CASE REPORT
Compensatory Treatment of a Complex Class III Malocclusion
Class III malocclusions are characterized by anteroposterior dental discrepancies, with or without a skeletal component. The facial aspect is usually compromised, and it is precisely this factor that most often motivates a patient to seek treatment.1
Treatment of a Class III skeletal discrepancy in adolescence or adulthood often involves orthognathic surgery or compensatory orthodontic therapy that may include extractions, depending on the severity of bone discrepancy as well as on patient expectations and cooperation.2 Although many patients decline surgery, recent technological advances in the use of thermoactivated and superelastic wires and skeletal anchorage have enabled simpler compensatory orthodontic treatment without extractions.3,4
One example of such treatment is mandibular arch retraction supported by temporary microscrews, which has proven effective in treating Class III malocclusions with predictable force application.5,6 When more significant tooth movements are permitted by the patient’s bone anatomy, the profile can be significantly improved, even by conservative orthodontic treatment that has little effect on the face.3 Superelastic archwires in low-friction appliances can resolve dental crowding by means of relatively low forces (under favorable periodontal and dental conditions). Several authors have shown that the arch perimeter can be increased, when indicated, to assist with leveling and alignment through buccal expansion.7,8 With careful diagnosis, this protocol can simplify treatment and reduce the risks involved in the complete correction of anteroposterior bone discrepancies,3-5 as the following case demonstrates.
Diagnosis and Treatment Planning
Similar articles from the archive:
- CASE REPORT Nonsurgical Treatment of an Adult Skeletal Class III Patient with Compensated Dentition November 2021
- CASE REPORT Retreatment of a Skeletal Class III Malocclusion Using Mandibular Extra-Alveolar Mini-Implants September 2021
- CASE REPORT Nonsurgical Correction of Class III Malocclusion and Anterior Open Bite with Mini-Implant Anchorage November 2018
A 15-year-old female with the chief complaints of an anterior crossbite and crowding was referred for orthodontic treatment. The patient had a Class III dental relationship, an anterior crossbite, ectopic canines, and a buccal crossbite on the left side (Fig. 1A).
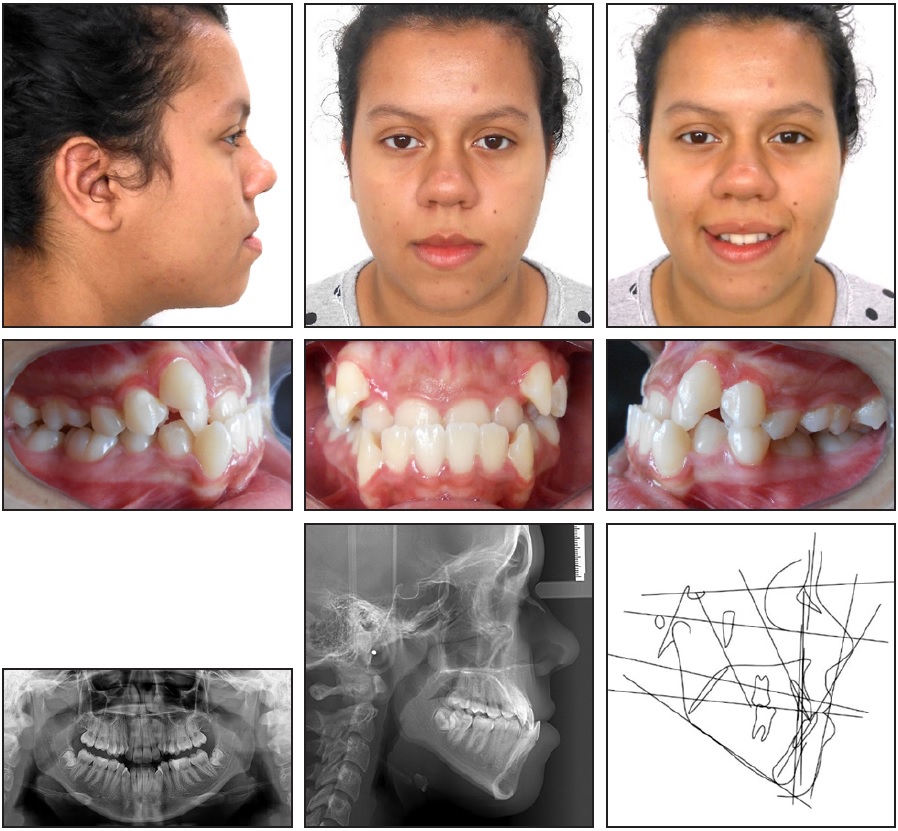
Fig. 1 15-year-old female patient with Class III dental relationship, anterior crossbite, ectopic canines, buccal crossbite on left side, and concave profile before treatment (continued in next image).
