Clinical Efficiency of LightForce 3D-Printed Custom Brackets
Advances in computerized design and manufacturing have made it possible to create customized orthodontic systems tailored to each patient’s unique dentition and treatment needs. The clinical premise behind customized bracket systems such as Insignia* and KLOwen** is that individualization will result in reduced treatment times, fewer appointments, and improved clinical performance. Previous research has shown mixed results, however, for customized orthodontic systems as compared with traditional brackets.1-5
Three-dimensional printing is the latest step in digital technology for customized fixed appliances. In 2019, LightForce*** introduced the first complete 3D-printed bracket system featuring customized, polycrystalline alumina brackets that are designed and printed de novo for each tooth based on a digital setup of the dentition (Fig. 1). The custom base and slot-prescription technology of LightForce brackets are industry-first features enabled by 3D printing.
This study compares the clinical efficiency and efficacy of treatment with LightForce brackets to treatment with conventional bracket systems.
Materials and Methods
This study was approved by the Advarra Institutional Review Board, Pro00065799.
The subjects for this retrospective study were obtained from a single-orthodontist private practice that began using LightForce 3D-printed appliances in May 2019. Pre- and post-treatment records were obtained from consecutively completed LightForce subjects debonded between October 2020 and July 2022 (N = 103) and consecutively completed conventional-appliance subjects debonded between January 2021 and December 2021 (N = 74). Conventional appliances included 3M Victory,† 3M Clarity,† Empower Clear,‡ and Empower Metal.‡
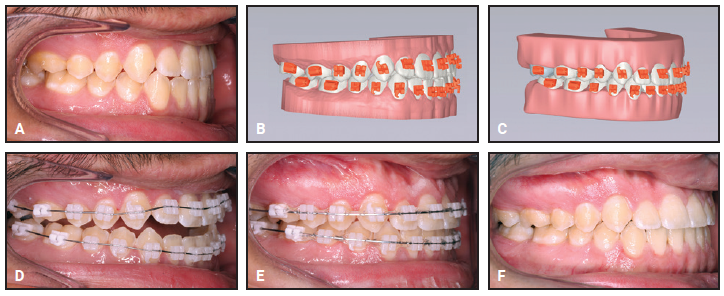
Fig. 1 Example of minor Class III case treated with .018" LightForce*** brackets. A. Undertorqued upper incisors resulting in edge-to-edge occlusion. B. Digital LightPlan*** setup showing initial malocclusion with planned bracket placement. C. Digital LightPlan setup showing planned final occlusion. D. LightForce brackets bonded and upper and lower .016" nickel titanium archwires inserted. E. After five months of treatment, .017" × .025" nickel titanium archwires used to express desired torque in .018" slots. F. Patient debonded after six and one-half months of treatment and five appointments, including bonding and debonding.
Inclusion criteria for both groups were the availability of pretreatment digital study models, the use of maxillary and mandibular full fixed appliances, and the eruption of all permanent teeth, except for second and third molars and congenitally missing teeth. Both groups excluded patients who required orthognathic surgery; had unerupted or impacted premolars or canines; were treated with temporary anchorage devices and palatal distalizers; had significant periodontal disease; chronically used any nonsteroidal anti-inflammatory medication, estrogen, calcitonin, or corticosteroids during treatment; or had a history of use (either before or during orthodontic treatment) of bisphosphonates or other medications for the treatment of osteoporosis.
The following data were derived from each patient’s records: Angle classification, any specific tooth extractions prescribed for treatment, bracket bonding and debonding dates, date of case submission to LightForce, number of scheduled appointments, number of unscheduled emergency appointments, number of loose brackets, and final upper and lower archwires. Pretreatment and post-treatment (when available) digital models were analyzed by a calibrated examiner who was blinded to the treatment group, using the Peer Assessment Rating (PAR) index6 in OrthoAnalyzer†† software.
SAS‡‡ version 9.4 was used for all statistical analyses. Data were inspected for missingness and distributional form. Groups were compared using t-tests for continuous data, Wilcoxon rank-sum tests for ordinal data, and chi-square tests for categorical data. The level of significance was set at .05 for two-sided tests. Data summaries are presented as side-by-side box plots; each box is bounded by the first (Q1) and third (Q3) quartiles of the data, and the median is the horizontal line within the box. Larger boxes indicate larger variations in the data. The “whiskers” show the approximate spread of the data estimated within 1.5 times the interquartile range (IQR = Q3-Q1). Outliers are shown as isolated data points outside the whiskers.
