Space Closure with Single Miniscrews in Patients with Upper Lateral-Incisor Agenesis
Agenesis of the maxillary lateral incisors is a common developmental anomaly, with a prevalence of 1-3%. Caucasians represent about 20% of these cases,1-4 and females seem to be affected more than males.
Clinical management generally requires a multidisciplinary approach to meet esthetic and functional goals. Two basic orthodontic options have been employed: space opening for prosthetic replacement, or the more conservative space closure with canine substitution.5,6 Space closure, where feasible, has the added benefit of preserving the natural teeth in the upper anterior region—an important area for esthetics.
Miniscrews offer several advantages when used as temporary anchorage devices (TADs), includingeasy placement and removal, the potential of immediate loading, and the flexibility of application in a variety of situations.7-9 This article demonstrates the use of miniscrews for space closure in young and adult patients with upper lateral-incisor agenesis. The innovative aspect of this technique is that the miniscrew is inserted on the buccal side between the upper central incisors, as opposed to the more typical palatal placement.
Case 1
A 48-year-old male presented with the chief complaint of an unesthetic smile (Fig. 1). He had a Class II malocclusion, a diastema between the upper central incisors, and missing upper lateral incisors, but the midlines were centered. The upper left central incisor appeared to be extruded and showed a loss of gingival attachment and bone. The patient displayed a convex profile with slight mandibular retrusion.
Similar articles from the archive:
- Unilateral Upper Central Incisor Space Closure Using Palatal Mini-Implants February 2022
- Maxillary Space Closure Using Aligners and Palatal Mini-Implants in Patients with Congenitally Missing Lateral Incisors January 2021
- Orthodontic Space Closure vs. Implant-Borne Crowns in Patients with Congenitally Missing Maxillary Lateral Incisors May 2018

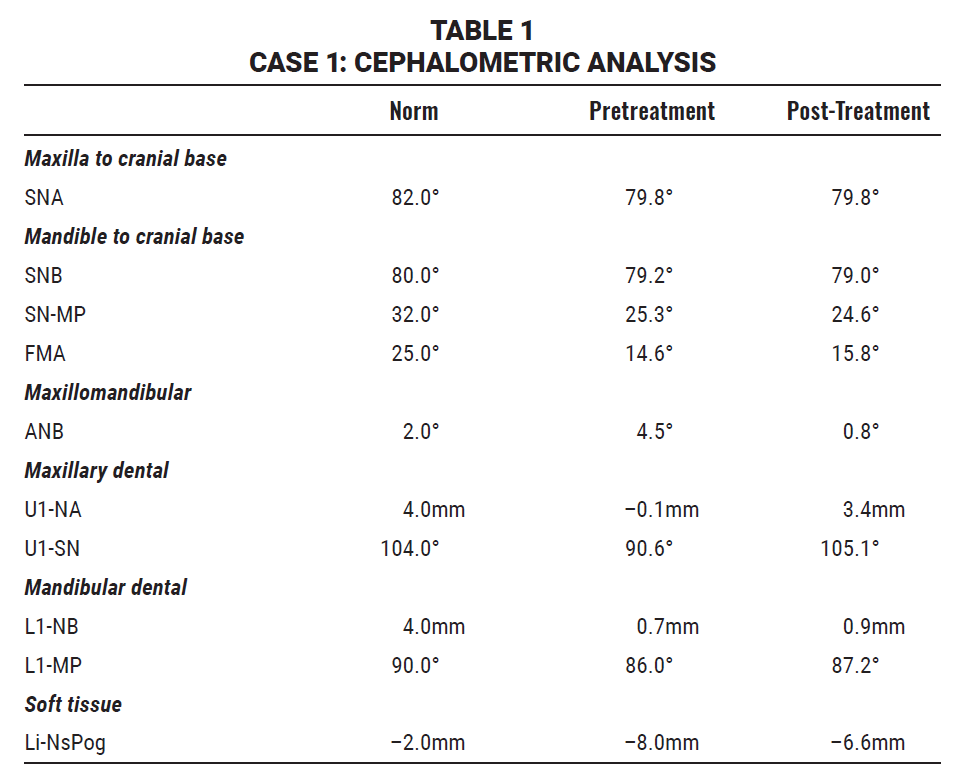
Fig. 1 Case 1. 48-year-old male patient with Class II malocclusion, convex profile, missing upper lateral incisors, and diastema between upper central incisors before treatment.
The panoramic radiograph revealed the presence of the lower left third molar, as well as granulomas on the lower left first premolar and first molar. The upper right second molar was absent, and the upper right canine root was dilacerated. Cephalometric analysis indicated a skeletal Class II malocclusion with a reduced divergence and palatal inclination of the upper central incisors (Table 1). The overjet was 1mm, and the overbite was 4mm.
Treatment goals were to eliminate the diastema by closing space in the maxillary anterior area, to intrude the upper left central incisor, and to properly incline the upper central incisors while improving the patient’s periodontal health. For better control of tooth movement during space closure, skeletal anchorage was planned from a miniscrew between the upper central incisors.