She exhibited a symmetrical face with a dolichofacial tendency and a concave profile with a strong chin projection. Intraoral examination found a negative overjet, a 4mm overbite, and edge-to-edge Class III molar relationships on both sides. The maxillary and mandibular arches displayed severe crowding (–13mm and –10mm, respectively) with a flat curve of Spee. The maxillary dental midline was coincident with the facial midline, but the mandibular dental midline was deviated 1mm to the left (Fig. 1B).
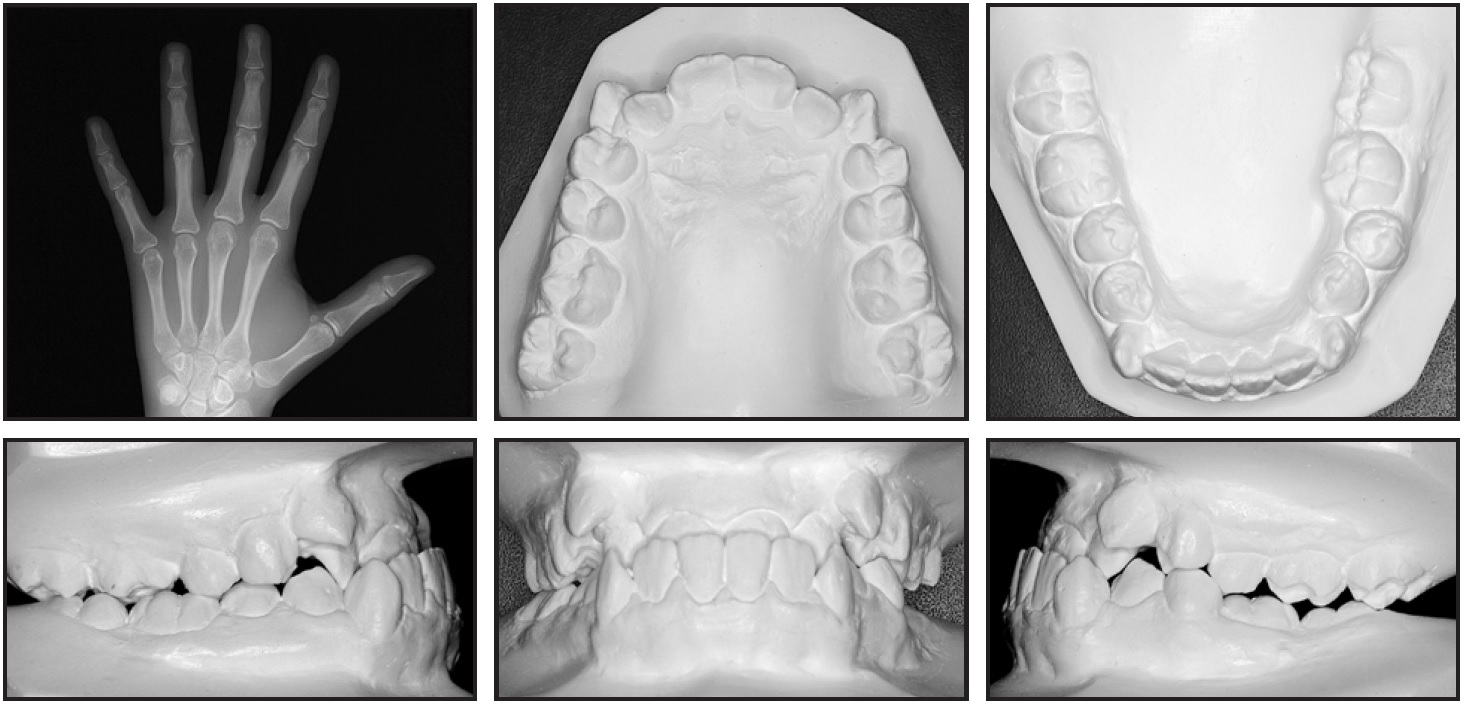
Fig. 1 (cont.) 15-year-old female patient with Class III dental relationship, anterior crossbite, ectopic canines, buccal crossbite on left side, and concave profile before treatment.