Results
The LightForce treatment group (39 male, 64 female) did not differ significantly from the conventional-bracket group (35 male, 39 female) in terms of age, initial case severity as determined by the PAR index (Table 1), percentage of extraction cases, Angle classification (Table 2), or sex (p = .1389) at the beginning of treatment. The treatment groups were representative of the practitioner’s case distribution, with a wide range of severity from mild (PAR < 5) to severe (PAR > 25).
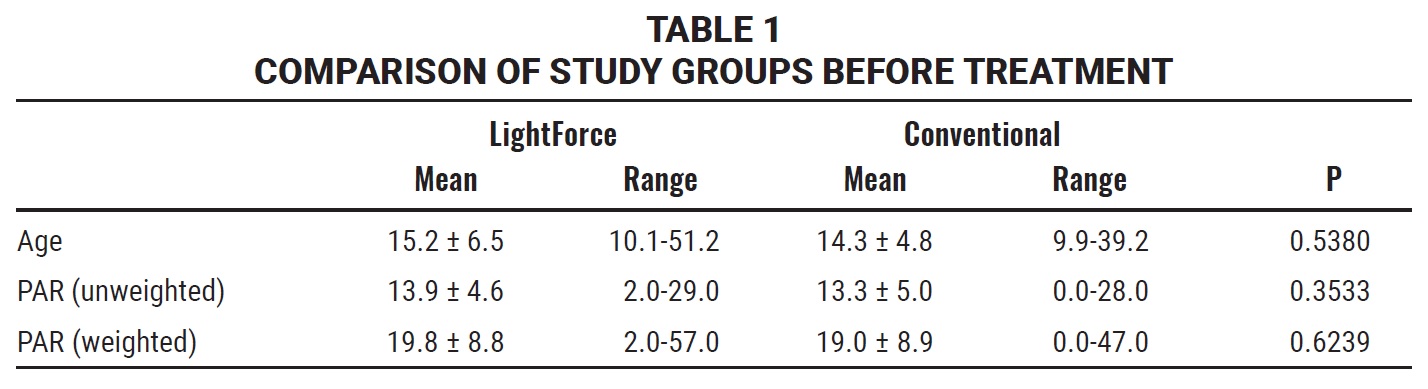
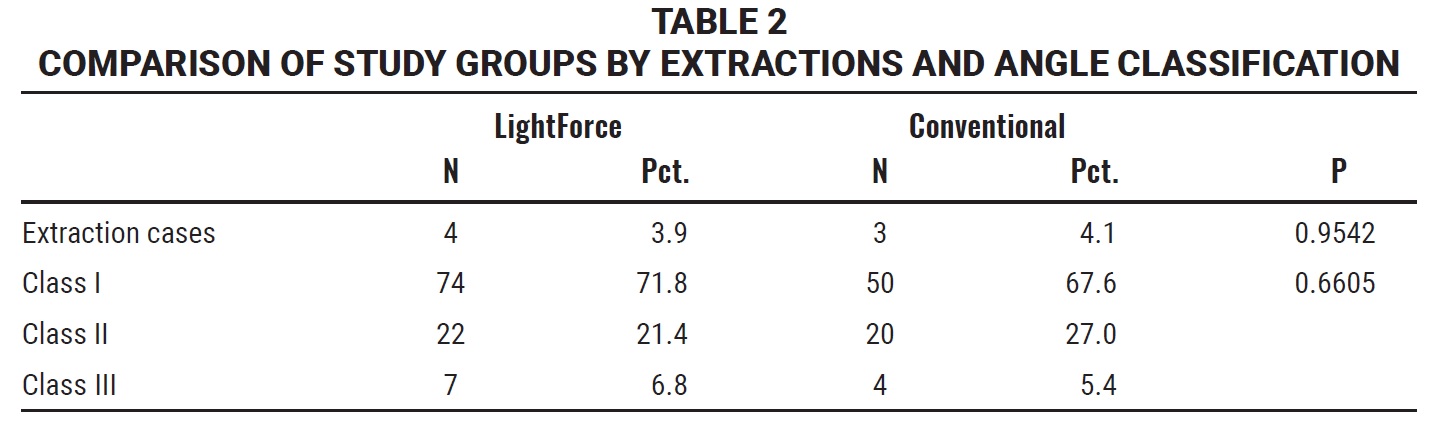
At the conclusion of treatment, the differences between the LightForce and conventional-bracket groups in terms of the length of treatment and the number of scheduled, emergency, and total appointments were all statistically significant. The LightForce group’s average treatment time was 45% shorter than the conventional group’s treatment time (Fig. 2, Table 3).
