CASE REPORT
Two-Phase Treatment of a Class III with Severe Anterior Open Bite and Hyperdivergent Growth Pattern: A Digital Workflow Option
Patients with anterior open bite tend to exhibit significant skeletal and dentoalveolar maxillary transverse constriction.1-3 When a skeletal Class III malocclusion is involved, early protraction treatment can promote maxillary development.4 Facemask therapy can produce purely skeletal changes, but it also tends to create undesirable side effects such as excessive forward movement, extrusion of the upper molars, and proclination of the upper incisors.5
When associated with maxillary skeletal expansion, the mechanics of Class III therapy seem to rely on simultaneous weakening and opening of the circummaxillary sutures. Recent studies have shown no significant enhancement of maxillary protraction with additional expansion, however, except when the Liou protocol was used.6 To provide an effective and efficient option with minimal side effects, Maino and colleagues developed a protocol for alternating expansion and constriction of the maxillary complex with a hybrid palatal expander anchored to both bone and teeth, followed by facemask therapy.7 A three-dimensional surgical guide was developed for reliable palatal miniscrew insertion.8,9
This case report demonstrates a two-phase approach to treatment of a complex Class III malocclusion in the vertical, transverse, and sagittal dimensions, using the skeletal Alt-RAMEC protocol for Class III (SKAR III) and a completely digital workflow.
Diagnosis and Treatment Planning
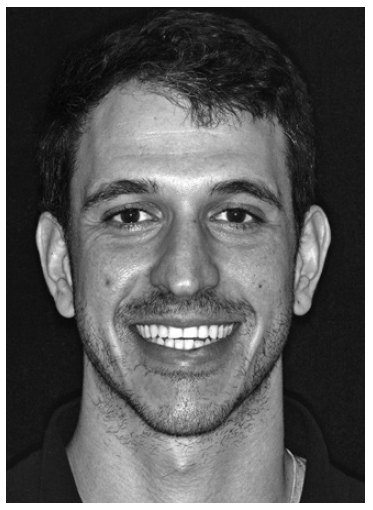
A 9-year-old female presented in the first stage of the transitional dentition (Fig. 1). She had a well-proportioned face with good mandibular symmetry; the upper midline was slightly deviated to the left with respect to the facial midline, and there was a pronounced anterior open bite. The patient also displayed a long lower facial third and a recessive chin. Intraoral examination found maxillary transverse constriction, lower anterior crowding, excessive overjet, and 6mm of negative overbite. A long-term tongue-thrust habit had contributed to the development and perseverance of the open bite (Fig. 1B).
The panoramic radiograph indicated the presence of all permanent teeth at the proper stages of eruption. According to the cephalometric analysis (Table 1), the patient had a hyperdivergent growth pattern (FMA = 29.3°) and a Class I sagittal skeletal relationship (Wits appraisal = 0mm). The upper incisors were proclined with respect to the palatal plane (U1-PP = 116.2°), but the lower incisors were normally inclined with respect to the mandibular plane (IMPA = 95.9°).
One option in this case was to wait until the end of growth to see if the anterior open bite would self-correct; in most cases, however, this condition worsens with growth.10 Another alternative was to perform orthognathic surgery after growth, in conjunction with pre- and postsurgical orthodontics. This would have led to the development of a complex malocclusion with anterior open bite and upper-incisor proclination, causing severe functional and esthetic problems during adolescence. Therefore, an interceptive phase of orthopedic treatment was planned to eliminate the tongue-thrust habit and thus prevent worsening of the malocclusion while promoting optimal development of the masticatory system.
