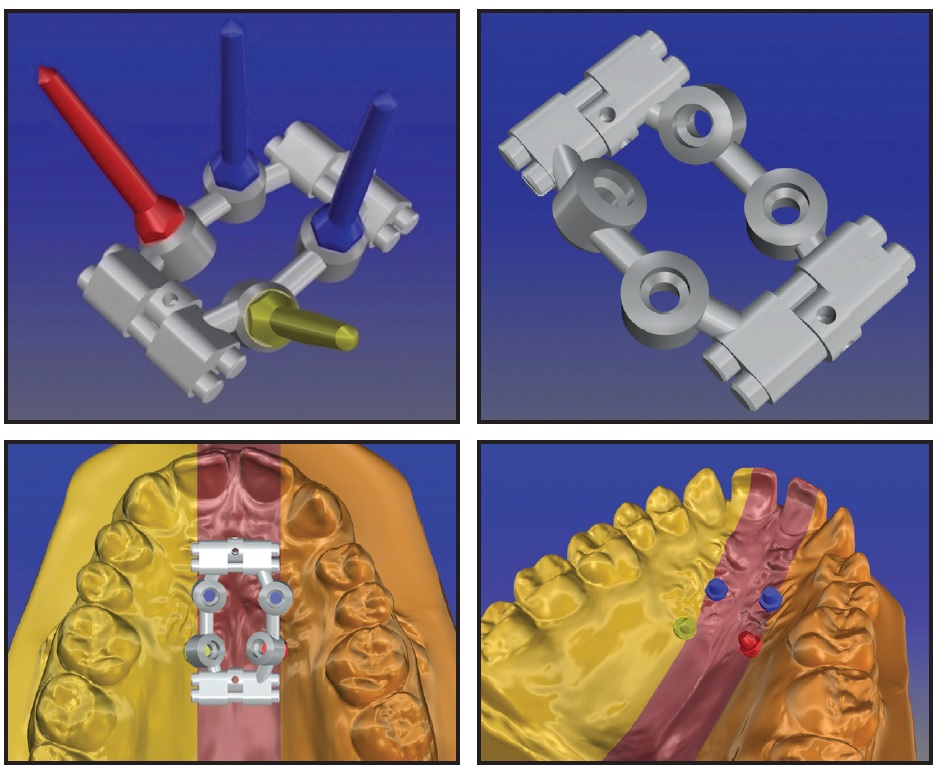
Fig. 4 Case 1. Digital design and placement of TSE.
Four 11mm × 2mm Spider*** miniscrews were inserted into the palate while carefully maintaining accurate control of the direction of insertion, and the TSE was attached. The patient was instructed to perform two activations per day. After 20 days, an increased upper incisor diastema was apparent, but the palatal constriction was not completely corrected (Fig. 5).
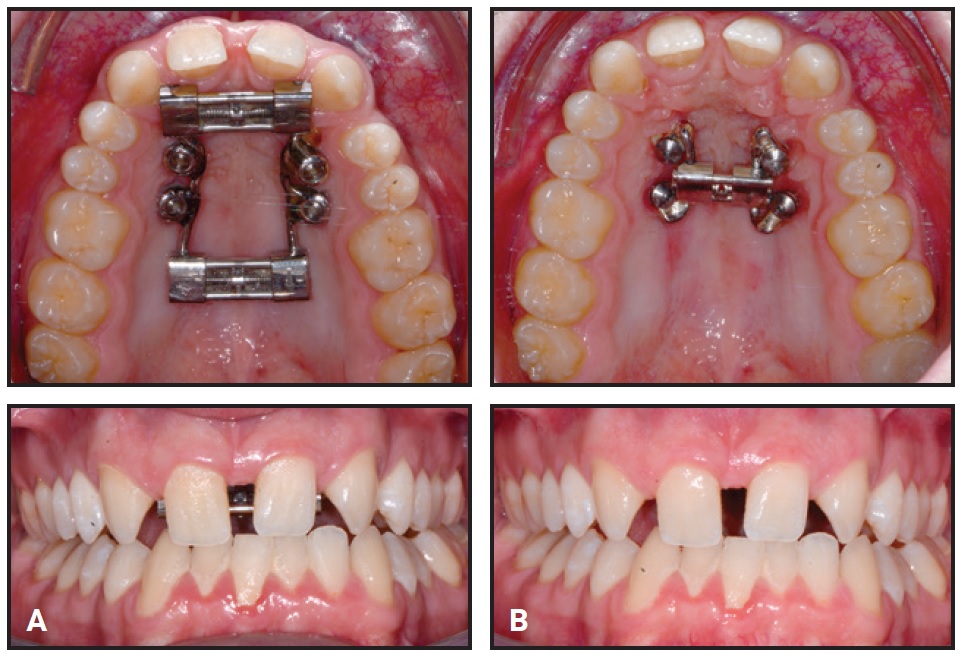
Fig. 5 Case 1. A. After 20 days of expansion, transverse deficiency not completely corrected. B. Second expander in place.
Therefore, we placed a second boneborne expander to achieve the orthopedic objective. The treatment protocol again involved two activations per day until the maxillary transverse deficiency was completely resolved.
After 10 days with the second TSE, the transverse constriction and lateral crossbite had been corrected by pure skeletal expansion of the midpalatal suture (Fig. 6).

Fig. 6 Case 1. After 10 days of expansion with second expander.
The amount of expansion ranged from 7.44mm in the anterior region to 5.05mm in the posterior region (Fig. 7).
