Unilateral Upper Central Incisor Space Closure Using Palatal Mini-Implants
Many factors complicate the diagnosis and treatment of growing children with missing maxillary central or lateral incisors.1,2 The need to maintain alveolar bone until growth has ceased presents a particular dilemma if implants are required. In addition, parents who are concerned about psychosocial pressures usually want early resolution of their children’s esthetic problems.3
Treatment alternatives include reimplantation of the avulsed tooth, autotransplantation, waiting until early adulthood to place a bridge or an implant, or substituting the central incisor with the lateral incisor after orthodontic space closure.4,5 The advantage of orthodontic treatment is that a concomitant malocclusion can be treated simultaneously.
Interdisciplinary collaboration between orthodontists and other dentists, such as oral surgeons, prosthodontists, and general practitioners, appears to be of increasing importance in these cases.6 The following patient is an example.
Case Report
A 14-year-old male who had lost his upper right central incisor from trauma was referred for orthodontic assessment. Since reimplantation of the avulsed tooth was not possible due to multiple root fractures, he had received a Maryland bridge to restore esthetics and maintain space.
The patient exhibited a well-balanced and symmetrical face with a convex facial profile and normal vertical proportions (Fig. 1A). He had edge-to-edge Class II molar and canine relationships, mild crowding in both arches, a 5mm overjet, and a 4mm overbite. Both arches were tapered and evidenced mild crowding, and the dental and facial midlines were coincident.
Similar articles from the archive:
- Maxillary Space Closure Using Aligners and Palatal Mini-Implants in Patients with Congenitally Missing Lateral Incisors January 2021
- Non-Compliance Space Closure in Patients with Missing Maxillary Lateral Incisors March 2013
- CASE REPORT Closure of Central Incisor Spaces: A 16-Year Follow-Up June 2011
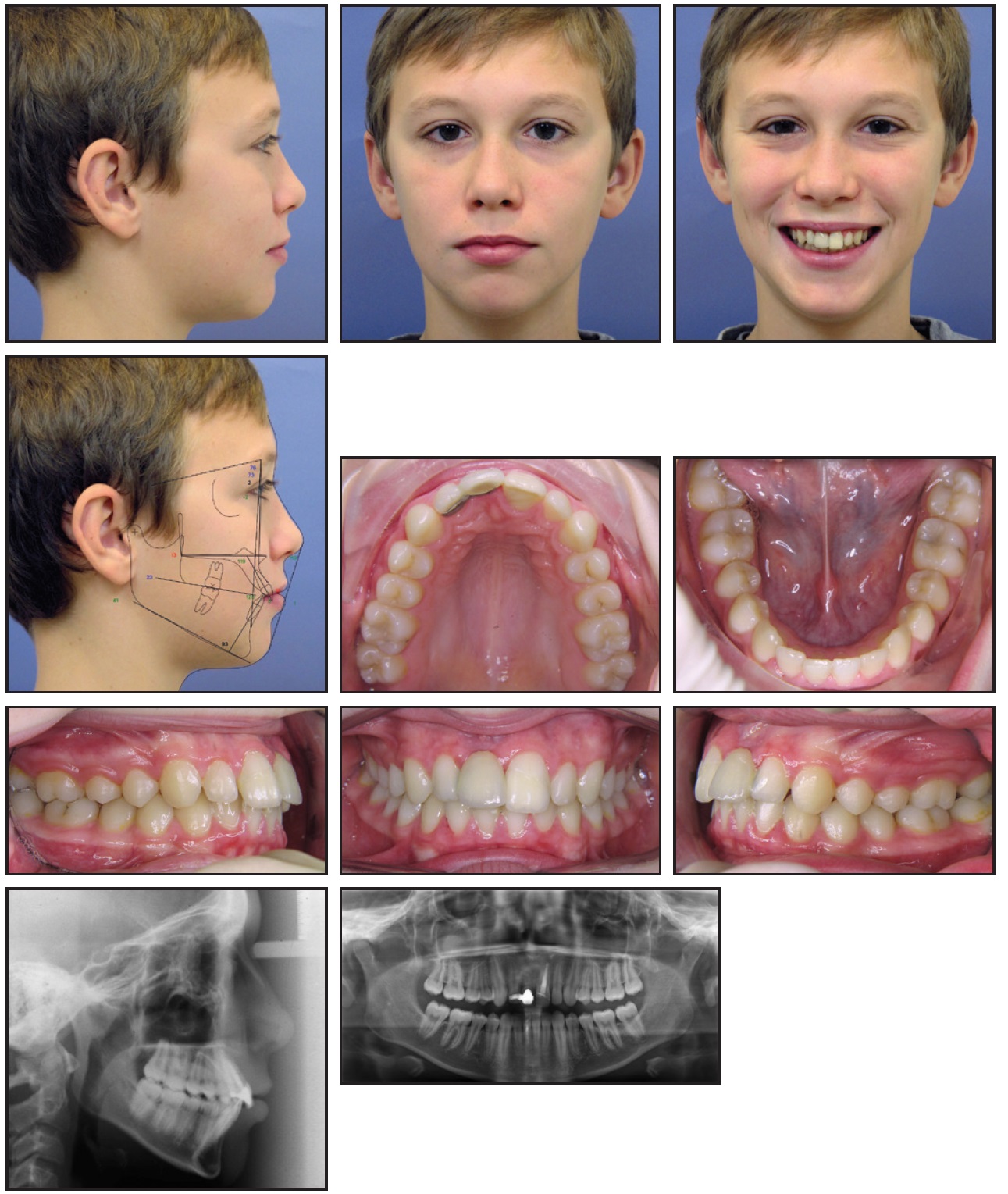
Fig. 1 14-year-old male patient with missing upper right central incisor, convex profile, edge-to-edge Class II molar relationships, and mild crowding in both arches before treatment (continued in next image).
No signs or symptoms of TMD were noted. A panoramic x-ray confirmed the presence of all permanent teeth except the avulsed right central incisor and the third molars. Root-canal fillings were evident in the upper left and lower right central incisors (Fig. 1B).