Similar articles from the archive:
- CASE REPORT Mandibular Arch Retraction with Retromolar Skeletal Anchorage in a Class III Open-Bite Patient December 2014
- CASE REPORT Three-Dimensional Treatment Planning and Management of an Asymmetrical Skeletal Class III Malocclusion and Open Bite January 2014
- Early Treatment of Skeletal Class III Open Bite with the Tandem Appliance June 2011
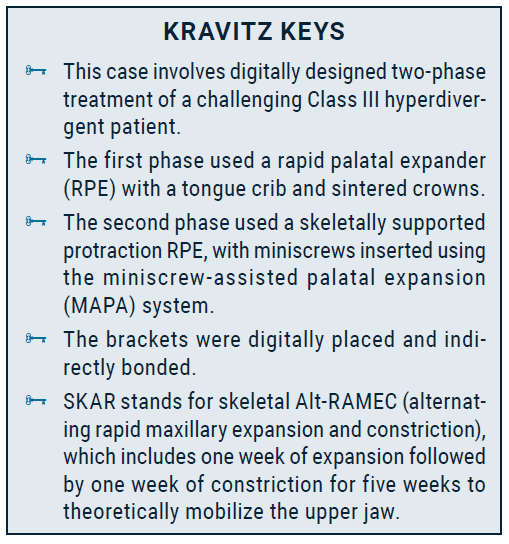
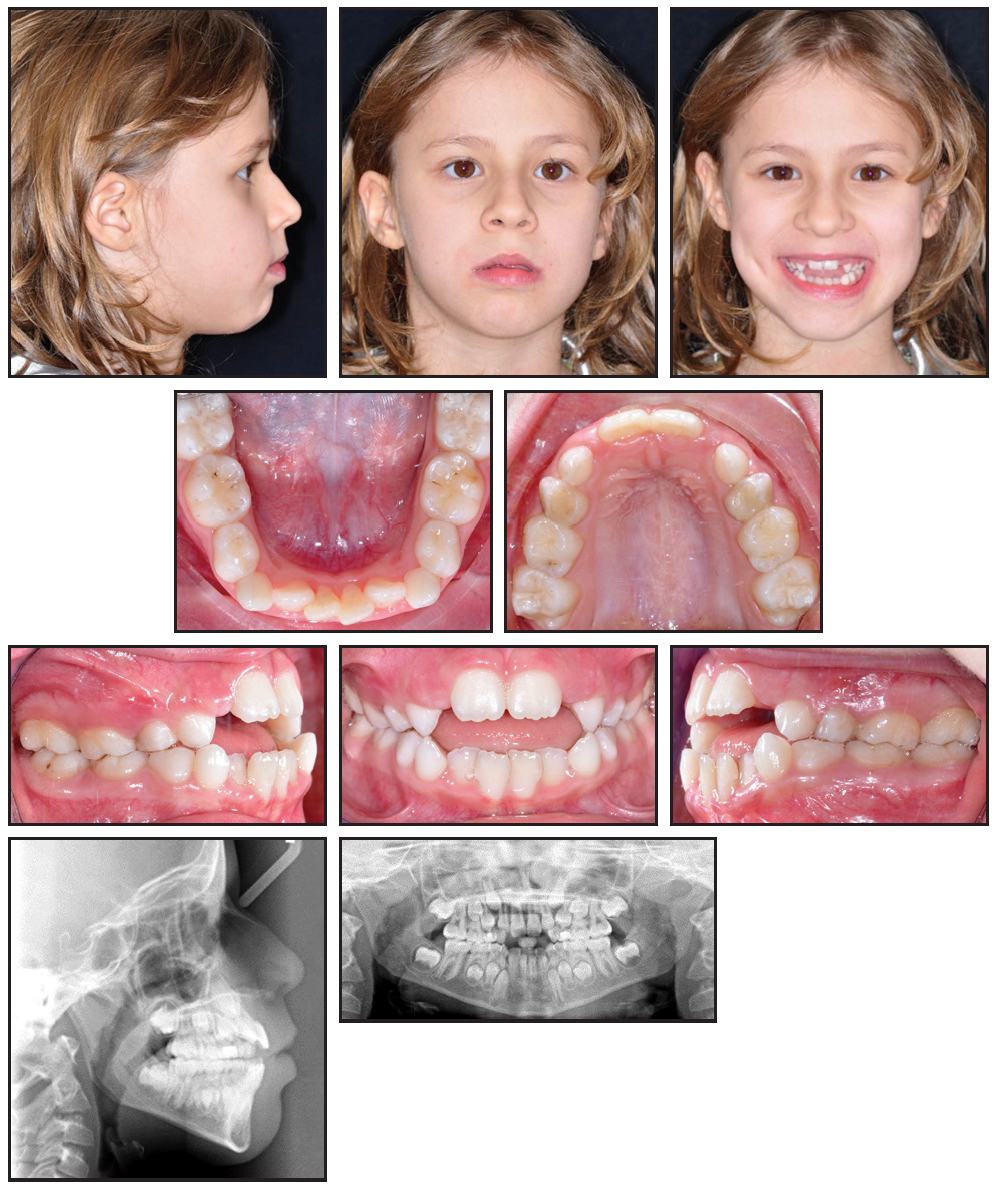
Fig. 1 9-year-old female patient with anterior open bite, midline deviated to left, long lower facial third, excessive overjet, negative overbite, and lower anterior crowding before treatment (continued in next image).