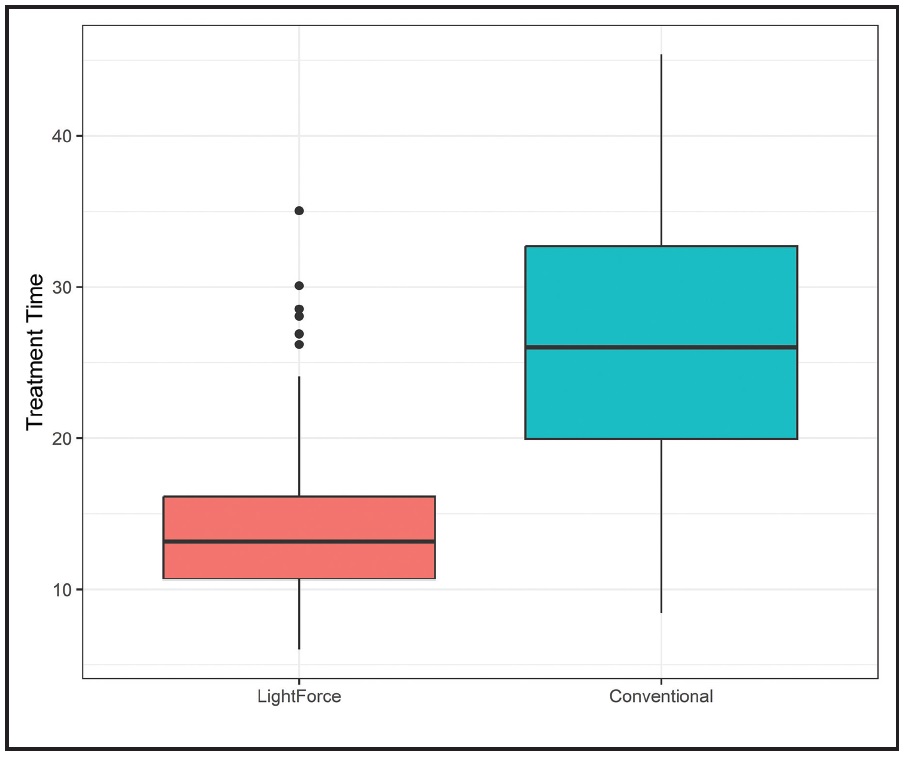
Fig. 2 Box plots of treatment time (in months) for patients in LightForce and conventional-bracket groups (p < .0001).
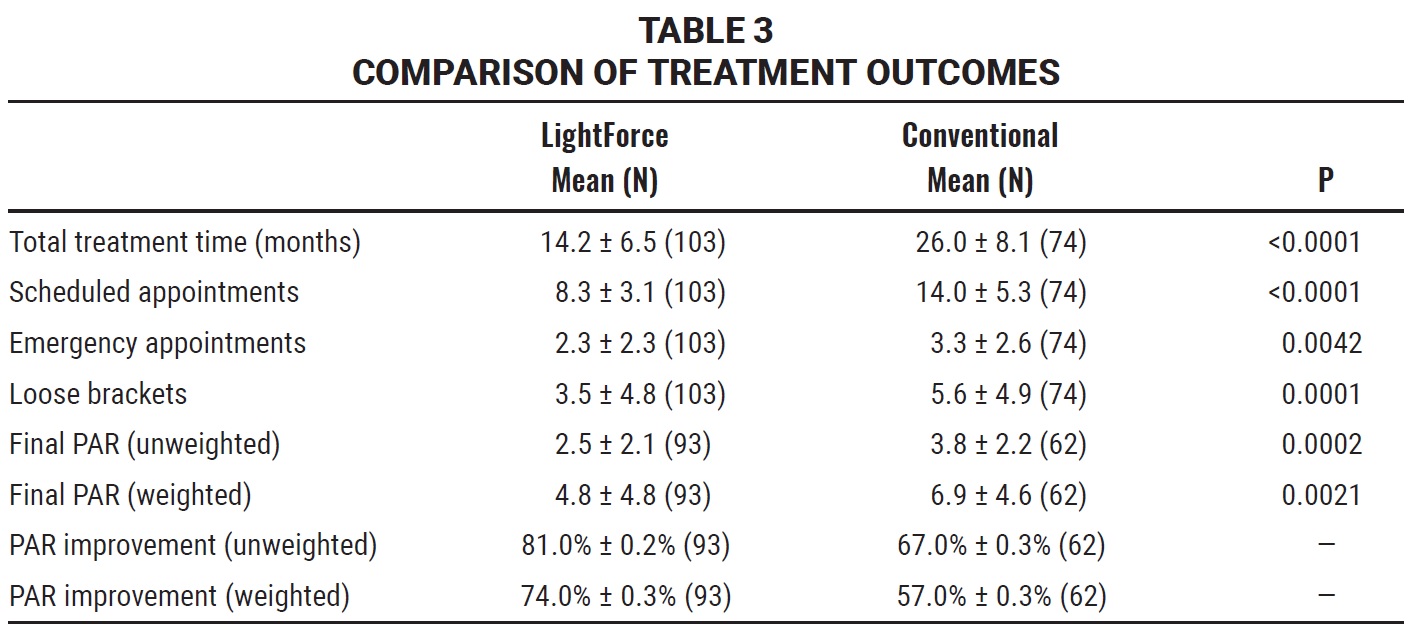
Treatment with the LightForce brackets required about six fewer scheduled appointments and one fewer emergency appointment, on average, than treatment with conventional brackets (Fig. 3).
