Orthodontic treatment with the Invisalign* system has become more refined and complex over the past several years, thanks to the constant review and critique of treated cases by Align Technology and by experienced clinicians. One of the most challenging areas has been treatment involving the extraction of lower incisors or one, two, or four premolars. The following report shows a four-premolar extraction case treated exclusively with Invisalign, using no conventional fixed appliances.
Diagnosis and Treatment Planning
A 28-year-old male presented with a severe arch-length discrepancy that had produced severe upper and lower crowding and labially blocked-out canines (Fig. 1). He had a Class I molar relationship, with the upper and lower left first molars in crossbite. Cephalometric analysis showed a Class I, straight skeletal profile and normal incisor relationships.
Similar articles from the archive:
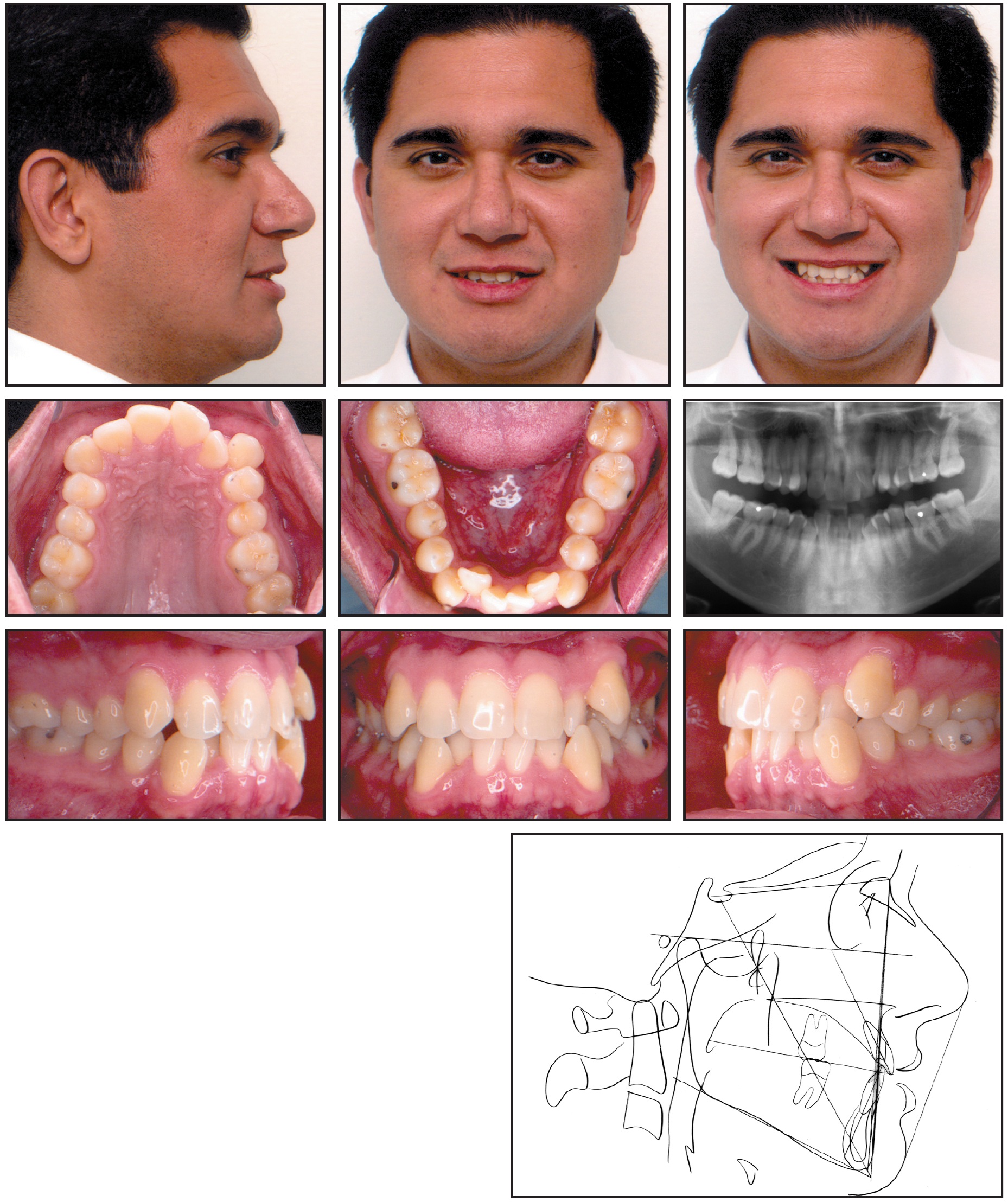
Fig. 1 28-year-old male with severe arch-length discrepancy before treatment.
