Clinical Efficiency of LightForce 3D-Printed Custom Brackets in Diverse Practice Settings
Orthodontic patients tend to prioritize convenience, making reductions in treatment time invaluable.1 Recent efforts to shorten orthodontic treatment have focused on increasing the rate of tooth movement by means of mechanical vibration,2,3 osteoperforation,2,4,5 corticotomy,6 low-intensity laser irradiation,2 pulsed electromagnetic fields, or hormone injections,7 but many of these approaches have failed to produce clinically significant results.2-5,7
Historically, treatment efficiency has been improved by developing better products and materials. Among the significant advancements of the past 50 years is the preadjusted appliance, which reduced the need for 1st-, 2nd-, and 3rd-order wire bends and thus reduced chairtime.8
Although preadjusted appliances did improve treatment efficiency, they presented a technical challenge: as Miethke and Melsen noted more than 20 years ago, to account for individual variations in tooth morphology, the brackets would have to be custom-made.9
The recent development of fully customized, 3D-printed orthodontic brackets has the potential to reduce treatment times even further. Our previous study of patients from one practice showed that those treated using LightForce 3D-printed custom brackets experienced shorter treatment times and fewer appointments, on average, than those treated with conventional preadjusted appliances.10 The present article expands the scope of the study to include four practices with different treatment philosophies, demographics, and practice-management models.
Materials and Methods
This retrospective study was approved by the Advarra Institutional Review Board, Pro00065799. The subjects were patients from four private orthodontic practices who were treated using either LightForce 3D-printed appliances or conventional preadjusted appliances between Aug. 5, 2019, and July 20, 2023. A subset of patients from practice 1 were involved in the previously reported study.10 Inclusion criteria for both groups were the availability of pretreatment photos, use of maxillary and mandibular full fixed appliances, and eruption of all permanent teeth except for the second and third molars and congenitally missing teeth. Patients were excluded if treatment involved Phase I, orthognathic surgery, or temporary anchorage devices, or if they presented with significant periodontal disease or with unerupted or impacted teeth. Additional exclusion criteria were current, chronic use of nonsteroidal anti-inflammatory medication, estrogen, calcitonin, or corticosteroids, or any history of the use of bisphosphonates or other medications for treatment of osteoporosis.
The following data were obtained from patient records in all four practices: date of birth, Angle classification, specific tooth extractions prescribed for orthodontic treatment, bracket bonding and debonding dates, number of non-emergency scheduled appointments, number of bracket-repositioning and archwire-detailing appointments, and treatment phase (I or II). The numbers of repositioned brackets and teeth requiring detailing bends per patient were collected from practices 1, 2, and 3, but were not available from practice 4.
To gauge initial case severity, pretreatment photos were scored independently by three calibrated examiners using the dental-health component of the Index of Orthodontic Treatment Need (IOTN),11 and the scores were averaged.
The data were inspected for missingness and distributional form and analyzed using SAS** version 9.4 software. Wilcoxon rank-sum tests were used to compare the LightForce and conventional-bracket groups for numerical and ordinal variables, and Kruskal-Wallis tests were used to assess these data across practices. Categorical variables were compared with chi-square or Fisher’s exact tests. The level of significance was set at .05 for two-sided tests.
Data summaries are presented as side-by-side box plots. Each box is bounded by the first (Q1) and third (Q3) quartiles of the data, with the median represented by the horizontal line within the box; larger boxes indicate larger variations in the data. The quartiles (Q1, median, and Q3) are the values dividing the data into four equal parts. The “whiskers” show the approximate spread of the data estimated within 1.5 times the interquartile range (Q3 – Q1). Outliers are shown as isolated data points outside the whiskers.
Results
In practices 1, 2, and 4, there were no significant differences in the mean age of the LightForce and conventional groups (Table 1).
