OVERVIEW
Indications and Management Protocol for the Use of Splints with the "Surgery First" Approach
In this regular column, JCO provides an overview of a clinical topic of interest to orthodontists. Contributions and suggestions for future subjects are welcome.
The objective of orthognathic surgery is to correct dentoskeletal deformities while improving facial esthetics and occlusal function.1-3 The traditional three-stage approach, involving 15-24 months of presurgical orthodontics, orthognathic surgery, and seven to 12 months of postsurgical orthodontics, is considered the standard therapy.4-10 Disadvantages include the overall duration of treatment and the temporary worsening of the patient’s esthetic and functional aspects during the presurgical orthodontic phase.8,11-14
The “surgery first” approach was proposed by Nagasaka and colleagues in 2009 to minimize or eliminate such drawbacks while still allowing excellent results to be achieved.15,16 Because of these advantages, the “surgery first” method can have a positive impact on patient compliance during postsurgical orthodontic treatment.17
While usage of the “surgery first” approach has grown exponentially in recent years because of improved three-dimensional planning techniques and increased demand, its potential seems to be limited by numerous contraindications.8-10,18-20 In general, the “surgery first” approach is indicated in patients who do not need too much presurgical orthodontic alignment and decompensation, such as those with well-aligned to mildly crowded anterior teeth, flat to mild curves of Spee, and normal to mildly proclined or retroclined incisors.21 Exclusion criteria, as defined by Peiró-Guijarro and colleagues, are any occlusal conditions with the potential to compromise the surgical procedure or the clinical outcome, including severe crowding that requires extractions; significant facial asymmetry with 3D dental compensations or chin deviation; severe transverse discrepancy treated previously with surgically assisted rapid palatal expansion; arch discrepancy; missing teeth; or Class II, division 2 malocclusion with overbite.8 In short, the literature suggests reserving the “surgery first” approach for milder malocclusions, primarily Class III.
The potential for skeletal and occlusal instability is a major drawback of the “surgery first” approach. A systematic review indicated that mandibular relapse in Class III patients is more conspicuous with the “surgery first” approach than with conventional surgical-orthodontic treatment.22 The difference was attributed to a marked tendency of mandibular counterclockwise rotation to compromise vertical stability, inevitably causing sagittal relapse. The authors therefore suggested more careful selection of patients for the “surgery first” approach, as well as a planned overcorrection in the surgical position of the jaws. In our opinion, however, the term “relapse” is inappropriate because the changes in the vertical dimension and the sagittal projection of the mandible are related to the conversion of an unstable occlusal relationship with cusp-to-cusp contacts to a maximum physiological intercuspation. These changes are predictable and should not be considered true relapse.23 In our experience, the counterclockwise rotation of the mandible is caused by the vertical reduction and mandibular advancement between the planned transitional malocclusion and the final occlusion. This movement should be anticipated during presurgical planning by simulating the final occlusion.
Regarding postoperative occlusal stability, many authors have identified orthodontic extractions as one of the main contraindications to the “surgery first” approach.8,9,18 Uribe and colleagues described a Class III extraction case utilizing a “surgery early” or “surgery first modified” approach, with the surgery following a brief initial orthodontic alignment.24 Depending on the timing of orthognathic surgery, various approaches have been categorized as “surgery first,” “surgery early,” “surgery late,” ”surgery last,” “surgery only,” or “surgery never.”4 In extraction cases, orthognathic surgery should not be performed until the overcrowding has been resolved and most of the extraction space has been closed (“surgery early”), even if there are premature occlusal contacts that could create occlusal instability after surgery.4
Splint Management
The role of the occlusal splint (or wafer) is well established in both elective orthognathic surgery and in the “surgery first” approach. During the analytic model surgery, the planned 3D movements are transferred to the patient through specific measurements and reference points and a custom-made surgical splint. For a one-jaw maxillary or mandibular procedure, a single final splint is required after reproduction of the osteotomized jaw movement. For a double-jaw procedure, an intermediate splint is recommended to relate the osteotomized maxilla (or mandible) to the stable mandible (or maxilla), in addition to a final splint that relates the osteotomized mandible (or maxilla) to the fixated maxilla (or mandible).