The patient was referred for regenerative mucogingival surgery to improve the periodontal defect on the upper left central incisor, using Biocoral* membrane. Subsequently, .022" Roth-prescription Empower** self-ligating brackets were bonded in the upper arch, and an .014" nickel titanium archwire was placed. A 1.5mm × 11mm miniscrew*** was inserted between the upper central incisors under local anesthesia (Fig. 2). The miniscrew was connected to both upper canines with a light elastomeric chain, to be changed once per month, for space closure.
Two months later, the miniscrew was connected to the upper central incisors; another two months later, a heavier elastomeric chain was attached from the miniscrew to the upper first premolars (Fig. 3).
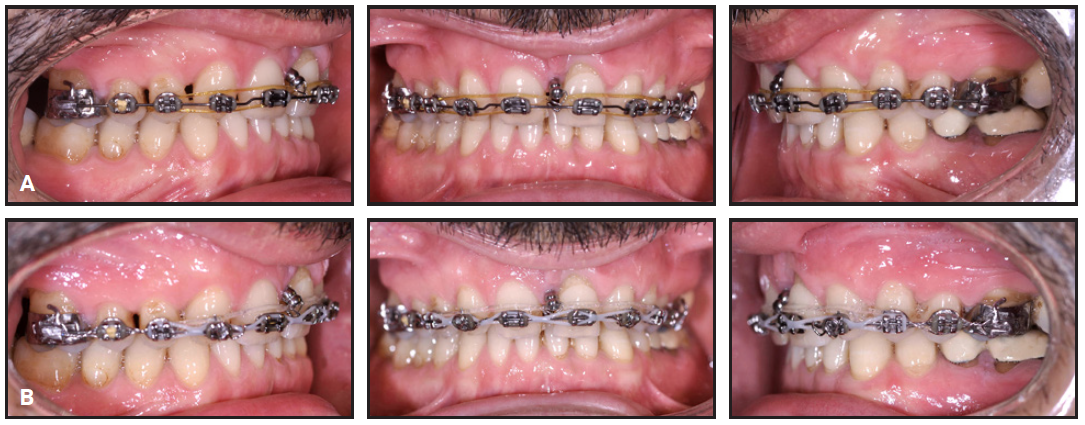
Fig. 3 Case 1. A. After two months of treatment, miniscrew connected to upper central incisors. B. Two months later, heavier elastomeric chain attached to upper first premolars.
After eight months of treatment, the miniscrew was removed and space closure was continued with only the elastomeric chain between the upper first premolars. At this point, the lower arch was bonded (Fig. 4). The wire sequence for both arches progressed from .014" nickel titanium to .016" nickel titanium, .016" × .022" nickel titanium, .018" × .022" stainless steel, and .018" × .025" stainless steel.
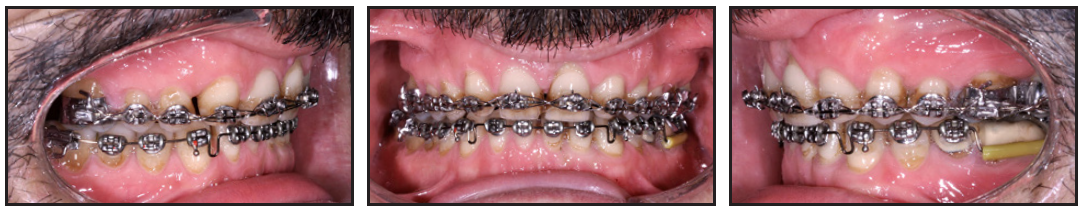
Fig. 4 Case 1. After eight months of treatment, miniscrew removed and lower arch bonded.
In the last stage of treatment, uprighting springs were applied to the upper central incisors to enhance torque control. This phase was crucial to avoid lingual tipping of the central incisors—a common side effect of a central miniscrew.
Treatment was concluded in three years (Fig. 5). A positioner retainer was initially delivered, but it was replaced with vacuformed retainers after three months. The patient’s anterior maxillary spaces were closed, as was the central diastema. The inclination of the upper central incisors was corrected (Table 1), and both arches were leveled and aligned. The periodontal problem on the upper left central incisor was improved.