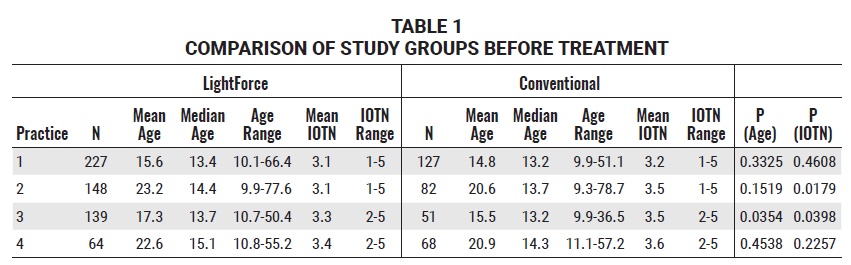
In practice 3, the difference in mean age was statistically significant, with the LightForce group (17.3) slightly older than the conventional group (15.5), but there was no significant difference in median age (13.7 and 13.2, respectively). The median patient age for all groups in all offices was approximately 14, and there were no significant differences among groups. In two practices, the mean age was 15-17; in the other two, it was 20-23. Evaluation of the age distribution revealed that the higher mean age in two practices could be explained by the inclusion of senior adult patients.
All groups comprised about 55-60% females. There were no statistically significant differences in mean IOTN grades between the LightForce and conventional-bracket groups for practices 1 (3.1 and 3.2, respectively) and 4 (3.4 and 3.6, respectively). The differences in mean IOTN grades for the LightForce and conventional-bracket groups were statistically significant for practices 2 (3.1 and 3.5, respectively) and 3 (3.3 and 3.5, respectively), but these differences were considered to be clinically unimportant.
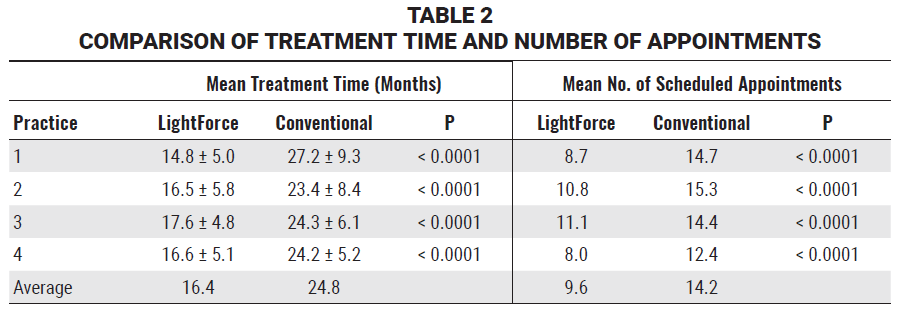
In all four practices, mean treatment times were consistently and significantly shorter for the LightForce group than for the group treated with conventional brackets. The average treatment time for the LightForce patients ranged from 15 to 17 months, whereas the conventional-bracket patients averaged about 24 months of treatment; thus, treatment time was about 30% shorter for the LightForce group (Fig. 1, Table 2).
The number of scheduled appointments followed the same trend in all practices. LightForce patients averaged 8-11 visits, whereas conventional-bracket patients averaged 12-15 visits (Fig. 2, Table 2). This resulted in about 30% fewer appointments for the LightForce-bracket patients across all practices.
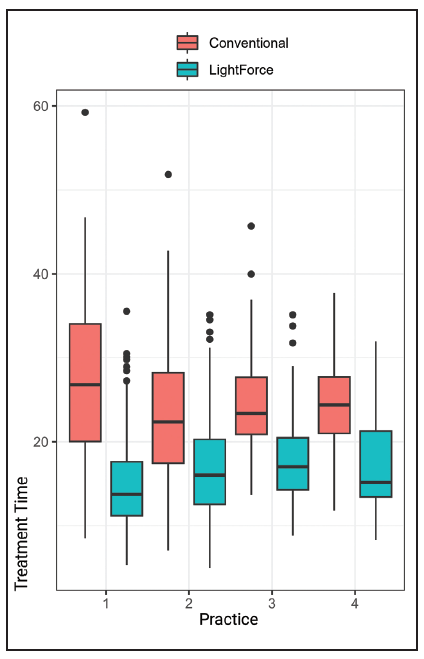
Fig. 1 Box plots of treatment time (in months) for LightForce* and conventional-bracket groups in each practice.