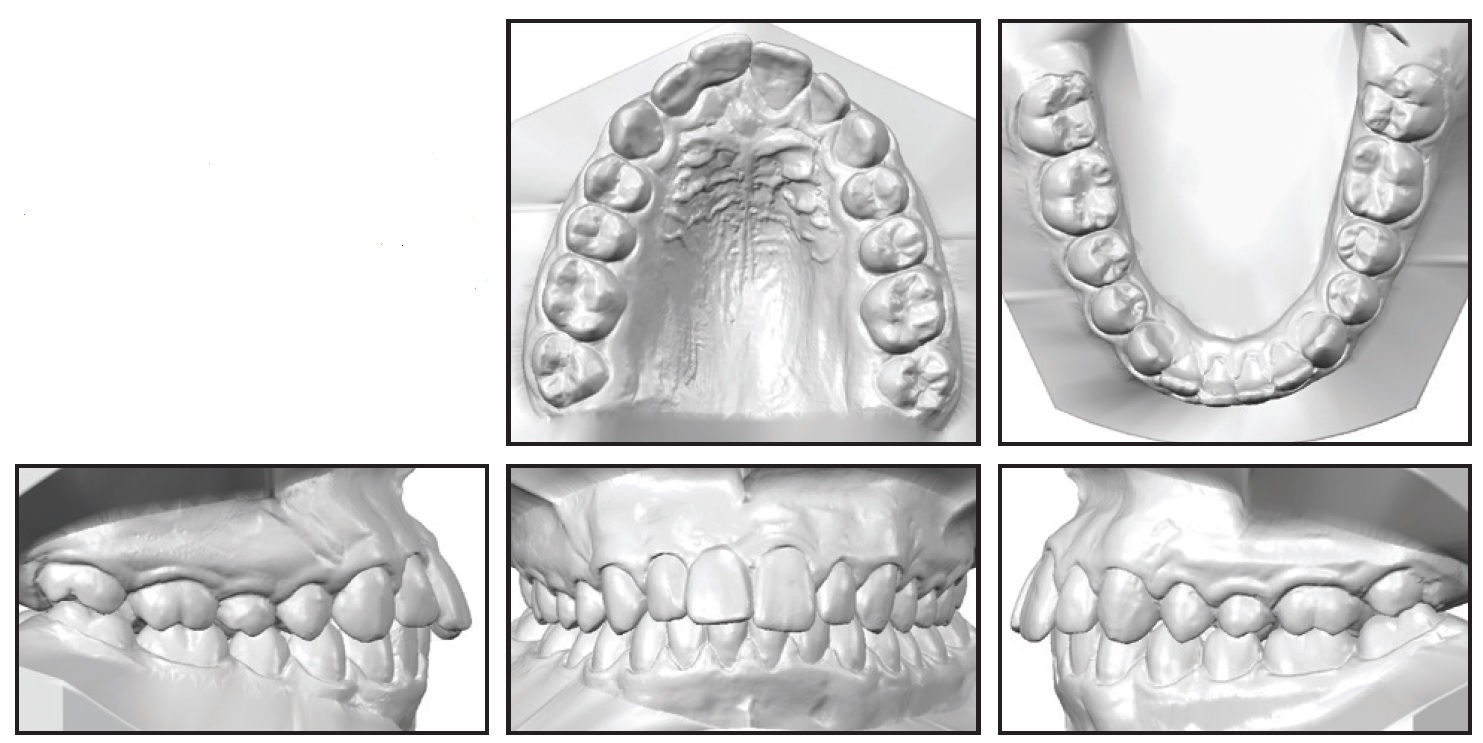
Fig. 1 (cont.) 14-year-old male patient with missing upper right central incisor, convex profile, edge-to-edge Class II molar relationships, and mild crowding in both arches before treatment.
Cephalometric analysis showed a skeletal Class I relationship (ANB = 2.5°) with retrusive jaws and an excessive mandibular plane angle to anterior cranial base (Table 1). The maxillary central incisors were slightly proclined, and the lower incisors were within normal limits relative to their dental bases, with a reduced interincisal angle (121.8°). The upper and lower incisal edges were 10.5mm and 5.4mm anterior to pogonion, respectively. Soft-tissue assessment revealed competent lips at rest, a normal smile arc, and a slightly increased nasolabial angle. The upper lip was slightly behind the Ricketts E-line, and the lower lip was 1mm in front of it.
The patient and parents’ main concern was the esthetics of the bridge. Two treatment options were discussed. The first aimed only to straighten the teeth and maintain the Maryland bridge, which would be replaced by an implant after growth had ceased. The second plan involved substitution of the upper right central with the upper right lateral incisor, followed by restorative modification. Under this option, all posterior teeth on the right side would need to be moved mesially, with the upper right canine and first premolar undergoing appropriate esthetic restorations. The patient and parents selected the second option.
Treatment objectives were to move the upper right lateral incisor into the position of the missing central incisor and, subsequently, to mesialize all posterior teeth on the right side using temporary anchorage devices (TADs). Alveolar ridge development would thus be promoted and future bone loss in the maxillary right central incisor area would be prevented, while the dental midlines would be maintained during space closure. Additional objectives were to eliminate the lower crowding, maintain or improve the skeletal pattern, improve the overbite and overjet, and achieve a functionally stable occlusion. Finally, an interdisciplinary approach involving the general dentist and prosthodontist would be implemented.