A diagnostic cast setup was performed with the four first premolars removed to evaluate the projected alignment of the treated case, assuming that the teeth distal to the extraction sites would not move forward (Fig. 2). The setup confirmed that the patient could be treated with Invisalign.

Fig. 2 Diagnostic cast setup with four premolar extractions.
The computer-generated ClinCheck** setup, showing the type and placement of attachments, was reviewed, modified, and accepted (Fig. 3). Because the canines were mesially angulated, the ClinCheck technician was instructed to maintain their root angles throughout the retraction phase and not to upright the virtual images as the extraction spaces were closed. The case required 50 upper and 49 lower aligners; interproximal reduction was not indicated until the middle and later stages (21 and 48).
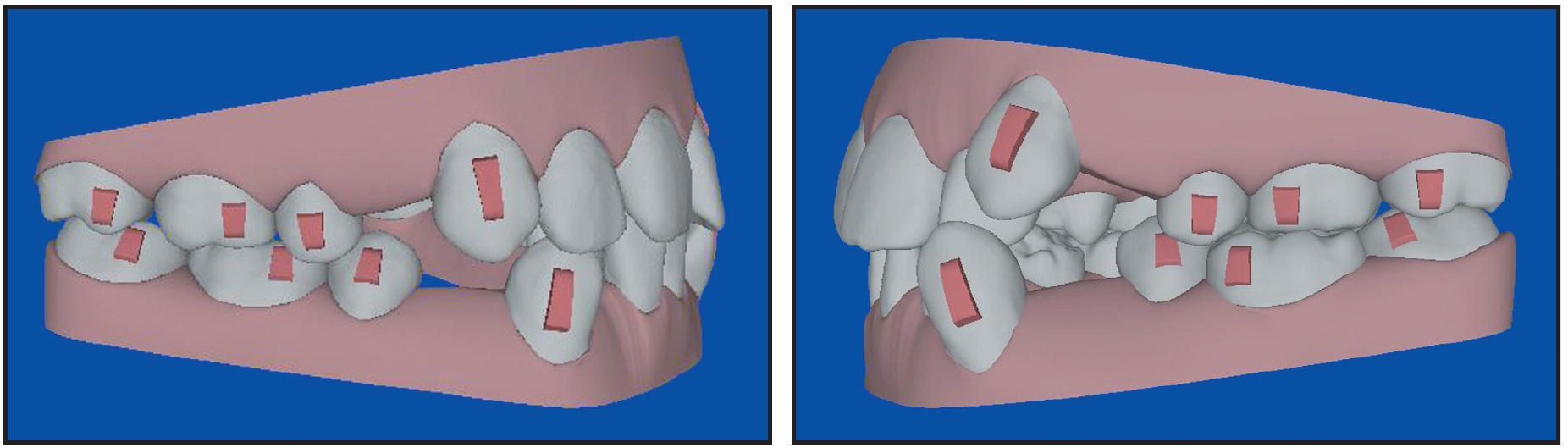
Fig. 3 Initial ClinCheck and attachments.
Treatment Progress
The patient was seen every eight to 12 weeks (four to six aligners) to check for aligner fit, attachment stability, and cooperation (Fig. 4A, Fig. 4B).