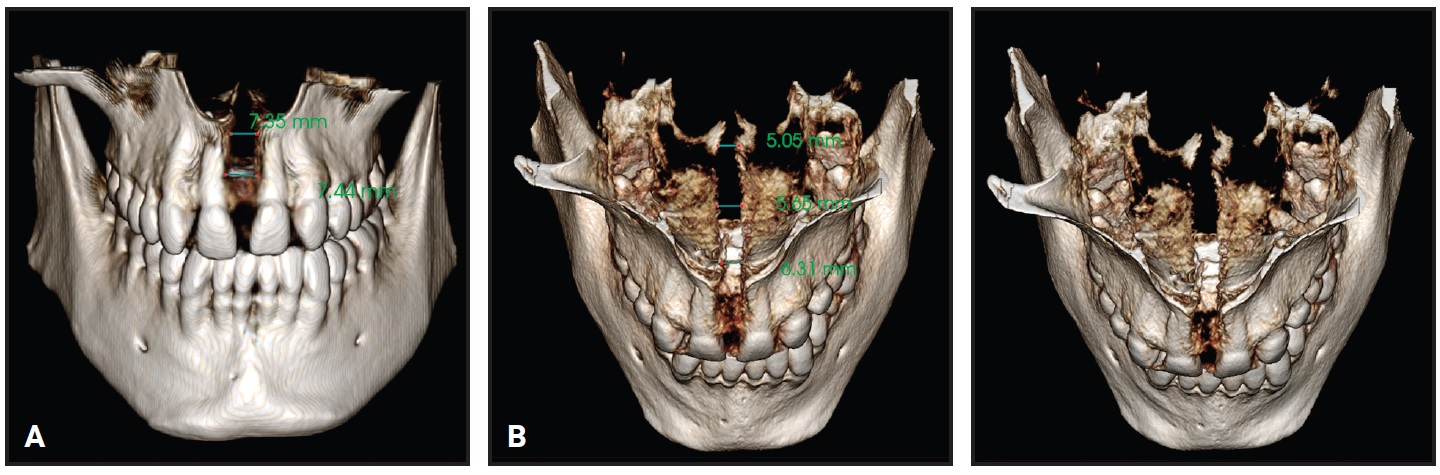
Fig. 7 Case 1. A. Anterior expansion of midpalatal suture. B. Posterior expansion.
An increased open bite was observed due to premature contact between the upper and lower third molars (Fig. 8), but no buccal tipping or molar protraction occurred (Fig. 9).
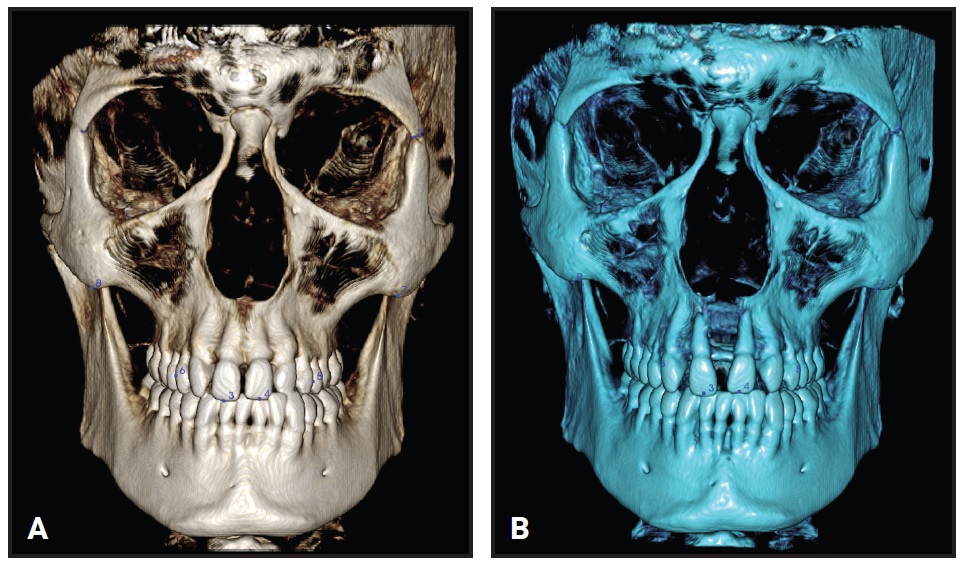
Fig. 8 Case 1. A. Before treatment. B. After expansion.