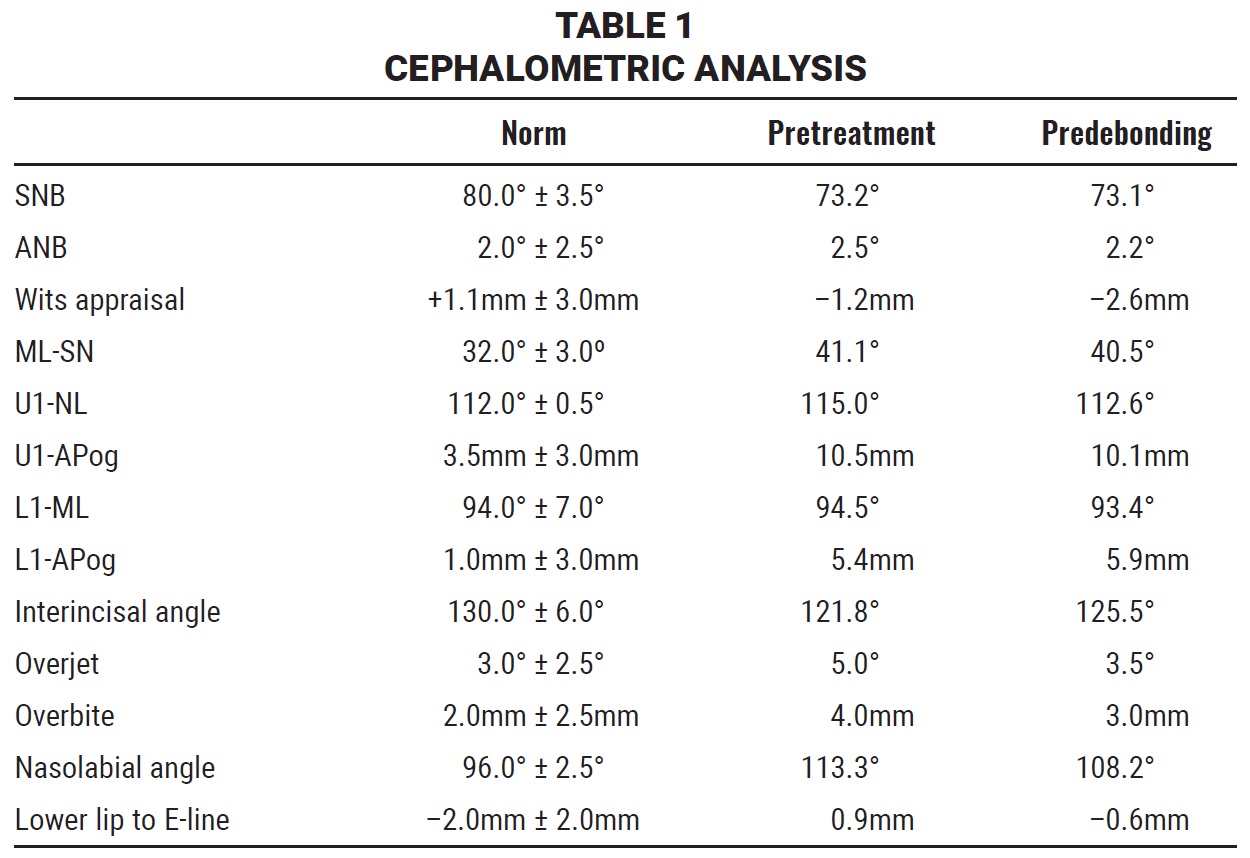
After oral-hygiene instruction and improvement, the upper and lower arches were bonded with MBT*-prescription .022" × .028" SPEED** brackets for leveling and alignment (Fig. 2). The wire sequence in both arches progressed from .012" to .016" nickel titanium, followed by .018" nickel titanium, .018" × .025" heat-activated nickel titanium, .019" × .025" stainless steel, and .019" × .025" TMA.*** All archwires had an ovoid form.

Fig. 2 Leveling and alignment using MBT*-prescription .022" × .028" SPEED** brackets and .018" nickel titanium archwires.
After six months, when final working wires were in place, two mini-implants† (1.8mm × 9mm) were inserted paramedian to the third palatal rugae, anterior to the second premolars, as recommended in the literature7-10 (Fig. 3).
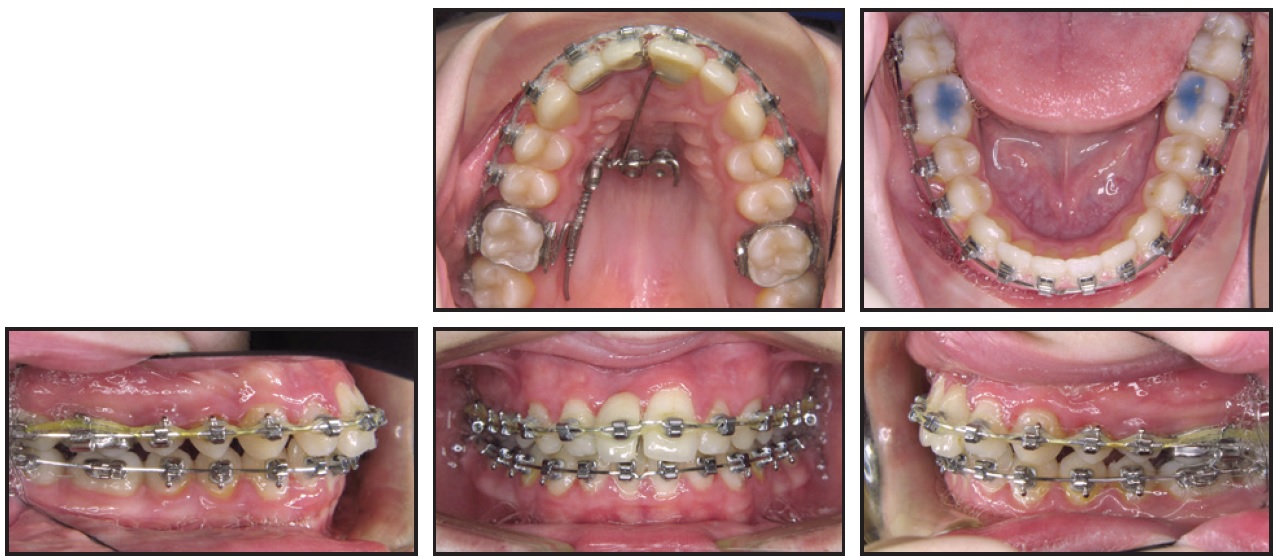
Fig. 3 After six months of treatment, insertion of temporary anchorage devices paramedian to third palatal rugae and anterior to second premolars.
An auxiliary arm from the palatal appliance was affixed to the palatal surface of the upper left central incisor for indirect anchorage (Fig. 4).
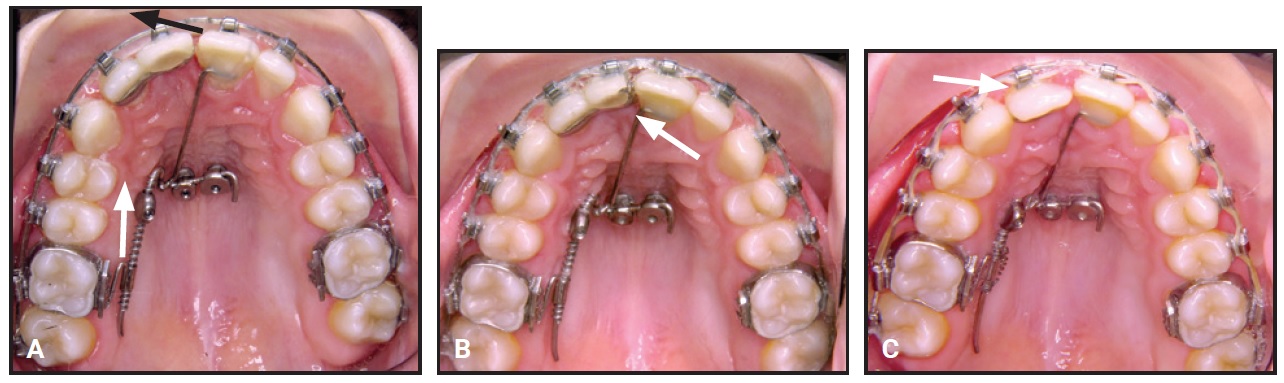
Fig. 4 A. Direction of labial force from elastomeric power chain, added to enhance space closure (black arrow); mesial force applied on palatal side from nickel titanium coil spring (white arrow); auxiliary arm bonded to upper left central incisor for indirect anchorage. B. Width of provisional Maryland bridge gradually reduced to avoid unsightly gap in anterior region during space closure. C. Maxillary arch after closure of right central incisor space, with upper right lateral incisor built up to match size and shape of central incisor.