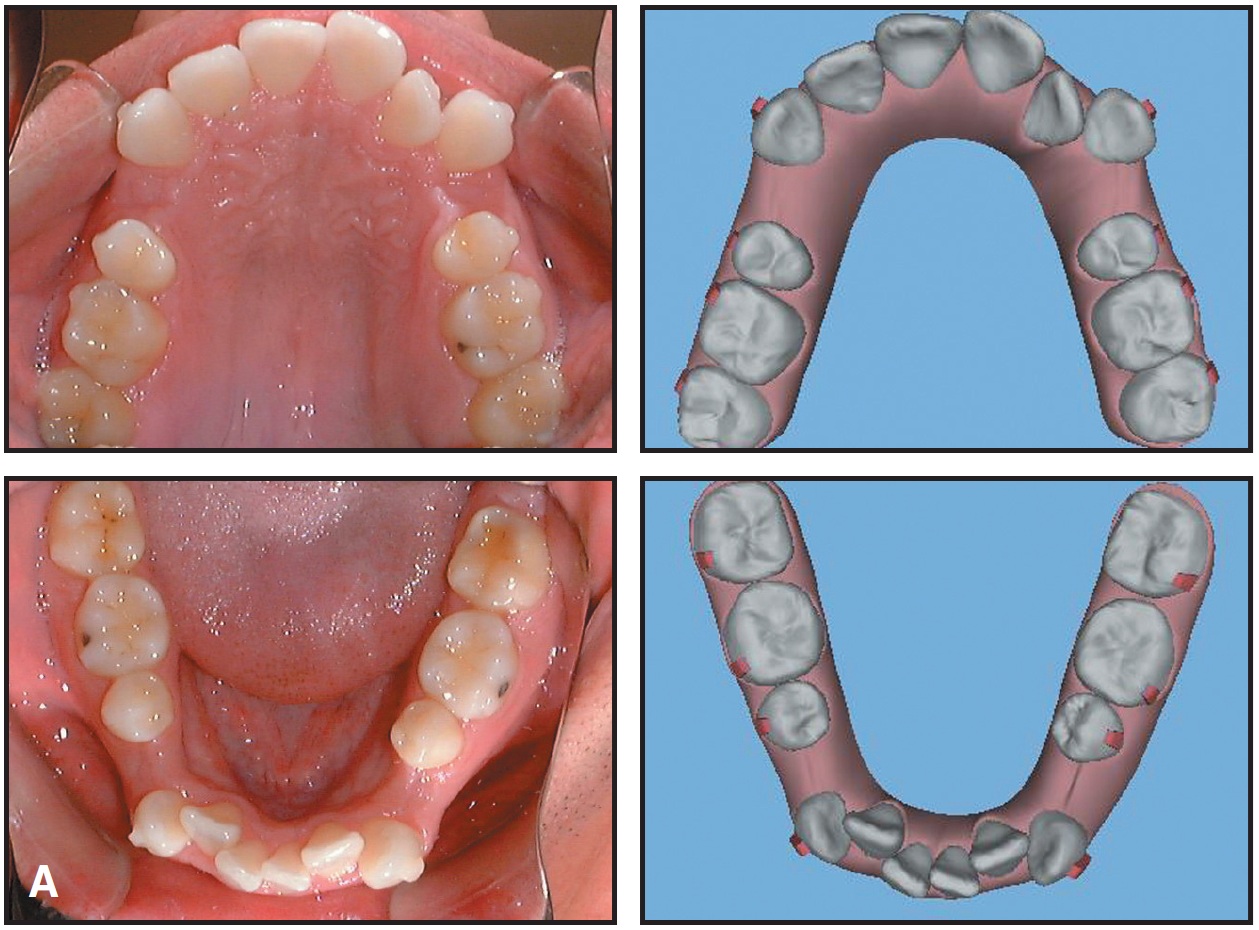
Fig. 4 A. Treatment progress compared to ClinCheck, Stage 10 (continued in next image).