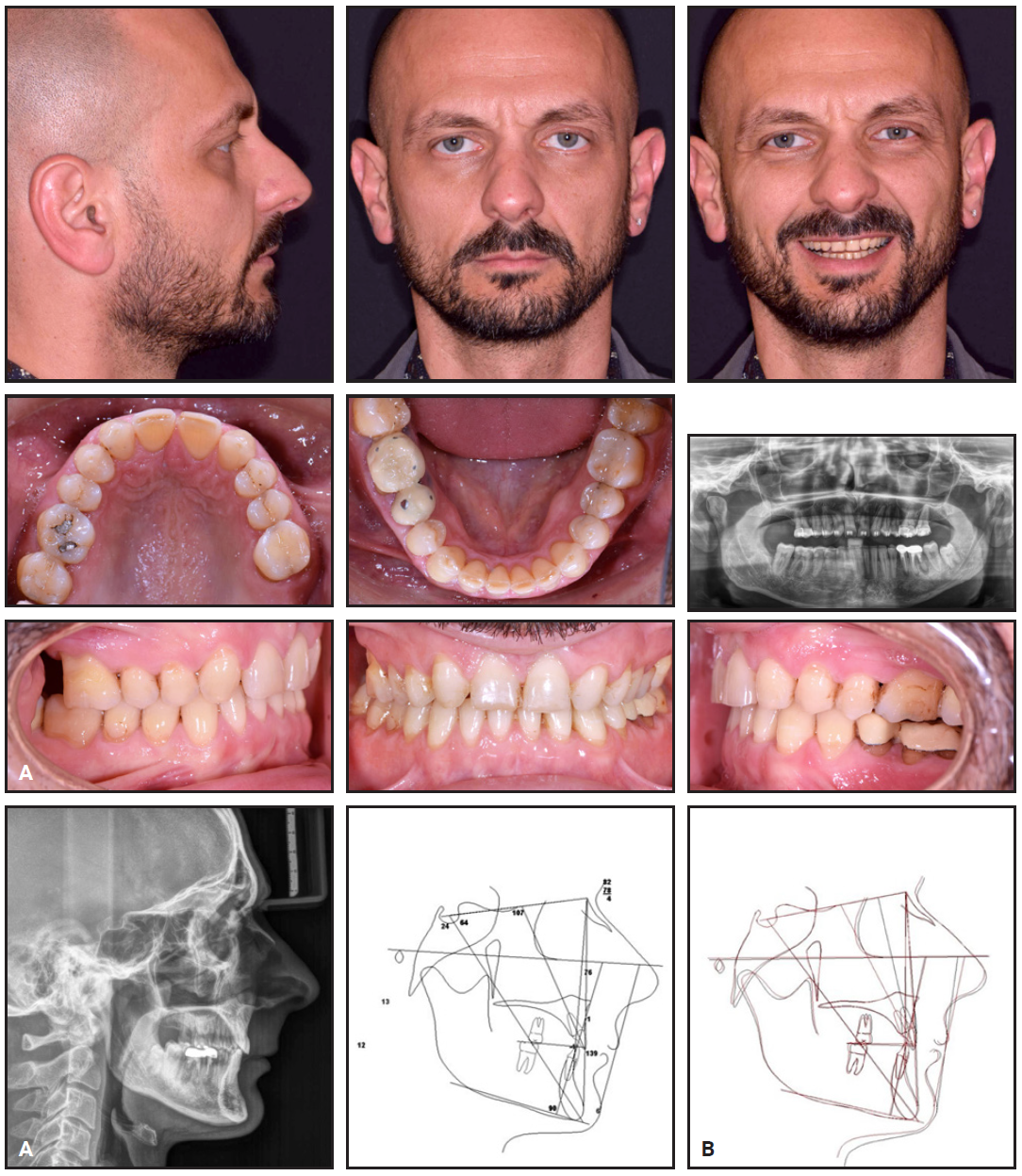
Fig. 5 Case 1. A. Patient after three years of treatment. B. Superimposition of pre- and post- treatment cephalometric tracings.
Case 2
A 10-year-old male in the mixed dentition presented for treatment (Fig. 6). His first molars, central incisors, and lower lateral incisors had erupted, but a panoramic radiograph confirmed the diagnosis of upper lateral-incisor agenesis. The patient had a Class I malocclusion with coincident midlines and a normal overbite and overjet. His profile was also normal, and his esthetic appearance was good except for a high smile line that resulted in excessive incisor display.

Fig. 6 Case 2. 10-year-old male patient with Class I malocclusion, missing upper lateral incisors, and excessive incisor display in smiling before treatment.
Cephalometric analysis showed a skeletal Class I malocclusion with a reduced divergence and a slight palatal inclination of the upper central incisors (Table 2). The overjet was 2mm; the overbite was 3mm.
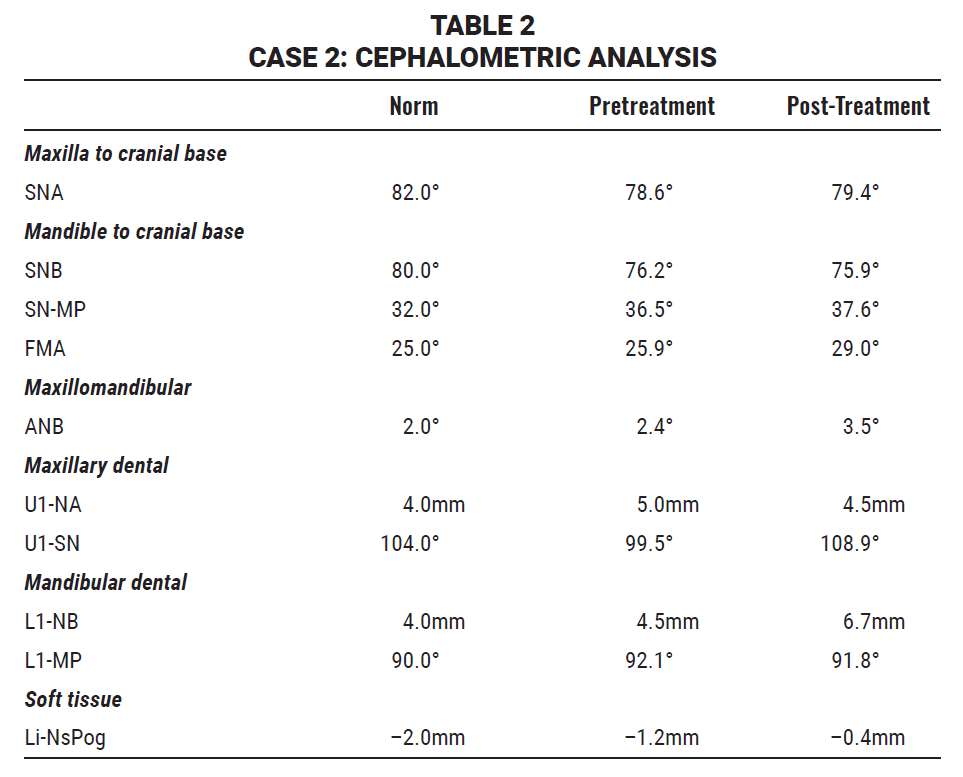
When the patient returned two years later for reevaluation, the upper deciduous lateral incisors and canines had exfoliated, and the permanent canines had erupted. A central diastema was evident, along with an excess of space around the permanent canines.