Impression caps were placed on the TADs prior to taking an impression. Laboratory analogs were then placed over the impression caps, and the auxiliary arm was welded to the appliance. The TADs were designed for use with the OrthoLox Snap-In† coupling mechanism, so that both abutments of the appliance could be snapped into the TADs (Fig. 5). The abutment screw, with a left-hand thread, was turned upward in the reverse direction to lock it securely in place.
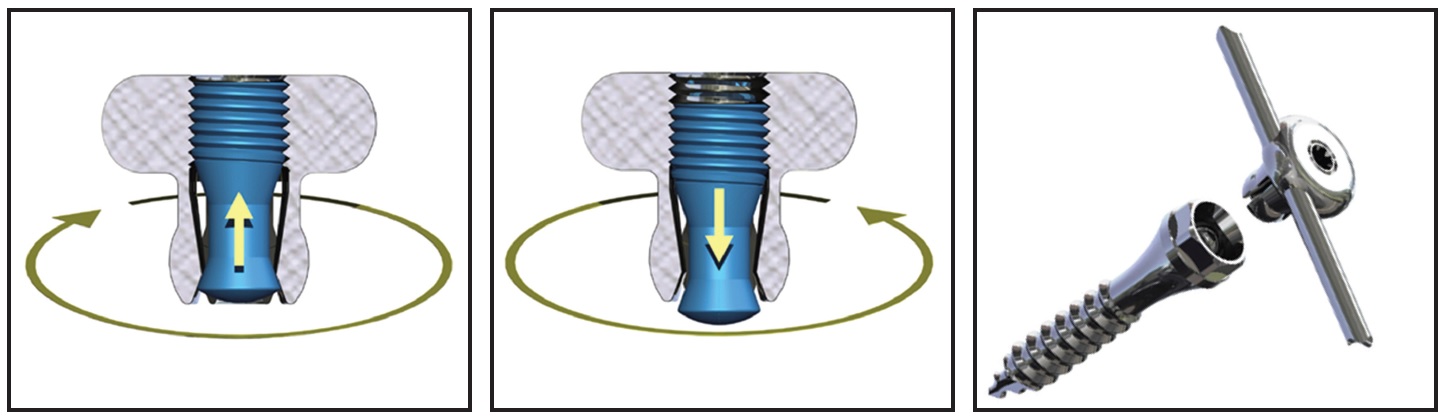
Fig. 5 OrthoLox-flyer† coupling system (courtesy of Promedia Medizintechnik).
A 200g nickel titanium coil spring was activated with a screwdriver every six weeks to close the upper right central incisor space. Concurrently, an elastomeric power chain was added to provide a labial force, thus enhancing the space closure. The width of the provisional Maryland bridge was gradually reduced to avoid the appearance of an unsightly gap in the anterior region (Fig. 4B). Class II elastics were worn on the left side during space closure to correct the Class II buccal relationship.
After 12 months of treatment, the upper right central incisor space was closed (Fig. 6).
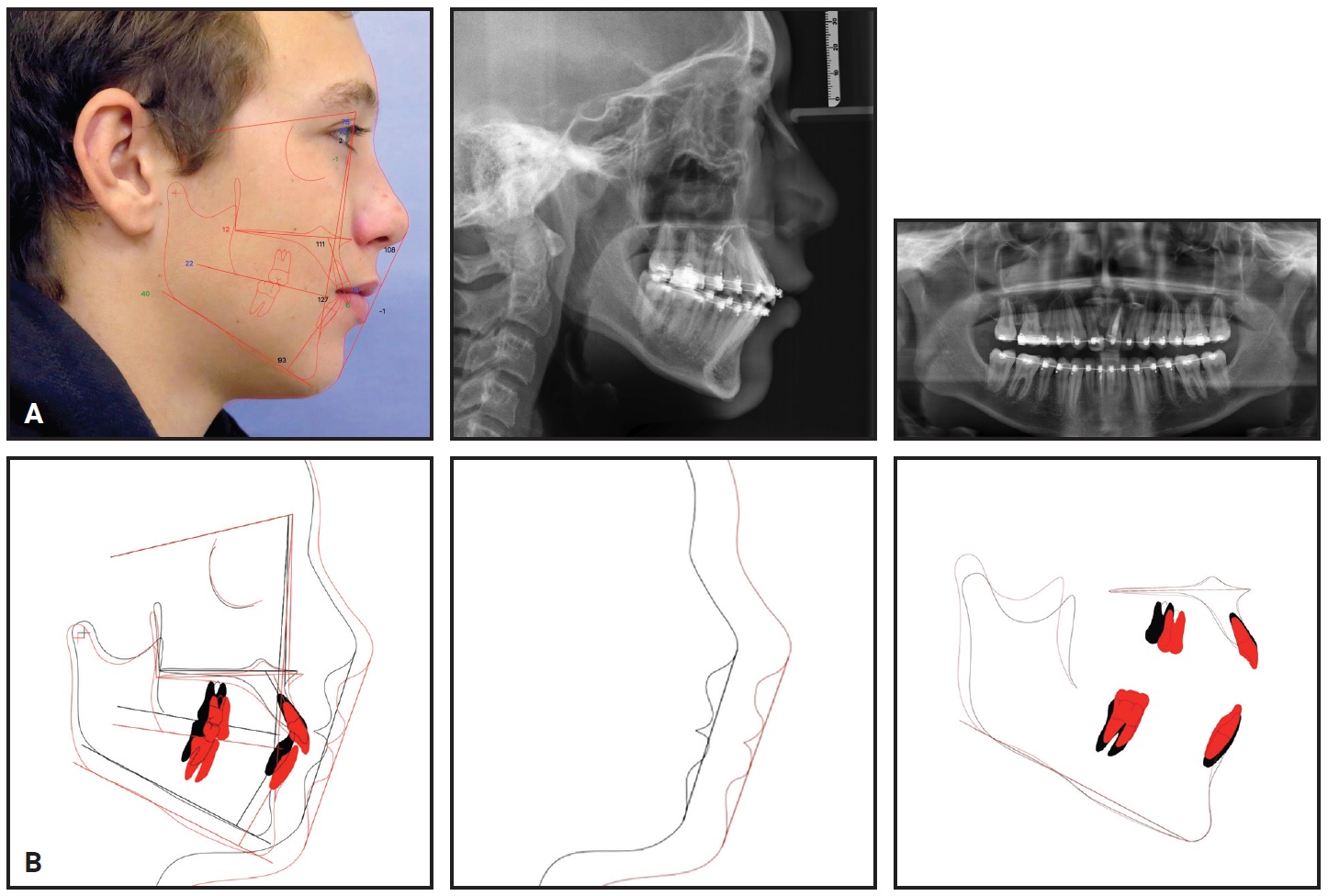
Fig. 6 A. After 12 months of space closure. B. Superimposition of pretreatment (black) and predebonding (red) cephalometric tracings.