The patient had no TMD symptoms, including pain, restricted jaw movement, or joint noise. A functional shift caused by the anterior and posterior crossbites was detected when her mandible was guided into centric relation. The anterior crossbite persisted even in centric relation, although the incisors did reach an almost edge-to-edge position.
The panoramic radiograph showed the presence of all teeth except the upper third molars. A hand-and-wrist x-ray indicated that the patient was in her final stage of growth, with fusion of the epiphysis and metaphysis of the radius almost completed.9 Cephalometric analysis (Table 1) confirmed a skeletal Class III pattern (ANB = .37°, Wits appraisal = 0mm) with protrusive jaws (SNA = 83.94°, SNB = 83.57°) and a hyperdivergent growth pattern (SN-MP = 41.12°). The maxillary incisors were proclined (U1-NA = 25.05°), as were the mandibular incisors (IMPA = 85.71°).
Treatment objectives were to correct the anterior and posterior crossbites, thus reducing the facial concavity and eliminating the functional shift; establish Class I molar and canine relationships; obtain a normal overjet and overbite; relieve the upper and lower crowding; and improve facial and dental esthetics by establishing a harmonious smile and a stable occlusal relationship.
The first treatment option called for orthognathic surgery to set back the mandible with the possibility of maxillary protraction, followed by fixed appliances. This approach would allow correction of the skeletal discrepancy, optimization of facial and dental esthetics, and establishment of an ideal occlusion. A second option involved orthodontic treatment with premolar extractions and intermaxillary elastics, which could help camouflage some skeletal and dental aspects of the malocclusion, partially improving esthetics and achieving a functional occlusion.
The patient declined orthognathic surgery. Extraction of the lower first premolars to correct the negative overjet was contraindicated by the left buccal crossbite and narrow mandible. Maxillary extractions for correction of crowding without corresponding extractions in the mandibular arch would worsen the discrepancy. Therefore, we decided to treat the patient with nonextraction orthodontic therapy, supported by skeletal anchorage and dentoalveolar expansion, using the Biofunctional technique to overcome the anticipated side effects.
Treatment Progress
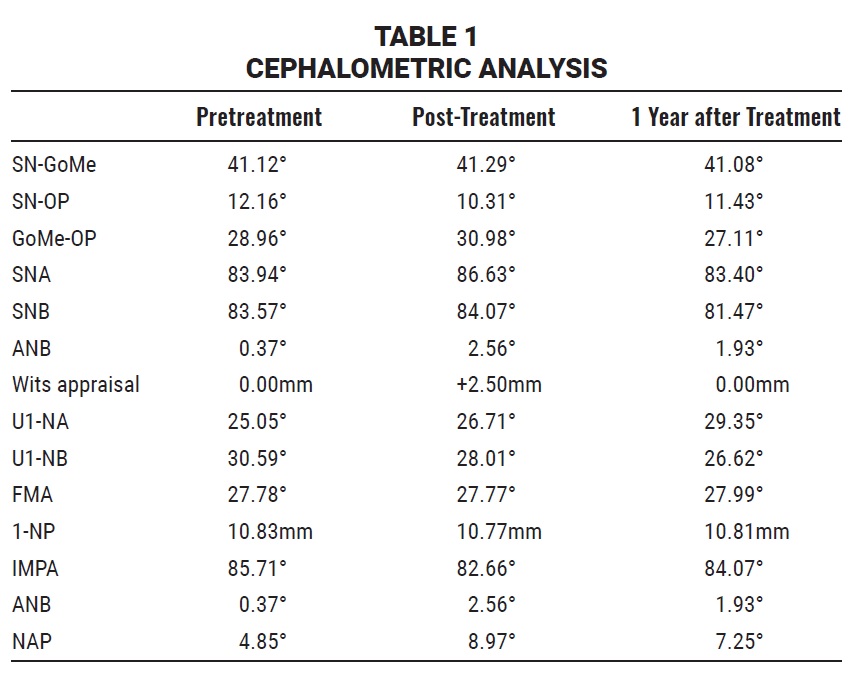
The lower third molars were extracted to allow mandibular posterior retraction. Upper MBT*-prescription passive self-ligating brackets were bonded, with the incisor brackets inverted to add buccal root torque. A light-cured acrylic bite ramp was placed over the lower incisors to allow the upper incisors to move buccally and thus correct the anterior crossbite (Fig. 2). The patient was asked to wear light Class III intermaxillary elastics to complement the anteroposterior correctional movement and criss-cross intermaxillary elastics to correct the left transverse relationship.