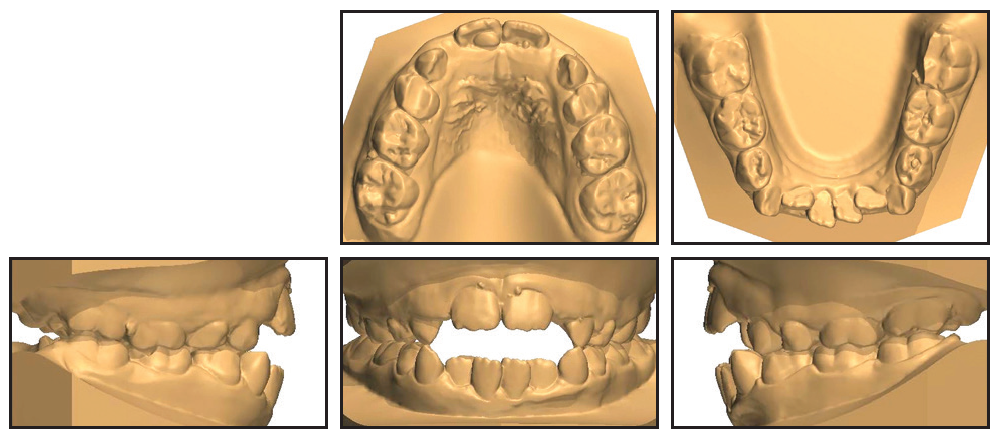
Fig. 1 (cont.) 9-year-old female patient with anterior open bite, midline deviated to left, long lower facial third, excessive overjet, negative overbite, and lower anterior crowding before treatment.
Treatment Progress
For the first phase of treatment, a customized RPE was digitally designed with bite blocks and an anterior tongue crib (Fig. 2A). This would provide the necessary transverse expansion while controlling the vertical dimension (Fig. 3). The tongue crib enabled natural closure of the open bite by blocking the tongue from interpositioning and by correcting its posture.11,12 The RPE was activated once per day for 40 days to obtain an overcorrection of the transverse dimension and resolve the bilateral crossbite of the deciduous canines (Fig. 2B).
The appliance was kept in place for 10 months to stabilize the result (Fig. 4). At the end of this phase, a new lateral cephalogram revealed a hyperdivergent Class III growth pattern (FMA = 33.4°), which was corroborated by familial traits observed in the parents. Cephalometric analysis confirmed a worsening of the sagittal maxillary relationship, with reduced values for both ANB and the Wits appraisal (Table 1).
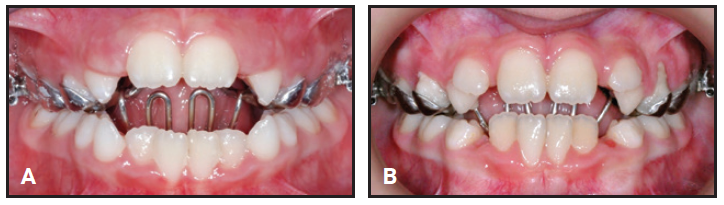
Fig. 2 A. Rapid palatal expander (RPE) placed with tongue crib. B. After 40 daily activations of RPE.
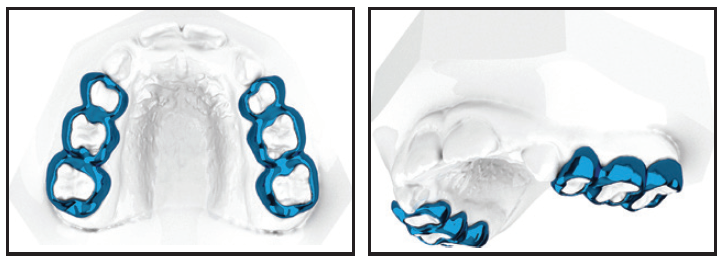
Fig. 3 Digital planning of sintered crowns.

Fig. 4 After 10 months of stabilization.
Eighteen months later, we initiated a second phase of orthopedic treatment to protract the maxilla using the SKAR III protocol. The choice of hybrid skeletal anchorage was based on the objective of maximizing the skeletal correction while avoiding undesirable dental side effects. In the expansion stage of Alt-RAMEC, the anchoring first molars tend to experience buccal tipping, mesialization, and extrusion—all movements that must be minimized in a hyperdivergent growth pattern. The expander in this case was anchored by two 13mm × 2mm anterior palatal miniscrews* and two upper first-molar bands (Fig. 5).7

Fig. 5 RPE anchored by 13mm × 2mm anterior palatal miniscrews* and bands on upper first molars.
The miniscrew positions were determined by superimposing cone-beam computed tomography images on the stereolithographic (STL) image of the digital model (Fig. 6). To ensure safe insertion, a 3D surgical guide was printed using the MAPA system.8
Under the SKAR III protocol, one week of expansion alternated with one week of constriction for five weeks13 (Fig. 7). This mobilized the upper jaw and thus improved the efficiency of a Petit facemask, promoting further expansion and canine eruption. The facemask was used in conjunction with 16oz, 1⁄8" extraoral elastics for five months, until a sagittal Class III overcorrection and an improvement in the profile had been achieved.