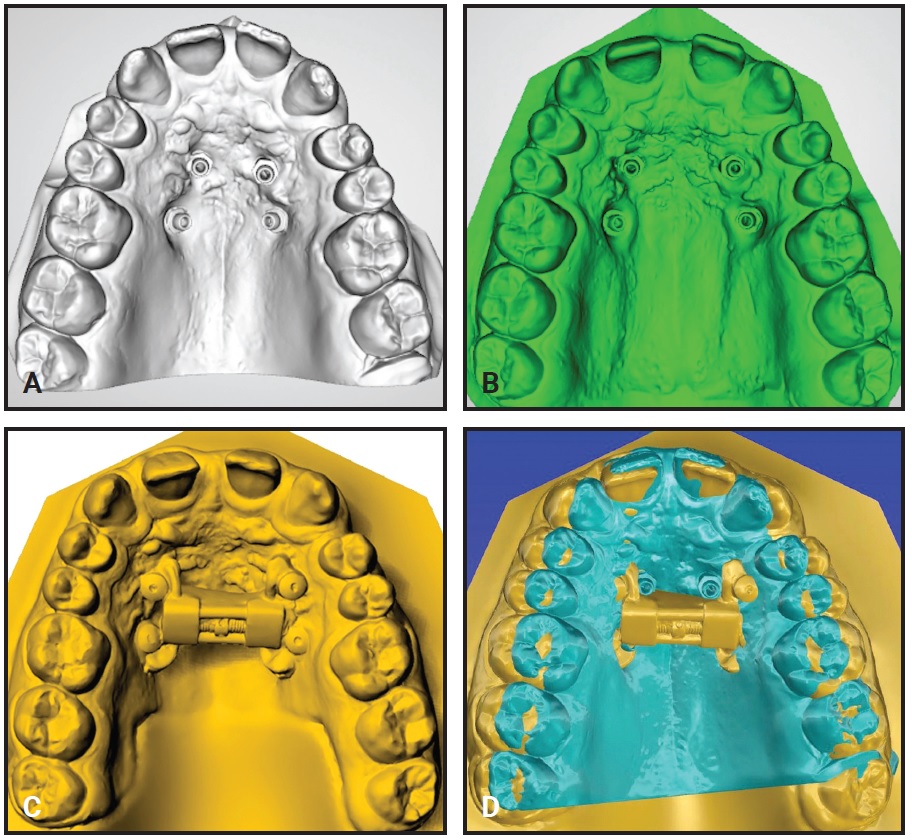
Fig. 9 Case 1. A. Before treatment. B. After first expansion. C. After second expansion. D. Superimposition of pre- and post-expansion models.
Treatment was completed using standard fixed lingual appliances in the upper arch and aligners in the lower arch. Total treatment time was 18 months.
Case 2
A 24-year-old male presented with a skeletal and dental Class III malocclusion (Fig. 10A). Bimaxillary orthognathic surgery had been planned when the patient was 18 years old. At that time, both lower first premolars had been extracted, and both arches had been leveled and aligned. The patient delayed the orthognathic surgery and returned six years later to continue treatment.

Fig. 10 Case 2. 24-year-old male patient with skeletal and dental Class III malocclusion and maxillary deficiency before treatment (continued in next image).
A maxillary deficiency was apparent from a frontal view. The dental midlines were coincident with the facial midline, and the lower third of the face was well balanced with the central and upper thirds. The patient exhibited a concave profile with a protrusive mandible and a backwardly positioned maxilla. Intraoral examination found Class III molar and canine relationships on the right and left sides, with no crowding in either arch (Fig 10B). Two miniscrews, which had been used as anterior anchorage for the previous orthodontic treatment, were present in the lower arch. Except for the lower first premolars, all teeth were present.
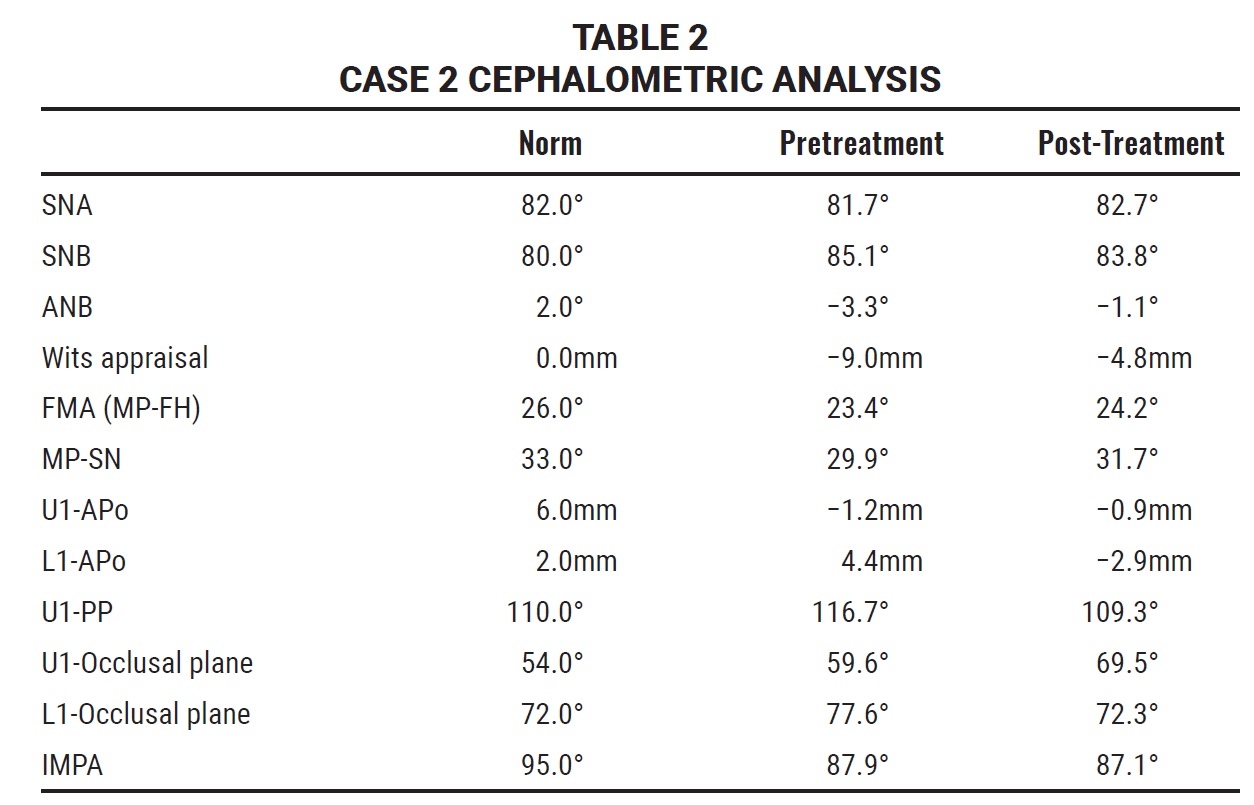
Cephalometric analysis (Table 2) confirmed a Class III relationship (ANB = −3.3°, Wits appraisal = −9mm). The skeletal growth pattern was normodivergent (FMA = 23.4°). The upper incisors were mesially inclined with respect to the palatal plane (U1-PP = 116.7°), and the lower incisors were normally inclined (IMPA = 87.9°).