In the “surgery first” approach, it is essential to reproduce and maintain the planned postoperative malocclusion, which can be unstable because of the lack of presurgical orthodontic treatment. The surgical splint helps to provide occlusal stability, to stabilize jaw osteotomies (often segmental), and sometimes to stabilize and control the malocclusion during the postsurgical period and the subsequent orthodontic treatment. If postoperative occlusal instability is not properly managed by the orthodontist, it could lead to unsatisfactory esthetic and occlusal results.
Despite the importance of splints in the “surgery first” approach, few studies have been reported. We published an article about the use of an occlusal splint to reposition the condyles before orthognathic surgery.39 Nine studies have described the use of intermediate splints10,13,19,20,34,37,39-41; six of these involved computer-aided design and manufacturing (CAD/CAM).13,19,34,37,39,40
Of 24 articles describing the management of final splints in the “surgery first” approach, two indicated their use only for surgery,30,34 18 reported their use for specific periods after surgery,13-16,19,20,25-29,31-33,35-38 and four did not report the duration of splint wear after surgery.10,39-41 Four case reports described modifications of the final splints during the postsurgical period.15,26,29,33
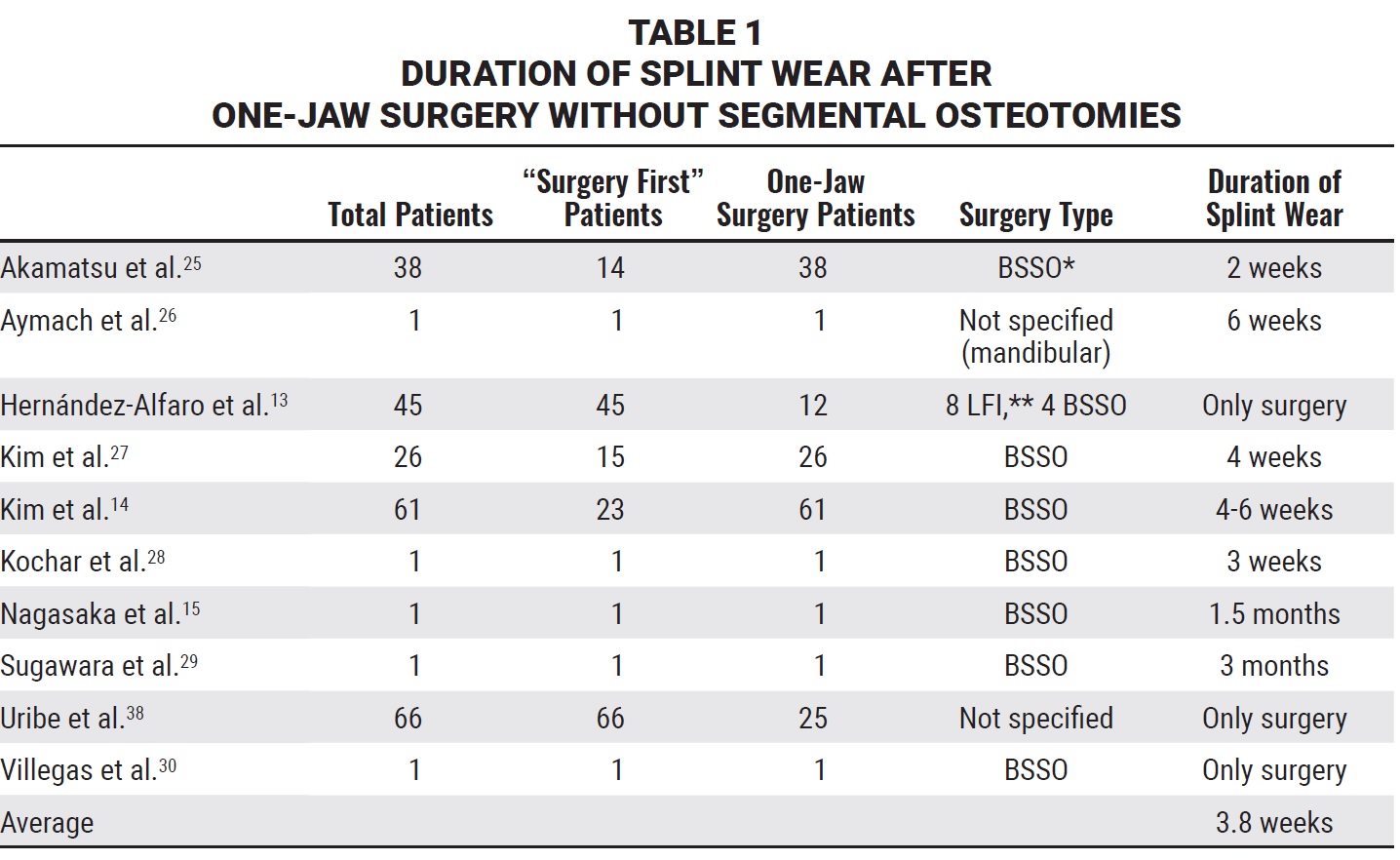