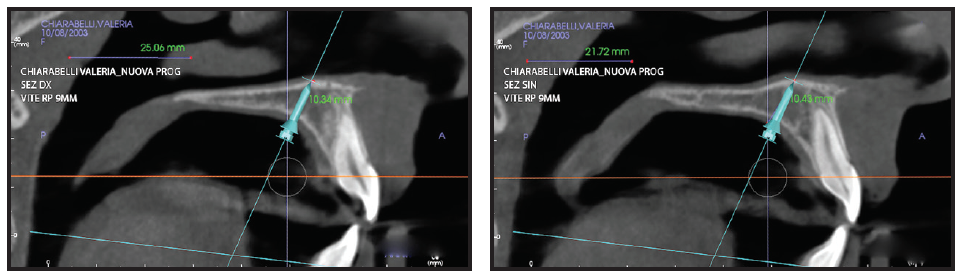
Fig. 6 Miniscrew insertion planning with cone-beam computed tomography.
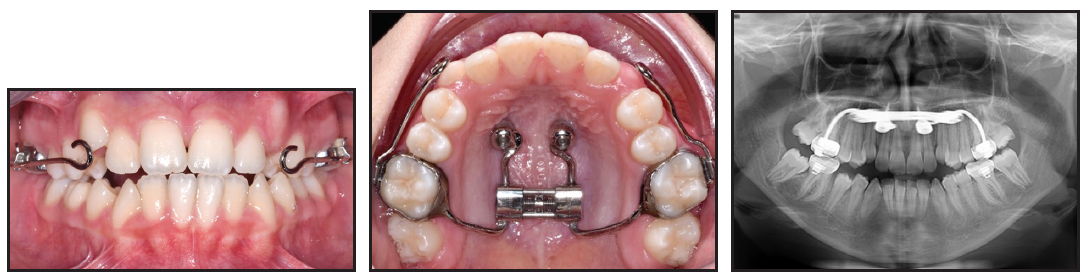
Fig. 7 After five weeks of expansion using skeletal alternating rapid maxillary expansion and constriction protocol for Class III (SKAR III).
Orthodontic treatment proceeded with fixed labial .022" Primo** brackets, using an archwire sequence of .016" and .019" × .025" copper nickel titanium and .019" × .025" stainless steel, to recover the upper canine and to coordinate the relationship between the arches.14,15 X-rays taken after expansion were used to determine the root inclinations for bracket positioning. Digital placement was planned using computer-aided design (CAD), while bonding was performed with a computer-aided manufacturing (CAM) transfer tray (Fig. 8). Direct bonding was needed for the unerupted teeth, the upper and lower first molars (after band removal), and the lower canines, where digital projections were not possible. Fixed appliance treatment lasted one year.
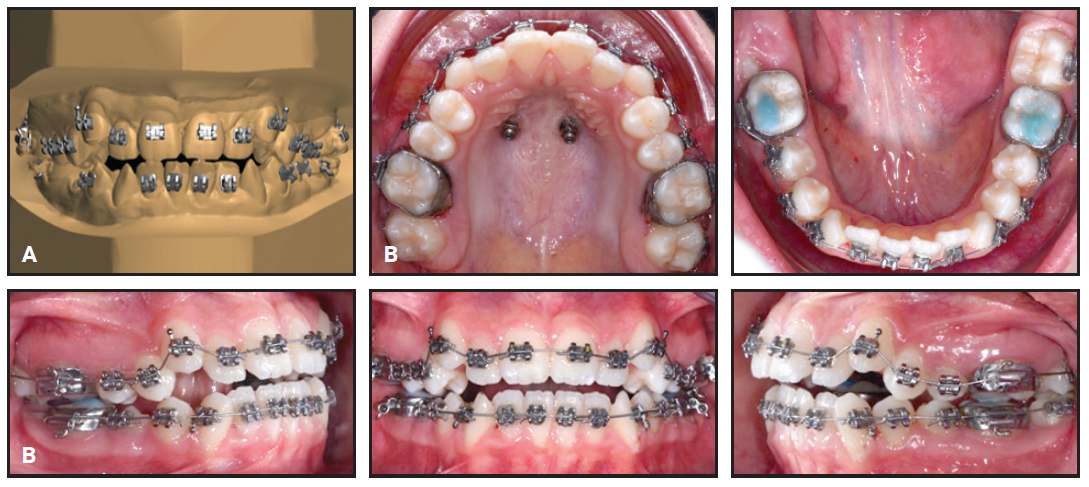
Fig. 8 A. Dental cast for indirect bonding. B. Both arches bonded with .022" Primo** brackets using transfer tray.