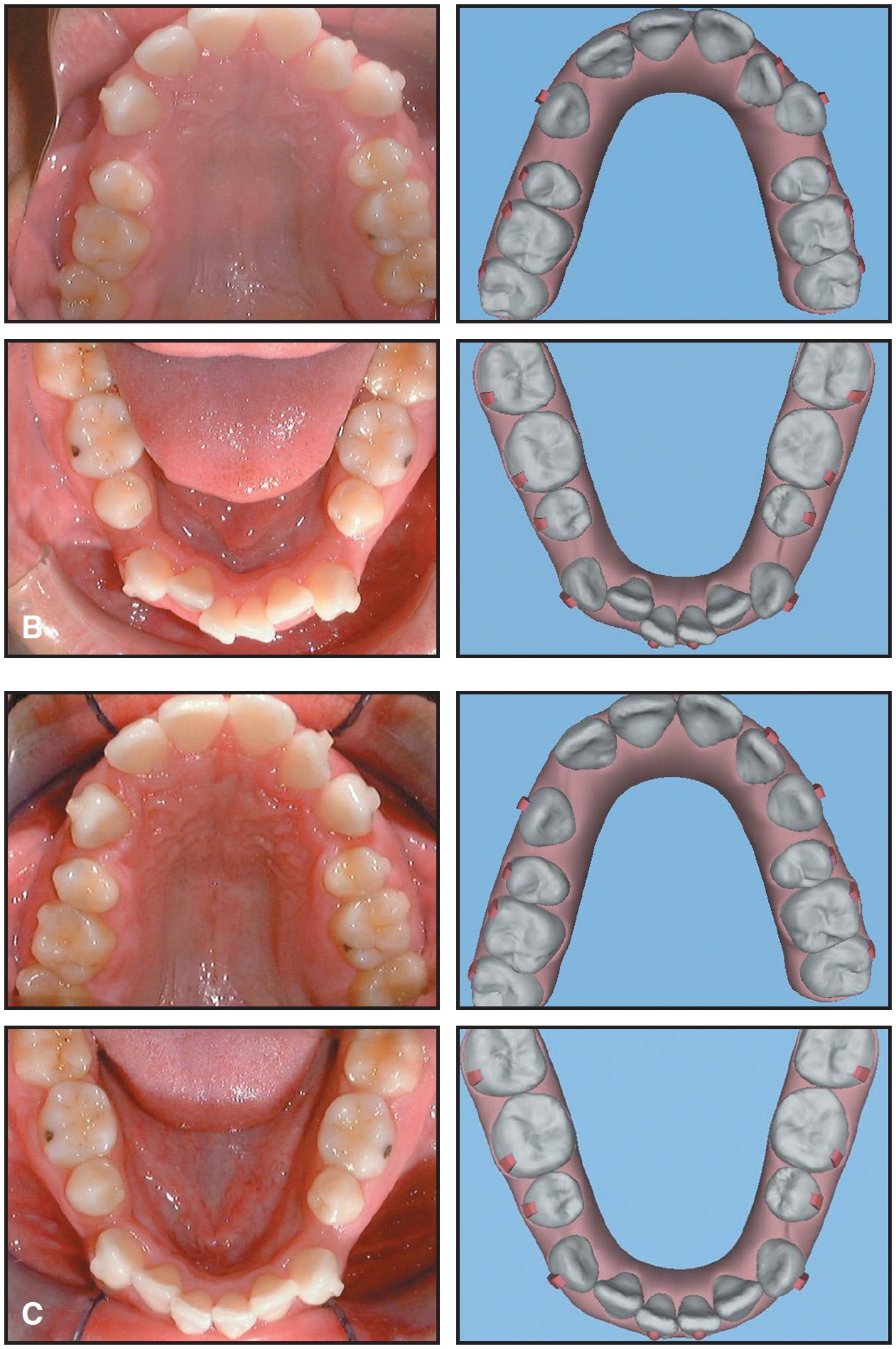
(cont.) B. Treatment progress compared to ClinCheck, Stage 20. C. Treatment progress compared to ClinCheck, Stage 28.
At these visits, I mark the attachments and then have the patient insert the aligners to confirm a positive connection between the "bumps" and the "bubbles" (Fig. 5).