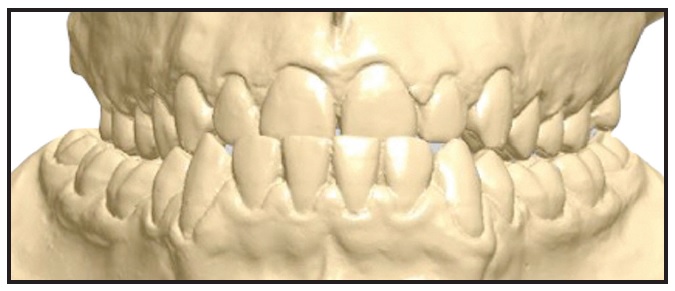
Fig. 10 (cont.) Case 2. 24-year-old male patient with skeletal and dental Class III malocclusion and maxillary deficiency before treatment. (Lower first premolars were extracted six years earlier during prior treatment.)
Axial CBCT slices at the upper canines and premolars and at the furcation of the first molars confirmed the maxillary transverse deficiency and the bilateral crossbite, which could also be observed in a diagnostic simulation of the proposed maxillary advancement surgery (Fig. 11).
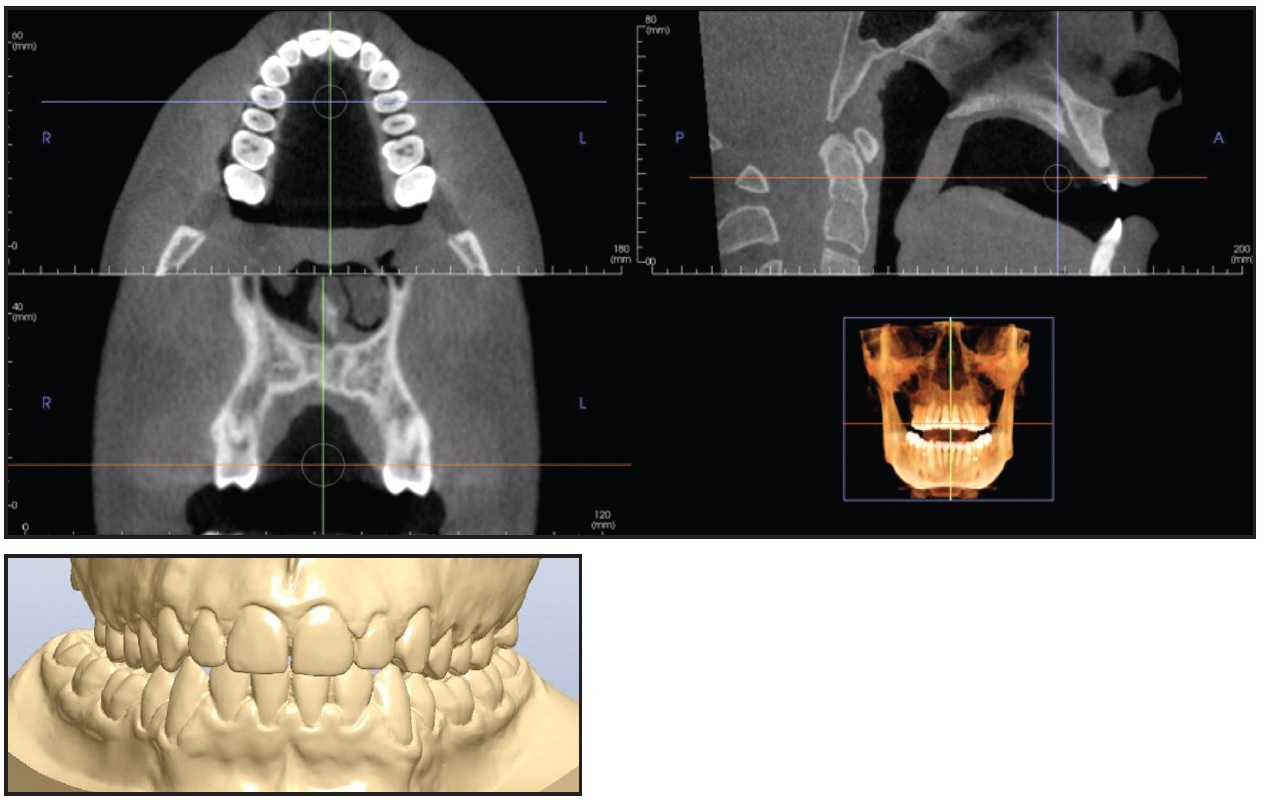
Fig. 11 Case 2. Transverse maxillary deficiency and bilateral crossbite apparent in cone-beam computed tomography and in diagnostic simulation of maxillary advancement surgery.