Treatment goals were to resolve the diastema by closing space in the maxillary anterior area and to properly incline the upper central incisors. Skeletal anchorage was planned, using a miniscrew between the upper central incisors.
The patient first underwent interceptive orthodontic treatment with a fixed palatal expander. After 30 days of expansion, .022" Roth-prescription Empower self-ligating brackets were bonded in both arches (Fig. 7).

Fig. 7 Case 2. After 30 days of rapid palatal expansion, .022" Roth-prescription Empower self-ligating brackets bonded in both arches, with 016" × .022" nickel titanium archwire in upper arch and .014" gold archwire in lower arch; 1.4mm × 8mm miniscrew inserted between upper central incisors and connected to upper first premolars with elastomeric chain.
A 1.4mm × 8mm miniscrew was inserted between the upper central incisors under local anesthesia. The miniscrew was connected to the upper first premolars with elastomeric chain, to be changed once per month. After five months, a new chain was attached to the second molars (Fig. 8).
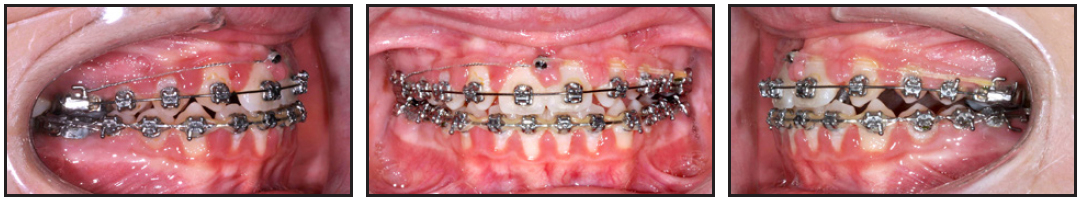
Fig. 8 Case 2. After six months of treatment, elastomeric chain attached from miniscrew to upper second molars.
The wire sequence for the upper arch progressed from .016" × .022" nickel titanium to .017" × .025" nickel titanium, .018" × .025" nickel titanium, .018" × .025" stainless steel, and .016" gold. In the lower arch, the sequence involved .014" gold, .016" gold, .018" × .025" nickel titanium, and .021" × .028" stainless steel wires.
During the last phase of treatment, the patient was asked to wear short Class III elastics** at night only on the right side and full-time on the left. After a few months, he wore triangular intercuspation elastics on both sides to improve the occlusal contacts and stability.
Treatment time was three years (Fig. 9). Vacuformed retainers were fabricated and delivered. The upper anterior spaces and central diastema were closed, and the upper central-incisor inclination was corrected (Table 2). Both arches were properly leveled and aligned.