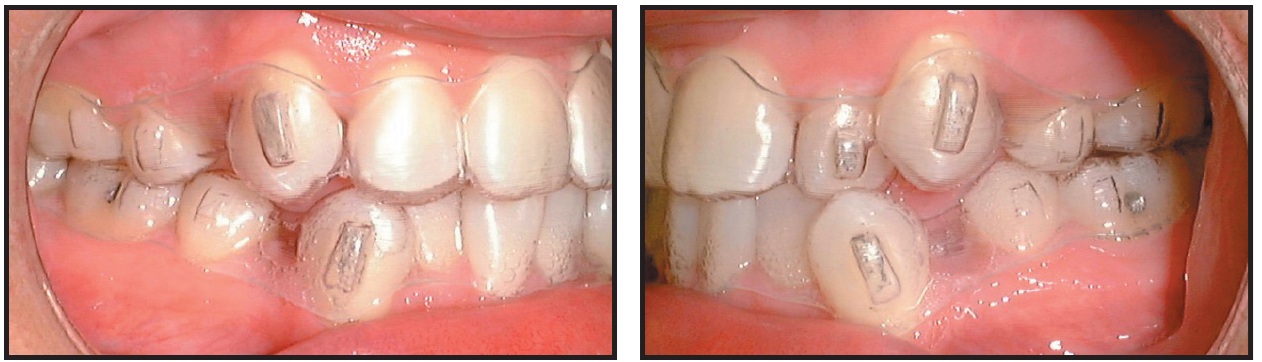
Fig. 5 Attachments marked to confirm positive connection with aligners.
Excellent patient compliance contributed significantly to the success of this case (Fig. 6).

Fig. 6 Excellent fit of aligners, demonstrating patient compliance. A. Stage 36. B. Stage 48.
Unfortunately, the lower right canine attachment debonded in the middle of treatment, resulting in several degrees of uprighting. When this was discovered, I elected to rebond the attachment and to continue treatment with the current aligner, knowing the canine root angulation would have to be addressed during the Case Refinement stage.
The initial aligner treatment took 24 months. I routinely take records at this point to determine what finishing and detailing will be required in Case Refinement. In the present case, I elected to keep the final aligners in place and to add power arms gingival to the upper and lower canines and buttons to the molars for the attachment of elastics (Fig. 7). These would be used to improve the canine root angulation.
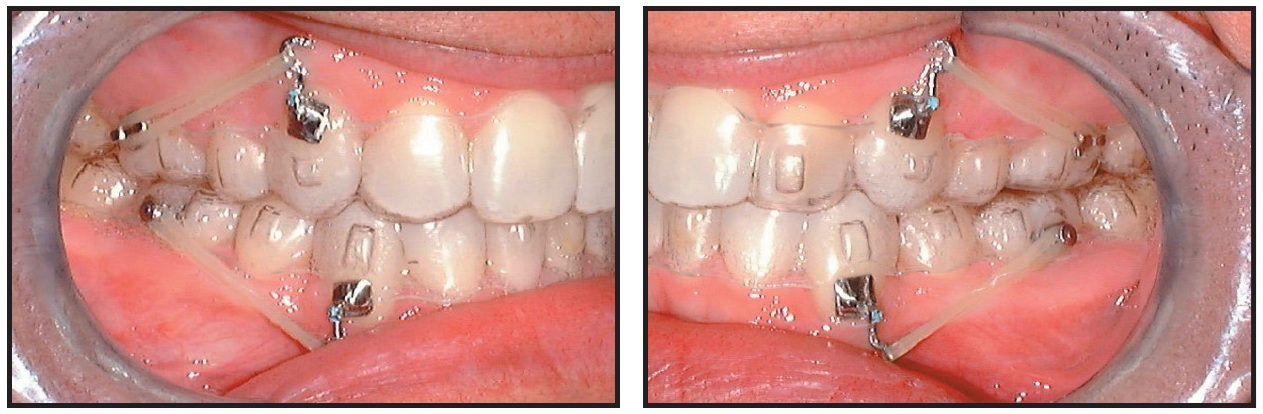
Fig. 7 Refinement of canine root angulation.
After four months of refinement, retainers were delivered.
Treatment Results
The final result showed good alignment and occlusion, with upright canines and ideal overbite and overjet (Fig. 8, Fig. 9).