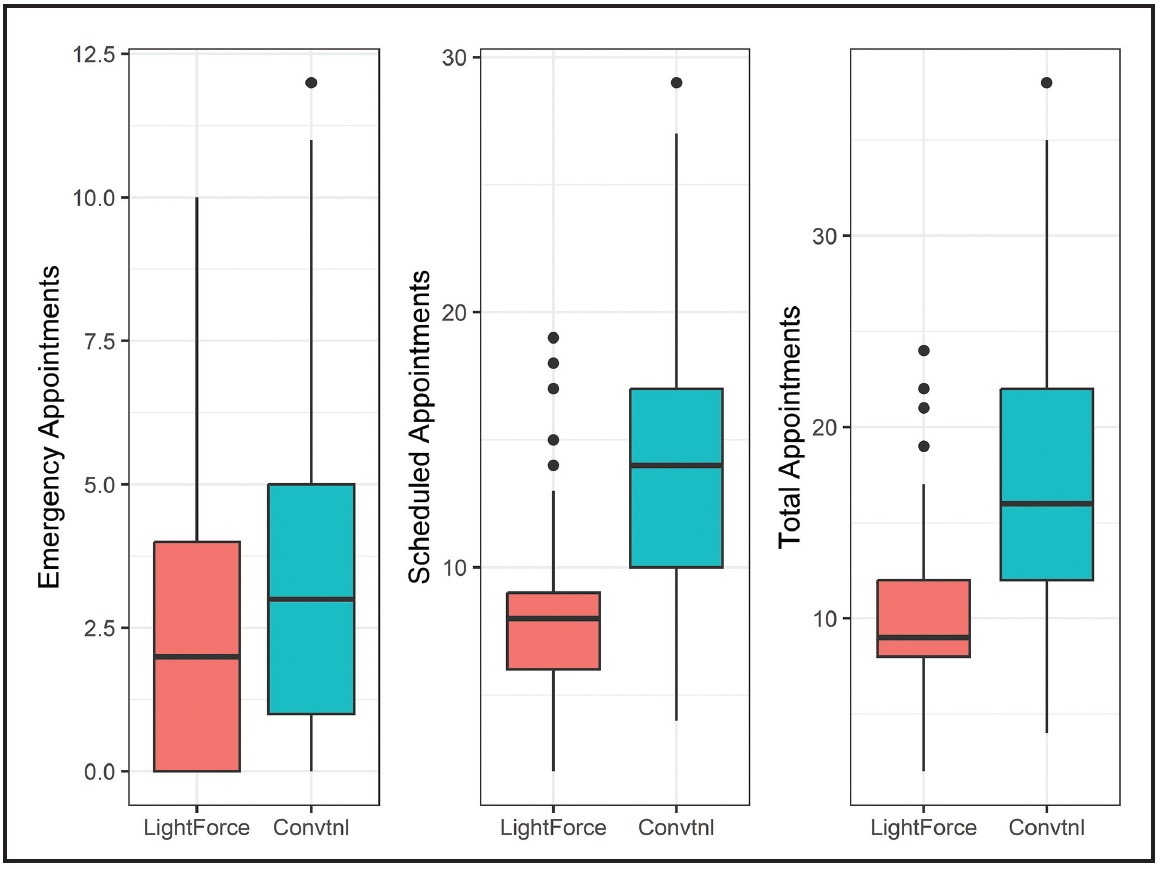
Fig. 3 Box plots of emergency (p = .0042), scheduled (p < .0001), and total (p < .0001) patient appointments in LightForce and conventional-bracket groups.
The LightForce group averaged about two fewer loose brackets than were found in the conventional-bracket group (Fig. 4).