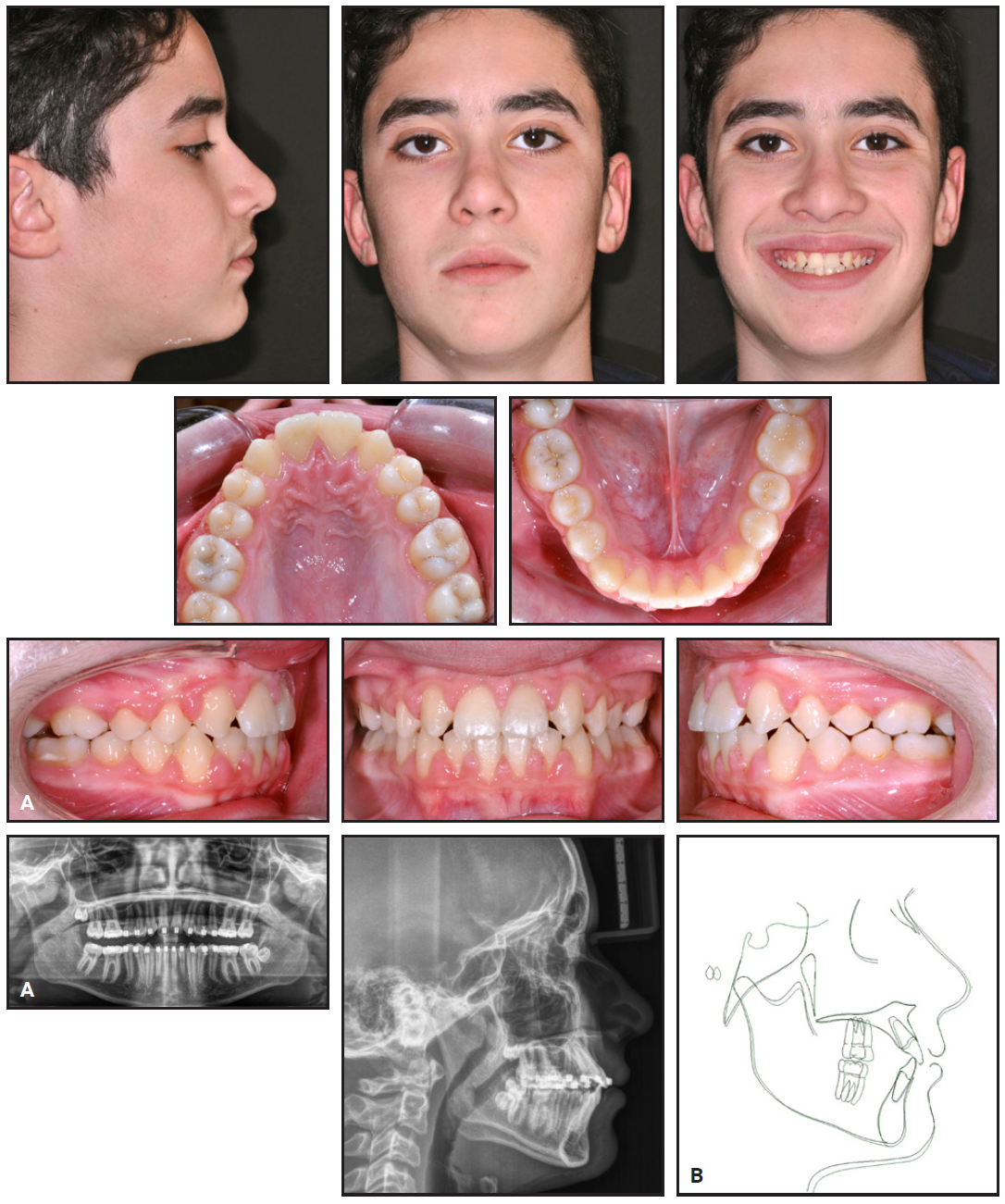
Fig. 9 Case 2. A. Patient after three years of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
Case 3
An 8-year-old female in the mixed dentition presented for treatment (Fig. 10). Her permanent first molars, upper and lower central incisors, and lower lateral incisors had erupted. A panoramic radiograph confirmed the diagnosis of upper lateral-incisor agenesis. The patient exhibited a Class I malocclusion with coincident midlines and a normal overbite and overjet. The upper arch had a triangular shape, and there was mild crowding in both arches. The patient had a normal profile with good esthetics.

Fig. 10 Case 3. 8-year-old female patient with Class I relationship, mild crowding in both arches, and missing upper lateral incisors before treatment.
Cephalometric analysis revealed a skeletal Class I malocclusion with increased divergence and a slight buccal inclination of the lower central incisors (Table 3). The overjet and overbite were within the normal range.
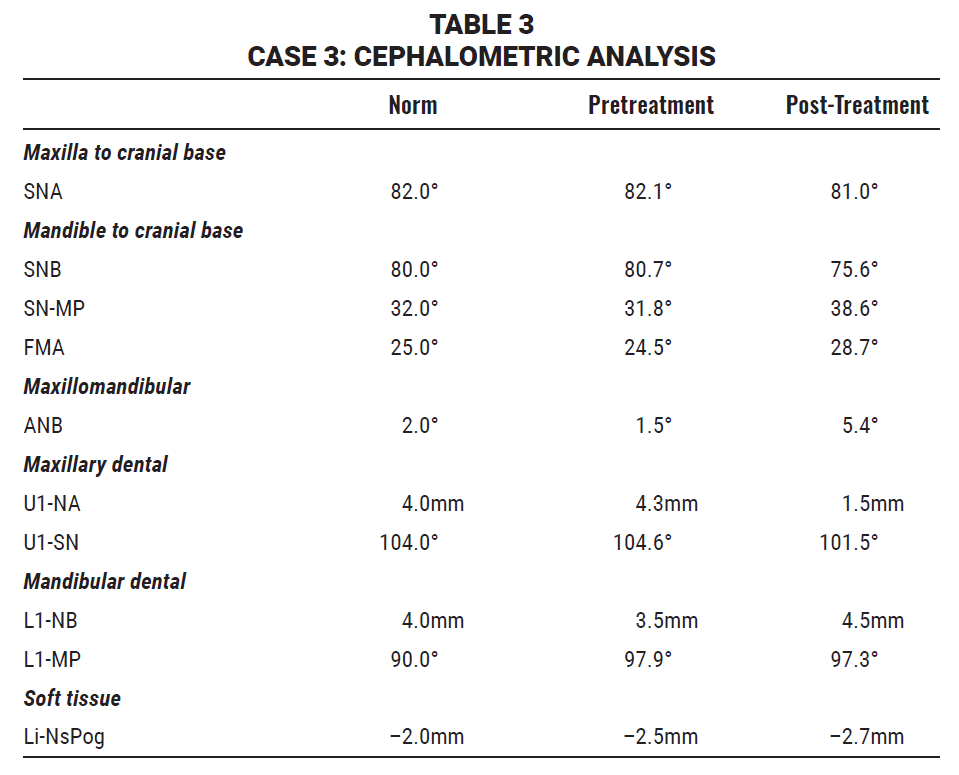
The treatment goal was to close spaces by protracting the upper posterior teeth and substituting the canines bilaterally. The challenge in treatment planning was to achieve protraction without losing torque on the upper incisors.