Treatment Results
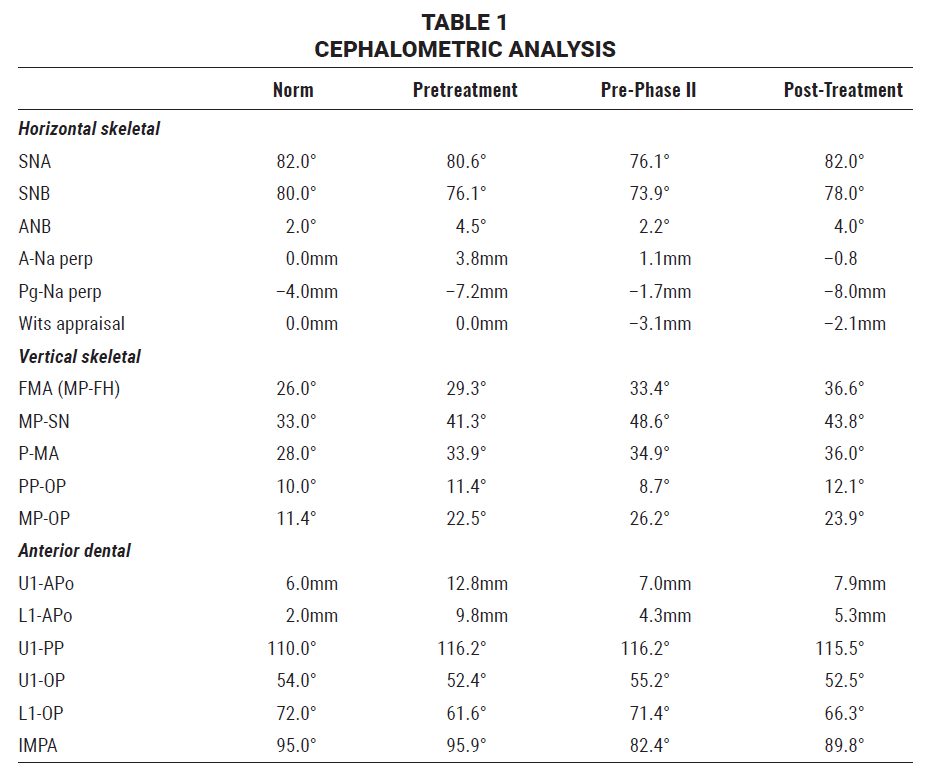
Phase II treatment time was 22 months (Fig. 9A).
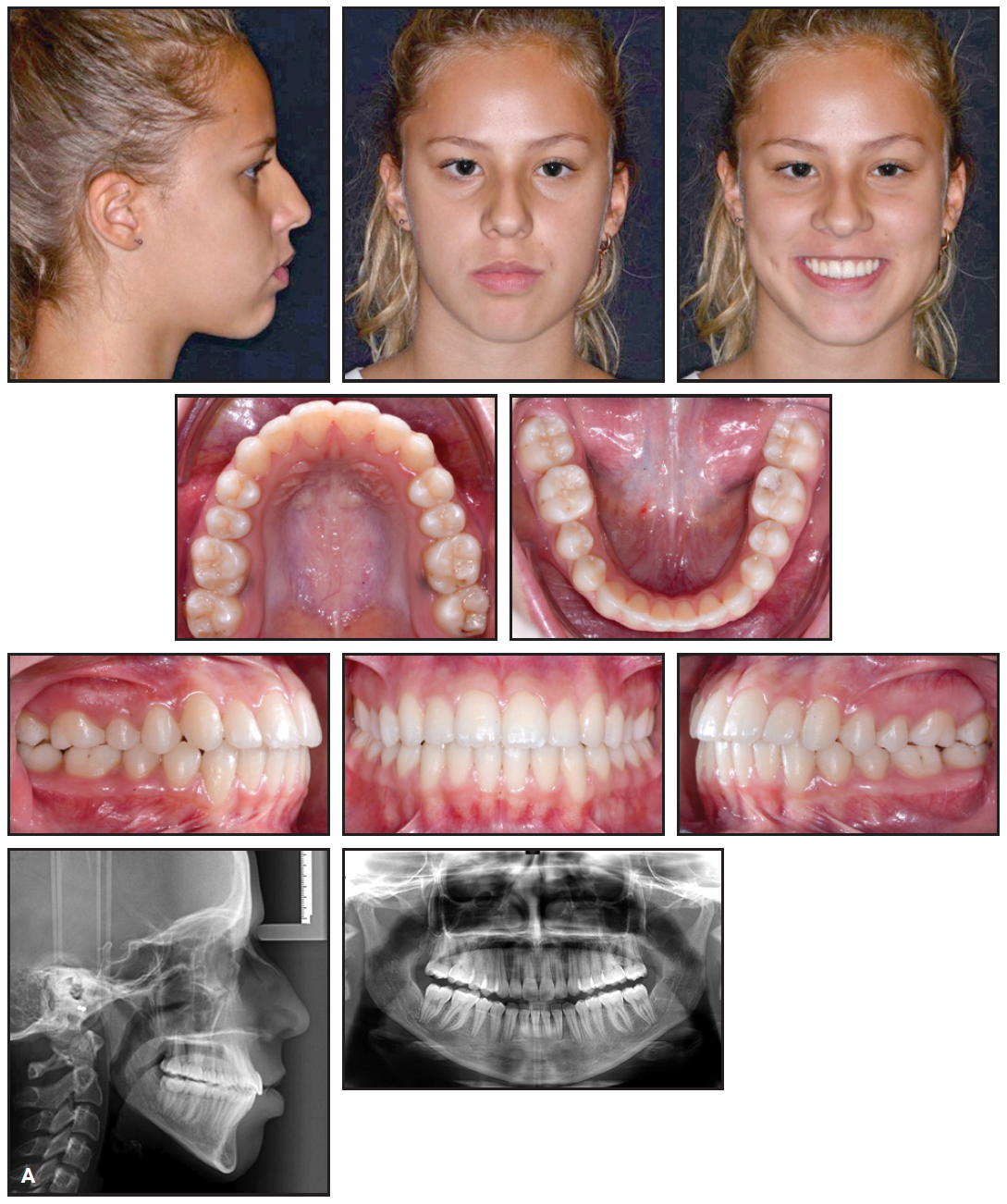
Fig. 9 A. Patient after 22 months of Phase II treatment (continued in next image).
The patient had a pleasant smile with ideal incisor exposure and no black corridors. Although she displayed a slightly accentuated nasolabial angle and an increased lower facial third, in accordance with her growth pattern, she had a stable Class I bilateral sagittal relationship and a centered dental midline. Ideal overjet and overbite were established, and the marginal crests were leveled. Final dental casts confirmed that all initial treatment objectives had been achieved, and the final panoramic x-ray showed root parallelism with no evident resorption. Final cephalometric analysis (Table 1) indicated an improvement in the maxillary sagittal relationship (ANB = 4.0°, Wits appraisal = –2.1mm), with a slightly buccal upper-incisor inclination with respect to the palatal plane (U1-PP = 115.5°) and good control of IMPA (89.8°). Superimposition of pre- and post-treatment cephalometric tracings according to Bjork16,17 highlighted an orthopedic effect as a result of the facemask use, with forward and downward movement of the upper maxilla. Moreover, the growth pattern resulted in a mandibular post-rotation with a predominantly vertical component. Despite the first orthopedic phase, the orthodontic treatment of the Class III relationship led to some dental compensation, including increased buccal inclination of the upper incisors and lingual inclination of the lower incisors (Fig. 9B).