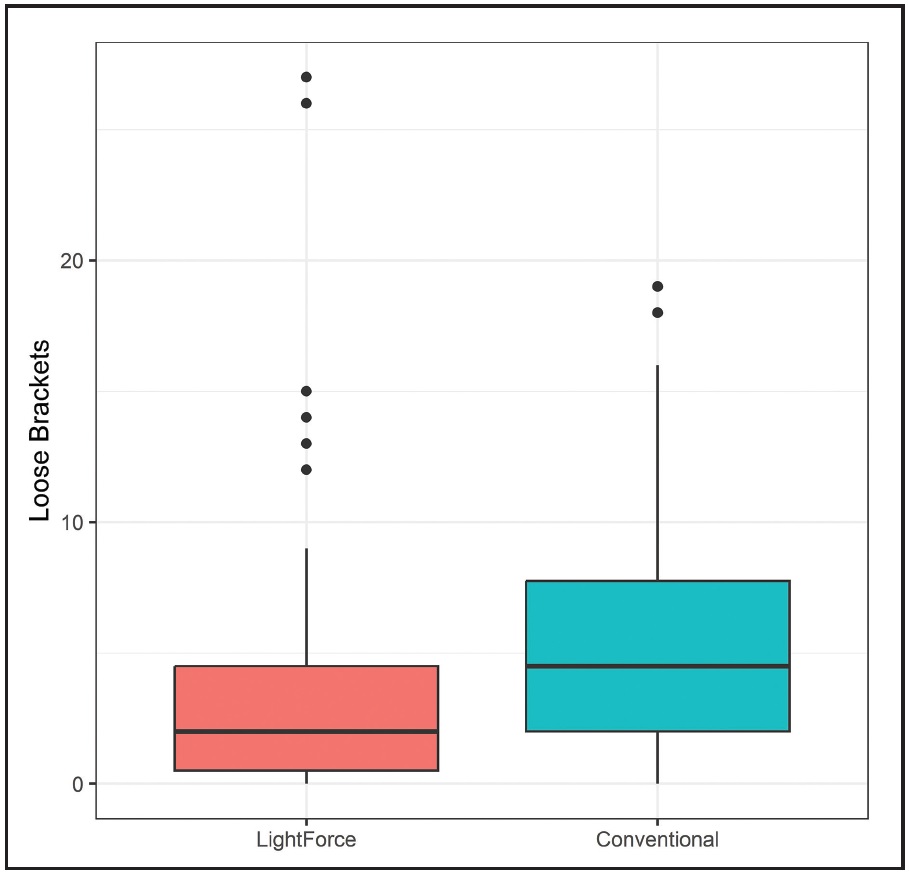
Fig. 4 Box plots of loose brackets in LightForce and conventional-bracket groups (p = .0001).
Nickel titanium wires were used as the final upper archwires in 78% of the LightForce subjects (Fig. 5), compared to 34% of the conventional-bracket subjects (p < .0001), and as the final lower archwires in 65% of the LightForce subjects, compared to 31% of the conventional-bracket subjects (p < .0001).
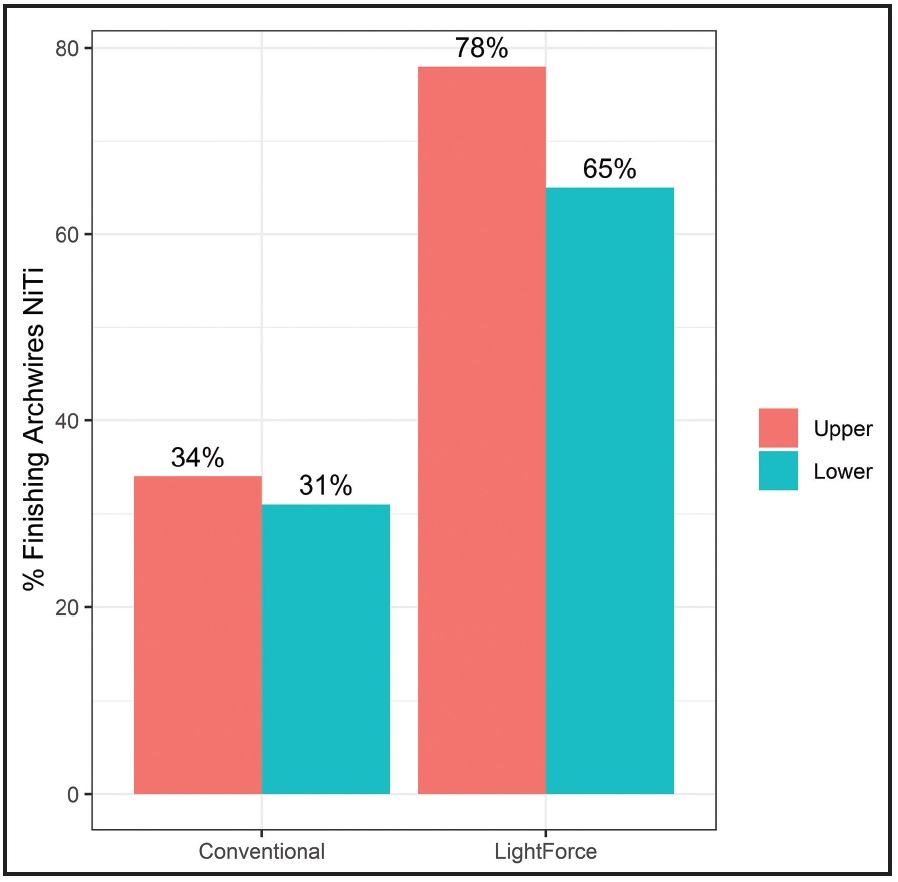
Fig. 5 Percentages of nickel titanium upper and lower finishing archwires in LightForce and conventional-bracket groups (p < .0001).