After 30 days of rapid maxillary expansion, .022" Roth-prescription Empower self-ligating brackets were bonded, and the diastema was maintained (Fig. 11).

Fig. 11 Case 3. After 30 days of palatal expansion, .022" Roth-prescription Empower self-ligating brackets bonded in both arches, with 016" × .022" nickel titanium archwire in upper arch and .014" gold archwire in lower arch; 1.4mm × 8mm miniscrew inserted between upper central incisors and connected to upper left canine with elastomeric chain.
Under local anesthesia, a 1.4mm × 8mm miniscrew was inserted between the upper central incisors. The miniscrew was connected to the upper left canine with an elastomeric chain, which was changed once per month. Five months later, the elastomeric chain was extended to incorporate both the canine and the first premolar (Fig. 12). Once the upper right canine erupted and a bracket could be positioned, the same pattern was used on the right side.

Fig. 12 Case 3. After six months of treatment, elastomeric chain extended from upper left canine to first premolar.
The archwire sequence in the upper arch progressed from .016" × .022" nickel titanium to .017" × .025" nickel titanium, .018" × .025" nickel titanium, and .018" × .025" stainless steel. In the lower arch, the archwire sequence progressed from .014" gold to .016" gold to .018" × .025" nickel titanium and .018" × .025" twisted stainless steel.
In the final stage of treatment, the patient was asked to wear short Class III elastics daily. After a few months, the elastics were changed to triangular intercuspation elastics to improve the occlusal contacts and stability.
Total treatment time was 21 months (Fig. 13, Table 3). Vacuformed retainers were delivered. The patient’s maxillary spaces were closed, the upper central-incisor torque was improved, and the midlines were coincident. Both arches were leveled and aligned, and the patient’s smile was esthetically improved.
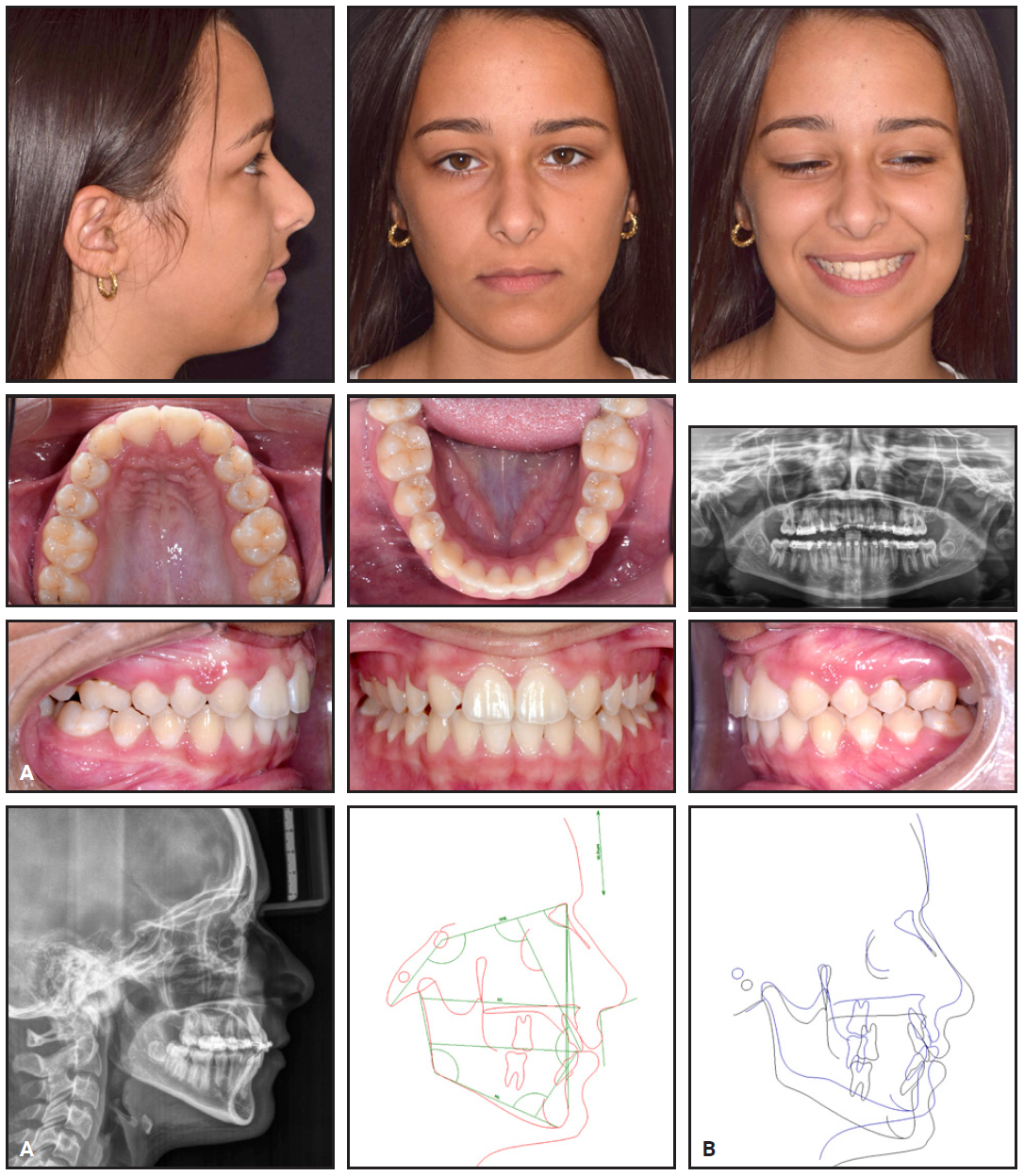
Fig. 13 Case 3. A. Patient after 21 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
Discussion
Treatment planning for a patient with upper lateral-incisor agenesis involves a number of aspects, including the patient’s periodontal biotype, local anatomy, esthetic demands, economic situation, and sociopsychological status.10-13 If a space-opening approach is chosen, the subsequent implant placement may require two surgeries, since a bone-graft procedure may be needed to enhance the buccopalatal thickness before the implant insertion.5,6 Another consideration is the potential esthetic failure of an implant in the smile zone.
In a recent study, orthodontic space closure and space opening for implant replacement produced similar esthetic results.14 Infraocclusion was evident in the implant patients, however, and the patients treated with space closure showed better periodontal health. Space closure does require careful anchorage management and biomechanical planning.15,16 TADs can be useful in many cases to overcome the limitations of traditional techniques and to reduce the dependence on patient compliance.7-9,17-19