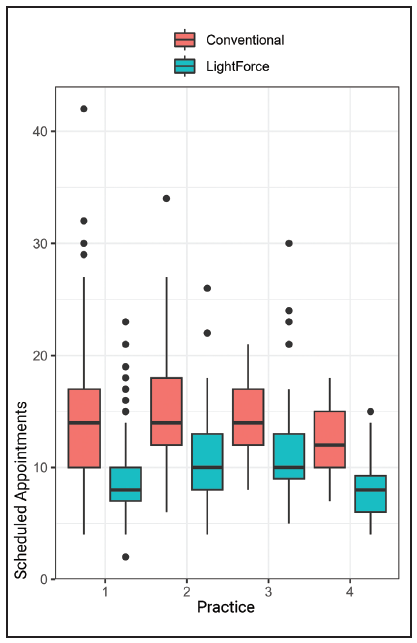
Fig. 2 Box plots of non-emergency scheduled appointments for LightForce and conventional-bracket groups in each practice.
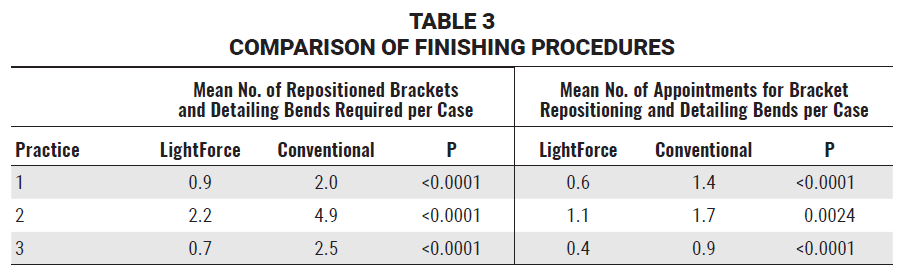
The numbers of repositioned brackets and teeth requiring detailing bends, as well as the numbers of appointments needed for these procedures, were analyzed for practices 1, 2, and 3. In all three practices, fewer cases in the LightForce group required finishing procedures involving either bracket repositioning or archwire bends (Fig. 3A, Table 3), and fewer appointments were required for these procedures (Fig. 3B, Table 3).
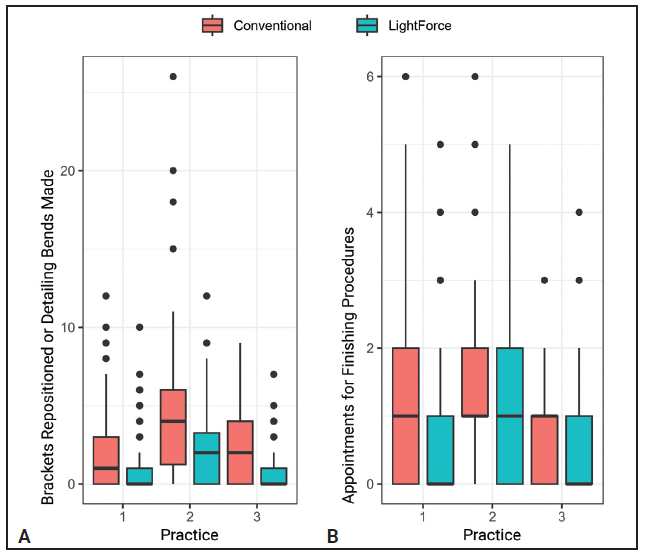
Fig. 3 A. Box plots of bracket-repositioning procedures performed or archwire-detailing bends needed for LightForce and conventional-bracket groups in each practice. B. Box plots of appointments for finishing procedures needed for LightForce and conventional-bracket groups in each practice.
