Orthodontic Treatment of an Adult Patient with Cleft Lip and Palate
Orofacial clefts are the most common congenital malformations of the craniofacial region, with an average worldwide prevalence of 1 in 700 live births.1 Characterized by the lack of fusion of various embryological processes,2 they can be divided into four clinical types, according to their position relative to the incisive foramen:
preforaminal (cleft lip), postforaminal (cleft palate), transforaminal (cleft lip and palate), and, more rarely, fissures of the face. Clefts can be unilateral, bilateral, or midline, with unilateral clefts being the most common.3
Midfacial growth in untreated cleft lip and palate patients is similar to that in non-cleft patients. Most growth disturbances—particularly maxillary retrusion—result instead from surgical repair of the lip and palate.4 A skeletal growth deficiency can affect the dental arch, resulting in severe crowding, especially in the cleft area, and in anterior or posterior crossbite in association with a constricted maxilla.4,5 When the patient enters adolescence, the severity of the skeletal malocclusion may increase due to ongoing mandibular growth.6
Considering the effects of clefts on jaw growth, tooth development and alignment, and occlusion, which can contribute to problems with eating, speech, hearing, and self-image,7,8 cleft lip and palate treatment should always be coordinated with orthodontic therapy. This article describes the orthodontic treatment of a 20-year-old female with a surgically repaired unilateral transforaminal cleft.
Diagnosis and Treatment Plan
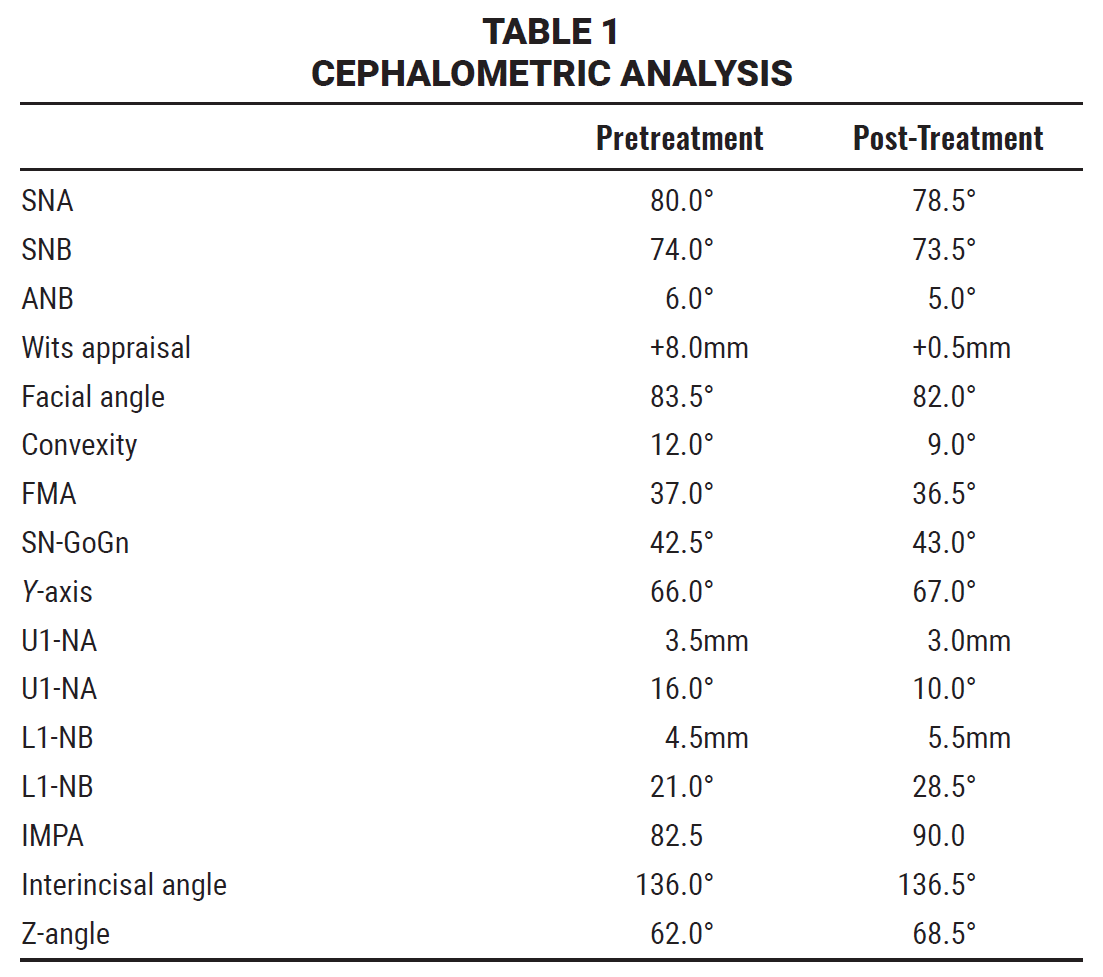
