Orthodontic Space Closure vs. Implant-Borne Crowns in Patients with Congenitally Missing Maxillary Lateral Incisors
Considering that the incidence of agenesis of one or both maxillary lateral incisors is .8-2% in the general population,1,2 orthodontic treatment involving either space closure by canine substitution or space opening and subsequent implant-borne crown substitution is relatively common.
Orthodontic space closure can produce excellent long-term treatment results when performed with optimal torque control, differential extrusion of the canines and intrusion of the first premolars, bleaching and subtractive recontouring of the canine cusps and buccal curvature, and additive reshaping of the six anterior teeth using either composite or ceramic veneers.3-9 Space closure allows the entire treatment to be finished within a relatively short time after orthodontic therapy, and the resulting dentition can adapt to continuous facial changes over the patient’s life.10
Recent evidence also suggests that good function, pleasing esthetics, and long-term stability of implant-supported crowns in the anterior maxilla can be achieved with accurate three-dimensional, prosthodontic-driven implant placement and hard- and soft-tissue enhancement procedures.11-17 Implant placement in the esthetic zone risks the development of infraocclusion, however, because of natural dentofacial changes over time. Consequent problems with dental esthetics and periodontal health can be resolved only with complex interdisciplinary approaches such as corticotomy and distraction followed by crown replacement.18-23
Similar articles from the archive:
Over the last decade, substantial improvements have been made in implantology, mucogingival surgery, abutment design, and prosthodontic materials, and more systematic protocols have been established to enhance the performance of implant-borne crowns.24-27 Long-term success seems to be correlated with proper implant placement, following the “2B-3D” rule (Fig. 1).
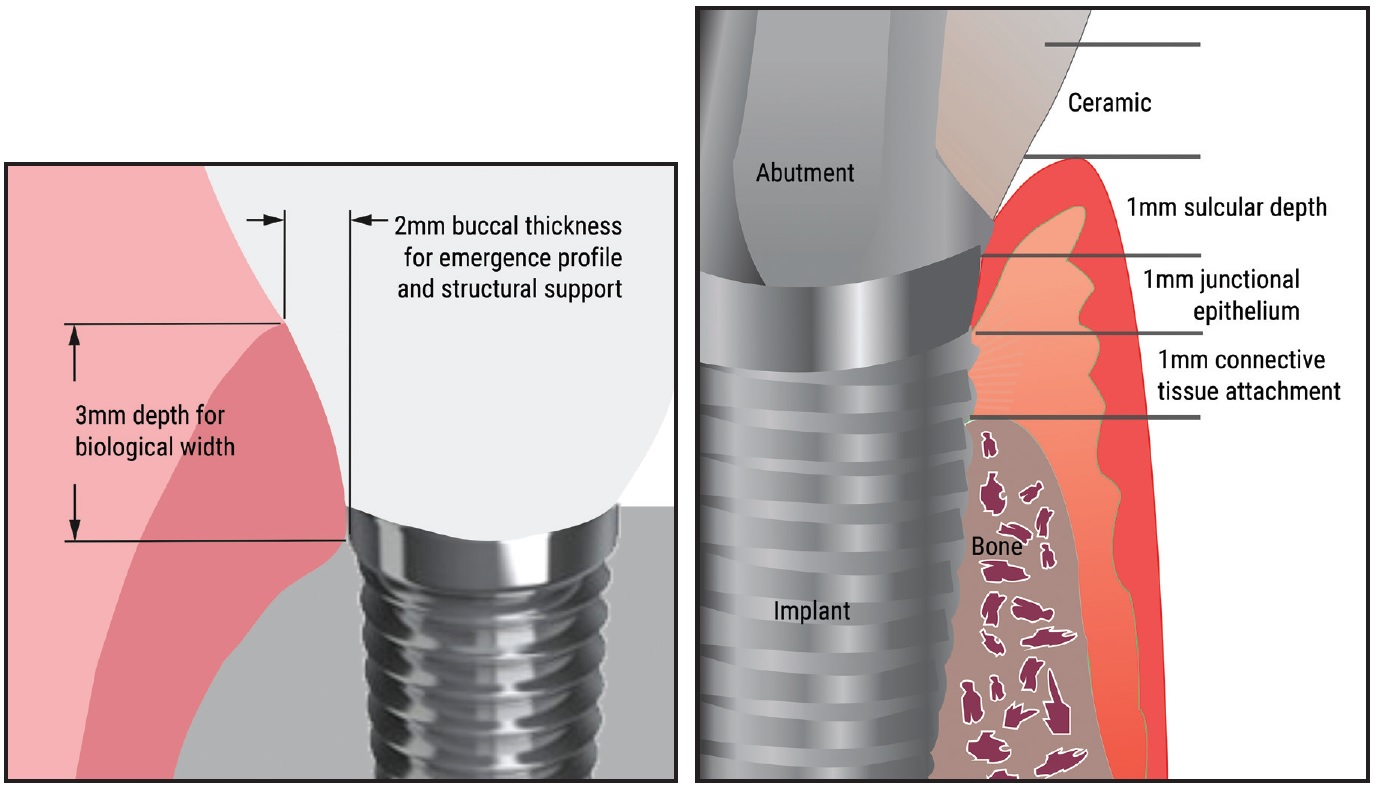
Fig. 1 “2B-3D” rule for implant placement.
Studies have shown that 2mm of buccal bone thickness is needed to provide a sufficient collateral blood supply from both the cortical bone and the adjacent connective tissue.17,28 In addition, the implant head must be placed 3mm deep, relative to the future labial crown margin, to allow the development of normal biological width and a physiological emergence profile for the ceramics, thus ensuring excellent esthetics.29,30
In the absence of a 2mm facial bony wall, a routine simultaneous bone graft before or during implant insertion is advocated. Such a graft will cover any osseous fenestration or dehiscence that could lead to an unesthetic shallow depression over the implant and thus increase the risk of subsequent midfacial gingival recession.31-33 If the gingival biotype is thin, a submucosal tissue graft harvested from the palate can create a natural-looking facial gingival emergence profile. The thicker peri-implant mucosa promotes a complete fill of the mesial and distal papillae and helps prevent midfacial gingival recessions and tissue discoloration, which have been reported as common sequelae of implant-supported crowns.34-36
The aim of the present investigation was to evaluate whether proper placement of implants as substitutes for congenitally missing upper lateral incisors, using concomitant hard- and soft-tissue grafts in the presence of a thin periodontal biotype and supported by adequate peri-implant molding, can establish and maintain excellent esthetic and periodontal conditions for at least five years. We compared these results to those of orthodontic space closure with canine substitution and recontouring after a similar post-treatment period and assessed patient satisfaction with the final outcomes in both groups.
Materials and Methods
This retrospective observational study was carried out with the approval of the Research Ethics Committee of the University of Ferrara. Two groups of patients treated consecutively in the private practice of Drs. Schneider and Moser were evaluated. All active orthodontic treatments and prosthodontic work were completed between August 2006 and October 2011. The inclusion criteria were agenesis of one or both upper lateral incisors and completion of treatment at least five years before the follow-up date. Patients with syndromes or cleft palate, any systematic or periodontal diseases, or history of heavy smoking were excluded.
The first group consisted of 16 patients (13 females, three males) who had been treated with full fixed appliances and orthodontic space closure (OSC) to replace their congenitally missing lateral incisors (Fig. 2).