Only four authors indicated that the duration of splint wear after surgery was dependent on the type of surgery performed; in these cases, the final splints were used only after maxillary transverse expansion or segmental osteotomies.13,19,37,38 Overall, the duration of final splint wear ranged from one week to three months. For one-jaw surgeries, the average duration of splint wear after surgery was 3.8 weeks (Table 1).
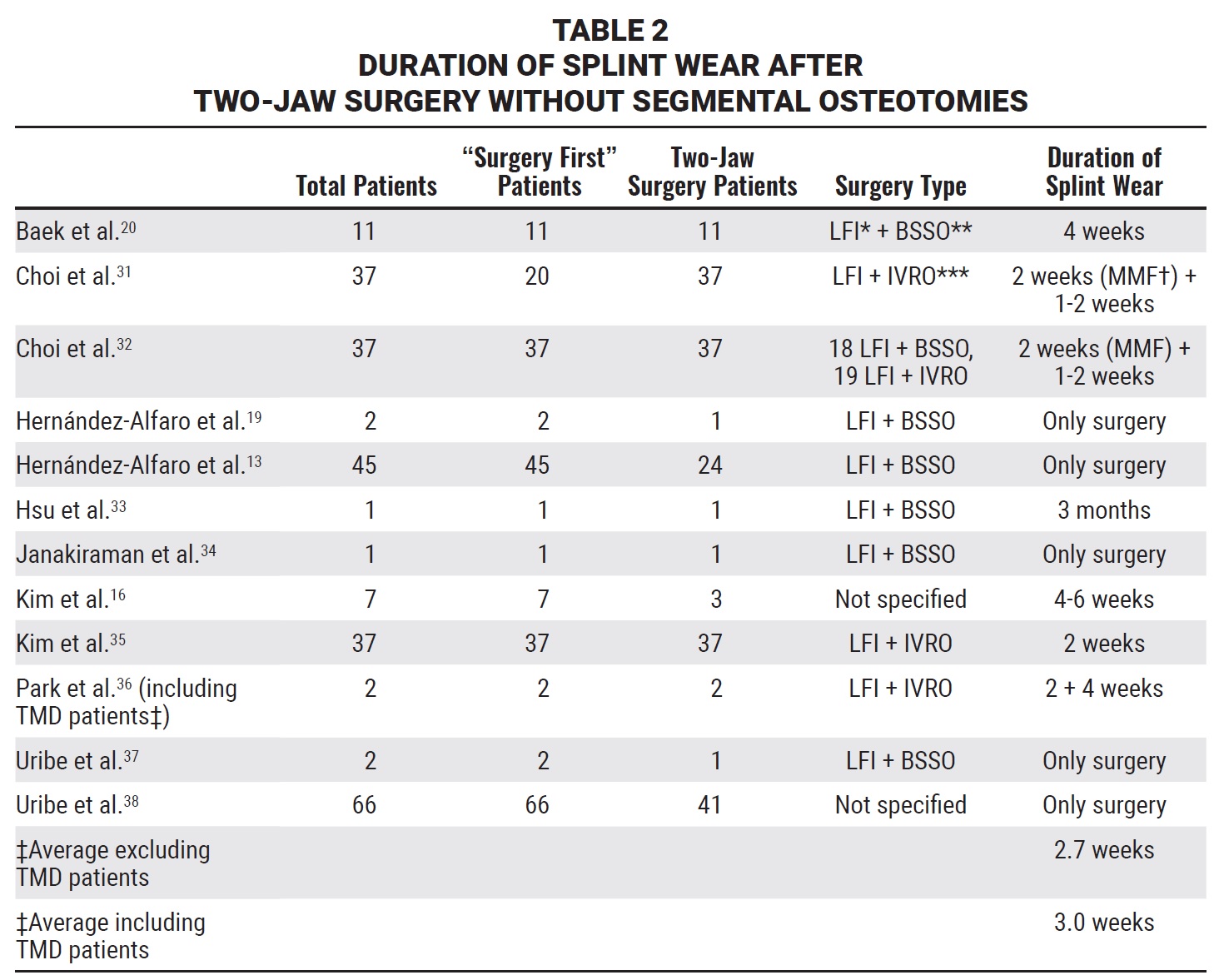
For two-jaw surgeries, the average was three weeks if the one study that enrolled TMD patients36 was included, and 2.7 weeks if that study was excluded (Table 2).
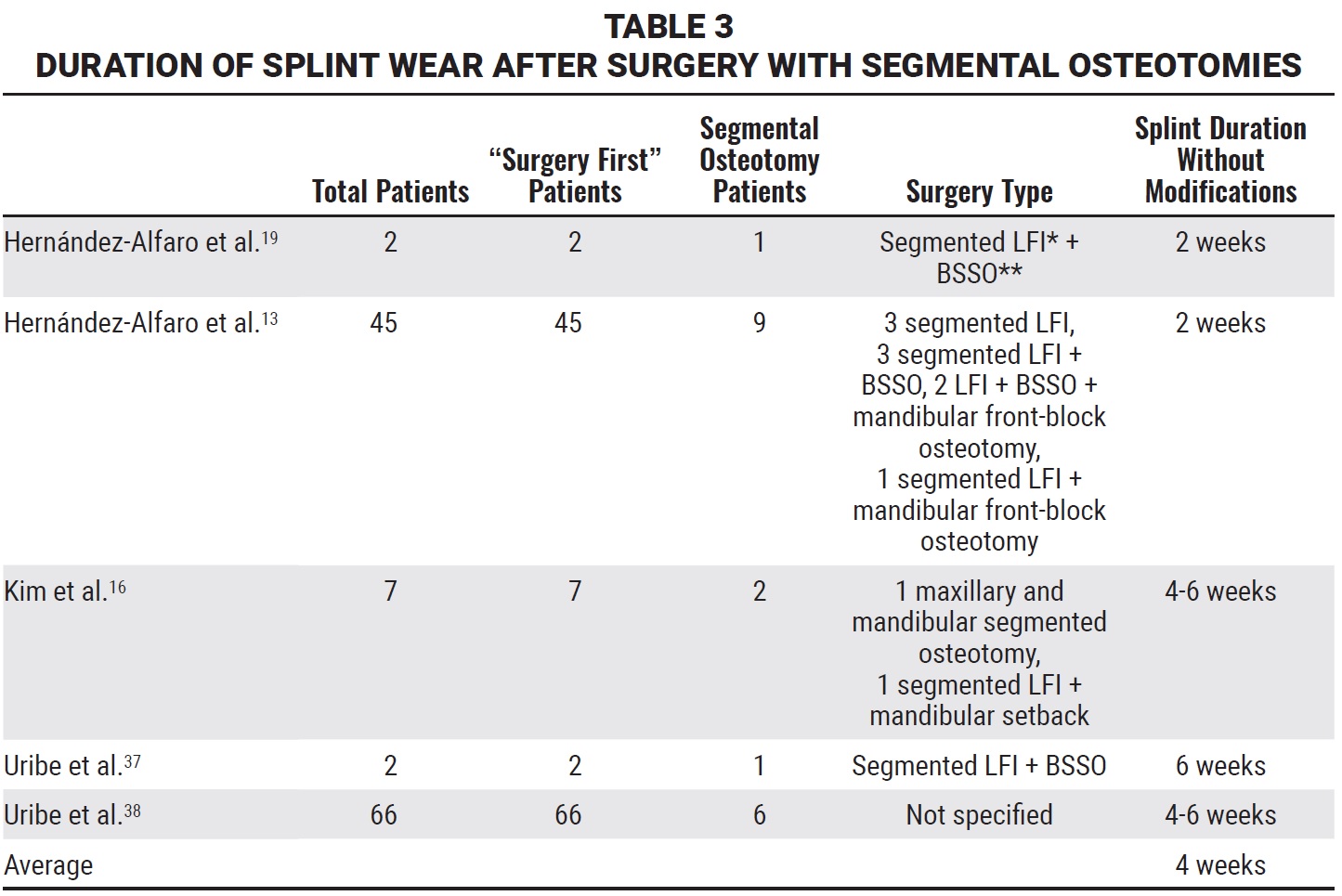
A longer average duration, four weeks, was reported after segmental osteotomies (Table 3).