The main difficulty in these cases is the loss of torque control on the maxillary central incisors from the use of elastic chain, particularly if the patient is noncompliant with Class III elastics.20-23 There is also a risk of damage to the buccal mucosa from the chains. A Mesialslider anchored by two or more palatal miniscrews is a reliable alternative for anterior space closure with more efficient torque control.24,25 This technique involves precise planning with cone-beam computed tomography and fabrication by a laboratory, however, and the clinical management can be challenging. A single buccal miniscrew is simpler and less expensive, and it can be considered even in mixed-dentition patients. Nevertheless, it should be reserved for patients with lower smile lines, so that the upper lip covers the miniscrew.26
Case 1 was complicated by a periodontal defect in the anterior region. Li and colleagues found that sites with bone defects are at a higher risk of periodontitis progression in patients who do not receive periodontal therapy.27 Treatment options for such a tooth include retention after periodontal treatment or extraction followed by prosthetic restoration.27-29
FOOTNOTES
- *Biocoral, Saint-Gonnéry, France; www.biocoral.com.
- **Registered trademark of American Orthodontics, Sheboygan, WI; www.americanortho.com.
- ***MAS Osstem Implant Co., Seoul, South Korea; en.osstem.com.
REFERENCES
- 1. Kavadia, S.; Papadiochou, S.; Papadiochos, I.; and Zafiriadis, L.: Agenesis of maxillary lateral incisors: A global overview of the clinical problem, Orthod. (Chic.) 12:296-317, 2011.
- 2. Andrade, D.C.; Loureiro, C.A.; Araújo, V.E.; Riera, R.; and Atallah, A.N.: Treatment for agenesis of maxillary lateral incisors: A systematic review, Orthod. Craniofac. Res. 16:129-136, 2013.
- 3. Bassiouny, D.S.; Afify, A.R.; Baeshen, H.A.; Birkhed, D.; and Zawawi, K.H.: Prevalence of maxillary lateral incisor agenesis and associated skeletal characteristics in an orthodontic patient population, Acta Odontol. Scand. 74:456-459, 2016.
- 4. Celikoglu, M.; Kamak, H.; Yildirim, H.; and Ceylan I.: Investigation of the maxillary lateral incisor agenesis and associated dental anomalies in an orthodontic patient population, Med. Oral Patol. Oral Cir. Bucal 17:e1068-e1073, 2012.
- 5. Kiliaridis, S.; Sidira, M.; Kirmanidou, Y.; and Michalakis, K.: Treatment options for congenitally missing lateral incisors, J. Oral Implantol. 9 suppl. 1:S5-S24, 2016.
- 6. Qadri, S.; Parkin, N.A.; and Benson, P.E.: Space closing versus space opening for bilateral missing upper laterals—aesthetic judgments of laypeople: A web-based survey, J. Orthod. 43:137- 146, 2016.
- 7. Chang, H.P. and Tseng, Y.C.: Miniscrew implant applications in contemporary orthodontics, Kaohsiung J. Med. Sci. 30:111-115, 2014.
- 8. Jasoria, G.; Shamim, W.; Rathore, S.; Kalra, A.; Manchanda, M.; and Jaggi, N.: Miniscrew implants as temporary anchorage devices in orthodontics: A comprehensive review, J. Contemp. Dent. Pract. 14:993-999, 2013.