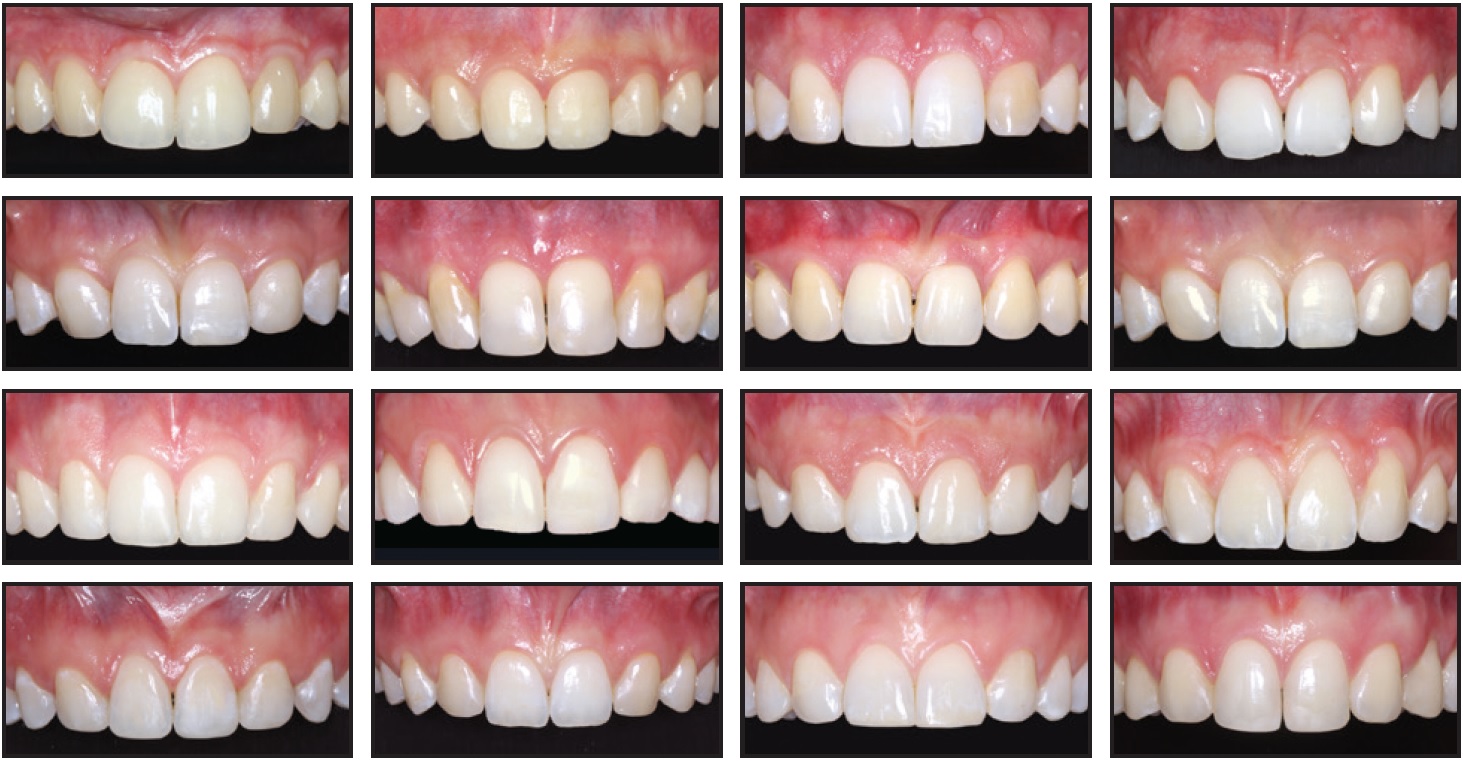
Fig. 2 Orthodontic space closure group: 13 female and three male patients after treatment with full fixed appliances and space closure.
Fifteen of these patients had bilateral agenesis of the lateral incisors; one female patient presented with agenesis of the upper right lateral incisor and a peg-shaped contralateral incisor, which was extracted. The mesialized canines were intruded and sequentially reshaped, and most of the premolars were intruded as described by Rosa and Zachrisson.4,7 After the active phase of treatment, all canines were bleached and restored with composite material. Composite build-ups were applied to the intruded premolars for crown lengthening and to achieve solid intercuspation.
Lingual retainers made of .019" Respond* wire were bonded to the six upper and lower anterior teeth in each OSC patient. Upper fixed retainers were still in place in 13 patients at follow-up, and lower fixed retainers remained in all 16 patients.
The second group of 16 patients (10 females, six males) had been treated with full fixed appliances for orthodontic space opening and subsequent insertion of implant-borne crowns (IMP) in place of their congenitally missing upper lateral incisors (Fig. 3).

Fig. 3 Implant group: 10 female and six male patients after treatment with full fixed appliances and placement of implant-borne crowns.
Except for one patient who received a submerged implant with delayed loading during the final stage of orthodontic treatment, all implants were placed after removal of the fixed appliances to allow immediate insertion of provisional resin crowns. All patients received second provisional crowns and at least three months of molding and maturation of the peri-implant tissues before final restorations were inserted.37-39 The final implants were made of zirconia-ceramic.
Any patient with a facial bony wall of less than 2mm upon implant insertion underwent concomitant augmentation of the alveolar crest with autologous bone (two cases) or with deproteinized bovine bone mineral (DBBM) particles (eight cases), which have demonstrated excellent osteoconductivity and a low substitution rate over time.31,32 Any patient who presented with a thin gingival biotype received either a concomitant connective-tissue graft (three cases) or a combined hard- and soft-tissue graft (two cases) upon implant insertion. A second soft-tissue graft was performed in a single patient to recuperate a residual shallow vestibular impression of the ridge. All implants, grafts, and crowns were performed by the same experienced dentist, Dr. Pellitteri.
For retention in the upper arch, a 1-1 bonded lingual .019" Respond wire and a Hawley retainer with resin pontics for intermediate replacement of the congenitally missing incisors were delivered. In the lower arch, a 3-3 lingual .019" Respond retainer was bonded. All upper and lower fixed lingual retainers were still in place at the time of follow-up.
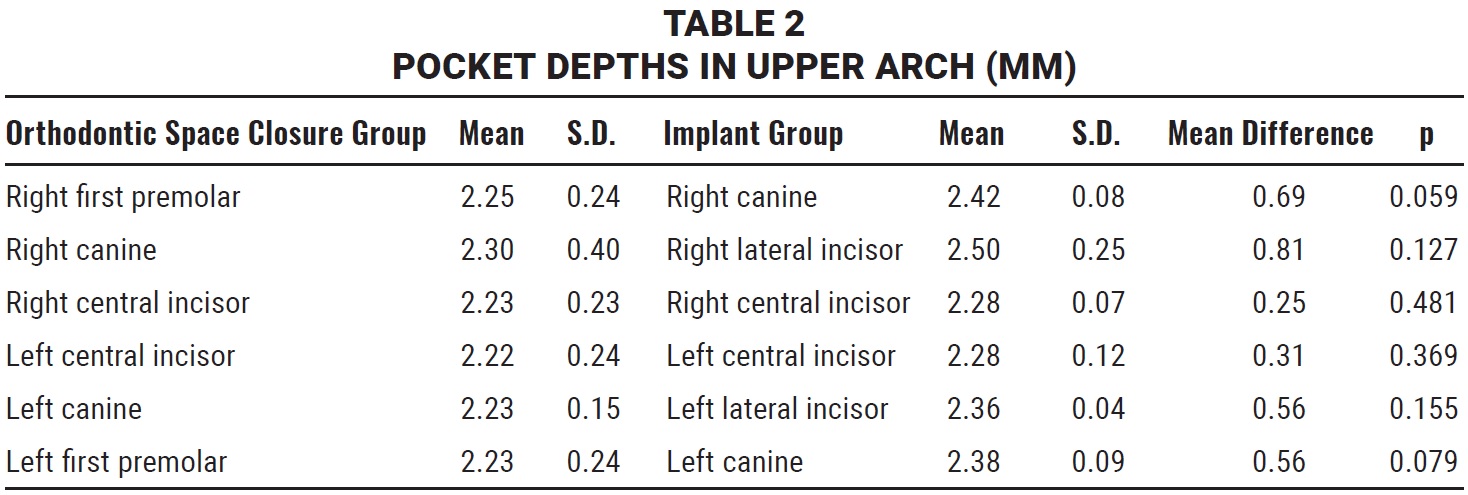
In both patient groups, the follow-up visit included evaluation of the facial and palatal plaque index (PI) according to Quigley and Hein,40 probing depth at four sites (mesial, distal, midfacial, and palatal) per tooth, dichotomous scores for bleeding on probing within 15 seconds (0 = no bleeding, 1 = bleeding), and gingival marginal recession of the six upper anterior teeth.41-44
In the IMP group, periapical radiographs were taken with the parallel technique at final crown delivery (baseline, T1) and at follow-up (T2) for evaluation of the crestal bone levels around the implants (Fig. 4). To calculate the change from T1 to T2, the distances from the crown-abutment junction to the first visible mesial and distal bone-to-implant contacts were measured at each time point.45,46 The radiographs were calibrated by adjusting them to the actual length of the various implants using the Dolphin Imaging 11.9 Annotations** program. Calibrated frontal intraoral photographs in maximum intercuspation, centered at the upper dental midline and parallel and slightly superior to the occlusal plane, were used to assess the development of visible infraocclusion between T1 and T2 (Fig. 5). All photographs were taken with a Canon EOS 700D*** digital camera using an EF 100mm f/2.8 Macro USM lens and Macro Ring Lite MR-14 EXII flash.