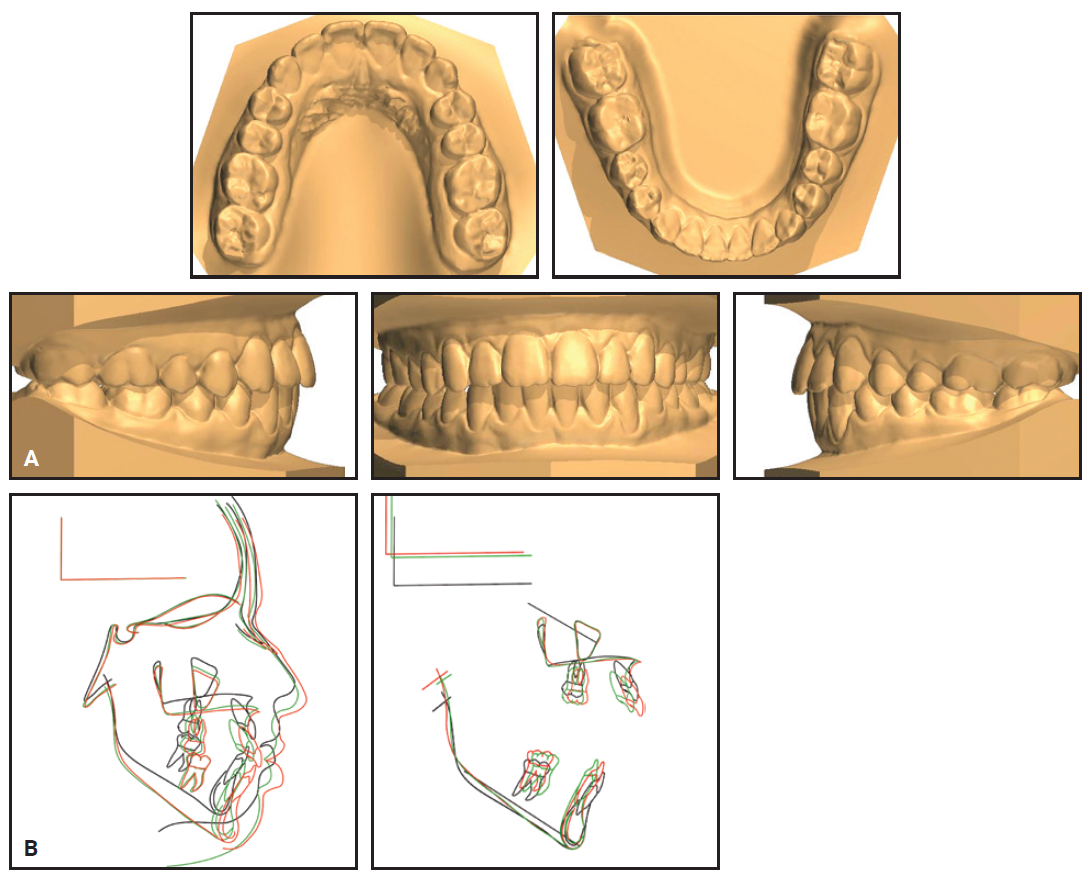
Fig. 9 (cont.) A. Patient after 22 months of Phase II treatment. B. Superimposition of pretreatment (black), pre-Phase II (green), and post-treatment (red) cephalometric tracings.
One year after treatment, the results were stable (Fig. 10).

Fig. 10 Patient one year after treatment.
Discussion
The use of an anterior tongue crib in the initial orthopedic phase was essential in correcting this patient’s parafunctional habits and anterior open bite.18 Bite blocks are commonly used in hyperdivergent patients to control posterior eruption, to facilitate anterior skeletal growth, and to maintain posterior facial height.19 Timing is an important factor in the correction of Class III malocclusion, since sutural ossification can inhibit a response to facemask treatment in adults.20 Despite the general effectiveness of early treatment with a facemask and RPE,13 however, a certain percentage of patients experience unfavorable growth with excessive clockwise mandibular rotation.21
The SKAR III protocol, with its repeated opening and closing of the expansion screw, increases mobilization of the circummaxillary sutures and thus enhances the appliance’s skeletal effects.13 Skeletal anchorage can prevent such unwanted dental side effects as mesial movement and extrusion of the upper molars, as well as proclination of the upper incisors from the indirect force.22 By maximizing the skeletal effects of the orthopedic appliance, we can often avoid orthognathic surgery, with its risks, expense, and increased treatment time.