A 20-year-old female presented with the chief complaints of crowding and a constricted maxillary arch resulting from multiple surgeries to repair a unilateral cleft lip and palate on the left side (Fig. 1). A convex profile, facial asymmetry, and slight flattening of the left nostril were observed, along with a scar on the left side of the upper lip from the cleft repair and a fenestrated dental bridge replacing the upper left incisors. The patient exhibited a Class II, division 1 malocclusion with a constricted maxillary arch, bilateral posterior crossbite, and severe crowding.
Similar articles from the archive:
- OVERVIEW Orthodontic Management of Patients with Cleft Lip and Palate: Phase I Treatment April 2024
- CASE REPORT Nonsurgical Treatment of Anterior Crossbite in a Cleft Lip and Palate Patient Using a Fan-Type Rapid Palatal Expander and Fixed Appliances July 2023
- CASE REPORT Comprehensive Treatment of Severe Cleft Lip and Palate June 2019
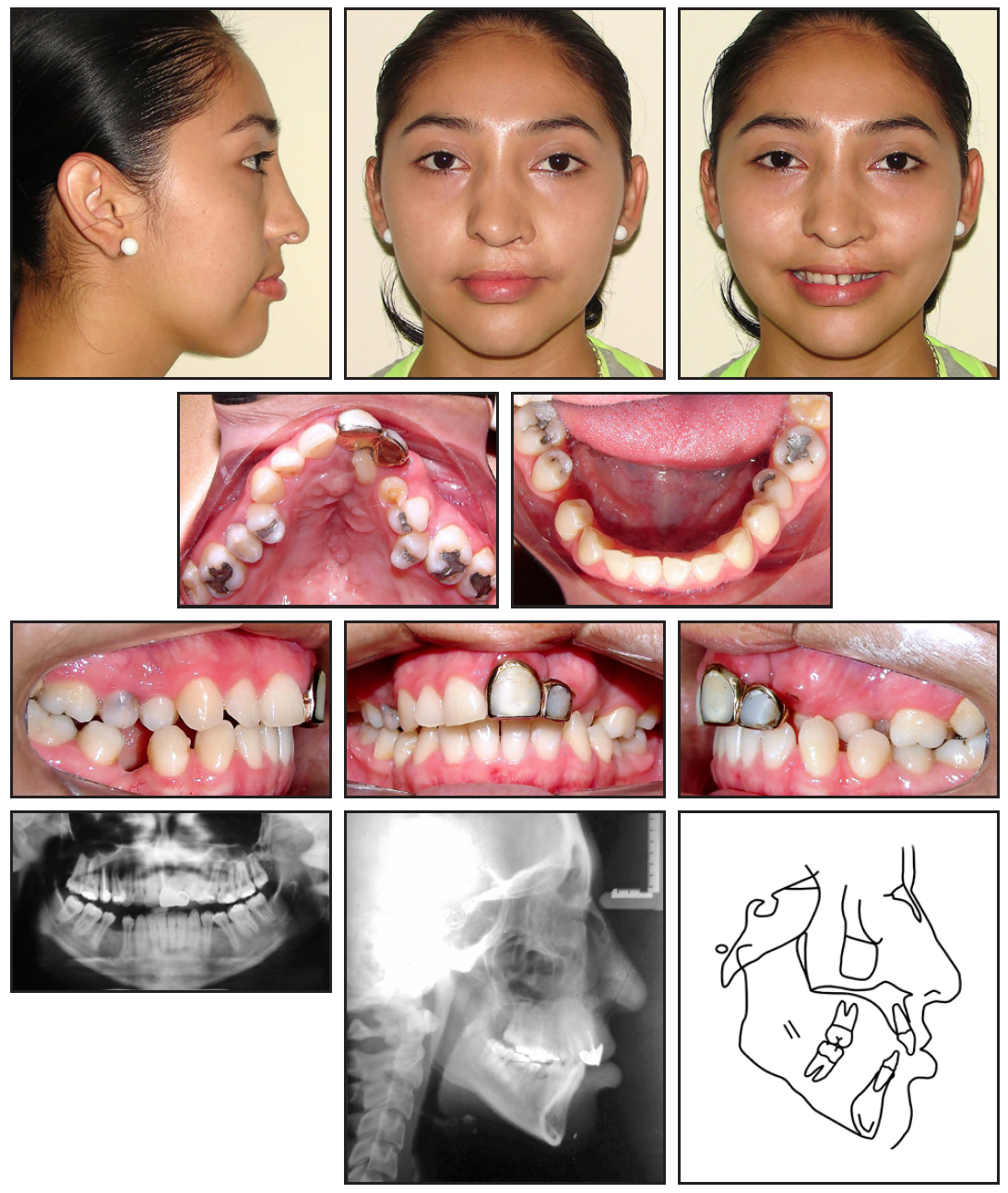
Fig. 1 20-year-old female patient with surgically closed unilateral transforaminal cleft, skeletal Class II relationship, constricted maxillary arch, missing upper left lateral incisor, and bilateral posterior crossbite before treatment.
The panoramic radiograph revealed the absence of the upper left lateral incisor and all third molars except the upper left. The upper left deciduous canine was retained, and the upper left permanent canine had erupted palatally.
Cephalometric analysis (Table 1) indicated a skeletal Class II relationship (ANB = 6°, Wits appraisal = +8mm) with a marked hyperdivergent growth pattern (SN-GoGn = 42.5°, FMA = 37°). The upper and lower incisors were retroclined (U1-NA = 16°, L1-NB = 21°), and the facial profile was convex (Z-angle = 62°).
Treatment objectives were to develop the transverse dimension of the upper arch, close the spaces in the lower arch, establish Class I relationships on the right side, and account for the missing upper left lateral incisor. Additional goals were to achieve adequate overjet and overbite and to improve the facial profile.