During leveling and alignment, the maxillary anterior teeth were moved buccally, supported by the canines, which were incorporated in the setup from the beginning, and by archwire stops placed mesial to the first-molar tubes. An omega loop was added mesial to the molar tubes to prevent wire slippage and help push the anterior teeth forward.10 One week after the start of leveling and alignment, the mandibular arch was bonded with the same appliance (Fig. 3). The archwire sequence in both arches included .014", .018", .014" × .025", and .018" × .025" nickel titanium.
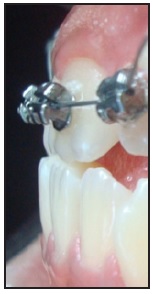
Fig. 2 Light-cured acrylic bite ramp placed on lingual surfaces of lower incisors to help correct anterior crossbite.

Fig. 3 Fixed appliance bonded in mandibular arch after one week of leveling and alignment.
After 14 months of treatment, 8mm × 2mm × 1.5mm extra-alveolar mini-implants were inserted into the right and left external oblique ridges, parallel to the long axes of the molars. Mandibular anterior retraction was initiated with the .014" × .025" nickel titanium archwire, using traction from elastomeric chains anchored to the microscrews.
After 19 months of treatment, a positive overjet and Class I canine relationship had been obtained. Finishing was carried out using .018" × .025" stainless steel archwires.
A lower 3-3 retainer was bonded, and a continuous upper Hawley appliance was delivered. Total treatment time was 34 months.
Treatment Results
A Class I molar relationship was achieved, while functional relationships were improved (Fig. 4). The enhanced soft-tissue harmony and esthetics resulted in a noticeable improvement in the patient’s smile attractiveness. Her Class III malocclusion was satisfactorily corrected, providing good intercuspation and an adequate overjet and overbite for both esthetics and function. Crowding was eliminated by maxillary and mandibular transverse expansion and maxillary anterior protrusion, thus improving the patient’s facial esthetics and profile.
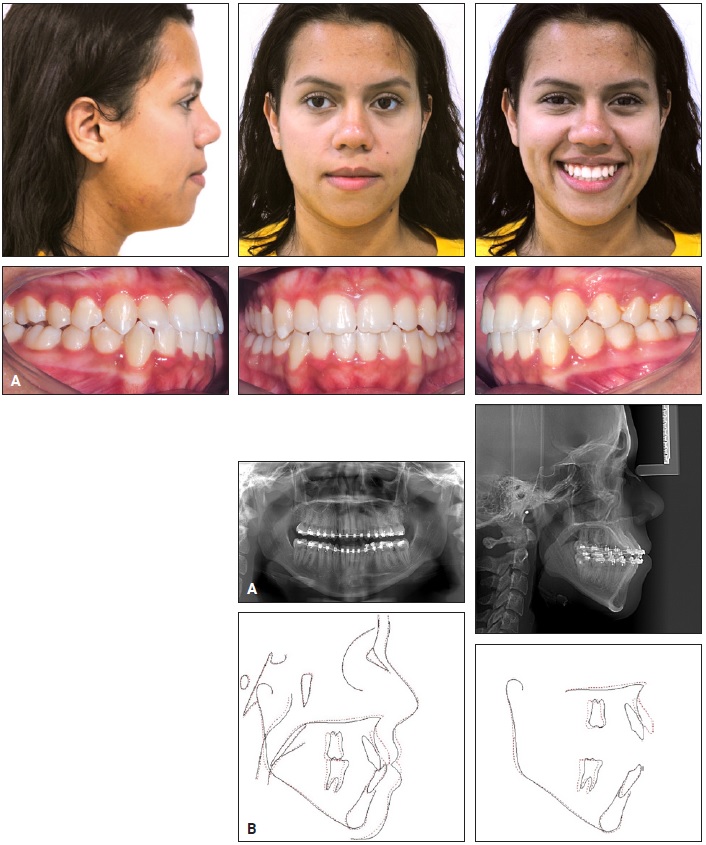
Fig. 4 A. Patient after 34 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
In the mandibular arch, anterior retraction was supported by the extra-alveolar mini-implants. The direction of traction produced a 1.85° counterclockwise rotation of the occlusal plane, promoting molar intrusion and incisor extrusion and thus reducing the vertical dimension. This rotational movement of the mandibular plane facilitated normalization of the overbite and restoration of the overjet, while the expected worsening of the anteroposterior relationship was counteracted by the anterior retraction. The posterior crossbite in the premolar region was corrected by patient collaboration in the use of intermaxillary elastics.
One year after treatment, the results remained stable (Fig. 5).

Fig. 5 Patient one year after treatment.
Discussion
Compensatory orthodontic treatment of Class III malocclusion is indicated when the jaw discrepancy is mild to moderate and the face has acceptable esthetics. Even in young adult patients with more severe dental discrepancies, however, the chances of success are now increasing, thanks to the availability of skeletal anchorage for significant tooth movement.11,12