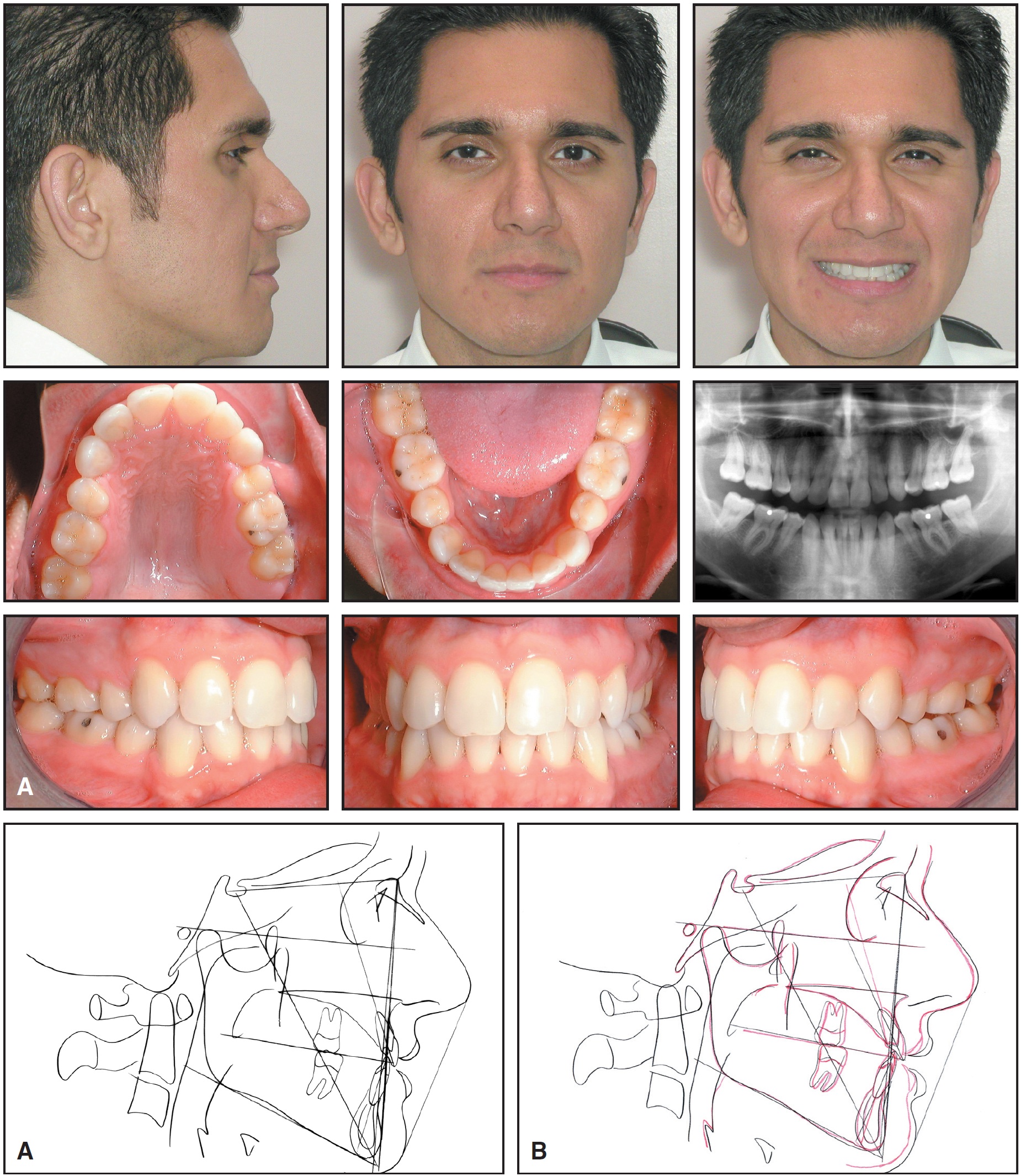
Fig. 8 A. Patient after 28 months of Invisalign treatment. B. Superimposition of cephalometric tracings before and after treatment.