Final models were available for 93 of the LightForce subjects and 62 of the conventional-bracket subjects. The final clinical outcomes, as measured by the PAR index, showed a mean improvement of 81% (unweighted) and 74% (weighted) in the LightForce group, compared to 67% (unweighted) and 57% (weighted) in the conventional group (Table 3).
Discussion
Authors have reported variable orthodontic treatment times for conventional fixed appliances. Beckwith and colleagues observed an average treatment time of 28.6 months with a range of 23.4-33.4 months in five offices,7 whereas Fink and Smith found an average of 23.1 months with a range of 19.4-27.9 months in six offices.8 The average length of treatment for the conventional-bracket group in this study was 26 months, which is generally consistent with other reports.7-11 The finding that treatment time decreased by 45% in the LightForce group, combined with a 41% reduction in the number of scheduled appointments, was not only statistically significant, but was clinically significant to the practitioner. Scatter plots of treatment times vs. unweighted initial PAR scores of LightForce and conventional brackets are shown, along with regression lines and 95% confidence bands (Fig. 6). The intercept and slope of the PAR by treatment time regression line for the LightForce bracket were estimated to be 9.6 (S.E. = 1.6) and .33 (S.E. = .11), respectively; the intercept and slope for the conventional brackets were estimated to be 19.2 (S.E. = 2.6) and .51 (S.E. = .18), respectively. It is clear from the regression lines that treatment time increased as the initial PAR increased for both groups, but that the treatment times were much shorter in the LightForce group for all levels of initial PAR scores.
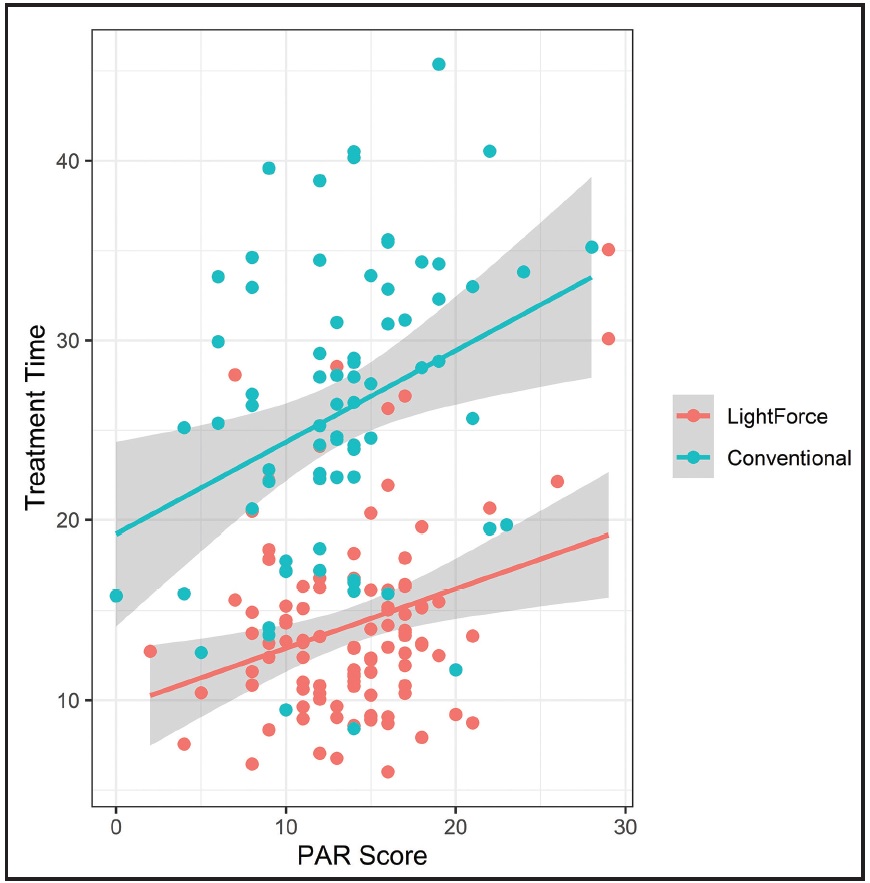
Fig. 6 Scatter plots of treatment time vs. unweighted initial PAR scores in LightForce and conventional-bracket groups. Regression lines are shown for each group with 95% confidence bands.