The treatment plan was to remove the fenestrated dental bridge, extract the upper left deciduous canine, and perform dentoalveolar expansion of the maxillary arch. Options for the missing upper left lateral incisor involved either space closure—in which the permanent canine would be moved into the lateral-incisor position and the first premolar into the canine position, leaving the left molars in a Class II relationship—or space opening to make room for an esthetic bridge. We elected the first option.
Treatment Progress
The dental bridge was removed, and a temporary crown was placed on the upper left central incisor. Both arches were bonded with MBT*-prescription .022" × .028" preadjusted brackets, with open-coil springs added to open space for the upper right first premolar and left second premolar.
Leveling and alignment were performed using .014", .016", .017" × .025", and .019" × .025" heat-activated nickel titanium archwires in both arches. During this stage, the upper left central-incisor bracket was repositioned more gingivally to promote extrusion and vertical bone growth,9,10 with the aim of leveling the gingival margins of the central incisors. The incisal edge of the upper left central incisor was progressively reduced to avoid premature contacts and a height discrepancy.
After about two years of treatment, the archwires were changed to .019" × .025" stainless steel for leveling and space closure. Medium Class II elastics (¼", 4.5oz) were worn full-time on the right side to achieve Class I molar and canine relationships, while light cross-elastics (1⁄8, 2.5oz) were also worn full-time on the right to reduce the lateral overjet ([img=2]Fig. 2[/img).

Fig. 2 After three years of treatment.