The palatal appliance was then removed (Fig. 7). The upper right lateral incisor was temporarily recontoured with composite resin to resemble a central incisor, and the upper right canine was reshaped to resemble a lateral incisor.
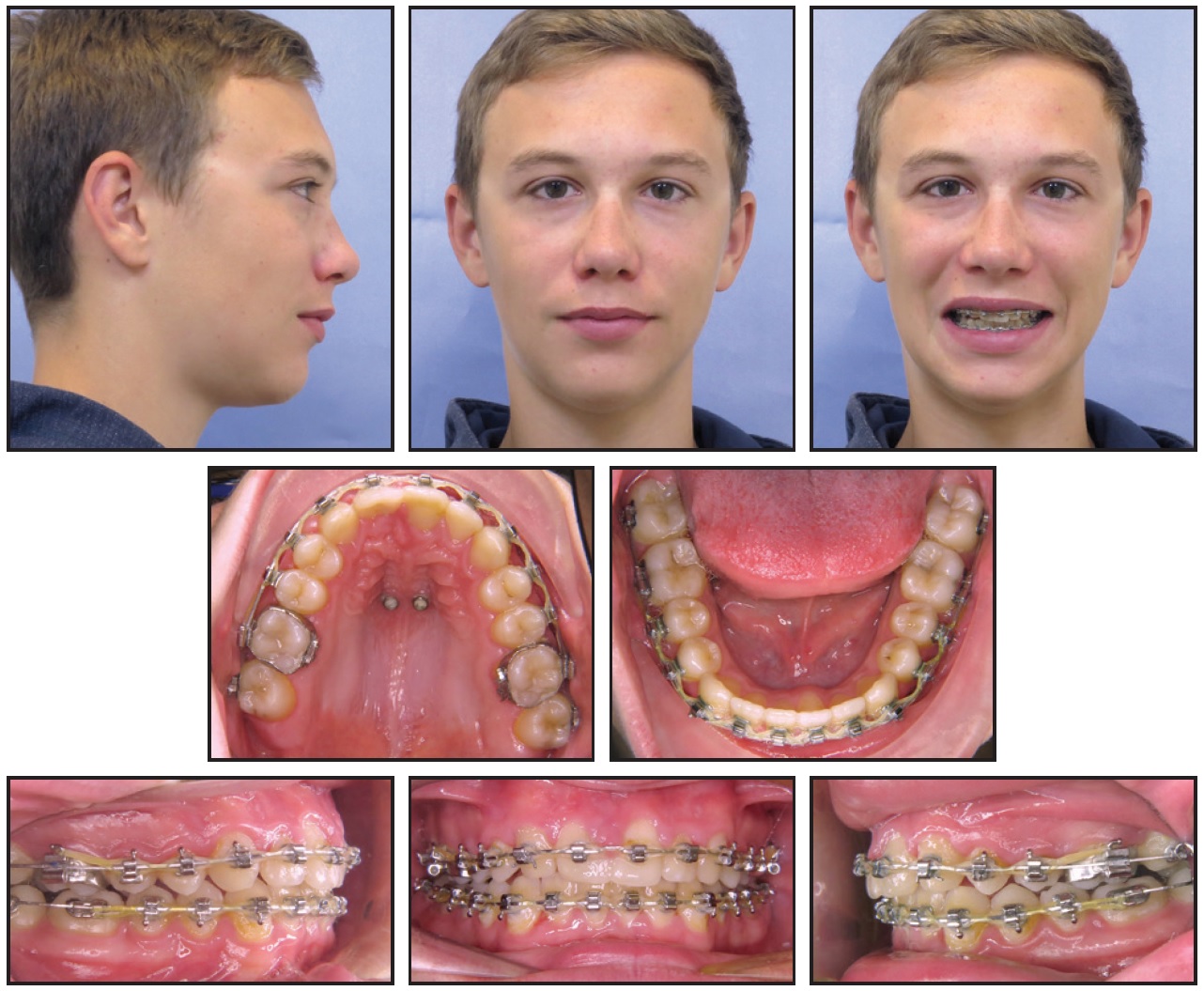
Fig. 7 After removal of palatal appliance.
Active treatment was completed in 27 months (Fig. 8A).