In the IMP group, modified Pink Esthetic Score (PES) and White Esthetic Score (WES) scales, which have proven to be reliable and reproducible,17,47-50 were used for objective professional esthetic evaluation of the implant-borne restorations. The PES index includes assessment of the mesial and distal papillae, contour and level of the facial mucosa, and facial root convexity of the implant site (Fig. 6), with a score of 0-2 assigned to each variable (Table 1). Any difference between the color of soft tissue over the implant and that around the natural teeth was also recorded. The WES index focuses on the crown of the implant restoration compared with the contralateral natural tooth, evaluating general tooth form; tooth proportion (outline and volume of the crown); color, including hue and value; texture; and translucency or characterization (Fig. 7). A score of 0 (major discrepancies), 1 (minor discrepancies), or 2 (no difference) is assigned to each parameter. Because both the PES and WES have highest possible totals of 10, the maximum PES + WES value is 20.
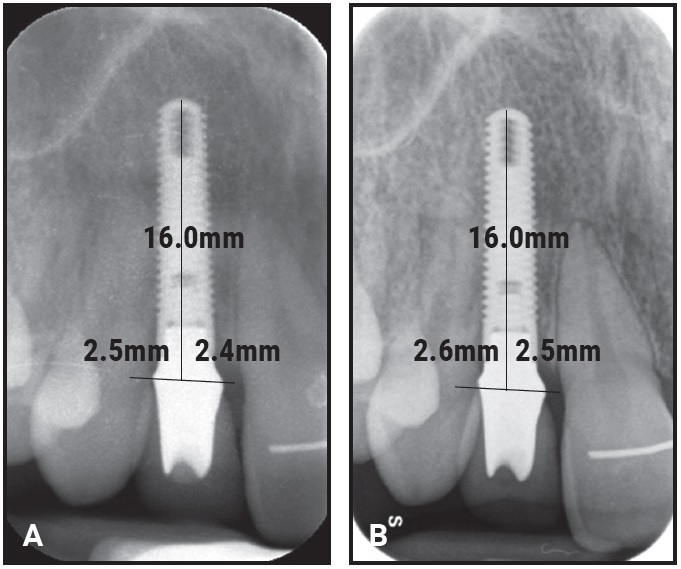
Fig. 4 Example of periapical radiographs used to measure distances from crown-abutment junction to first visible mesial and distal bone-to-implant contacts at baseline (A) and follow-up (B).
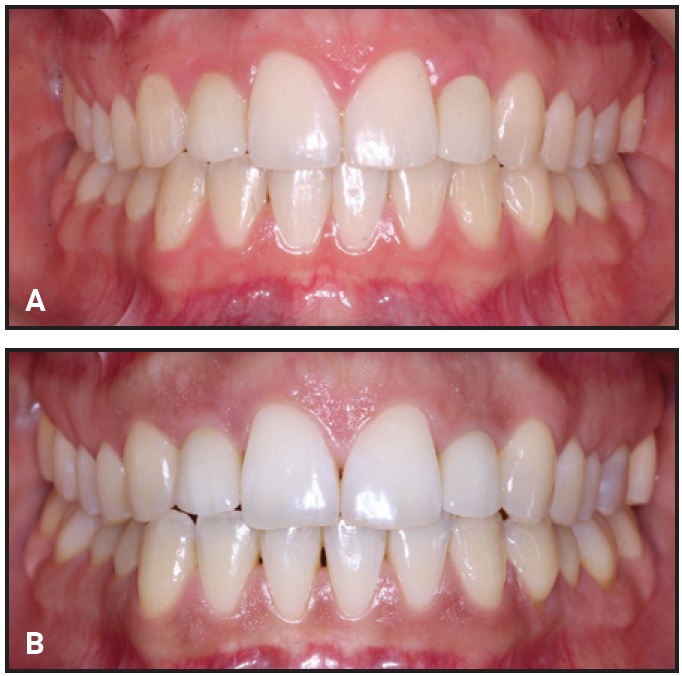
Fig. 5 Examples of calibrated intraoral photographs used for clinical assessment of visible infraocclusion between baseline (A) and follow-up (B).

Fig. 6 Pink Esthetic Scores (1 = mesial papilla, 2 = distal papilla, 3 = soft-tissue contour, 4 = soft-tissue level, 5 = alveolar process).
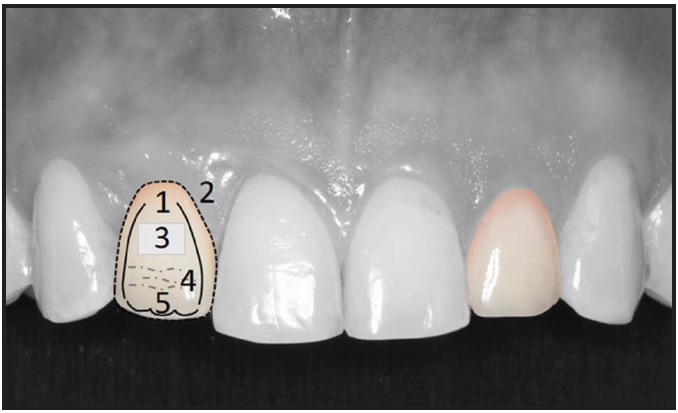
Fig. 7 White Esthetic Scores (1 = tooth form, 2 = outline and volume, 3 = color: hue and value, 4 = surface, 5 = translucency).
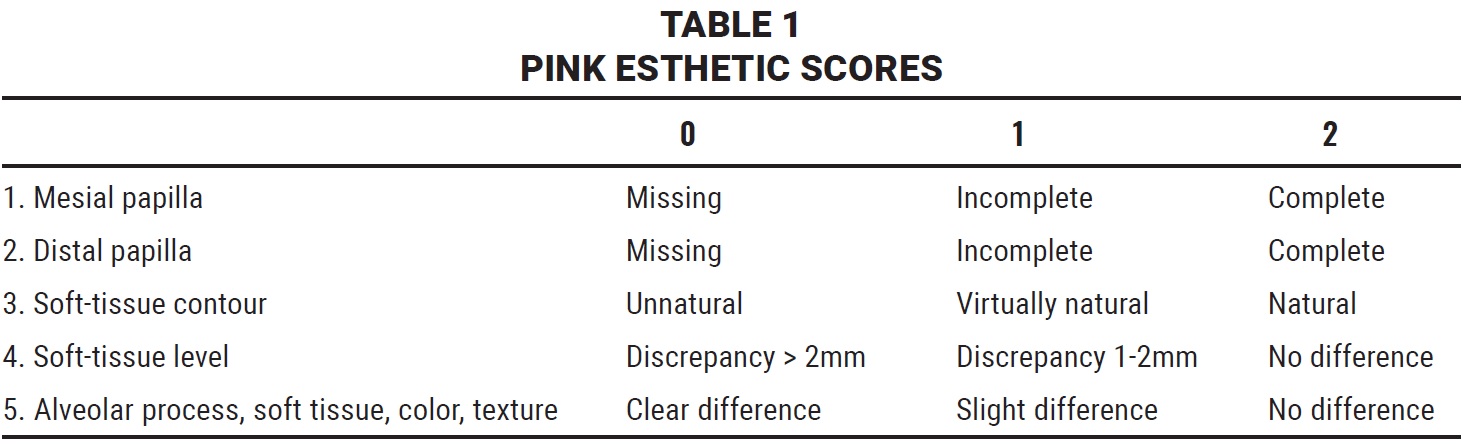
A score of 0 (major discrepancies), 1 (minor discrepancies), or 2 (no difference) is assigned to each parameter. Because both the PES and WES have highest possible totals of 10, the maximum PES + WES value is 20.