Discussion
Our previous study of a single-orthodontist private practice found reductions in both treatment time and the number of scheduled appointments for patients treated with LightForce 3D-printed brackets, as compared to those treated with conventional brackets.10 The goal of the present study was to determine whether the same reductions would be seen in multiple practices with different treatment philosophies, practice-management models, and preferred brands of conventional appliances.
In the previous study, the quality of finished LightForce-bracket cases was considered equivalent to, if not better than, that of finished conventional-bracket cases.10 In the present study, because final study casts were not available for all practices, the quality of the treatment results could not be assessed. While this is a shortcoming of the study, we believe the practitioners would have ensured outcomes similar to or better than those of their conventional cases before debonding their LightForce patients.
In this study, the mean treatment time with LightForce brackets was reduced to 15-17 months, regardless of patient age (Tables 1,2), and was similar across practices despite their diversity. Differences in treatment philosophies and mechanics were to be expected, since the orthodontists in this study had clinical experience ranging from six to 41 years, each practitioner had studied in a different orthodontic program, and the four practices were in different states (Table 4). Furthermore, two of the practices were single-orthodontist offices with multiple locations, another was a partnership of two orthodontists with multiple locations and shared patients, and the last practice had a single location and was part of an orthodontic service organization. The diversity of management models potentially indicated different scheduling practices and policies that could have affected treatment efficiency.
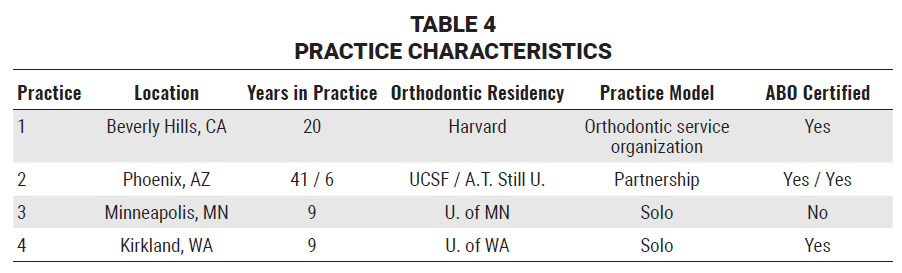
Fixed appliance techniques also varied between practices (Table 5). The conventional brackets were made by various manufacturers from either stainless steel or ceramic materials, and they included both twin and self-ligating designs with .018" or .022" slots. Each practice used the standard MBT*** prescription for its conventional brackets, except for one office that used the Roth prescription for the upper incisors. Regardless of the conventional bracket used, the mean treatment time at each office was about 24 months—consistent with published reports.12-16
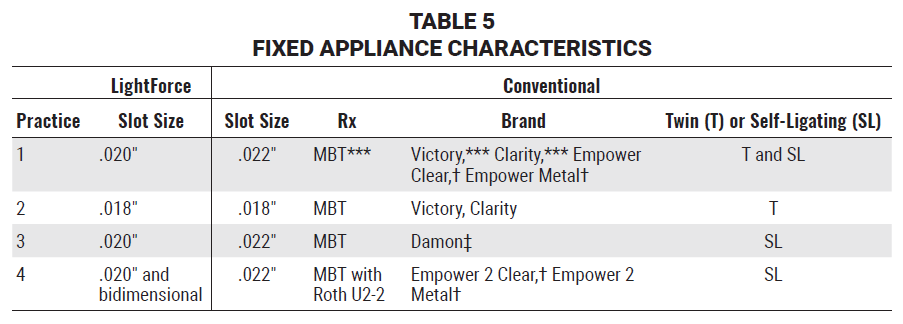
For their LightForce brackets, two of the practices used .020" slots, another used both .020" slots and a bidimensional setup, and the other used .018" slots; thus, three of the four practices selected the .020" slot size, which is unique to LightForce brackets.17,18 The practices were able to employ their individual treatment philosophies and mechanics, yet all experienced the same significant reductions in treatment times, indicating that fully customized, 3D-printed brackets can predictably increase clinical efficiency regardless of fixed appliance system or technique.