A palatal retainer was bonded from the upper right central incisor to right canine to prevent movement of the right central incisor. The upper left canine was moved into the space of the missing lateral incisor, the first premolar was moved into the position of the canine, and the remaining posterior teeth were mesialized to close the spaces (Fig. 3).
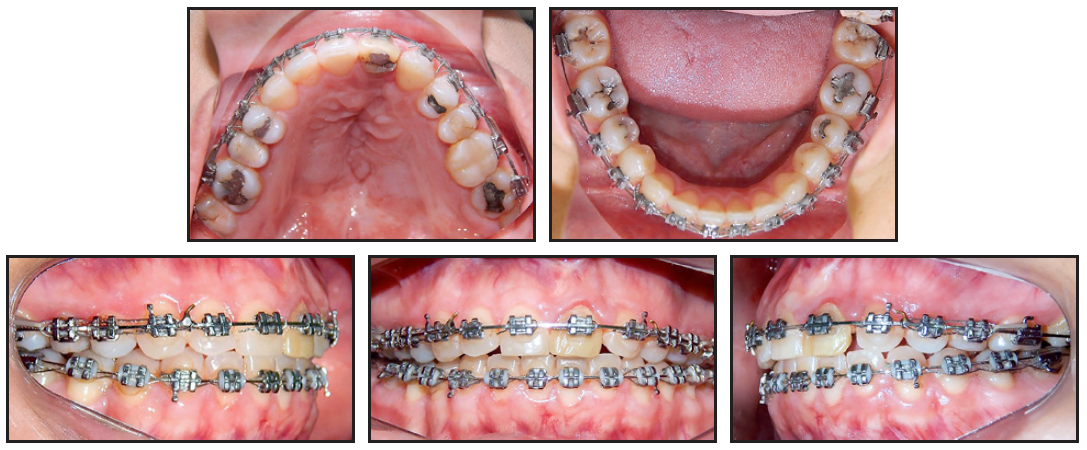
Fig. 3 After four years of treatment.
After a total five years and two months of treatment, upper and lower 3-3 lingual retainers were bonded, and a removable wraparound retainer was delivered for the upper arch, to be worn 20 hours per day for four months and at night thereafter (Fig. 4).
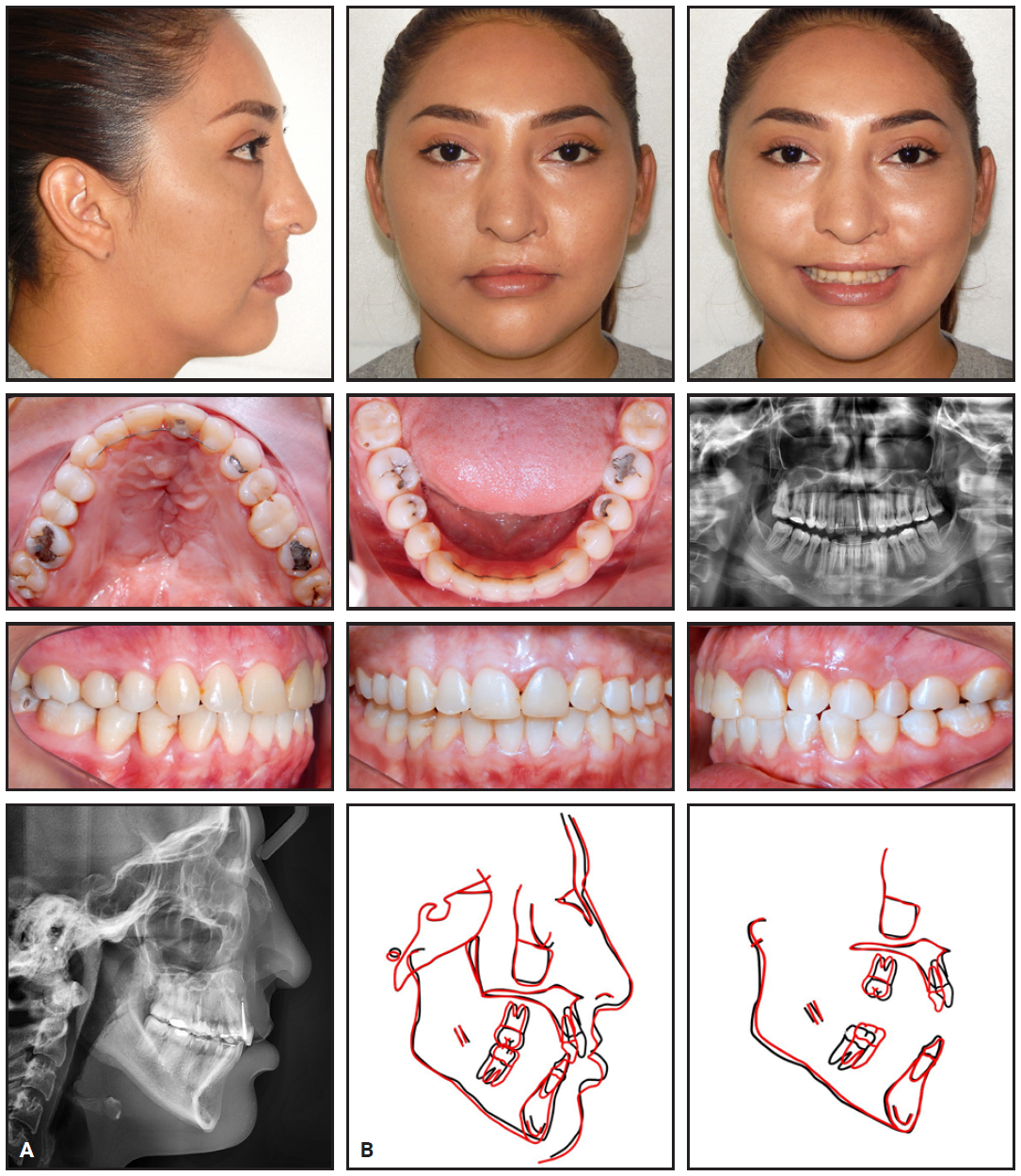
Fig. 4 A. Patient after about five years of treatment. B. Superimposition of pretreatment (black) and post-treatment (red) cephalometric tracings.
Treatment Results
All treatment objectives were achieved, resulting in significantly improved esthetics and function. The bilateral posterior crossbite was corrected, while the upper left canine was successfully substituted for the missing left lateral incisor, leaving a Class II molar relationship on the left side and Class I relationships on the right. In accordance with the findings of Silveira and colleagues, no signs or symptoms of TMD or impaired occlusal function were noted despite the lack of Class I relationships on the left side.11 Normal overjet and overbite were obtained, along with satisfactory intercuspation.