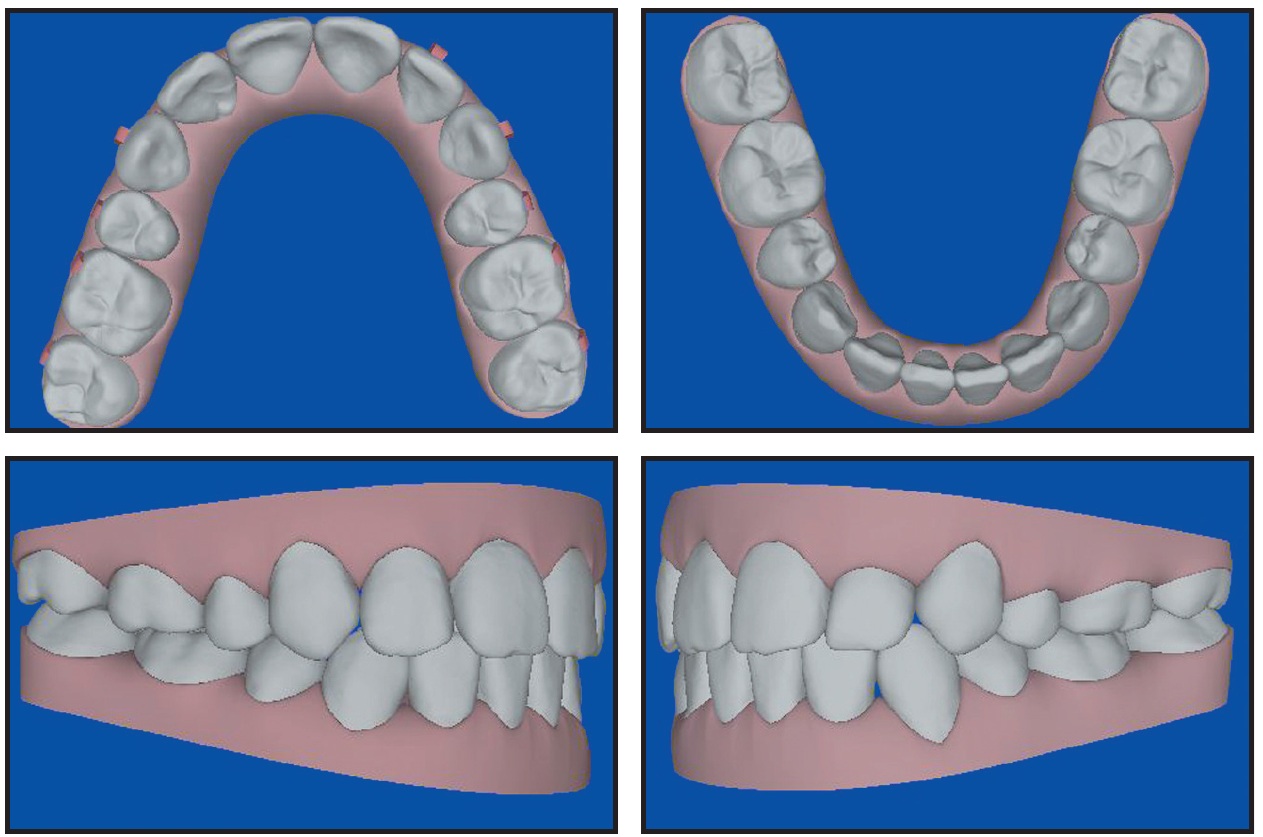
Fig. 9 Post-treatment ClinCheck projections.
Although the angulations of the canine roots were not perfect on the panoramic x-ray, they compared favorably with many published cases treated with fixed appliances. The lower right canine root angle was the least satisfactory due to the loss of its attachment in the middle of treatment. Had the patient been willing to continue with the refinement elastics, I believe additional improvement could have been achieved.
The upper left molar did not exhibit tight occlusion because the buccal cusps were worn down through attrition when the tooth was in crossbite before treatment. Restoring the anatomy of this tooth would enhance the occlusal fit with the lower molar.
If I were treating this case over, I would consider moving all the teeth at the same time in ClinCheck so that the canine movements would occur over the entire length of treatment. Smaller increments of movement in each stage would help keep the teeth tracking in the aligners. I would also consider placing miniscrew implants between the upper and lower molars and adding power-arm auxiliaries to the canines early in treatment, enabling the patient to wear elastics at night during the canine retraction stages. The power arms can be fabricated from clear plastic to make them more esthetic. The addition of elastic forces would have enhanced the root angle control, possibly to the point that additional refinement would not have been needed.