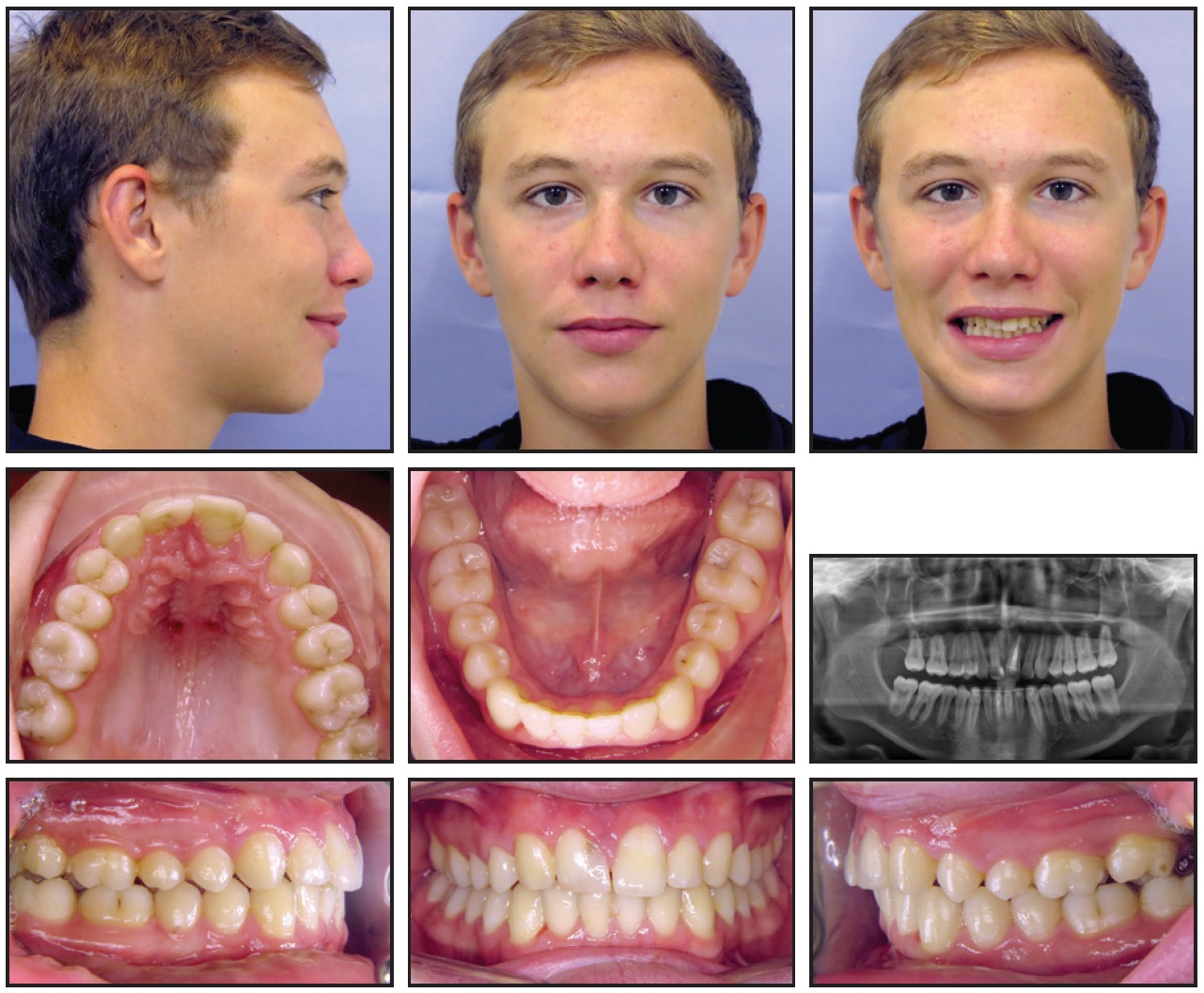
Fig. 8 Patient after 27 months of treatment (continued in next image).
A Hawley retainer was delivered for the maxillary arch, and an .0155" multistranded, gold-plated stainless steel 3-3 retainer was bonded in the mandibular arch. After a ceramic veneer was affixed to the upper right lateral incisor by the prosthodontist, an .0155" multistranded, gold-plated stainless steel 3-3 retainer was bonded in the maxillary arch.
Post-treatment panoramic photographs showed acceptable root parallelism and no evidence of root resorption. A good esthetic result and acceptable smile were achieved, with coincident dental and facial midlines. Acceptable dental alignment was obtained, and the overbite and overjet were improved. A full Class II molar relationship was achieved on the right, and a quarter-Class II canine and molar relationship on the left (Fig. 8B). The patient and his parents were pleased with the results.
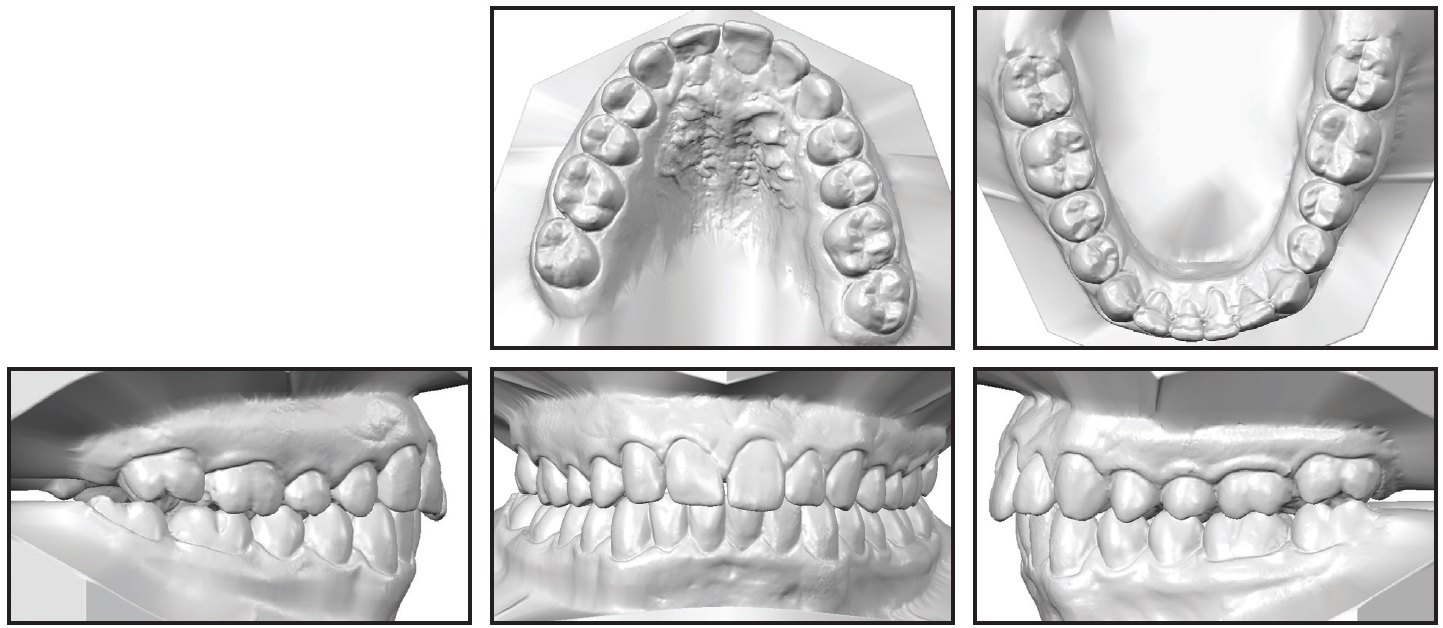
Fig. 8 (cont.) Patient after 27 months of treatment.
Cephalometric analysis showed no skeletal changes. The upper and lower central incisors were slightly retroclined, and the interincisal angle was increased (Table 1). The entire upper right quadrant was moved mesially without anchorage loss of the upper right incisors.
One year after treatment, no relapse was seen (Fig. 9).

Fig. 9 Patient one year after treatment.