In patients with unilateral implant-supported crowns, the contralateral natural lateral incisors served as reference teeth. In patients with bilateral agenesis of the lateral incisors, the contralateral implants were used as references for evaluation of overall symmetry and harmony of the pink and white tissues. In addition, close-up photographs of all implant sites and the contralateral teeth allowed for a more detailed evaluation of papillary fill (Fig. 8).
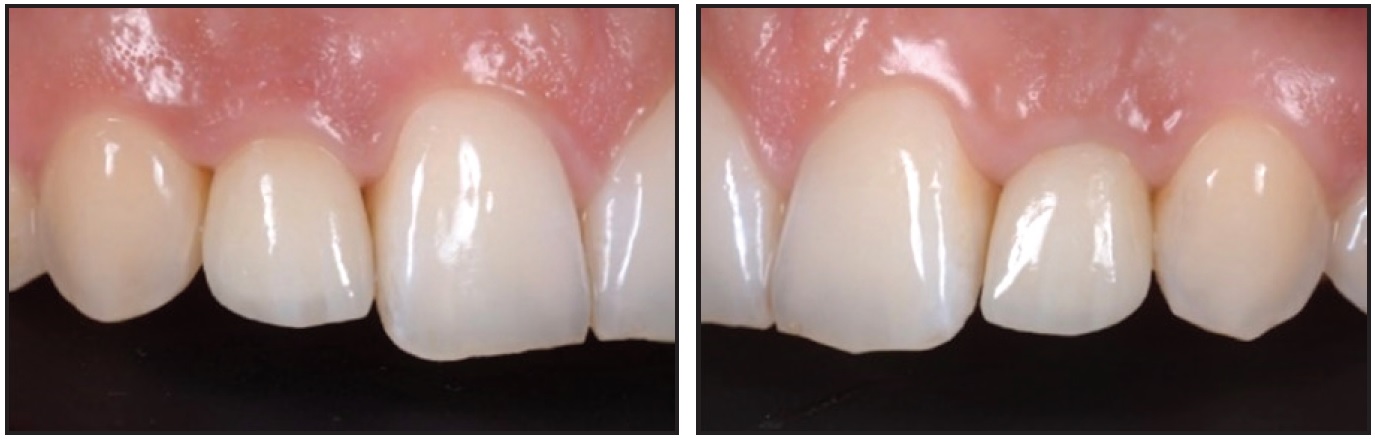
Fig. 8 Examples of additional close-up photographs used to evaluate mesial and distal papillary fill.
The PES and WES criteria were also applied to assess the impact of the mesialized and reshaped canines on white and pink tissue esthetics in the OSC group. All intraoral photographs were assessed on a 42" monitor screen† by an independent examiner who was familiar with the PES and WES parameters but was not part of the interdisciplinary treatment team. To avoid bias and ensure reproducibility of the measurements, the assessment was performed a second time two weeks later with a reversed order of the photographs.
Patient satisfaction with the overall esthetics of the upper front teeth was assessed on a horizontal 100mm visual analog scale (VAS) ranging from 0 (totally unsatisfied) to 100 (completely satisfied). The questionnaire was accompanied by simple, precise instructions for marking the degree of satisfaction on the calibrated line, and an example was provided to explain the VAS.51,52
Statistical Analysis
Analysis was performed using SPSS‡ version 22.0 and GraphPad Prism†† version 6.0. Differences in patient age at T1 and T2 and in observation time between the OSC and IMP groups were assessed with the Mann-Whitney U test, as were the PI and bleeding on probing. Differences between the groups in the frequency of recessions were analyzed with a chi-square test. Probing depth and severity of recessions were evaluated using multivariate analysis of variance (MANOVA) with six dependent variables. Differences between the mesial and distal bone levels adjacent to the implants at T1 and T2 were analyzed with a repeated-measures analysis of variance (ANOVA).
Reproducibility of all PES and WES variables was verified using the Wilcoxon test for paired data. The MANOVA test with dependent variables was applied to compare individual PES and WES variables with unbalanced data (32 sites in the OSC group and 20 in the IMP group) and the total PES + WES values with balanced data (16 patients in each group). The Mann-Whitney U test was used to compare VAS scores between the two groups, and the correlation between PES + WES and VAS was evaluated with a one-tailed Spearman test.
Results were considered statistically significant at the level of p < .05.
Results
Mean patient age was significantly higher in the IMP group at the end of treatment (24 years, 6 months) and at follow-up (30 years, 1 month) than in the OSC group (20 years, 0 months, and 26 years, 4 months; p = .004 and .010, respectively)—a logical outcome considering implants could not be placed until the end of growth. Differences between the mean observation times were not significant (5 years, 9 months, vs. 6 years, 4 months; p = .150).
In the OSC group, eight patients showed noticeable color differences that required repeated canine bleaching during the observation period (five to 10 years). In two patients, the mesialized left canines became nonvital due to obliteration of the pulp. Five patients had to undergo repair of partially fractured or abraded composite restorations of the canines, while four needed repair of the premolar cusps.
In the IMP group, all implants were firmly integrated without any suppuration in the implant sulcus or any signs of peri-implant tissue inflammation. No prosthodontic failures occurred.
PI assessment of 192 sites in each group evidenced a high standard of oral hygiene. Separate flecks of plaque at the cervical margin (grade 1) could be detected on only 13 surfaces (6.8%) in the OSC group and 14 surfaces (7.3%) in the IMP group. Of the 384 examined sites per patient sample, only nine (2.5%) in the OSC group and 11 (2.9%) in the IMP group showed bleeding within 15 seconds after probing. The differences between groups were not statistically significant either for PI (p = .794) or for bleeding on probing (p = .521).
Only one patient in the IMP group exhibited a pocket depth of as much as 4mm on the mesial and distal aspects of the implant. All other evaluated sites in both groups had pocket depths between 2-3mm, with overall means of 2.24mm in the OSC group and 2.37mm in the IMP group (Table 2). No statistical difference was observed between the two groups or between the similarly positioned teeth.
Twenty-two gingival recessions occurred in the OSC group (14 at the premolars) and nine in the IMP group—a significant difference according to the chi-square test (χ2 = 6.501,1; p = .011), although no recession exceeded 2mm in either group. The odds ratio was 2.874, meaning recessions were nearly three times as likely to occur in the OSC group. A MANOVA test found no significant difference in lesion severity between the groups (p = .178), but the OSC right first premolars (p = .008) and left canines (p = .047) showed significantly more severe recessions than their counterparts in the IMP group.