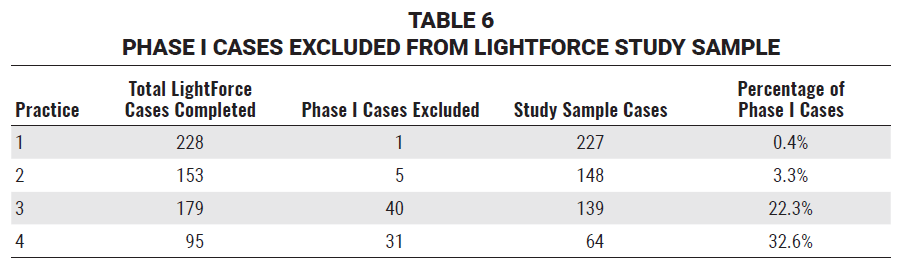
Orthodontists may also have philosophical differences about when to treat different types of malocclusions, particularly Class II patients.19,20 Although Phase I cases were excluded from the results of this study, practices 3 and 4 reported performing substantially more Phase I LightForce treatment than practices 1 and 2 did (Table 6). Therefore, it can be observed that practices with different approaches to Phase I treatment experienced similar improvements in efficiency during comprehensive Phase II treatment.
Finishing is widely considered one of the most difficult phases of orthodontic treatment.21-25 While the overall importance of proper bracket placement has been recognized,25-28 to our knowledge, no studies have investigated the amount of time needed at the end of treatment for detailing with bracket repositioning, wirebending, or finishing elastics. In a study of treatment times across six orthodontic practices, Fink and Smith surmised that finishing procedures significantly affected treatment duration, but they did not report any data to support this conclusion.13
In the present study, among the three practices for which finishing data were available, the mean numbers of bracket-repositioning and wire-adjustment procedures were 50-70% lower in the LightForce group, and the mean numbers of appointments for these procedures were reduced by 30-60% (Fig. 3, Table 3). It is reasonable to assume that this reduction in finishing procedures would correlate with the observed reduction in overall treatment time.
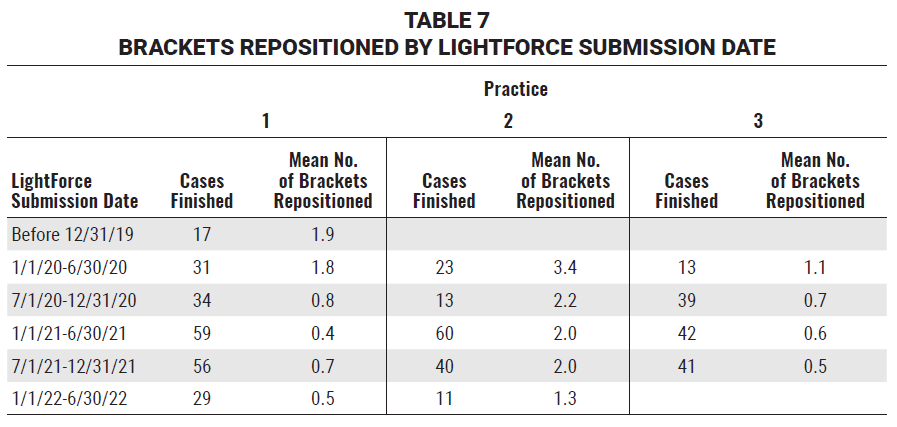
Even though bracket repositioning and wire bends were required less frequently for LightForce patients, they were still necessary in some cases. The reasons for this are under further study, but could involve incorrect digital planning of final tooth positions on the LightPlan* or a technical issue with the indirect bonding procedure, such as inadequate seating of the trays. Since the LightForce cases in this study were the first cohort finished by all four offices with this new technology, the doctors and clinical assistants were still learning new digital-planning, bonding, and clinical-management techniques. In each practice, as the office gained experience with the LightForce system, the number of bracket-repositioning procedures and detailing bends declined significantly (Fig. 4, Table 7).