The failure rate for mini-implants is relatively low, affecting only 7% of patients.11 The sites most commonly indicated for extra-alveolar microscrew insertion in the mandibular buccal shelf are between the first and second molars13-15 and at the distobuccal-cusp level of the lower second molars.16,17 In the present case, we chose to insert them distal to the second molars due to a lack of bone thickness between the first and second molars. This anchorage allowed efficient retraction of the entire mandibular arch and counterclockwise rotation of the occlusal plane to correct the overjet and overbite (Fig. 6). Because the direction of the retraction force is above the center of resistance of the basal bone, it produced molar intrusion simultaneously with the occlusal plane rotation.12,18,19 The lower incisors maintained a negative inclination, respecting the limits of the alveolar bone in the symphysis and establishing a functional and esthetic relationship with the upper incisors.
In the maxillary arch, compensatory treatment was accomplished primarily by maxillary and mandibular dentoalveolar expansion from a combination of superelastic wires and low-friction brackets. This transverse expansion, which occurs primarily through buccal tipping, was justified by the initial dental positions and favorable bone conditions. According to Maltagliati and colleagues, the technique is well suited for cases of dentoalveolar atresia, producing an average arch-space gain of 3-3.5mm in the premolar region.7 The use of heat-activated wires to increase the transverse dimensions of the dental arches is also supported by the literature.7,20-22
The buccal inclination of the upper incisors was a concern in this patient, considering the important role played by the upper incisors in facial harmony and smile esthetics.23 Our compensatory mechanics tended to increase the buccal inclination by tipping the crowns, thereby compromising the smile arc and causing relative incisor intrusion. In such a situation, lingual crown torque can be added to the rectangular wire to promote buccal root movement, or a negative torque prescription can be used. Since no negative-torque brackets for upper incisors are available on the market, we bonded the incisor brackets in inverted positions to apply lingual crown and buccal root torque (due to the play between wire and slot), thus promoting verticalization through greater root movement. We chose this protocol, called Biofunctional mechanics,24-26 based on a well-known partial loss of clinical expression of the torque prescription.23,27
Superimposition of the pre- and post-treatment cephalometric tracings showed that the premaxilla (point A) moved forward, as confirmed by the difference between the initial (83.94°) and final (86.63°) SNA angles (Table 1). The upper molars were also displaced distally, probably as a side effect of alignment with superelastic wires. The incorporation of negative torque in the upper anterior brackets may have promoted this advancement of point A as a consequence of root movement, with a potential compensatory remodeling of the alveolar bone. The approximation of the roots to the buccal cortical bone indicates the need for caution in such torque application. Studies are needed to confirm the degree of alveolar remodeling caused by bracket inversion in an alveolus affected by a skeletal condition, where it could be used to improve dental inclinations.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
- **Reprinted with permission from Marassi, C. and Marassi, C.: Orthodontic mini-implants assisting the anterior retraction phase, Dent. Press J. Orthod. 13:57-75, 2008.