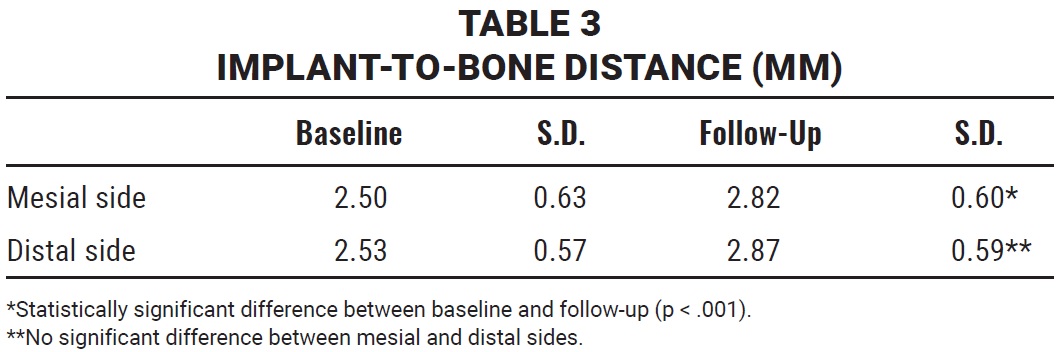
No statistically significant difference in clinical periodontal condition could be observed between the two patient groups. Comparison of the IMP periapical radiographs at T1 and T2 revealed only minor changes between the marginal bone levels at baseline (crown delivery) and follow-up. The mean differences in implant-to-bone distance from T1 to T2 were .32mm on the mesial and .34mm on the distal sides of the implants (Table 3). Differences between baseline and follow-up were statistically significant (p < .001), but there was no significant difference between the mesial and distal sides of the implants (p = .868).
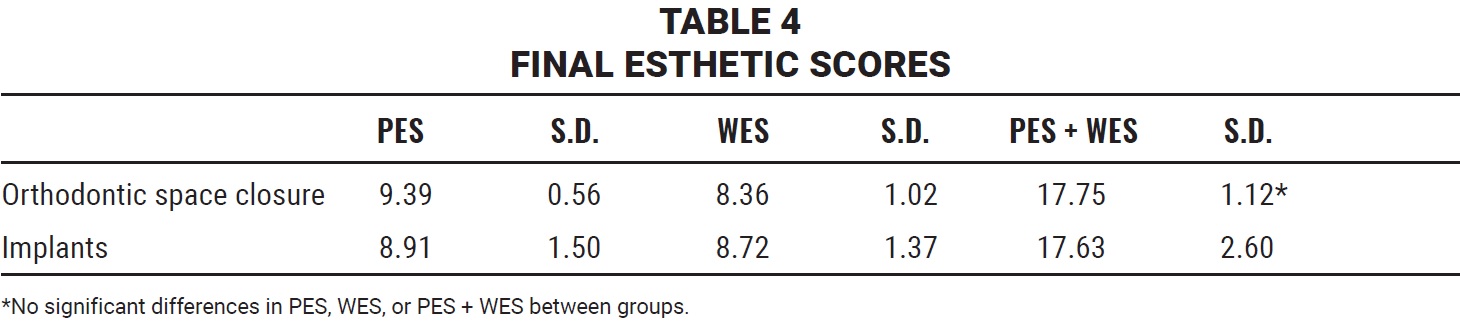
The Wilcoxon test for paired data confirmed the reproducibility of PES and WES measurements in both patient groups (p > .317 for all variables). The OSC group had a mean total PES of 9.39 and WES of 8.36, compared with a PES of 8.91 and a WES of 8.72 in the IMP group; the mean PES + WES was 17.75 in the OSC group and 17.63 in the IMP group (Table 4). None of the differences was statistically significant according to MANOVA analysis (p = .183). When individual PES variables were compared, a significantly lower score for root convexity was found in the IMP group (p = .013), but no statistically significant differences were observed for mesial or distal papillary fill or for level or curvature of the gingival margins. Evaluation of the individual WES variables showed significantly higher scores in the IMP group for all factors except tooth proportion (p = .746).
Patients in both groups were highly satisfied with their esthetic treatment outcomes, as evidenced by mean VAS scores of 97.50 in the OSC patient group and 96.25 in the IMP group (p = .748). No statistical correlation could be established between the professional PES + WES ratings and the patients’ VAS in either the OSC group (p = .431) or the IMP group (p = .084). The OSC patients, in particular, were less critical than the professional examiner was.
Discussion
Evidence regarding which treatment option to choose for patients affected by maxillary lateral incisor agenesis must be considered incomplete. In one systematic review of the literature, the esthetic and periodontal outcome was seen as more favorable after OSC than after space opening and insertion of implant-borne crowns.53 Other systematic reviews, however, have reached no definitive conclusions about the superiority of OSC over prosthodontic intervention, calling for more studies with direct comparisons.54,55 Rosa and colleagues, comparing patients after OSC with canine extrusion and premolar intrusion to a group of treated nonextraction patients 10 years after treatment, showed that OSC carried no risk of periodontal tissue deterioration or TMD in the long term.6 Unfortunately, no patients with implant-supported crowns were evaluated in that study.
The present investigation, which directly compared consecutive patients treated for maxillary lateral incisor agenesis, provides evidence that similar esthetic and periodontally stable outcomes can be achieved and maintained with either approach over more than five years, as long as correct 3D implant positioning is used and the patient has at least a 2mm vestibular bony wall and a thick gingival biotype. The importance of these criteria, especially for immediate and early single-tooth implants in the esthetic zone, has been confirmed by various researchers.28,31-33
The level of oral hygiene—an important factor for long-term periodontal health in general and implant success in particular—was excellent in both patient groups. According to Albrektsson and Isidor, an implant should cause no more than .2mm of bone loss per year after the first year of function.56 Recent studies have reported mean bone losses of only .18mm after three years57 and differences in implant-to-bone distance of only .27mm and .44mm after five years58-60 for implants in the anterior maxilla, corroborating the mean differences of .32mm on the mesial and .34mm on the distal aspects of the implants in the present study.
The one patient who developed a clinically relevant infraocclusion (1.5mm) showed a 2mm gingival recession and a 4mm probing depth at follow-up (Fig. 9). This patient had the only submerged implant—one that had been placed with a DBBM graft during orthodontic treatment. Without a provisional crown, the flap could not be sutured with vertical traction for better stabilization of the coagulum. Therefore, the DBBM granules were pushed apically, so that the implant was not completely covered. A cone-beam computed tomography scan confirmed the almost total absence of a facial bony wall over the implant. Superimposition of calibrated lateral and upper occlusal photographs taken at T1 and T2 indicated minor orthodontic relapse, with slight anterior bite opening and loss of upper incisor torque.
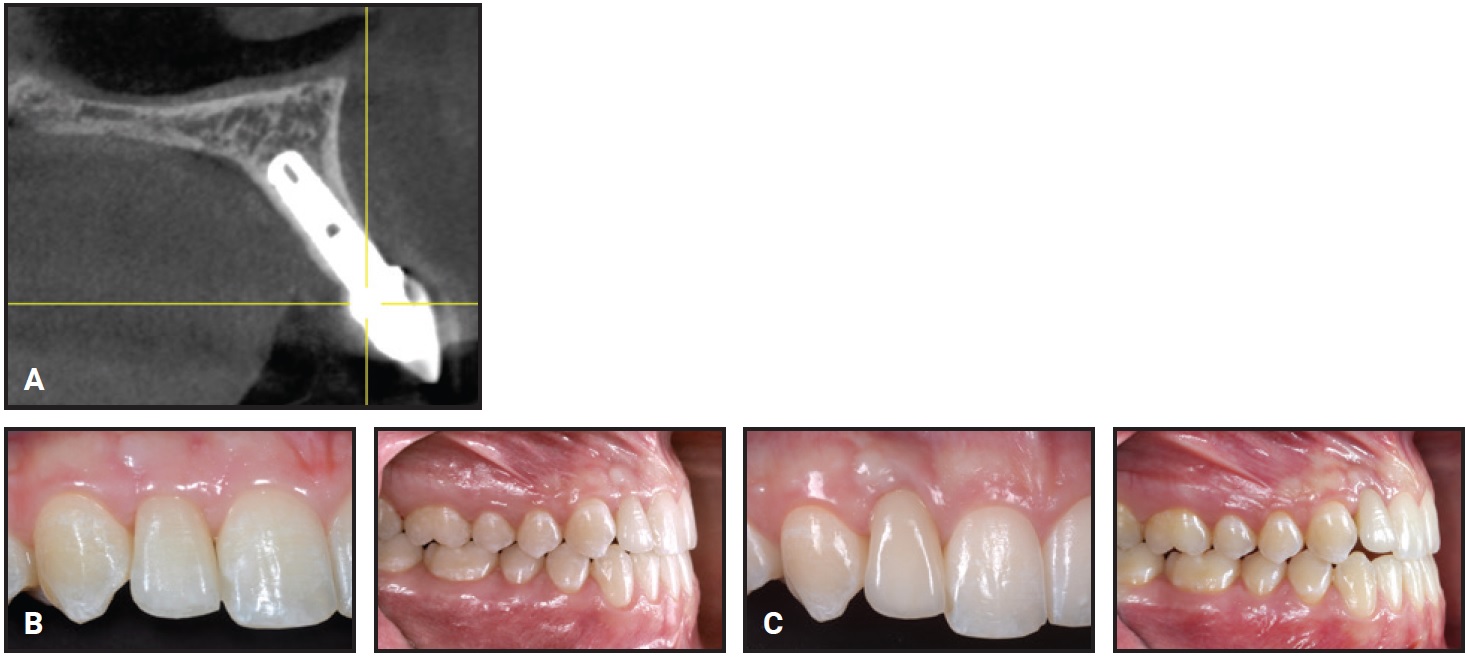
Fig. 9 Only patient to develop infraocclusion had submerged implant placed with graft (deproteinized bovine bone mineral particles) during orthodontic treatment. A. Minimal facial bony wall over implant. B. At final crown delivery. C. At follow-up, showing minor orthodontic relapse.