Variables that can extend treatment time include broken appointments, broken brackets and bands, and individual office procedure variations.7-11 In this study, the reduced number of scheduled appointments needed for LightForce treatment, along with the increased time interval between scheduled appointments, could have improved patient compliance, resulting in fewer broken appointments and a concomitant reduction in treatment time. The reduced number of loose brackets in the LightForce group could also have contributed to the shorter treatment time.
An important variable noted by Fink and Smith in their study of six orthodontic practices was the time spent on detailed finishing procedures.8 In this study, the majority of LightForce subjects were finished with nickel titanium archwires, as compared to about one-third of the conventional subjects (Fig. 5). The ability to complete treatment with nickel titanium wires implies a reduced need for wirebending, which would normally be performed with TMA* or stainless steel wires. The reduction or even elimination of wire-detailing appointments can substantially shorten treatment time.
The quality of results, as measured by the weighted PAR score, was less than 5 for the LightForce group and less than 7 for the conventional-bracket group. Richmond and colleagues considered a PAR score of 5 or less to be an almost ideal occlusion, and a score of 10 or less to be acceptable.6 Therefore, while the difference in the final PAR scores was statistically significant, the clinical difference would be minimal, since both groups finished with nearly ideal or acceptable occlusions on average.
While a prospective study is the gold standard for clinical trials, an inherent problem with this approach is that a predetermined protocol would establish appointment frequency, which could affect the treatment time.2,4 This retrospective study was designed to evaluate group differences in the practice of a single orthodontist, who completed all cases to the same standard without the prior knowledge that a study would be undertaken. There was no defined treatment protocol for either group that would inherently alter the treatment time or affect the scheduling of appointments. Further study is needed to determine how the treatment efficiencies and outcomes would differ in other practitioners’ offices, where there might be different treatment philosophies.
An additional limitation of retrospective studies is that they are prone to selection bias. The present study used only consecutively completed subjects for whom initial digital study models were available. All LightForce patients had initial digital models because they are required for case submission to LightForce; not all conventional subjects had initial digital models. Although this criterion could introduce a selection bias, the initial PAR scores indicated that the LightForce and conventional-bracket cases were similar in severity.
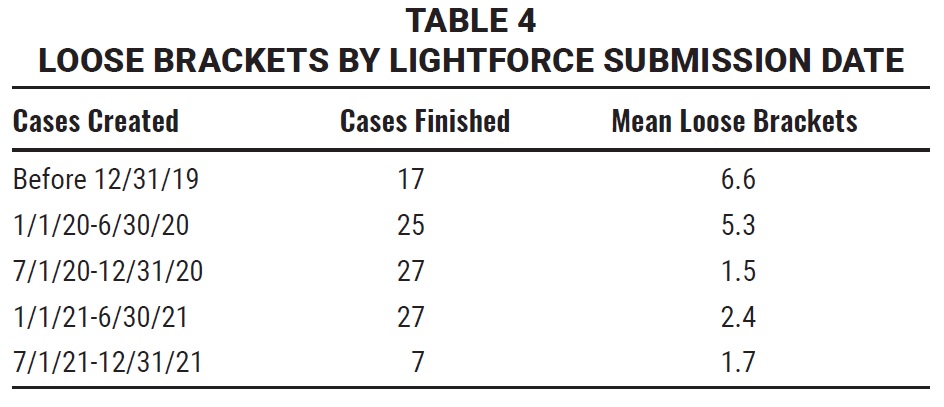
It should be noted that the LightForce bracket system, indirect bonding trays, and proprietary digital treatment-planning software (LightPlan***) were in the early stages of development for the first patients in this study, and were continuously updated and improved during the study period. The clinical impact of such improvements can be seen, for example, in the decreasing number of loose brackets according to when the LightForce case was submitted (Table 4). Cases created before July 1, 2020, averaged 5-6 loose brackets, whereas cases created after that date averaged 1-2 loose brackets. Improvements in the bracket base, indirect bonding trays, and bonding protocols during this time could have enhanced bracket retention and thus contributed to the reduction in loose brackets. Digitally designed indirect-bonded bite turbos, introduced in early 2020, may also have contributed because of a lower initial occlusal force on the mandibular brackets. Another possible explanation for the reduction in loose brackets could be a gradual learning curve in staff experience with the indirect bonding system.