- 9. Creekmore, T.D. and Eklund, M.K.: The possibility of skeletal anchorage, J. Clin. Orthod. 17:266-269, 1983.
- 10. De Molon, R.S.; Kim, Y.J.; Dos Santos-Pinto, A.; and Cirelli, J.A.: Improvement of an anterior infrabone defect using combined periodontal and orthodontic therapy: A 6-year follow-up case report, Eur. J. Dent. 8:407-411, 2014.
- 11. Zasciurinskiene, E.; Lindsten, R.; Slotte, C.; and Bjerklin, K.: Orthodontic treatment in periodontitis-susceptible subjects: A systematic literature review, Clin. Exp. Dent. Res. 2:162-173, 2016.
- 12. Eliasson, L.A.; Hugoson, A.; Kurol, J.; and Siwe, H.: The effects of orthodontic treatment on periodontal tissues in patient with reduced periodontal support, Eur. J. Orthod. 4:1-9, 1982.
- 13. Javaheri, H.H.: The side effects of orthodontic mechanics in orthodontic treatments, Int. J. Orthod. Milw. 19:11-12, 2008.
- 14. Jamilian, A.; Perillo, L.; and Rosa, M.: Missing upper incisors: A retrospective study of orthodontic space closure versus implant, Prog. Othod. 16:2, 2015.
- 15. Rosa, M. and Zachrisson, B.U.: Missing maxillary lateral incisors: New procedures and indications for optimal space closure, in Esthetics and Biomechanics in Orthodontics, 2nd ed., ed. R. Nanda, Elsevier Saunders, St. Louis, 2014, pp. 528-559.
- 16. Ludwig, B.; Zachrisson, B.U.; and Rosa, M.: Non-compliance space closure in patients with missing maxillary lateral incisors, J. Clin. Orthod. 47:180-187, 2013.
- 17. Migliorati, M.; Drago, S.; Schiavetti, I.; Olivero, F.; Barberis, F.; Lagazzo, A.; Capurro, M.; Silvestrini-Biavati, A.; and Benedicenti, S.: Orthodontic miniscrews: An experimental campaignon primary stability and bone properties, Eur. J. Orthod. 37:531-538, 2015.
- 18. Migliorati, M.; Benedicenti, S.; Signori, A.; Drago, S.; Barberis, F.; Tournier, H.; and Silvestrini-Biavati, A.: Miniscrew design and bone characteristics: An experimental study of primary stability, Am. J. Orthod. 142:228-234, 2012.
- 19. Manni, A.; Cozzani, M.; Tamborrino, F.; De Rinaldis, S.; and Menini, A.: Factors influencing the stability of miniscrews: A retrospective study on 300 miniscrews, Eur. J. Orthod. 33:388-395, 2011.
- 20. Proffit, W.R.; Fields, H.W. Jr.; and Sarver, D.M.: Contemporary Orthodontics, 5th ed., Mosby Elsevier, St. Louis, 2013, p. 585.
- 21. Tsomos, G.; Ludwig, B.; Grossen, J.; Pazera, P.; and Gkantidis, N.: Objective assessment of patient compliance with removable orthodontic appliances: A cross-sectional cohort study, Angle Orthod. 84:56-61, 2014.
- 22. Nel, W.R. and Dawjee, S.M.: Compliance and satisfaction in the orthodontic patient, SADJ 67:452-456, 2012.
- 23. Veeroo, H.J.; Cunningham, S.J.; Newton, J.T.; and Travess, H.C.: Motivation and compliance with intraoral elastics, Am. J. Orthod. 146:33-39, 2014.
- 24. Wilmes, B.; Nienkemper, M.; Nanda, R.; Lübberink, G.; and Drescher, D.: Palatally anchored maxillary molar mesialization using the mesialslider, J. Clin. Orthod. 47:172-179, 2013.
- 25. Wilmes, B.; Schwarze, J.; Vasudavan, S.; and Drescher, D.: Maxillary space closure using aligners and palatal mini-implants in patients with congenitally missing lateral incisors, J. Clin. Orthod. 55:20-33, 2021.
- 26. Kasim, S.A.V.; Bharadwaj, R.; and Kasim, N.A.V.: Simple and secure ligation technique for anterior intrusion using a miniscrew, J. Clin. Orthod. 54:121-122, 2020.
- 27. Li, Y.; Xu, L.; Zhou, Y.H.; Ouyang, X.Y.; and Cao, T.: Combination of periodontal, orthodontic and endodontic therapy in upper anterior teeth with hopeless prognosis and longtime follow-up: A case report, J. Pek. Univ. Health Sci. 49:740-744, 2017.
- 28. Derton, N.; Derton, R.; Perini, A.; Gracco, A.; and Fornaciari, P.A.: Orthodontic treatment in periodontal patients: A case report with 7 years follow-up, Int. Orthod. 9:92-109, 2011.
- 29. Cao, T.; Xu, L.; Shi, J.; and Zhou, Y.: Combined orthodontic-periodontal treatment in periodontal patients with anteriorly displaced incisors, Am. J. Orthod. 148:805-813, 2015.







COMMENTS
.