We noted a higher incidence of gingival recession in the OSC group, with the first premolar being the most affected tooth. Because the facial bony wall in the first premolar area is often thin and may already be fenestrated before treatment, even a slight increase in premolar root torque during orthodontic mesialization can lead to gingival recession in this area. Extremely careful monitoring and meticulous torque control are required during treatment.
Although the total PES was slightly higher and the total WES slightly lower in the OSC group, the differences were not statistically significant. Individual WES values for surface texture, hue, value, and translucency were slightly lower in the OSC group—possibly because all OSC restorations were made of composite material that can discolor and roughen over time, compared to the more stable color and texture of ceramic crowns. One WES variable, root convexity, scored better in the OSC group, indicating that the maintenance of a natural-
looking vestibular implant “bombé” over time is critical, even when hard- or soft-tissue grafts have been performed during implant placement.
Our mean PES + WES for the IMP group (17.63) was higher than that found in other studies. Kolerman and colleagues reported a mean PES + WES of 14.44 for immediately restored implants.61 Similarly, three years after immediate post-extraction placement of single-tooth implants in the esthetic zone, Cosyn and colleagues found a PES + WES of 20 in 21% of the patients, between 14 and 20 in 58%, and less than 14 in 21%.62 After two to four years of loading, Buser and colleagues noted a PES + WES of 14.757; after six years in function, Eccellente and colleagues reported a PES + WES of 14.4.30 These studies evaluated only immediate and early post-extraction implants, however, in locations where hard-tissue peri-implant conditions may be less ideal than in orthodontically prepared alveolar ridges.
To our knowledge, the only published evaluation of PES + WES and peri-implant crestal bone levels in consecutively placed implants for substitution of congenitally missing lateral incisors after a functional loading period of at least three years is a study of 20 patients by Mangano and colleagues.59,60 In that investigation, however, patients who received any additive hard- or soft-tissue grafting were excluded. The success rate for osseointegration and prosthetic compliance was 100%, with only minor changes found in the implant-to-bone distance over time. The mean PES of 8.35 was significantly improved compared with the baseline and with a three-year follow-up of the same patients, while the mean WES of 8.8 remained unchanged. The authors concluded that single-tooth implants could be successful at least medium-term in replacing congenitally missing lateral incisors after orthodontic treatment.
While the total WES in our IMP group (8.36) was comparable to that reported by Mangano and colleagues,59,60 the higher PES in our implant patients (9.39) might be attributed to the additional surgical hard- and soft-tissue grafts that were routinely performed when the peri-implant framework was insufficient. Another explanation could be that all the implants and grafts were performed by the same experienced dentist.
We found no significant difference between groups in PES values for curvature and level of the gingival margin, indicating that a correct high-low-high gingival architecture can be achieved either with orthodontic space closure or with space opening and placement of implant-borne crowns. Whether this outcome influences patient satisfaction remains unclear. Two studies have suggested that patients tend to prefer larger and longer maxillary lateral incisors than professional standards might indicate.8,63 The only PES parameters that seem to influence patient satisfaction with anterior implant restorations are preservation of the mesial and distal papillae—underlining the necessity of peri-implant tissue preservation or enhancement by grafting and meticulous molding procedures when implant-borne crowns are used. Other studies have similarly indicated that patients are less critical and more satisfied with esthetic results than professionals tend to be.64-66 Although our sample was too small to permit generalizations, the 16 patients in the IMP group reported more pleasing esthetics and healthier soft-tissue conditions over the observation time of five to 10 years than other studies have suggested in recent years.30,31,57,61-63,65-67 These favorable results may be explained by the close collaboration of experienced specialists, the implementation of all necessary criteria for implant success, and excellent long-term patient compliance.
Implant-borne crowns cannot necessarily be recommended as first-line treatment for congenitally missing upper lateral incisors, considering that this approach—compared with orthodontic space closure—requires additional surgical procedures, has a higher cost, needs more time to complete, may be more dependent on clinical skill, can increase morbidity, and, above all, carries the undeniable risk of infraocclusion in the long run. On the other hand, to achieve optimal esthetics after orthodontic space closure, the clinician must perform extensive grinding of the canines and restoration of the entire anterior dentition from first premolar to first premolar with composite bonding or ceramic veneers, sacrificing an extensive amount of tooth structure and incurring substantial short- and long-term costs. All pros and cons associated with both treatment modalities must be carefully weighed and discussed with the patient and cooperating dental specialists.
Correct three-dimensional tissue-driven implant placement, coupled with hard- or soft-tissue enhancement procedures and all-ceramic crowns, may be more important in achieving a stable peri-implant tissue framework than has previously been reported. More prospective and retrospective studies with larger sample sizes are needed to confirm whether the favorable esthetic outcomes and healthy periodontal conditions seen in our investigation can be maintained over longer observation periods.
ACKNOWLEDGEMENTS: The authors are indebted to Drs. Donata Rodi, Michele Piattella, and Laura Pozzatti, P & R Stat Analysis, University of Ferrara, Italy, for statistical assistance with the research data.
FOOTNOTES
- *Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- **Trademark of Dolphin Imaging and Management Solutions, Chatsworth, CA; www.dolphinimaging.com.
- ***Trademark of Canon Inc., Melville, NY; www.canon.com.
- †Apple Inc., Cupertino, CA; www.apple.com.
- ‡Registered trademark of International Business Machines Corporation, Armonk, NY; www.ibm.com.
- ††Trademark of GraphPad Software, La Jolla, CA; www.graphpad.com.
REFERENCES
- 1. Polder, B.J.; Van’t Hof, M.A.; Van der Linden, F.P.; and Kuijpers-Jagtman, A.M.: A meta-analysis of the prevalence of dental agenesis of permanent teeth, Comm. Dent. Oral Epidemiol. 32:217-226, 2004.
- 2. Lamour, C.J.; Mossey, P.A.; Thind, B.S.; Forgie, A.H.; and Stirrups, D.R.: Hypodontia—A retrospective review of prevalence and etiology, Part I, Quintess. Int. 36:263-270, 2005.
- 3. Kokich, V.O. Jr. and Kinzer, G.A.: Managing congenitally missing lateral incisors, Part I: Canine substitution, J. Esth. Restor. Dent. 17:5-10, 2005.
- 4. Rosa, M. and Zachrisson, B.U.: Integrating space closure and esthetic dentistry in patients with missing maxillary lateral incisors, J. Clin. Orthod. 41:563-573, 2007.