The duration of splint wear would understandably increase in cases of occlusal instability or following segmental osteotomies, as would be true with conventional surgical-orthodontic treatment.
In the Maxillofacial Surgery Unit of the Fondazione Policlinico Universitario Agostino Gemelli IRCCS, we distinguish among four types of splints for use with the “surgery first” approach.
Repositioning splint.39 This splint is helpful in a patient who exhibits TMD before surgery and undergoes a gnathological therapy to determine the analgesic and functional position of the condyles and their proper relationship to the other joint structures. The purpose of the repositioning splint is to record the positions of the condyles as defined by the gnathological therapy and to maintain them after the surgical osteotomies and repositioning of the dental arches.
Intermediate splint. An osteotomy wafer is routinely used in orthognathic surgery as an intermediate guide for repositioning the mobilized jaw relative to the intact jaw. An intermediate splint is used in bimaxillary surgery to guide the movement of one jaw relative to the other. There is some margin of error because the mandible is not a fixed bone, and therefore the condyle may not maintain its exact position within the glenoid fossa. An intermediate splint is mandatory in “mandible first” procedures and in “maxilla first” procedures when complex 3D movements of the maxilla are planned.
Final splint. Conventional orthognathic surgical planning requires precise movement of the jawbone segments. An interocclusal final wafer records and stabilizes the final occlusal relationship between the osteotomized maxilla and mandible. With the “surgery first” approach, however, the final splint establishes the objectives of a postsurgical transitional malocclusion.
In our initial experience with the “surgery first” approach, the final splint was maintained for 20 days and eventually used with elastics for occlusal stability. In most cases today, we use a final splint only as an occlusal check during the surgical procedure. For surgery involving segmental osteotomies or transverse maxillary expansion or in patients with occlusal instability due to deflecting precontacts, we maintain the final splint for at least two weeks after surgery.
Dynamic splint. We have recently developed a modification of the final splint to be worn during the initial phase of postsurgical orthodontic therapy, until the removal of occlusal interferences. Postsurgical occlusal instability seems to be the most critical disadvantage of the “surgery first” approach, because it can lead to skeletal instability.8,9,21 Some authors recommend the presence of at least three occlusal stops during the postsurgical transitional malocclusion.16 Alternatively, with a “surgery early” approach, a short period of presurgical orthodontic treatment could eliminate the source of postoperative occlusal instability.4
The dynamic splint allows orthodontic treatment to be started as soon as possible after surgery, taking full advantage of the regional acceleratory phenomenon (RAP), which begins immediately after surgery and lasts for about three months. Even with a segmental osteotomy, when splint stabilization is needed for several days after surgery, the dynamic splint can promote the RAP during the stabilization phase, thus reducing the overall treatment time. The dynamic splint can also be used as an occlusal build-up to permit orthodontic movements that would otherwise be impeded by the opposing teeth, as with the proclination of upper anterior teeth in a Class II, division 2 malocclusion.