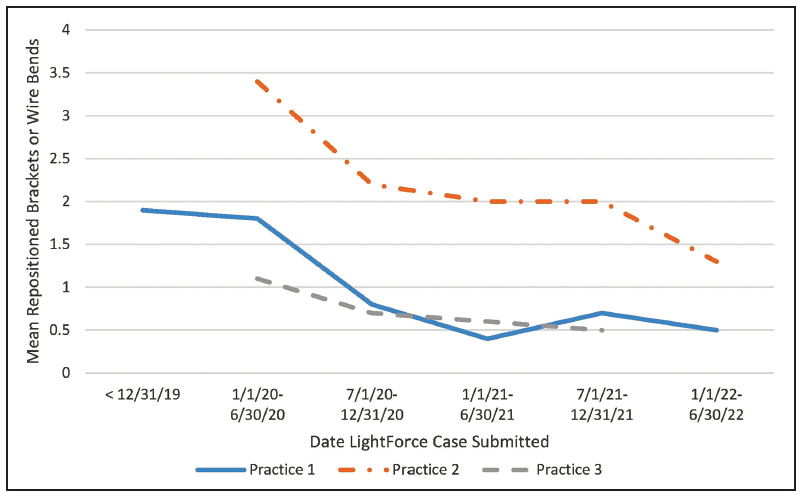
Fig. 4 Mean number of finishing procedures per case for each practice by date of LightForce case submission.
Indirect bonding was introduced 50 years ago28 and has improved along with advances in digital technology26; while the procedure remains technique-sensitive, its overall advantages will likely make it the standard of care in the future. The LightForce system utilizes indirect bonding with 3D-printed trays. To illustrate the efficacy of the LightForce indirect bonding system, scans of a patient taken after bracket bonding were superimposed on the digital LightPlan, and the differences were analyzed with Autodesk Meshmixer†† software (Fig. 5).
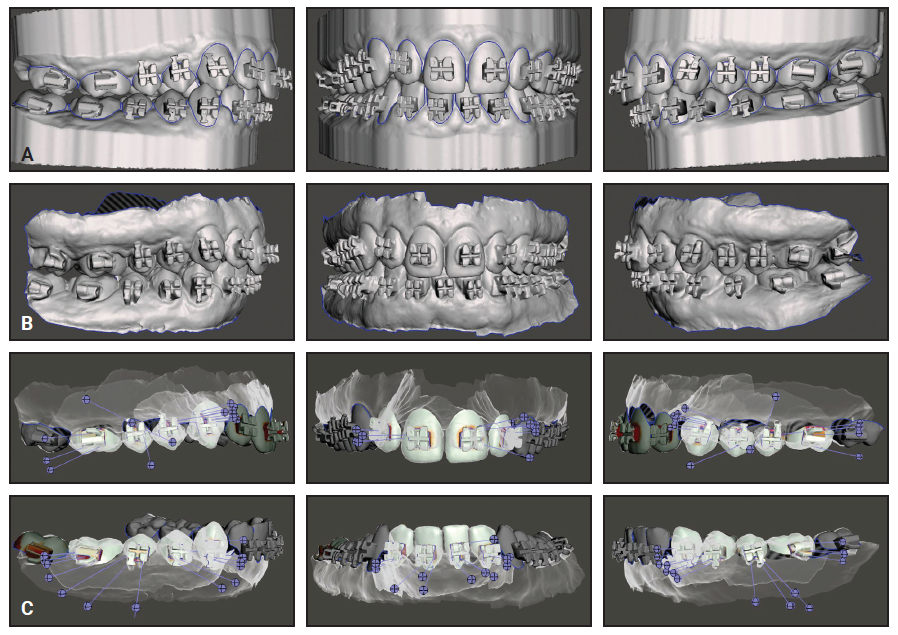
Fig. 5 Example of LightForce bracket placement. A. Digital LightPlan* of bracket placement. B. Scan of patient after bracket bonding. C. Superimpositions of planned and actual bracket placement using Autodesk Meshmixer†† software (red = deviation of .5mm or greater; yellow, pink, or brown = deviation of less than .5mm; white or no color = perfect match).