- 5. Zachrisson, B.U.; Rosa, M.; and Toreskog, S.: Congenitally missing maxillary lateral incisors: Canine substitution, Point, Am. J. Orthod. 139:434, 436, 438 passim, 2011.
- 6. Rosa, M.; Lucchi, P.; Ferrari, S.; Zachrisson, B.U.; and Caprioglio, A.: Congenitally missing maxillary lateral incisors: Long-term periodontal and functional evaluation after orthodontic space closure with first premolar intrusion and canine extrusion, Am. J. Orthod. 149:339-348, 2016.
- 7. Rosa, M. and Zachrisson, B.U.: Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors, J. Clin. Orthod. 35:221-234, 2001.
- 8. Armbruster, P.C.; Gardiner, D.M.; Whitley J.B. Jr.; and Flerra, J.: The congenitally missing maxillary lateral incisor, Part 2: Assessing dentists’ preferences for treatment, World J. Orthod. 6:376-381, 2005.
- 9. Qadri, S.; Parkin, N.A.; and Benson, P.E.: Space closing versus space opening for bilateral missing upper laterals—Aesthetic judgments of laypeople: A web-based survey, J. Orthod. 43:137-146, 2016.
- 10. Johal, A.; Katsaros, C.; and Kuijpers-Jagtman, A.M.: State of the science on controversial topics: Missing maxillary lateral incisors—A report of the Angle Society of Europe 2012 meeting, Prog. Orthod. 14:20, 2013.
- 11. Kinzer, G.A and Kokich, V.O. Jr.: Managing congenitally missing upper lateral incisors, Part III: Single-tooth implants, J. Esth. Restor. Dent. 17:202-210, 2005.
- 12. Kokich, V.O. Jr.; Kinzer, G.A.; and Janakievski, J.: Congenitally missing maxillary lateral incisors: Restorative replacement, Am. J. Orthod. 139:435, 437, 439 passim, 2011.
- 13. Schneider-Moser, U.; Moser, L.; and Pellitteri, G.: To open or to close spaces for congenitally missing upper lateral incisors: Is this really the question? Eur. J. Clin. Orthod. 1:32-43, 2013.
- 14. Kinsel, R.P. and Lamb, R.E.: Tissue directed placement of dental implants in the esthetic zone for long-term biologic synergy: A clinical report, Int. J. Oral Maxillofac. Implants 20:913-922, 2005.
- 15. Kan, J.Y.; Rungcharassaeng, K.; Umezu, K.; and Kois, J.C.: Dimensions of peri-implant mucosa: An evaluation of maxillary anterior single implants in humans, J. Periodontol. 74:557-562, 2003.
- 16. Chen, S.T. and Buser, D.: Clinical and esthetic outcomes of implants placed in postextraction sites, Int. J. Oral Maxillofac. Implants 24:186-217, 2009.
- 17. Buser, D.; Bornstein, M.M.; Weber, H.P.; Grütter, L.; Schmid, B.; and Belser, U.C.: Early implant placement with simultaneous guided bone regeneration following single-tooth extraction in the esthetic zone: A cross-sectional, retrospective study in 45 subjects with a 2- to 4-year follow-up, J. Periodontol. 79:1773-1781, 2008.
- 18. Ainamo, A.: Influence of age on the location of the maxillary mucogingival junction, J. Period. Res. 13:189-193, 1978.
- 19. Forsberg, C.M.; Eliasson, S.; and Westergren, H.: Face height and tooth eruption in adults: A 20-year follow-up investigation, Eur. J. Orthod. 13:249-254, 1991.
- 20. Thilander, B.; Odman, J.; and Lekholm, U.: Orthodontic aspects of the use of oral implants in adolescents: A 10-year follow-up study, Eur. J. Orthod. 23:715-731, 2001.
- 21. Jemt, T.; Ahlberg, G.; Henriksson, K.; and Bondevik, O.: Changes of anterior clinical crown height in patients provided with single-implant restorations after more than 15 years of follow-up, Int. J. Prosthod. 19:455-461, 2006.
- 22. Bernard, J.P.; Schatz, J.P.; Christou, P.; Belse, U.; and Kiliaridis, S.: Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults: A retrospective study, J. Clin. Periodontol. 31:1024-1028, 2004.
- 23. Zitzmann, N.U.; Arnold, D.; Ball, J.; Brusco, D.; Triaca, A.; and Verna, C.: Treatment strategies for infraoccluded dental implants, J. Prosth. Dent. 113:169-174, 2015.
- 24. Belser, U.C.; Schmid, B.; Higginbottom, F.; and Buser, D.: Outcome analysis of implant restorations located in the anterior maxilla: A review of the recent literature, Int. J. Oral Maxillofac. Implants 19:30-42, 2004.
- 25. Buser, D.; Martin, W.; and Belser, U.C.: Optimizing esthetics for implant restorations in the anterior maxilla: Anatomic and surgical considerations, Int. J. Oral Maxillofac. Implants 19:43-61, 2004.
- 26. Belser, U.; Buser, D.; and Higginbottom, F.: Consensus statements and recommended clinical procedures regarding esthetics in implant dentistry, Int. J. Oral Maxillofac. Implants 19:73-74, 2004.
- 27. Misch, C.E.; Perel, M.L.; Wang, H.L.; Sammartino, G.; Galindo-Moreno, P.; Trisi, P.; Steigmann, M.; Rebaudi, A.; Palti, A.; Pikos, M.A.; Schwartz-Arad, D.; Choukroun, J.; Gutierrez-Perez, J.L.; Marenzi, G.; and Valavanis, D.K.: Implant success, survival, and failure: The International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference, Implant Dent. 17:5-15, 2008.
- 28. Chen S.T. and Buser D.: Esthetic outcomes following immediate and early implant placement in the anterior maxilla: A systematic review, Int. J. Oral Maxillofac. Implants, 29:186-215, 2014.
- 29. Grunder, U.; Gracis, S.; and Capelli, M.: Influence of the 3-D bone-to-implant relationship on esthetics, Int. J. Period. Restor. Dent. 25: 113-119, 2005.
- 30. Eccellente, T.; Rossi, A.; D’Errico, M.; Grande, C.; Ortolani, M.; and Adaimo, R.: Esthetic outcome of maxillary single-tooth implants, Clin. Oral Implants Res. 25:69, 2014.
- 31. Buser, D.; Chappuis, V.; Bornstein, M.M.; Wittneben, J.G.; Frei, M.; and Belser, U.C.: Long-term stability of contour augmentation with early implant placement following single tooth extraction in the esthetic zone: A prospective, cross-sectional study in 41 patients with a 5- to 9-year follow-up, J. Periodontol. 84:1517-1527, 2013.
- 32. Jensen, S.S.; Bosshardt, D.D.; Gruber, R.; and Buser, D.: Long-term stability of contour augmentation in the esthetic zone: Histologic and histomorphometric evaluation of 12 human biopsies 14 to 80 months after augmentation, J. Periodontol. 85:1549-1556, 2014.
- 33. Weigl, P. and Strangio, A.: The impact of immediately placed and restored single-tooth implants on hard and soft tissues in the anterior maxilla, Eur. J. Oral Implantol. 9:S89-S106, 2016.
- 34. Beyer, A.; Tausche, E.; Boening, K.; and Harzer, W.: Orthodontic space opening in patients with congenitally missing lateral incisors, Angle Orthod. 77:404-409, 2007.
- 35. Uribe, F.; Chau, V.; Padala, S.; Neace, W.P.; Cutrera, A.; and Nanda, R.: Alveolar ridge width and height changes after orthodontic space opening in patients congenitally missing maxillary lateral incisors, Eur. J. Orthod. 35:87-92, 2013.
- 36. Marchi, L.M.; Pini, N.I.; Hayacibara, R.M.; Silva, R.S.; and Pascotto, R.C.: Congenitally missing maxillary lateral incisors: Functional and periodontal aspects in patients treated with implants or space closure and tooth re-contouring, Open Dent. J. 6:248-254, 2012.