Two consecutive clinical cases are presented in this article to illustrate our protocol for the management of orthognathic occlusal splints, which allows us to treat even complex malocclusions.
Case 1
A 22-year-old female presented for treatment (Fig. 1). Facial esthetic analysis42-48 noted a symmetrical face with good proportions, although the nasolabial fold, the angular area of the labial rim, and the cheekbone contour at Mx point indicated middle-third retrusion. The patient exhibited a complex smile with a smile index49,50 of 62; the lip line was extremely low, with the upper lip almost totally concealing the incisors (−6mm) and the premolars (−6mm). The upper lip was festooned in a commissural smile. Black corridors were noticeable, owing to the retrusion and hypoplasia of the middle facial third. The profile was flat, with a facial angle of 179°. The nasolabial angle (103°), upper (29°) and lower (−74°) side angles, and chin-throat distance were normal.

Fig. 1 Case 1. 22-year-old female patient with skeletal Class III malocclusion and retrusive maxilla before treatment.
Intraoral examination found agenesis of the four second premolars, previous extraction of the lower right first molar, and a retained deciduous upper right canine and second molar. The upper right canine and lateral incisor were transposed, the upper right lateral incisor was palatally positioned, and the upper right central incisor was rotated 90°. The lower left first and second molars and lower right second molar were mesially inclined; the molar relationship was Class III. The upper arch was narrow, with severe crowding in the anterior segment, but the lower anterior teeth exhibited spacing. The Bolton Index was affected by the presence of hypoplastic lateral incisors.
Cephalometric analysis confirmed a mesofacial pattern (FMA = 24°, LFH = 47°), a skeletal Class III malocclusion (convexity = −7.3mm), and a retrusive maxilla (maxillary depth = 82°). The upper incisors were proclined (U1-OP = 47°), and the lower incisors were retroclined (L1-OP = 81°). The anterior maxillary height was deficient (Sn′-U1 = 17.5), but the anterior mandibular height (L1-M′) was almost normal. Projections to the true vertical line (TVL) appeared normal except for soft-tissue B-point (4mm) and soft-tissue pogonion (7mm), which were protrusive.
Radiological examination revealed previous endodontic treatment of the lower central incisors and a malformed upper right central incisor root. Three-dimensional facial images acquired with the 3dMDtrio* system (Fig. 2) showed that the maxillary retrusion was much more serious than it had appeared from the two-dimensional study of facial esthetics. The patient showed no signs or symptoms of TMD.
After being informed of the advantages and disadvantages of the “surgery first” approach compared with conventional surgical-orthodontic treatment, the patient opted for “surgery first” treatment. The surgery would involve a Le Fort I osteotomy for advancement and transverse expansion of the maxilla, as well as a bilateral sagittal split osteotomy (BSSO) with slight setback of the mandible to achieve the planned occlusion (Fig. 3).
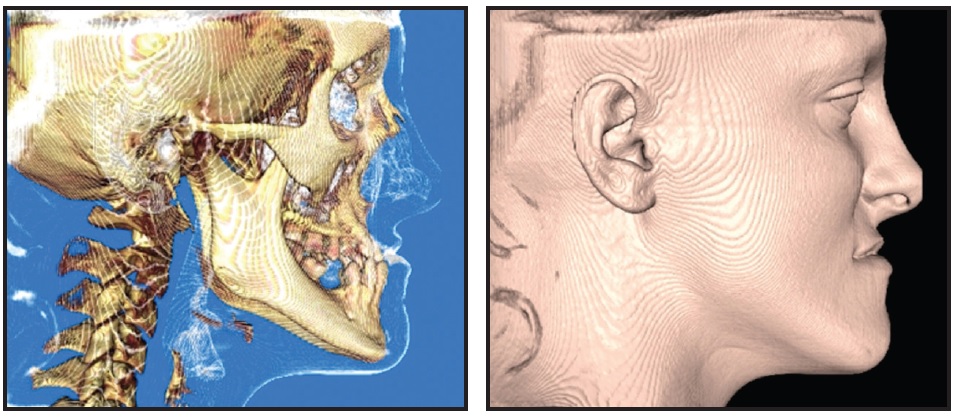
Fig. 2 Case 1. Three-dimensional facial analysis of hard- and soft-tissue images from cone-beam computed tomography (CBCT).