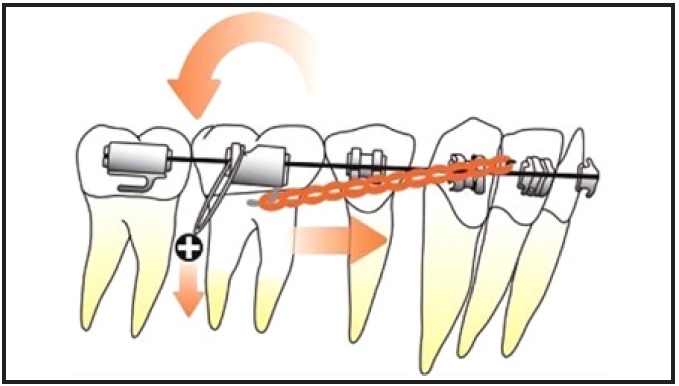
Fig. 6 Rotational movement of occlusal plane from retraction with skeletal anchorage and molar intrusion vector.**
REFERENCES
- 1. Bittencourt, M.A.V.: Angle Class III malocclusion with marked anteroposterior discrepancy, Dent. Press J. Orthod. 1:132-142, 2009.
- 2. Hakami, Z.; Chen, P.J.; Ahmida, A.; Janakiraman, N.; and Uribe, F.: Miniplate-aided mandibular dentition distalization as a camouflage treatment of a Class III malocclusion in an adult, Case Rep. Dent. 12:3542792, 2018.
- 3. Chen, K. and Cao, Y.: Class III malocclusion treated with distalization of the mandibular dentition with miniscrew anchorage: A 2-year follow-up, Am. J. Orthod. 148:1043-1053, 2015.
- 4. Marassi, C. and Marassi, C.: Mini-implant assisted anterior retraction, Dent. Press J. Orthod. 5:57-75, 2008.
- 5. Roberts, W.E.; Viecilli, R.F.; Chang, C.; Katona, T.R.; and Paydar, N.H.: Biology of biomechanics: Finite element analysis of a statically determinate system to rotate the occlusal plane for correction of a skeletal Class III open-bite malocclusion, Am. J. Orthod. 148:943-955, 2015.
- 6. Camci, H.; Doruk, C.; and Talay, B.: Treatment of midline deviation with miniscrews: A case report, Turk. J. Orthod. 2:56-60, 2017.
- 7. Maltagliati, L.A.; Myiahira, Y.I.; Fattori, L.; Capelozza Filho, L.; and Cardoso, M.: Transversal changes in dental arches from non-extraction treatment with self ligating brackets, Dent. Press J. Orthod. 3:39-45, 2013.
- 8. Atik, E.; Akarsu-Guven, B.; Kocadereli, I.; and Ciger, S.: Evaluation of maxillary arch dimensional and inclination changes with self-ligating and conventional brackets using broad archwires, Am. J. Orthod. 149:830-837, 2016.
- 9. Hägg, U. and Taranger, J.: Skeletal stages of the hand and wrist as indicators of the pubertal growth spurt, Acta Odontol. Scand. 38:187-200, 1980.
- 10. Roy, A.S.; Singh, G.K.; Tandon, P.; and Chaudhary, R.: Modified protrusion arch for anterior crossbite correction—a case report, Int. J. Orthod. Milwaukee 24:41-43, 2013.
- 11. Almeida, M.R.; Almeida, R.R.; and Chang, C.: Biomechanics of compensatory treatment of Class III malocclusion using extra-alveolar skeletal anchorage, Rev. Clin. Ortod. 15:74-86, 2016.
- 12. Chang, C.H.; Lin, J.S.Y; and Yeh, H.Y.: Extra-alveolar bone screws for conservative correction of severe malocclusion without extractions or orthognathic surgery, Curr. Osteoporos. Rep. 16:387-394, 2018.