At the one-year follow-up appointment, the occlusion remained stable, and the smile esthetics were still pleasant (Fig. 5). The patient expressed satisfaction with the results.

Fig. 5 Patient one year after treatment.
Discussion
The orthodontist is a crucial member of the multidisciplinary team involved in cleft care.12 Such orthodontic treatment can be challenging, however, due to the complex mechanics involved in correcting dental anomalies associated with cleft lip and palate, including asymmetries, crossbites, and malpositioned or missing teeth. Among these issues, agenesis is the most prevalent.13,14
Compared with orthodontic space closure, prosthodontic rehabilitation of missing teeth tends to produce lower scores on periodontal indices such as the Gingival Index, Plaque Index, Papilla Bleeding Index, Irritant Index, probing pocket depth, and measurements of bone loss, and the esthetic results are more critically evaluated by dental professionals, patients, and laypeople.11 Therefore, missing lateral incisors in cleft lip and palate patients are more often treated with space closure.15,16
Collapse of the maxillary anterior segment is another common complication in patients who have undergone surgical repair of unilateral cleft lip and palate. This issue can be addressed with dentoalveolar expansion in conjunction with fixed appliance treatment, as demonstrated by the present case.
FOOTNOTES
- *Registered trademark of Solventum, St. Paul, MN; www.solventum.com.
REFERENCES
- 1. Rahimov, F.; Jugessur, A.; and Murray, J.C.: Genetics of nonsyndromic orofacial clefts, Cleft Palate Craniofac. J. 49:73-91, 2012.