- 37. Elian, N.; Tabourian, G.; Jalbout, Z.N.; Classi, A.; Cho, S.C.; Froum, S.; and Tarnow, D.P.: Accurate transfer of peri-implant soft tissue emergence profile from the provisional crown to the final prosthesis using an emergence profile cast, J. Esth. Restor. Dent. 19:306-314, 2007.
- 38. Su, H.; Gonzalez-Martin, O.; Weisgold, A.; and Lee, E.: Considerations of implant abutment and crown contour: Critical contour and subcritical contour, Int. J. Period. Restor. Dent. 23:335-343, 2010.
- 39. Wittneben, J.G.; Buser, D.; Belser, U.C.; and Brägger, U.: Peri-implant soft tissue conditioning with provisional restorations in the esthetic zone: The dynamic compression technique, Int. J. Period. Restor. Dent. 33:447-455, 2013.
- 40. Quigley, G.A. and Hein, J.W.: Comparative cleansing of manual and power brushing, J. Am. Dent. Assoc. 65:26-29, 1962.
- 41. Kornman, K.S. and Löe, H.: The role of local factors in the etiology of periodontal diseases, Periodontol. 2000 2:83-97, 1993.
- 42. Joss, A.; Adler, R.; and Lang, N.P.: Bleeding on probing: A parameter for monitoring periodontal conditions in clinical practice, J. Clin. Periodontol. 6:402-408, 1994.
- 43. Lang, N.P.; Adler, R.; Joss, A.; and Nyman, S.: Absence of bleeding on probing: An indicator of periodontal stability, J. Clin. Periodontol. 17:714-721, 1990.
- 44. Miller, P.D. Jr.: A classification of marginal tissue recession, Int. J. Period. Restor. Dent. 5:8-13, 1985.
- 45. Weber, H.P.; Buser, D.; Fiorellini, J.P.; and Williams, R.C.: Radiographic evaluation of crestal bone levels adjacent to nonsubmerged titanium implants, Clin. Oral Implants Res. 3:181-188, 1992.
- 46. Weber, H.P.; Crohin, C.C.; and Fiorellini, J.P.: A 5-year prospective clinical and radiographic study of non-submerged dental implants, Clin. Oral Implants Res. 11:144-153, 2000.
- 47. Fürhauser, R.; Florescu, D.; Benesch, T.; Mailath, G.; and Watzek, G.: Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score, Clin. Oral Implants Res. 16:639-644, 2005.
- 48. Gehrke, P.; Lobert, M.; and Dhom, G.: Reproducibility of the pink esthetic score—Rating soft tissue esthetics around single-implant restorations with regard to dental observer specialization, J. Esth. Restor. Dent. 20:375-384, 2008.
- 49. Belser, U.C.; Grütter, L.; Vailati, F.; Bornstein, M.M.; Weber, H.P.; and Buser, D.: Outcome evaluation of early placed maxillary anterior single-tooth implants using objective esthetic criteria: A cross-sectional, retrospective study in 45 patients with a 2- to 4-year follow-up using pink and white esthetic scores, J. Periodontol. 80:140-151, 2009.
- 50. Annibali, S.; Bignozzi, I.; La Monaca, G.; and Cristalli, M.P.: Usefulness of the aesthetic result as a success criterion for implant therapy: A review, Clin. Implant Dent. Relat. Res. 14:3-40, 2012.
- 51. O’Neill, K.; Harkness, M.; and Knight, R.: Ratings of profile attractiveness after functional appliance treatment, Am. J. Orthod. 118:371-376, 2000.
- 52. Schabel, B.J.; McNamara, J.A. Jr.; Franchi, L.; and Baccetti, T.: Q-sort assessment vs visual analog scale in the evaluation of smile esthetics, Am. J. Orthod. 135:S61-71, 2009.
- 53. Silveira, G.S.; de Almeida, N.V.; Pereira, D.M.; Mattos, C.T.; and Mucha, J.N.: Prosthetic replacement vs space closure for maxillary lateral incisor agenesis: A systematic review, Am. J. Orthod. 150:228-237, 2016.
- 54. Andrade, D.C.; Loureiro, C.A.; Araújo, V.E.; Riera, R.; and Atallah, A.N.: Treatment for agenesis of maxillary lateral incisors: A systematic review, Orthod. Craniofac. Res. 16:129-136, 2013.
- 55. Kiliaridis, S.; Sidira, M.; Kirmanidou, Y.; and Michalakis, K.: Treatment options for congenitally missing lateral incisors, Eur. J. Oral Implantol. 9:S5-S24, 2016.
- 56. Albrektsson, T. and Isidor, F.: Consensus report of session IV, in Proceedings of the 1st European Workshop on Periodontology, ed. N.P. Lang and T. Karring, Quintessence Publishing Co., Inc., Hanover Park, IL, 1993, pp. 365-369.
- 57. Buser, D.; Wittneben, J.; Bornstein, M.M.; Grütter, L.; Chappuis, V.; and Belser, U.S.: Stability of contour augmentation and esthetic outcomes of implant-supported single crowns in the esthetic zone: 3-year result of a prospective study with early implant placement post extraction, J. Periodontol. 82:342-349, 2011.
- 58. Berberi, A.N.; Sabbagh, J.M.; Aboushelib, M.N.; Noujeim, Z.F.; and Salameh, Z.A.: A 5-year comparison of marginal bone level following immediate loading of single-tooth implants placed in healed alveolar ridges and extraction sockets in the maxilla, Front. Physiol. 5:29, 2014.
- 59. Mangano, C.; Levrini, L.; Mangano, A.; Mangano, F.; Macchi, A.; and Caprioglio, A.: Esthetic evaluation of implants placed after orthodontic treatment in patients with congenitally missing lateral incisors, J. Esth. Restor. Dent. 26:61-71, 2014.
- 60. Mangano, A.; Caprioglio, A.; Mangano, F.; Macchi, A.; Levrini, L.; and Mangano, C.: Five-year esthetic evaluation of implants used to restore congenitally missing maxillary lateral incisors after orthodontic space opening treatment, J. Oral Sci. Rehab. 2:62-71, 2016.
- 61. Kolerman, R.; Nissan, J.; Mijritsky, E.; Hamoudi, N.; Mangano, C.; and Tal, H.: Esthetic assessment of immediately restored implants combined with GBR and free connective tissue graft, Clin. Oral Implants Res. 27:1414-1422, 2016.
- 62. Cosyn, J.; Eghbali, A.; De Bruyn, H.; Collys, K.; Cleymaet, R.; and De Rouck, T.: Immediate single-tooth implants in the anterior maxilla: 3-year results of a case series on hard and soft tissue response and aesthetics, J. Clin. Periodontol. 38:746-753, 2011.
- 63. Schneider, U.; Moser, L.; Fornasetti, M.; Piattella, M.; and Siciliani, G.: Esthetic evaluation of implants vs canine substitution in patients with congenitally missing maxillary lateral incisors: Are there any new insights? Am. J. Orthod. 150:416-424, 2016.
- 64. Vilhjálmsson, V.H.; Klock, K.S.; Størksen, K.; and Bårdsen, A:. Aesthetics of implant-supported single anterior maxillary crowns evaluated by objective indices and participants’ perceptions, Clin. Oral Implants Res. 22:1399-1403, 2011.
- 65. Cho, H.L.; Lee, J.K.; Um, H.S.; and Chang, B.S.: Esthetic evaluation of maxillary single-tooth implants in the esthetic zone, J. Peridontol. Implant Sci. 40:188-193, 2010.
- 66. Hosseini, M. and Gotfredsen, K.: A feasible, aesthetic quality evaluation of implant-supported single crowns: An analysis of validity and reliability, Clin. Oral Implants Res. 23:453-458, 2012.
- 67. Benic, G.I.; Wolleb, K.; Sancho-Puchades, M.; and Hämmerle, C.H.: Systematic review of parameters and methods for the professional assessment of aesthetics in dental implant research, J. Clin. Periodontol. 39:160-192, 2012.