- 13. Chang, C.; Huang, C.; and Roberts, W.E.: 3D cortical bone anatomy of the mandibular buccal shelf: A CBCT study to define sites for extra-alveolar bone screws to treat Class III malocclusion, Int. J. Orthod. Implantol. 41:74-82, 2016.
- 14. Chang, C. and Roberts, W.E.: A retrospective study of the extra-alveolar screw placement on buccal shelves, Int. J. Orthod. Implantol. 32:80-89, 2013.
- 15. Chang, C.; Lui, S.S.Y.; and Roberts, W.E.: Primary failure rate for 1680 extra-alveolar mandibular buccal shelf mini-screws placed in movable mucosa or attached gingiva, Angle Orthod. 85:905-910, 2015.
- 16. Elshebiny, T.; Palomo, J.M.; and Baumgaertel, S.: Anatomic assessment of the mandibular buccal shelf for miniscrew insertion in white patients, Am. J. Orthod. 153:505-511, 2018.
- 17. Nucera, R.; Lo Giudice, A.; Bellocchio, A.M.; Spinuzza, P.; Caprioglio, A.; Perillo, L.; Matarese, G.; and Cordasco, G.: Bone and cortical bone thickness of mandibular buccal shelf for miniscrew insertion in adults, Angle Orthod. 87:745-751, 2017.
- 18. Roberts, W.E.; Viecilli, R.F.; Chang, C.H.; Katona, T.R.; and Paydar, N.H.: Biology of biomechanics: Finite element analysis of a statically determinate system to rotate the occlusion plane for correction of a skeletal Class III open-bite malocclusion, Am. J. Orthod. 148:943-955, 2015.
- 19. Su, B.; Chang, C.H.; and Roberts, W.E.: Conservative management of a severe Class III open bite malocclusion, Int. J. Orthod. Implantol. 30:40-60, 2013.
- 20. Pandis, N.; Polychronopoulou, A.; and Eliades, T.: Self-ligating vs conventional brackets in the treatment of mandibular crowding: A prospective clinical trial of treatment duration and dental effects, Am. J. Orthod. 132:208-215, 2007.
- 21. Pandis, N.; Polychronopoulou, A.; Makou, M.; and Eliades, T.: Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets, Eur. J. Orthod. 32:248-253, 2010.
- 22. Cattaneo, P.M.; Treccani, M.; Carlsson, K.; Thorgeirsson, T.; Myrda, A.; Cevidanes, L.H.S.; and Melsen, B.: Transversal maxillary dento-alveolar changes in patients treated with active and passive self-ligating brackets: A randomized clinical trial using CBCT-scans and digital models, Orthod. Craniofac. Res. 14:222-233, 2011.
- 23. Jing, Y.; Han, X.; Guo, Y.; Li, J.; and Bai, D.: Nonsurgical correction of a Class III malocclusion in an adult by miniscrew-assisted mandibular dentition distalization, Am. J. Orthod. 143:877-887, 2013.
- 24. Valarelli, F.P.; Nascimento, F.E.C.; Batista, D.M.; Freitas, K.M.S.; and Cançado, R.H.: Class III camouflage treatment with the Biofunctional technique, J. Clin. Orthod. 52:351-358, 2018.
- 25. Janson, G.; de Souza, J.E.P.; Andrade Alves, F.; Andrade Jr., P.; Nakamura, A.; Freitas, M.R.; and Henriques, J.F.C.: Extreme dentoalveolar compensation in the treatment of Class III malocclusion, Am. J. Orthod. 128:787-794, 2005.
- 26. Janson, G.; de Souza, J.E.P.; Cavalcante Barros, S.E.; Andrade Jr., P.; and Nakamura, A.Y.: Orthodontic treatment alternative to a Class III subdivision malocclusion, J. Appl. Oral Sci. 17:354-363, 2009.
- 27. Maltagliati, L.A.: Torque expression of straightwire brackets: A realistic proposal for individualization, Ortho Science: Orthod. Sci. Prac. 31:364-371, 2015.




COMMENTS
.