- 2. Mossey, P.: Epidemiology underpinning research in the aetiology of orofacial clefts, Orthod. Craniofac. Res. 10:114-120, 2007.
- 3. Garib, D.G.; Rosar, J.P.; Sathler, R.; and Ozawa, T.O.: Dual embryonic origin of maxillary lateral incisors: Clinical implications in patients with cleft lip and palate, Dent. Press J. Orthod. 20:118-125, 2015.
- 4. Farronato, G.; Kairyte, L.; Giannini, L.; Galbiati, G.; and Maspero, C.: How various surgical protocols of the unilateral cleft lip and palate influence the facial growth and possible orthodontic problems: Which is the best timing of lip, palate and alveolus repair? Literature review, Stomatologija 16:53-60, 2014.
- 5. Menezes, R. and Vieira, A.R.: Dental anomalies as part of the cleft spectrum, Cleft Palate Craniofac. J. 45:414-419, 2008.
- 6. Sischo, L.; Wilson-Genderson, M.; and Broder, H.L.: Quality-of-life in children with orofacial clefts and caregiver well-being, J. Dent. Res. 96:1474-1481, 2017.
- 7. Bukhari, O.M.; Sohrabi, K.; and Tavares, M.: Factors affecting patients’ adherence to orthodontic appointments, Am. J. Orthod. 149:319-324, 2016.
- 8. Crerand, C.E.; Da Silveira, A.C.; Kapa, H.; Litteral, J.; Markey, M.K.; Mercado, A.; and Scott, M.: Adherence to orthodontic treatment in youth with cleft lip and/or palate, Cleft Palate Craniofac. J. 57:218-227, 2020.
- 9. Freitas, J.A.S.; Garib, D.G.; Oliveira, M.; Lauris, R.C.M.C.; de Almeida, A.L.P.F.; Neves, L.T.; Trindade-Suedam, I.K.; Yaedú, R.Y.F.; Soares, S.S.; and Pinto, J.H.N.: Rehabilitative treatment of cleft lip and palate: Experience of the Hospital for Rehabilitation of Craniofacial Anomalies-USP (HRAC-USP)—Part 2: Pediatric dentistry and orthodontics, J. Appl. Oral Sci. 20:268-281, 2012.
- 10. Paolone, M.G. and Kaitsas, R.: Orthodontic-periodontal interactions: Orthodontic extrusion in interdisciplinary regenerative treatments, Int. Orthod. 16:217-245, 2018.
- 11. Silveira, G.S.; de Almeida, N.V.; Pereira, D.M.T.; Mattos, C.T.; and Mucha, J.N.: Prosthetic replacement vs space closure for maxillary lateral incisor agenesis: A systematic review, Am. J. Orthod. 150:228-237, 2016.
- 12. Shaw, W.C.; Williams, A.C.; Sandy, J.R.; and Devlin, H.B.: Minimum standards for the management of cleft lip and palate: Efforts to close the audit loop—Royal College of Surgeons of England, Ann. R. Coll. Surg. Engl. 78:110-114, 1996.
- 13. De Souza, R.M.; de Oliveira, H.T.; and Farret, M.M.: Orthodontic treatment of unilateral cleft lip and palate associated with maxillary canine/premolar transposition: Case report, Dent. Press J. Orthod. 25:54-64, 2020.
- 14. Da Silva, A.P.R.; Costa, B.; and de Carvalho Carrara, C.F.: Dental anomalies of number in the permanent dentition of patients with bilateral cleft lip: Radiographic study, Cleft Palate Craniofac. J. 45:473-476, 2008.
- 15. Chetpakdeechit, W.; Stavropoulos, D.; and Hagberg, C.: Dental appearance, with focus on the anterior maxillary dentition, in young adults with bilateral cleft lip and palate (CLP): A follow up study, Swed. Dent. J. 34:27-34, 2010.
- 16. Zreaqat, M.H; Hassan, R.; and Hanoun, A.: Cleft lip and palate management from birth to adulthood: An overview, in Insights into Various Aspects of Oral Health, ed. J.F. Manakil, Intech Open, London, 2017.





COMMENTS
.