One of the major advantages of digitally designed 3D-printed brackets is the ability to institute improvements almost at the speed of software development. The agile nature of advanced additive manufacturing technology allows for design, bench testing, and clinical implementation of new bracket features within weeks, compared to the months or years needed for traditional manufacturing techniques. This has enabled LightForce to implement many clinically significant changes and improvements to its bracket, hook design, and custom base since the launch of the original bracket in 2019. The LightForce patients in this study were all treated prior to the introduction of custom first- and second-molar tubes. As innovation continues, further research should be conducted to assess the efficacy and efficiency of the LightForce bracket.
ACKNOWLEDGMENT: We would like to thank Ms. Lorretta Zimmerman in Dr. Waldman’s office for her assistance in gathering chart data for this study. We also acknowledge 3Shape for its support in providing OrthoAnalyzer software. This study was supported by LightForce Orthodontics, Burlington, MA.
FOOTNOTES
- *Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- **KLOwen Orthodontics, Richardson, TX; www.klowenortho.com.
- ***LightForce Orthodontics, Burlington, MA; www.lf.co.
- †3M, Monrovia, CA; www.3M.com.
- ‡American Orthodontics, Sheboygan, WI; www.americanortho.com.
- ††3Shape, Copenhagen, Denmark; www.3shape.com.
- ‡‡The SAS Institute, Cary, NC; www.sas.com.
REFERENCES
- 1. Brown, M.W.; Koroluk, L.; Ko, C.C.; Zhang, K.; Chen, M.; and Nguyen, T.: Effectiveness and efficiency of a CAD/CAM orthodontic bracket system, Am. J. Orthod. 148:1067-1074, 2015.
- 2. Hegele, J.; Seitz, L.; Claussen, C.; Baumert, U.; Sabbagh, H.; and Wichelhaus, A.: Clinical effects with customized brackets and CAD/CAM technology: A prospective controlled study, Prog. Orthod. 22:40, 2021.
- 3. Jackers, N.; Maes, N.; Lambert, F.; Albert, A.; and Charavet, C.: Standard vs computer-aided design/computer-aided manufacturing customized self-ligating systems using indirect bonding with both, Angle Orthod. 91:74-80, 2021.
- 4. Penning, E.W.; Peerlings, R.H.J.; Govers, J.D.M.; Rischen, R.J.; Zinad, K.; Bronkhorst, E.M.; Breuning, K.H.; and Kuijpers-Jagtman, A.M.: Orthodontics with customized versus noncustomized appliances: A randomized controlled clinical trial, J. Dent. Res. 96:1498-1504, 2017.
- 5. Weber, D.J. II; Koroluk, L.D.; Phillips, C.; Nguyen, T.; and Proffit, W.R.: Clinical effectiveness and efficiency of customized vs. conventional preadjusted bracket systems, J. Clin. Orthod. 47:261-266, 2013.
- 6. Richmond, S.; Shaw, W.C.; Roberts, C.T.; and Andrews, M.: The PAR Index (Peer Assessment Rating): Methods to determine outcome of orthodontic treatment in terms of improvement and standards, Eur. J. Orthod. 14:180-187, 1992.
- 7. Beckwith, F.R.; Ackerman, R.J. Jr.; Cobb, C.M.; and Tira, D.E.: An evaluation of factors affecting duration of orthodontic treatment, Am. J. Orthod. 115:439-447, 1999.
- 8. Fink, D.F. and Smith, R.J.: The duration of orthodontic treatment, Am. J. Orthod. 102:45-51, 1992.
- 9. Mavreas, D. and Athanasiou, A.E.: Factors affecting the duration of orthodontic treatment: A systematic review, Eur. J. Orthod. 30:386-395, 2008.
- 10. Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; and Harding, W.J.: Factors influencing treatment time in orthodontic patients, Am. J. Orthod. 129:230-238, 2006.
- 11. Vig, P.S.; Weintraub, J.A.; Brown, C.; and Kowalski, C.J.: The duration of orthodontic treatment with and without extractions: A pilot study of five selected practices, Am. J. Orthod. 97:45-51, 1990.





COMMENTS
.