Because both the upper and lower arches had been leveled and aligned, the front teeth were correctly inclined, and the Class III molar and canine relationships were symmetrical, a “surgery first” approach was chosen to correct the transverse discrepancy. In consultation with the maxillofacial surgeon, we planned a noninvasive skeletal maxillary expansion with a boneborne RME. Because of the narrow and high palatal vault, a TSE was used with the MAPA System.
The optimal sites for miniscrew insertion were identified on the CBCT scan, considering the thickness and width of the palatal vault (Fig. 12).
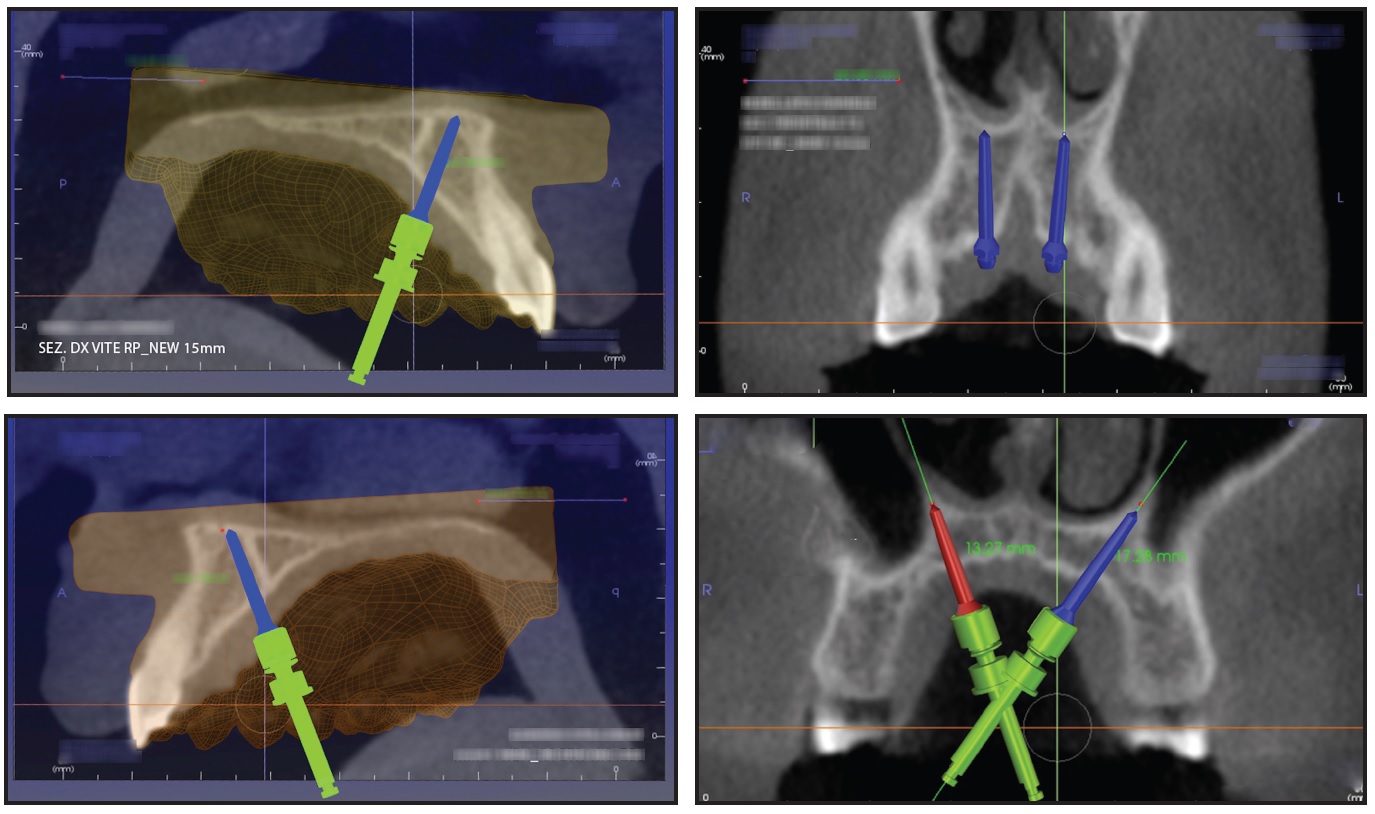
Fig. 12 Case 2. Virtual programming of miniscrew insertion using DICOM images.
Four miniscrews (2mm in diameter) were inserted in the palatal vault: two 15mm miniscrews in the front, one 13mm miniscrew in the posterior right side, and one 15mm miniscrew in the posterior left side (Fig. 13). A TSE was placed, and the patient was instructed to perform two activations per day. The palatal expansion was completed after 21 days, when a diastema had developed between the central incisors as a result of opening the midpalatal suture (Fig. 14).
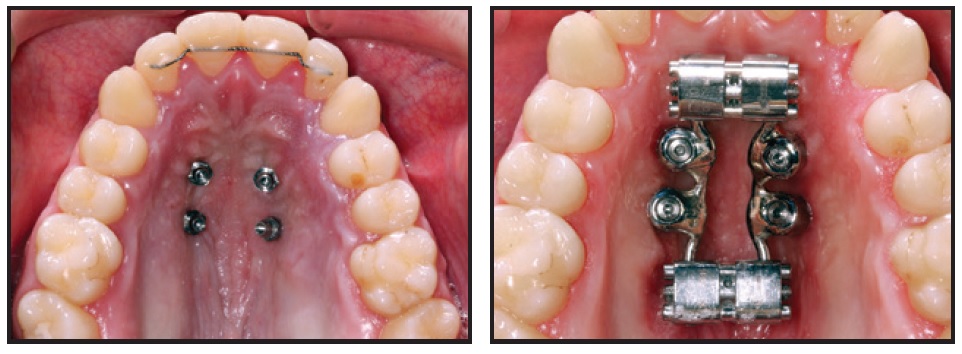
Fig. 13 Case 2. TSE anchored by four miniscrews.