Discussion
The esthetic improvement in this case was achieved in accordance with the protocol established by Rosa and Zachrisson.11-15 The canine and molar relationships were not fully Class I on the left side, which may have been due to the mild Bolton discrepancy. Interproximal enamel reduction could have been performed in the mandibular arch to achieve a full Class I relationship on the left side.
Although some authors have suggested that osseointegrated implants are the optimal choice for replacement of missing lateral incisors, we opted for the space-closure approach in this case.16 Other authors have noted that space closure for a missing maxillary central incisor can have a functional disadvantage: when a canine is relocated to the position of the lateral incisor, the small first premolars carry the functional load during lateral jaw excursions.17 The premolars may then lose bone support, compromising their long-term prognosis.
Zachrisson18 and several others have extensively investigated various treatment options. Continuing vertical changes in tooth positions, even after cessation of growth, can negatively affect long-term results following implant placement, since the implant is ankylosed and cannot change position as the neighboring teeth erupt. Even small tooth movements after implant placement can create esthetic problems.19-21 Making an implant-supported crown with a shade and translucency that blend well with the surrounding teeth can be difficult; moreover, the color difference can worsen as the patient ages.18 The color of a canine usually approximates that of the adjacent teeth rather than that of a porcelain crown.22 In this case, only a ceramic veneer was needed to make the upper lateral incisor resemble a central incisor.
Our decision was corroborated by a nine-year follow-up study supporting natural tooth substitution in cases of dental agenesis in the maxillary anterior region.23 Some 11% of patients experience relapse significant enough to prevent implant placement after orthodontic treatment.24 In addition, a 10-year follow-up study reported that some patients showed progressive loss of bone support at the buccal aspects of implant-supported crowns that were replacing upper incisors.19 That finding was confirmed by a recent study in which bone augmentation was needed in most of the cases.25 Similar results were found in a dental-cast analysis that showed a significant decrease in alveolar ridge width and height immediately after orthodontic space opening for congenitally missing upper lateral incisors. The presence of a labial concavity between the central incisor and canine is evidence of such alveolar ridge loss. Although distal movement of the canine may develop the alveolar ridge in a patient with a congenitally missing lateral incisor, the bone width may not be sufficient for ideal placement of an implant without grafting.26
Some patients have experienced progressive reduction of the marginal bone levels at the teeth adjacent to implants.13,19,27-29 Finally, implant crowns are more likely than natural teeth to experience gingivitis, increased probing depths, and bleeding on probing.21,30
Collaboration among the orthodontist, general dentist, and prosthodontist is of paramount importance in cases such as this.31-33 In our patient, as in similar reports of canine substitution,32 the functional guidance achieved during lateral excursions was bilateral group function. According to Nordquist and McNeill, there are no significant differences in occlusion and periodontal health between canine guidance and group function.34
TADs can provide adequate support in asymmetrical situations, such as our patient’s, and when maximum anchorage is required.35,36 We preferred to use mini-implants because they are simple to insert and no healing time is required, unlike with osseointegrated anchorage devices.37,38 Mini-implants have a mean failure rate of only 13.5%, indicating their usefulness in clinical practice.39 Palatal implants and miniscrews exhibit even lower failure rates, according to a systematic review by Kakali and colleagues: 6% for palatal implants (range 0-26.1%) and 6.1% for palatal miniscrews (range 0-33.3%).40 Therefore, in most orthodontic cases, the choice of anchorage devices may be determined by other factors, including cost, patient comfort, personal preference, familiarity with the device, and insertion procedures.40
The main advantage of the appliance we used over other palatal devices41 is the indirect anchorage provided by the auxiliary arm affixed to the palatal surface of the upper central incisor. The appliance can easily be bent without welding the auxiliary arm. This system prevents further anchorage loss, especially with asymmetrical tooth movement. Additionally, our method applies not only a palatal force, but also a concurrent labial force from elastomeric power chain, thus enhancing the space closure.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
- **Trademark of Strite Industries Ltd., Cambridge, ON, Canada; www.speedsystem.com.
- ***Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- †Promedia Medizintechnik, Siegen, Germany; www.ortholox.de.
REFERENCES
- 1. Sabri, R.: Treatment of a unilateral Class II crossbite malocclusion with traumatic loss of a maxillary central incisor and a lateral incisor, Am. J. Orthod. 130:759-770, 2006.
- 2. Huang, S.; Kang, T.; and Duan, Y.: Traumatic loss of a maxillary central incisor treated with nonextraction orthodontics, Am. J. Orthod. 143:246-253, 2013.
- 3. Turpin, D.L.: Treatment of missing lateral incisors, Am. J. Orthod. 125:129, 2004.
- 4. Kokich, V.G.; Nappen, D.L.; and Shapiro, P.A.: Gingival contour and clinical crown length: Their effects on the esthetic appearance of maxillary anterior teeth, Am. J. Orthod. 86:89-94, 1984.
- 5. Kokich, V.G. and Crabill, K.E.: Managing the patient with missing or malformed maxillary central incisors, Am. J. Orthod. 129:S55-S63, 2006.
- 6. Zachrisson, B.U.: Planning esthetic treatment after avulsion of maxillary incisors, J. Am. Dent. Assoc. 139:1484-1490, 2008.
- 7. Bourassa, C.; Hosein, Y.K.; Pollmann, S.I.; Galil, K.; Bohay, R.N.; Holdsworth, D.W.; and Tassi, A.: In-vitro comparison of different palatal sites for orthodontic miniscrew insertion: Effect of bone quality and quantity on primary stability, Am. J. Orthod. 154:809-819, 2018.
- 8. Baumgaertel, S.: Quantitative investigation of palatal bone depth and cortical bone thickness for mini-implant placement in adults, Am. J. Orthod. 136:104-108, 2009.
- 9. Hourfar, J.; Ludwig, B.; Bister, D.; Braun, A.; and Kanavakis, G.: The most distal palatal ruga for placement of orthodontic mini-implants, Eur. J. Orthod. 37:373-378, 2015.
- 10. Hourfar, J.; Bister, D.; Lux, C.J.; Al-Tamimi, B.; and Ludwig, B.: Anatomic landmarks and availability of bone for placement of orthodontic mini-implants for normal and short maxillary body lengths, Am. J. Orthod. 151:878-886, 2017.
- 11. Rosa, M. and Zachrisson, B.U.: Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors, J. Clin. Orthod. 35:221-234, 2001.
- 12. Rosa, M. and Zachrisson, B.U.: Integrating esthetic dentistry and space closure in patients with missing maxillary lateral incisors: Further improvements, J. Clin. Orthod. 41:563-573, 2007.