In this example, the superimpositions demonstrate a high degree of accuracy; deviations within the bracket slots or around the bracket bases are attributable to the difficulty in obtaining scans of sufficient quality to evaluate those areas. The technologies, materials, and procedures used for indirect bonding will continue to improve, allowing clinicians to place fully customized, 3D-printed brackets precisely as planned in the digital setups, in accordance with their preferred treatment mechanics and philosophies.
Conclusion
This multi-office retrospective study demonstrates consistent reductions in treatment duration and the number of appointments needed for fully bonded treatment with LightForce 3D-printed custom brackets. The results were consistent across all four practices, despite substantial differences in demographics, practitioner experience, treatment philosophies, and practice-management models. Although every attempt was made to eliminate potential sources of bias in this study, a randomized clinical trial would provide a higher level of evidence.
ACKNOWLEDGMENT: We would like to acknowledge Ms. Lorretta Zimmerman at Waldman Orthodontics, Ms. Angela Shreeve and Ms. Becky Menard at Serrano Orthodontics, Ms. Mari Schwarz at Mint Orthodontics, and Ms. Allie Erickson at Kirkland Redmond Orthodontics for their assistance in gathering data for this study. We would also like to acknowledge Dr. Celestino Nobrega’s assistance with IOTN scoring. This study was supported by LightForce Orthodontics, Burlington, MA.
FOOTNOTES
- *LightForce Orthodontics, Burlington, MA; www.lf.co.
- **SAS, Cary, NC; www.sas.com.
- ***3M, Monrovia, CA; www.3M.com.
- †American Orthodontics, Sheboygan, WI; www.americanortho.com.
- ‡Ormco Corporation, Brea, CA; www.ormco.com.
- ††Autodesk, Inc., San Francisco, CA; www.meshmixer.com.
REFERENCES
- 1. Kazancı, F.; Aydoğan, C.; and Alkan, Ö.: Patients’ and parents’ concerns and decisions about orthodontic treatment, Kor. J. Orthod. 46:20-26, 2016.
- 2. El-Angbawi, A.; McIntyre, G.T.; Fleming, P.S.; and Bearn, D.R.: Non-surgical adjunctive interventions for accelerating tooth movement in patients undergoing fixed orthodontic treatment, Cochrane Database Syst. Rev. CD010887, 2023.
- 3. Pavlin, D.; Anthony, R.; Raj, V.; and Gakunga, P.T.: Cyclic loading (vibration) accelerates tooth movement in orthodontic patients: A double-blind, randomized controlled trial, Semin. Orthod. 21:187-194, 2015.
- 4. Alkebsi, A.; Al-Maaitah, E.; Al-Shorman, H.; and Abu Alhaija, E.: Three-dimensional assessment of the effect of microosteoperforations on the rate of tooth movement during canine retraction in adults with Class II malocclusion: A randomized controlled clinical trial, Am. J. Orthod.153:771-785, 2018.
- 5. Shahrin, A.A.; Ghani, S.H.A.; and Norman, N.H.: Effectiveness of microosteoperforations in accelerating alignment of maxillary anterior crowding in adults: A randomized controlled clinical trial, Am. J. Orthod. 160:784-792, 2021.
- 6. Aboul-Ela, S.M.B.E.; El-Beialy, A.R.; El-Sayed, K.M.F.; Selim, E.M.N.; El-Mangoury, N.H.; and Mostafa, Y.A.: Miniscrew implant-supported maxillary canine retraction with and without corticotomy-facilitated orthodontics, Am. J. Orthod. 139:252-259, 2011.