Fig. 14 Case 2. After 21 days of expansion.
At this point, the bilateral crossbite was still present. A new impression of the upper arch was used to simulate surgical forward movement of the maxilla into a Class I canine relationship (Fig. 15). Because this diagnostic simulation showed that the transverse expansion was adequate (Fig. 16), we decided to block the TSE and proceed with surgical-orthodontic treatment. The amount of expansion ranged from 6.1mm in the anterior region to 5.71mm in the posterior region (Fig. 17). No dental or periodontal side effects were observed, nor was any buccal tipping or molar protraction (Fig. 18).
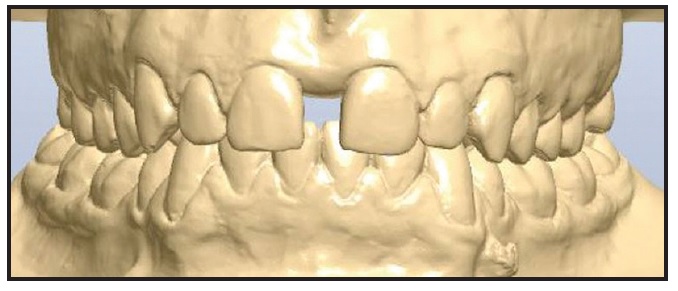
Fig. 15 Case 2. Diagnostic simulation of maxillary advancement.
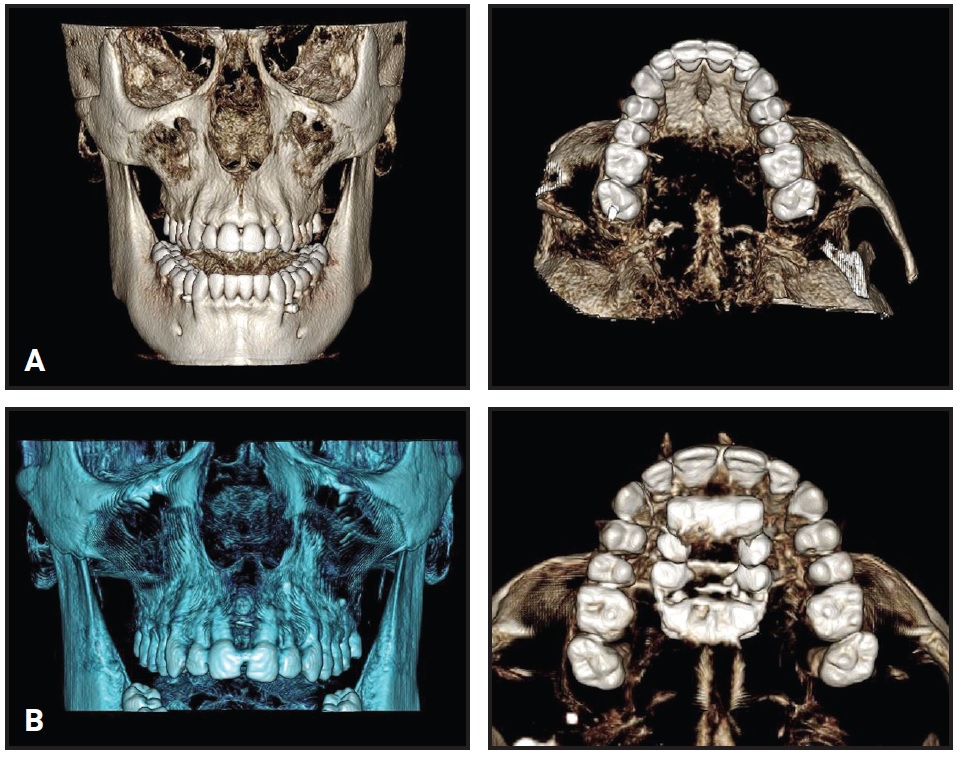
Fig. 16 Case 2. A. Before treatment. B. After expansion.