- 13. Rosa, M. and Zachrisson, B.U.: The space-closure alternative for missing maxillary lateral incisors: An update, J. Clin. Orthod. 44:540-549, 2010.
- 14. Rosa, M. and Zachrisson, B.U.: Missing maxillary lateral incisors: New procedures and indications for optimal space closure, in Esthetics and Biomechanics in Orthodontics, 2nd ed., ed. R. Nanda, Elsevier Saunders, St. Louis, 2014.
- 15. Rosa, M.; Lucchi, P.; Ferrari, S.; Zachrisson, B.U.; and Caprioglio, A.: Congenitally missing maxillary lateral incisors: Long-term periodontal and functional evaluation after orthodontic space closure with first premolar intrusion and canine extrusion, Am. J. Orthod. 149:339-348, 2016.
- 16. Wilson, T.G. Jr. and Ding, T.A.: Optimal therapy for missing lateral incisors? Am. J. Orthod. 126:22A-23A, 2004.
- 17. Antosz, M.: Space closure for a missing central incisor, letter to the editor, Am. J. Orthod. 124:18A, 2003.
- 18. Zachrisson, B.U. and Stenvik, A.: Single implants—optimal therapy for missing lateral incisors? Am. J. Orthod. 126:A13-A15, 2004.
- 19. Thilander, B.; Odman, J.; and Lekholm, U.: Orthodontic aspects of the use of oral implants in adolescents: A 10-year follow-up study, Eur. J. Orthod. 23:715-731, 2001.
- 20. Oesterle, L.J. and Cronin, R.J. Jr.: Adult growth, aging, and the single-tooth implant, Int. J. Oral Maxillofac. Implants 15:252-260, 2000.
- 21. Chang, M.; Wennström, J.L.; Odman, P.; and Andersson, B.: Implant supported single-tooth replacements compared to contralateral natural teeth: Crown and soft tissue dimensions, Clin. Oral Implants Res. 10:185-194, 1999.
- 22. Tuverson, D.L.: Close space to treat missing lateral incisors, Am. J. Orthod. 125:17A, 2004.
- 23. Plakwicz, P.; Fudalej, P.; and Czochrowska, E.M.: Transplant vs implant in a patient with agenesis of both maxillary lateral incisors: A 9-year follow-up, Am. J. Orthod. 149:751-756, 2016.
- 24. Olsen, T.M. and Kokich, V.G. Sr.: Postorthodontic root approximation after opening space for maxillary lateral incisor implants, Am. J. Orthod. 137:158-159, 2010.
- 25. Gakonyo, J.; Mohamedali, A.J.; and Mungure, E.K.: Cone beam computed tomography assessment of the buccal bone thickness in anterior maxillary teeth: Relevance to immediate implant placement, Int. J. Oral Maxillofac. Implants 33:880-887, 2018.
- 26. Uribe, F.; Chau, V.; Padala, S.; Neace, W.P.; Cutrera, A.; and Nanda, R.: Alveolar ridge width and height changes after orthodontic space opening in patients congenitally missing maxillary lateral incisors, Eur. J. Orthod. 35:87-92, 2013.
- 27. Silveira, G.S.; de Almeida, N.V.; Pereira, D.M.T.; Mattos, C.T.; and Mucha, J.N.: Prosthetic replacement vs space closure for maxillary lateral incisor agenesis: A systematic review, Am. J. Orthod. 150:228-237, 2016.
- 28. Muhamad, A.H.; Nezar, W.; and Azzaldeen, A.: Managing congenitally missing lateral incisors with single tooth implants, Dent. Oral Craniofac. Res. 2:318-324, 2016.
- 29. Jamilian, A.; Perillo, L.; and Rosa, M.: Missing upper incisors: A retrospective study of orthodontic space closure versus implant, Prog. Orthod. 16:2, 2015.
- 30. Thordarson, A.; Zachrisson, B.U.; and Mjör, I.A.: Remodeling of canines to the shape of lateral incisors by grinding: A long-term clinical and radiographic evaluation, Am. J. Orthod. 100:123-132, 1991.
- 31. Park, J.H.; Okadakage, S.; Sato, Y.; Akamatsu, Y.; and Tai, K.: Orthodontic treatment of a congenitally missing maxillary lateral incisor, J. Esth. Restor. Dent. 22:297-312, 2010.
- 32. Konstantonis, D.; Brenner, R.; Karamolegkou, M.; and Vasileiou, D.: Torturous path of an elastic gap band: Interdisciplinary approach to orthodontic treatment for a young patient who lost both maxillary central incisors after do-it-yourself treatment, Am. J. Orthod. 154:835-847, 2018.
- 33. Janson, G.; Valarelli, D.P.; Valarelli, F.P.; de Freitas, M.R.; and Pinzan, A.: Atypical extraction of maxillary central incisors, Am. J. Orthod. 138:510-517, 2010.
- 34. Nordquist, G.G. and McNeill, R.W.: Orthodontic vs. restorative treatment of the congenitally absent lateral incisor—long term periodontal and occlusal evaluation, J. Periodontol. 46:139-143, 1975.
- 35. Jung, M.H.: Asymmetric extractions in a patient with a hopeless maxillary central incisor, followed by treatment with mini-implant anchorage, Am. J. Orthod. 153:716-729, 2018.
- 36. Ganzer, N.; Feldmann, I.; and Bondemark, L.: Anchorage reinforcement with miniscrews and molar blocks in adolescents: A randomized controlled trial, Am. J. Orthod. 154:758-767, 2018.
- 37. Chen, Y.; Kyung, H.M.; Zhao, W.T.; and Yu, W.J.: Critical factors for the success of orthodontic mini-implants: A systematic review, Am. J. Orthod. 135:284-291, 2009.
- 38. Feldmann, I. and Bondemark, L.: Anchorage capacity of osseointegrated and conventional anchorage systems: A randomized controlled trial, Am. J. Orthod. 133:339.e19-e28, 2008.
- 39. Papageorgiou, S.N.; Zogakis, I.P.; and Papadopoulos, M.A.: Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis, Am. J. Orthod. 142:577-595, 2012.
- 40. Kakali, L.; Alharbi, M.; Pandis, N.; Gkantidis, N.; and Kloukos, D.: Success of palatal implants or mini-screws placed median or paramedian for the reinforcement of anchorage during orthodontic treatment: A systematic review, Eur. J. Orthod. 41:9-20, 2019.
- 41. Wilmes, B.; Nienkemper, M.; Nanda, R.; Lübberink, G.; and Drescher, D.: Palatally anchored maxillary molar mesialization using the Mesialslider, J. Clin. Orthod. 47:172-179, 2013.






COMMENTS
.