- 7. McGorray, S.P.; Dolce, C.; Kramer, S.; Stewart, D.; and Wheeler, T.T.: A randomized, placebo-controlled clinical trial on the effects of recombinant human relaxin on tooth movement and short-term stability, Am. J. Orthod. 141:196-203, 2012.
- 8. Magness, W.B.: The straight-wire concept, Am. J. Orthod. 73:541-550, 1978.
- 9. Miethke, R.R. and Melsen, B.: Effect of variation in tooth morphology and bracket position on first and third order correction with preadjusted appliances, Am. J. Orthod. 116:329-335, 1999.
- 10. Waldman, A.; Garvan, C.S.; Yang, J.; and Wheeler, T.T.: Clinical efficiency of LightForce 3D-printed custom brackets, J. Clin. Orthod. 57:274-282, 2023.
- 11. Shaw, W.C.; Richmond, S.; and O’Brien, K.D.: The use of occlusal indices: A European perspective, Am. J. Orthod. 107:1-10, 1995.
- 12. Beckwith, F.R.; Ackerman, R.J. Jr.; Cobb, C.M.; and Tira, D.E.: An evaluation of factors affecting duration of orthodontic treatment, Am. J. Orthod. 115:439-447, 1999.
- 13. Fink, D.F. and Smith, R.J.: The duration of orthodontic treatment, Am. J. Orthod. 102:45-51, 1992.
- 14. Mavreas, D. and Athanasiou, A.E.: Factors affecting the duration of orthodontic treatment: A systematic review, Eur. J. Orthod. 30:386-395, 2008.
- 15. Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; and Harding, W.J.: Factors influencing treatment time in orthodontic patients, Am. J. Orthod. 129:230-238, 2006.
- 16. Vig, P.S.; Weintraub, J.A.; Brown, C.; and Kowalski, C.J.: The duration of orthodontic treatment with and without extractions: A pilot study of five selected practices, Am. J. Orthod. 97:45-51, 1990.
- 17. Waldman, A. and Bonebreak-Jackson, C.: Introduction to LightForce, Part 2: Treatment planning and clinical management, J. Clin. Orthod. 57:594-605, 2023.
- 18. Waldman, A.; Moshiri, M.; and Bonebreak-Jackson, C.: Introduction to LightForce, Part 1: 3D-printing the next generation of fixed appliances, J. Clin. Orthod. 57:500-510, 2023.
- 19. Batista, K.B.; Thiruvenkatachari, B.; Harrison, J.E.; and O’Brien, K.D.: Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents, Cochrane Database Syst. Rev. CD003452, 2018.
- 20. King, G.J.; Keeling, S.D.; Hocevar, R.A.; and Wheeler, T.T.: The timing of treatment for Class II malocclusions in children: A literature review, Angle Orthod. 60:87-97, 1990.
- 21. Poling, R.: A method of finishing the occlusion, Am. J. Orthod. 115:476-487, 1999.
- 22. Vagdevi, H.K.; Nayak, R.S.; and Pasha, A.: Finishing and detailing in orthodontics: A short review, J. Dent. Med. Sci. 18:7-12, 2019.
- 23. Haltom, T.: Finishing and retention procedures in the Alexander discipline, Semin. Orthod. 7:132-137, 2001.
- 24. McLaughlin, R.P. and Bennett, J.C.: Finishing with the preadjusted orthodontic appliance, Semin. Orthod. 9:165-183, 2003.
- 25. Sondhi, A.: The implications of bracket selection and bracket placement on finishing details, Semin. Orthod. 9:155-164, 2003.
- 26. Christensen, L.R. and Cope, J.B.: Digital technology for indirect bonding, Semin. Orthod. 24:451-460, 2018.
- 27. Guenthner, T.A. and Larson, B.E.: Indirect bonding: A technique for precision and efficiency, Semin. Orthod. 13:58-63, 2007.
- 28. Kalange, J.T. and Thomas, R.G.: Indirect bonding: A comprehensive review of the literature, Semin. Orthod. 13:3-10, 2007.





COMMENTS
.