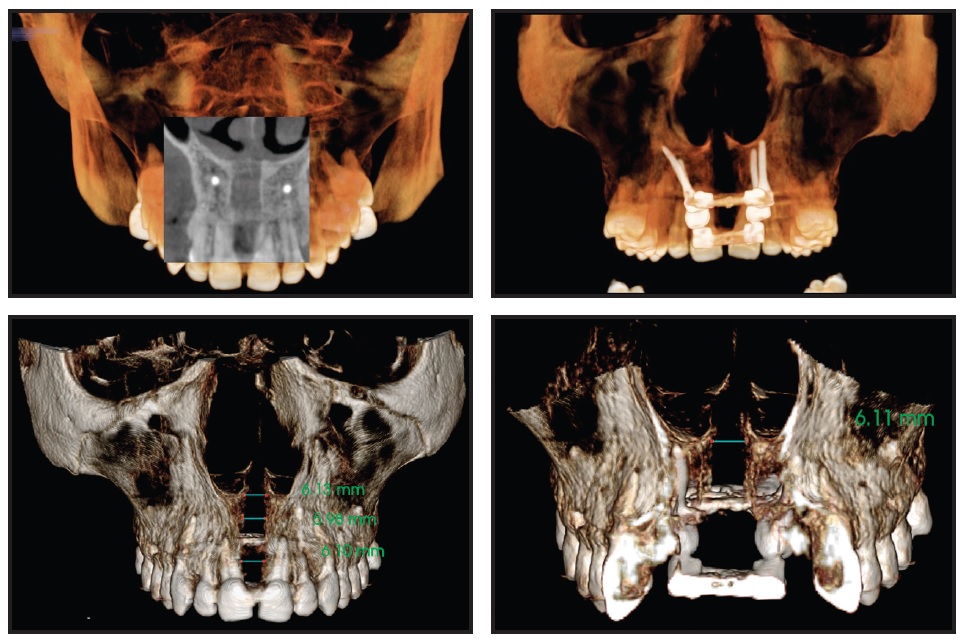
Fig. 17 Case 2. Expansion of midpalatal suture.

Fig. 18 Case 2. A. Before treatment. B. After expansion. C. Superimposition of pre- and post-expansion models.
Treatment was completed in a total of 20 months using a combination of fixed labial appliances and orthognathic surgery.
Discussion
Rapid maxillary expansion is the preferred treatment for correcting posterior crossbite and transverse deficiency when the midpalatal suture can be separated before its ossification.15 When RME is performed in an adult, however, the maxillary adaptation shifts from a skeletal level to a dentoalveolar level. The constriction is then corrected by buccal tipping of the posterior teeth,16 which may lead to collateral effects such as bending of the alveolar bone, fenestration of the buccal cortex, pain, and instability of the expansion.17,18 Lee and colleagues successfully treated a transverse discrepancy in a 20-year-old patient a using a miniscrew-assisted rapid palatal expander (MARPE), an expansion appliance supported by palatal miniscrews, with minimal damage to the teeth and periodontium and a stable long-term outcome.9 In each of the two cases shown here, we used four miniscrews to anchor the palatal expander, thus avoiding any damage to anatomical structures while achieving true skeletal expansion.
Because the palatal vault is often narrow and high, with little available bone, the proximity of four miniscrews would force the clinician to place the expansion screw off-center in the palate. This configuration could expose the expansion screw to excessive mechanical stress, which, along with the considerable resistance of the maxillary suture in an adult, could cause distortion of the appliance and consequent blockage of the expansion screw.19,20 The TSE was developed to address these problems. The use of two off-center expansion screws can overcome the biomechanical limitations of the system and increase resistance to deformation. Because the appliance is digitally designed, the virtual positions of the expansion screws can be checked in occlusal and sagittal views (Fig. 19).
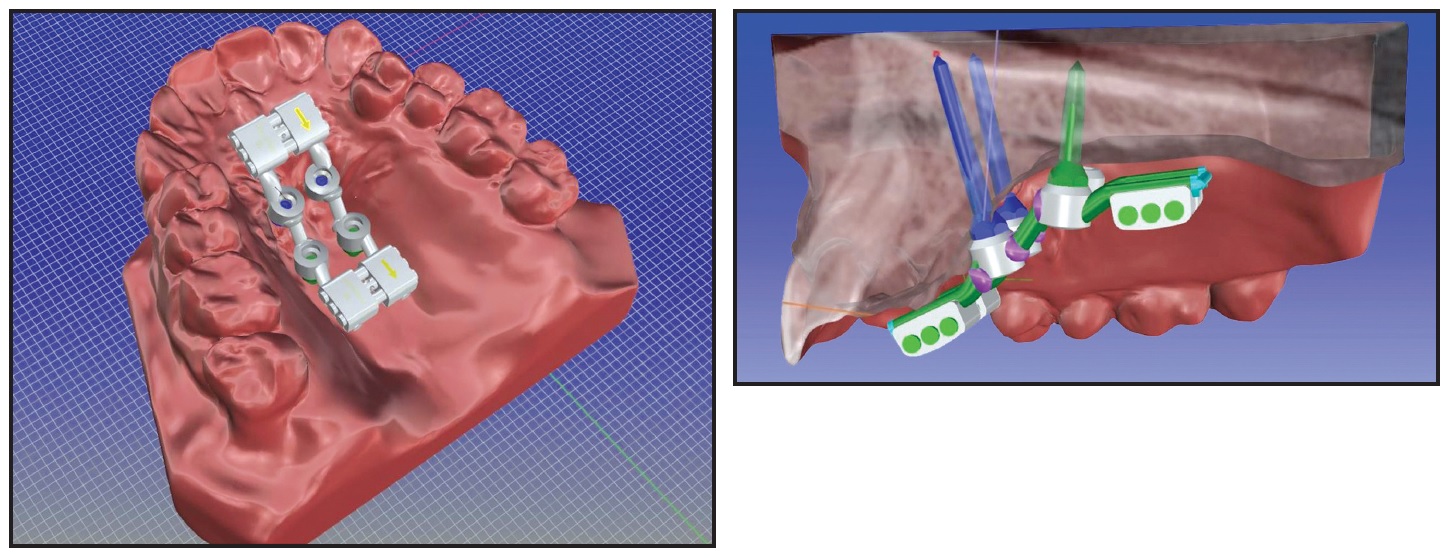
Fig. 19 Digital occlusal and sagittal views of TSE and miniscrews.