Discussion
There were several key issues in this case:
• This patient required minimal mesial movement of the posterior teeth. If 4-5mm of mesial movement is needed to close the extraction spaces, I use fixed appliances rather than the Invisalign system.
• Although I requested in ClinCheck that the canines not be uprighted as the extraction spaces were closed, they will always tend to upright as they are retracted. Maintaining the distal canine root angles in the virtual images is actually a form of overcorrection that will improve the canine root angulation at the end of treatment.
• Attachments are critical in extraction cases. In this patient, the posterior attachments were standard, but the canine attachments were 5mm long, 2mm wide, and 1mm thick. Because the gingival aspects of these attachments are not critical to mesiodistal movement, we recontour them into a "ski slope" shape, allowing the plastic to slide over the attachments when the patient removes the aligners. We also give Aligner Removal Tools*** to patients with multiple rectangular attachments.
• It is important to compare the clinical positions of the teeth with the ClinCheck images every six to 10 aligners. If the comparison is not within 10%, the clinician should stop treatment at that point and determine what must be done to get on track. This might mean going back to an aligner that fits and then repeating the succeeding ones. Or if tight contacts are keeping the teeth from moving, it might mean performing interproximal reduction earlier than planned. The doctor may also need to confront the patient about compliance at this stage. If nothing else works, a midcourse correction might be required. Whatever the choice, the clinician cannot continue to give the patient aligners that are fitting worse and worse.
• My procedure for either midcourse correction or Case Refinement is to remove all attachments, take new photos and polyvinyl siloxane impressions, complete the online treatment form, and send the case to Align Technology for a new ClinCheck. This ClinCheck can then be modified as necessary to accurately produce the finishing aligners, and new attachments can be placed where they are most needed--which may be on entirely different teeth than in the initial treatment.
• In my experience with more than 600 cases, the majority of problems are caused by lack of compliance. I instruct my Invisalign patients to wear the aligners 24 hours a day, except for eating and brushing. I emphasize that in my successful cases, the patients say that they wear them "all the time". More than half of my Invisalign patients are "orthodontic relapse" cases, who always state, without exception, that they "would never have metal braces again" and that "this time I am going to wear my retainers for the rest of my life". Excellent compliance during aligner treatment and indefinite retention are the keys to high-quality results that will be maintained over time.
Conclusion
This report demonstrates the capacity of the Invisalign system to treat a complex case requiring the removal of four first premolars. It is important to note that I did not start this treatment until I had already finished 275 Invisalign cases. It is the only case of this type that I have treated thus far, because I wanted to evaluate the process from beginning to end. Both the patient and I are highly pleased with the results.
REFERENCES
- 1. Boyd, R.L.; Miller, R.J.; and Vlaskalic, V.: The Invisalign system in adult orthodontics: Mild crowding and space closure cases, J. Clin. Orthod. 34:203-212, 2000.
- 2. Boyd, R.L. and Vlaskalic, V.: Three-dimensional diagnosis and orthodontic treatment of complex malocclusions with the Invisalign appliance, Semin. Orthod. 7:274-293, 2001.
- 3. Chenin, D.; Trosien, A.H.; Fong, P.F.; Miller, R.; and Lee, R.S.: Orthodontic treatment with a series of removable appliances, J. Am. Dent. Assoc. 134:1232-1239, 2003.
- 4. Womack, W.R.; Ahn, J.H.; Ammari, Z.; and Castillo, A.: A new approach to correction of crowding, Am. J. Orthod. 122:310-316, 2002.
- 5. Bishop, A.; Womack, W.R.; and Derakhshan, M.: An esthetic and removable orthodontic treatment option for patients: Invisalign, Dent. Assist. 71:14-17, 2002.
- 6. Miller, R.J.; Duong, T.T.: and Derakhshan, M.: Lower incisor extraction treatment with the Invisalign system, J. Clin. Orthod. 36:95-102, 2002.
- 7. Womack, R.: Clinical report, Clin. Rep. Tech. Invisalign 1:6-11, 2005.
- 8. Turatti, G.; Womack, R.; and Bracco, P.: Incisor intrusion with Invisalign treatment, J. Clin. Orthod. 40:171-174, 2006.