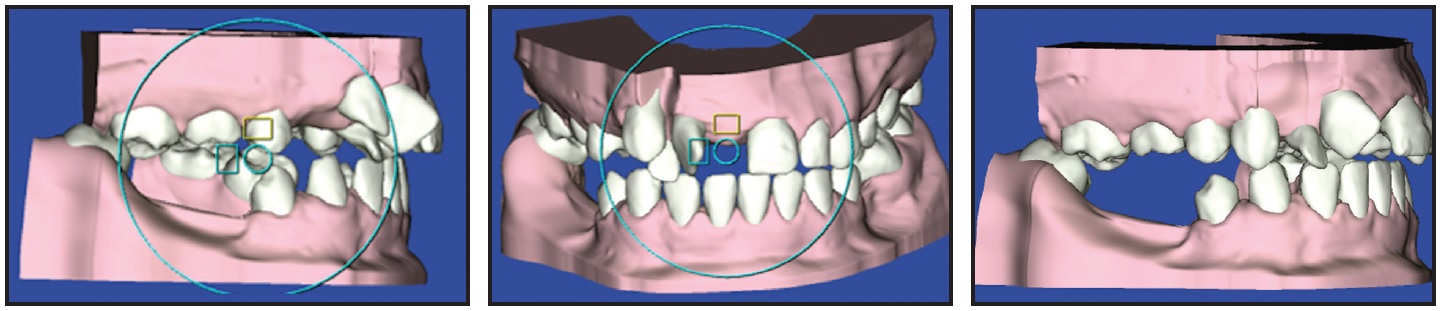
Fig. 3 Case 1. 3D SureSmile** simulations used to plan postsurgical occlusion in “surgery first” approach, with upper right canine to be distalized orthodontically while occlusal splint is worn.
Orthodontic treatment objectives in the upper arch were to distalize the permanent right canine into contact with the right first premolar, after extraction of the retained deciduous right canine, and to derotate the right central incisor. We planned to gain enough space between the root apices of the right central incisor and permanent canine to allow proclination of the right lateral incisor and subsequent labial root torque. The distally inclined left first premolar and mesially inclined left first molar would be uprighted. Treatment objectives for the lower arch were to procline the incisors and close the anterior spaces, allowing mesialization of the premolars and canines and distal inclination of the left first and second molars and right second molar. This would reestablish the correct dental inclinations for subsequent prosthetic treatment.
Visual treatment simulations were performed using Dolphin*** version 9.0 (Fig. 4). The first visual tracing represented the overall surgical-orthodontic treatment, in which the final positions of the upper incisors were predicted, and the second referred only to the “surgery first” approach, copying the final position of the jaws from the first tracing. This second tracing allowed the postsurgical overjet to be predicted.
Dental casts were mounted on a SAM 2† articulator, and model surgery was performed based on the clinical facial analysis and surgical prediction tracings. Using ProPlan CMF‡ software, the patient’s cone-beam computed tomography†† (CBCT) images (Fig. 2) were combined with intraoral digital scans of the dental arches from a TRIOS‡‡ scanner.
The postsurgical occlusion (Fig. 3) was established with virtual models using Elemetrix††† software. The surgeon first reproduced the movements of the upper jaw in 3D, working with all six degrees of freedom (Fig. 5).
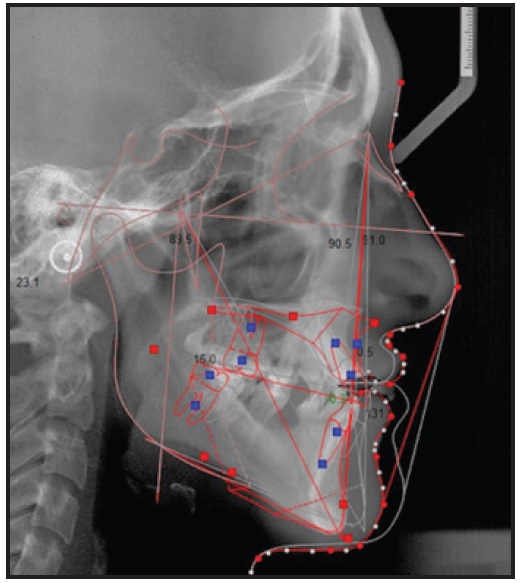
Fig. 4 Case 1. 2D visual treatment simulation created with Dolphin*** version 9.0.