A six-month stabilization was planned after the end of maxillary expansion in each of our cases, although there is no evidence in the literature to suggest such a period. Because a double boneborne expander was used in each patient, no buccal tipping or molar protraction occurred. Transverse expansion was achieved by a purely skeletal and almost symmetrical expansion of the anterior and posterior areas of the palate, without any dental side effects. Once the transverse deficiency was resolved, each patient was ready to continue with a second phase of treatment according to the original plan. Digital design and the use of a 3D surgical guide with the MAPA System made the procedure simple for the clinician and minimally invasive for the patient, while protecting the anatomical structures.
FOOTNOTES
- *Orthomodul, Thiene, Italy; www.orthomodul.it.
- **Registered trademark of Orthomodul, Thiene, Italy; www.orthomodul.it.
- ***Registered trademark of HDC SRL, Thiene, Italy. Distributed by Ortho Technology, Inc., Lutz, FL; www.orthotechnology.com.
REFERENCES
- 1. Brunelle, J.; Bhat, M.; and Lipton, J.: Prevalence and distribution of selected occlusal characteristics in the US population, 1988-1991, J. Dent. Res. 75:706-713, 1996.
- 2. Kutin, G. and Hawes, R.: Posterior cross-bites in the deciduous and mixed dentitions, Am. J. Orthod. 5:491-504, 1969.
- 3. Kurol, J. and Berglund, L.: Longitudinal study and cost-benefit analysis of the effect of early treatment of posterior cross-bites in the primary dentition, Eur. J. Orthod. 3:173-179, 1992.
- 4. Zhou, Y.; Long, H.; Niansong, Y.; Xue, J.; Yang, X.; Liao, L.; and Lai, W.: The effectiveness of non-surgical maxillary expansion: A meta-analysis, Eur. J. Orthod. 2:233-242, 2013.
- 5. Capelozza, F.L.; Cardosa Neto, J.; da Silva Filho, O.G.; and Ursi, W.J.: Non-surgically assisted rapid maxillary expansion in adults, Int. J. Adult Orthod. Orthog. Surg. 1:57-66, 1996.
- 6. Gurel, H.G.; Memili, B.; Erkan, M.; and Sukurica, Y.: Long-term effects of rapid maxillary expansion followed by fixed appliances, Angle Orthod. 1:5-9, 2010.
- 7. Lee, H.K.; Bayome, M.; Ahn, C.S.; Kim, S.H.; Kim, K.B.; Mo, S.S.; and Kook, Y.A.: Stress distribution and displacement by different bone-borne palatal expanders with micro-implants: A three-dimensional finite-element analysis, Eur. J. Orthod. 5:531-540, 2014.
- 8. Byloff, F.K. and Mossaz, C.F.: Skeletal and dental changes following surgically assisted rapid palatal expansion, Eur. J. Orthod. 4:403-409, 2004.
- 9. Lee, K.; Park, Y.C.; Park, J.; and Hwang, W.: Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism, Am. J. Orthod. 6:830-839, 2010.
- 10. Cantarella, D.; Dominquez-Mompell, R.; Mallya, S.M.; Moschik, C.; Pan, H.C.; Miller, J.; and Moon, W.: Changes in the midpalatal and pterygopalatine sutures induced by micro-implant-supported skeletal expander, analyzed with a novel 3D method based on CBCT imaging, Prog. Orthod. 1:34, 2017.
- 11. Gracco, A.; Lombardo, L.; Cozzani, M.; and Siciliani, G.: Quantitative cone-beam computed tomography evaluation of palatal bone thickness for orthodontic miniscrew placement, Am. J. Orthod. 3:361-569, 2008.
- 12. Winsauer, H.; Vlachojannis, C.; Bumann, A.; Vlachojannis, J.; and Chrubasik, S.: Paramedian vertical palatal bone height for mini-implant insertion: A systematic review, Eur. J. Orthod. 5:541-549, 2014.
- 13. Maino, G.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: MAPA: A new high-precision 3D method of palatal miniscrew placement, Eur. J. Clin. Orthod. 3:41-47, 2015.
- 14. Maino, G.B.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: A three dimensional digital insertion guide for palatal miniscrew placement, J. Clin. Orthod. 1:12-22, 2016.
- 15. McNamara, J.J.: Long-term adaptation to changes in the transverse dimension in children and adolescents: An overview, Am. J. Orthod. 4:71-74, 2006.
- 16. Baccetti, T.; Franchi, L.; Cameron, C.G.; and McNamara, J.A.: Treatment timing for rapid maxillary expansion, Angle Orthod. 5:343-350, 2001.
- 17. Greenbaum, K. and Zachrisson, B.U.: The effect of palatal expansion therapy on the periodontal supporting tissues, Am. J. Orthod. 1:12-21, 1982.
- 18. Alpern, M. and Yurosko, J.: Rapid palatal expansion in adults with and without surgery, Angle Orthod. 7:245-263, 1987.
- 19. Lombardo, L.; Carlucci, A.; Maino, B.G.; Colonna, A.; Paoletto, E.; and Siciliani, G.: Class III malocclusion and bilateral cross-bite in an adult patient treated with miniscrew-assisted rapid palatal expander and aligners, Angle Orthod. 5:649-664, 2018.
- 20. Maino, B.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: From planning to delivery of a bone-borne rapid maxillary expander in one visit, J. Clin. Orthod. 4:196-207, 2017.





COMMENTS
.