Indirect bonding can ensure more accurate and precise bracket placement in less chairtime than with direct bonding.15,23 The CAD/CAM system used in our patient minimized positioning errors, with no rebracketing and only one archwire bend needed to refine the case. Digital indirect bonding can reportedly reduce orthodontic treatment time by 26% over traditional indirect bonding.24 In fact, the digital workflow was the key to successful resolution of this complex case. Thanks to careful treatment timing and accurate digital planning, the effectiveness of the appliances was maximized while unwanted side effects were minimized.
FOOTNOTES
- *K2 Regular Plus, registered trademark of HDC, Thiene, Italy; hdc-italy.com.
- **Registered trademark of Sweden & Martina, Due Carrare, Padova, Italy; www.sweden-martinainc.com.
REFERENCES
- 1. Tausche, E.; Luck, O.; and Harzer, W.: Prevalence of malocclusions in the early mixed dentition and orthodontic treatment need, Eur. J. Orthod. 26:237-244, 2004.
- 2. Silvestrini-Biavati, A.; Salamone, S.; Silvestrini-Biavati, F.; Agostino, P.; and Ugolini, A.: Anterior open-bite and sucking habits in Italian preschool children, Eur. J. Paediat. Dent. 17:43-46, 2016.
- 3. Ballanti, F.; Franchi, L.; and Cozza, P.: Transverse dentoskeletal features of anterior open bite in the mixed dentition, Angle Orthod. 79:615-620, 2009.
- 4. Baccetti, T.; Franchi, L.; and McNamara, J.A. Jr.: Treatment and posttreatment craniofacial changes after rapid maxillary expansion and facemask therapy, Am. J. Orthod. 118:404-413, 2000.
- 5. Cordasco, G.; Matarese, G.; Rustico, L.; Fastuca, S.; Caprioglio, A.; Lindauer, S.J.; and Nucera, R.: Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: A systematic review and meta-analysis, Orthod. Craniofac. Res. 17:133-143, 2014.
- 6. Foersch, M.; Jacobs, C.; Wriedt, S.; Hechtner, M.; and Wehrbein, H.: Effectiveness of maxillary protraction using facemask with or without maxillary expansion: A systematic review and meta-analysis, Clin. Oral Investig. 19:1181-1192, 2015.
- 7. Maino, G.; Turci, Y.; Arreghini, A.; Paoletto, E.; Siciliani, G.; and Lombardo, L.: Skeletal and dentoalveolar effects of hybrid rapid palatal expansion and facemask treatment in growing skeletal Class III patients, Am. J. Orthod. 153:262-268, 2018.
- 8. Maino, G.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: MAPA: A new high-precision 3D method of palatal miniscrew placement, Eur. J. Clin. Orthod. 3:41-47, 2015.
- 9. Maino, B.G.; Paoletto, E.; Lombardo, L. III; and Siciliani, G.: A three-dimensional digital insertion guide for palatal miniscrew placement, J. Clin. Orthod. 50:12-22, 2016.
- 10. Pisani, L.; Bonaccorso, L.; Fastuca, R.; Spena, R.; Lombardo, L.; and Caprioglio, A.: Systematic review for orthodontic and orthopedic treatments for anterior open bite in the mixed dentition, Prog. Orthod. 17:28, 2016.
- 11. Franco, F.C.M.; Araùjo, T.M.; and Habib, F.: Lingual spurs: A resource for the treatment of anterior open bite [in Portuguese], Ortod. Gaùch. 5:6-12, 2001.
- 12. Huang, G.J.; Justus, R.; Kennedy, D.B.; and Kokich, V.G.: Stability of anterior openbite treated with crib therapy, Angle Orthod. 60:17-24, 1990.
- 13. Liou, E.J.: Effective maxillary orthopedic protraction for growing Class III patients: A clinical application simulates distraction osteogenesis, Prog. Orthod. 6:154-171, 2005.
- 14. Mah, J. and Sachdeva, R.: Computer-assisted orthodontic treatment: The SureSmile process, Am. J. Orthod. 120:85-87, 2001.
- 15. Silverman, E.; Cohen, M.; Gianelly, A.A.; and Dietz, V.S.: A universal direct bonding system for both metal and plastic brackets, Am. J. Orthod. 62:236-244, 1972.
- 16. Björk, A. and Skieller, V.: Growth of the maxilla in three dimensions as revealed radiographically by the implant method, Br. J. Orthod. 4:53-64, 1977.
- 17. Björk, A.: Prediction of mandibular growth rotation, Am. J. Orthod. 55:585-599, 1969.
- 18. Cozza, P.; Mucedero, M.; Baccetti, T.; and Franchi, L.: Treatment and posttreatment effects of quad-helix/crib therapy of dentoskeletal open bite, Angle Orthod. 77:640-645, 2007.
- 19. McLaughlin, R.P.; Bennett, J.C.; and Trevisi, H.: Systemized Orthodontic Treatment Mechanics, 1st ed., Mosby, St. Louis, 2001.
- 20. Melsen, B. and Melsen, F.: The postnatal development of the palatomaxillary region studied on human autopsy material, Am. J. Orthod. 82:329-342, 1982.
- 21. Baccetti, T.; Franchi, L.; and McNamara, J.A. Jr.: Cephalometric variables predicting the long-term success or failure of combined rapid maxillary expansion and facial mask therapy, Am. J. Orthod. 126:16-22, 2004.
- 22. Franchi, L.; Baccetti, T.; and McNamara, J.A. Jr.: Postpubertal assessment of treatment timing for maxillary expansion and protraction therapy followed by fixed appliances, Am. J. Orthod. 126:555-568, 2004.
- 23. Brown, M.W.; Koroluk, L.; Ko, C.C.; Zhang, K.; Chen, M.; and Nguyen, T.: Effectiveness and efficiency of a CAD/CAM orthodontic bracket system, Am. J. Orthod. 148:1067-1074, 2015.
- 24. Jackers, N.; Maes, N.; Lambert, F.; Albert, A.; and Charavet, C.: Standard vs computer-aided design/computer-aided manufacturing customized self-ligating systems using indirect bonding with both, Angle Orthod. 91:74-80, 2021.





COMMENTS
.