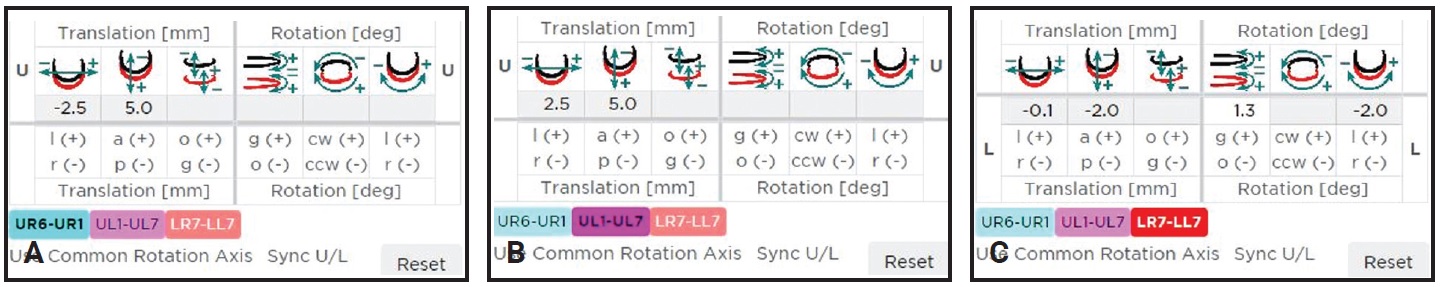
Fig. 5 Case 1. Six degrees of freedom (translation vector and rotation matrix). A. Osteotomized right hemimaxilla. B. Osteotomized left hemimaxilla. C. Osteotomized mandibular segments.
Some of these shifts were copied from the 2D visual tracings. The mandible was then positioned in the final occlusion, based on the prediction tracings. Finally, the surgical expansion of the maxilla required to achieve a stable occlusion was added. The virtual image of the final splint was obtained from the stereolithographic (STL) files of the postsurgical occlusion (Fig. 6).
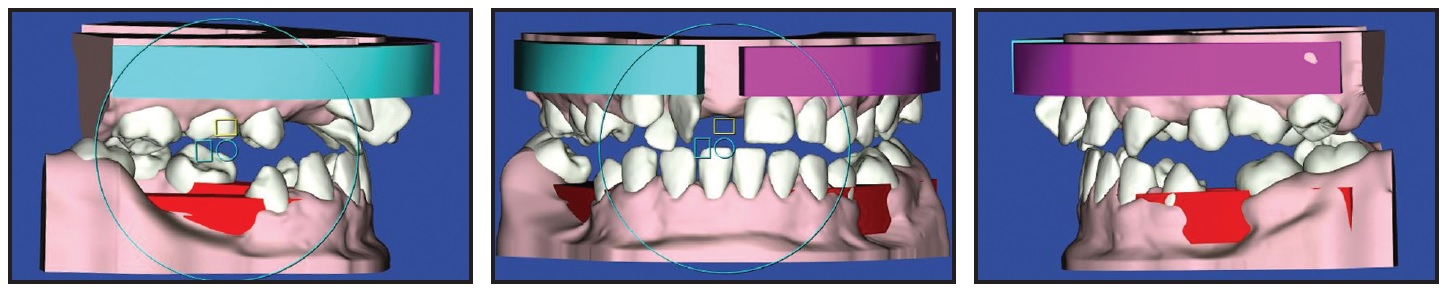
Fig. 6 Case 1. Planned postsurgical occlusion used to obtain stereolithographic (STL) file of virtual final splint.
In a second step, all surgical movements of the lower jaw were eliminated, and the STL file of the intermediate splint occlusion was obtained from this position (Fig. 7).
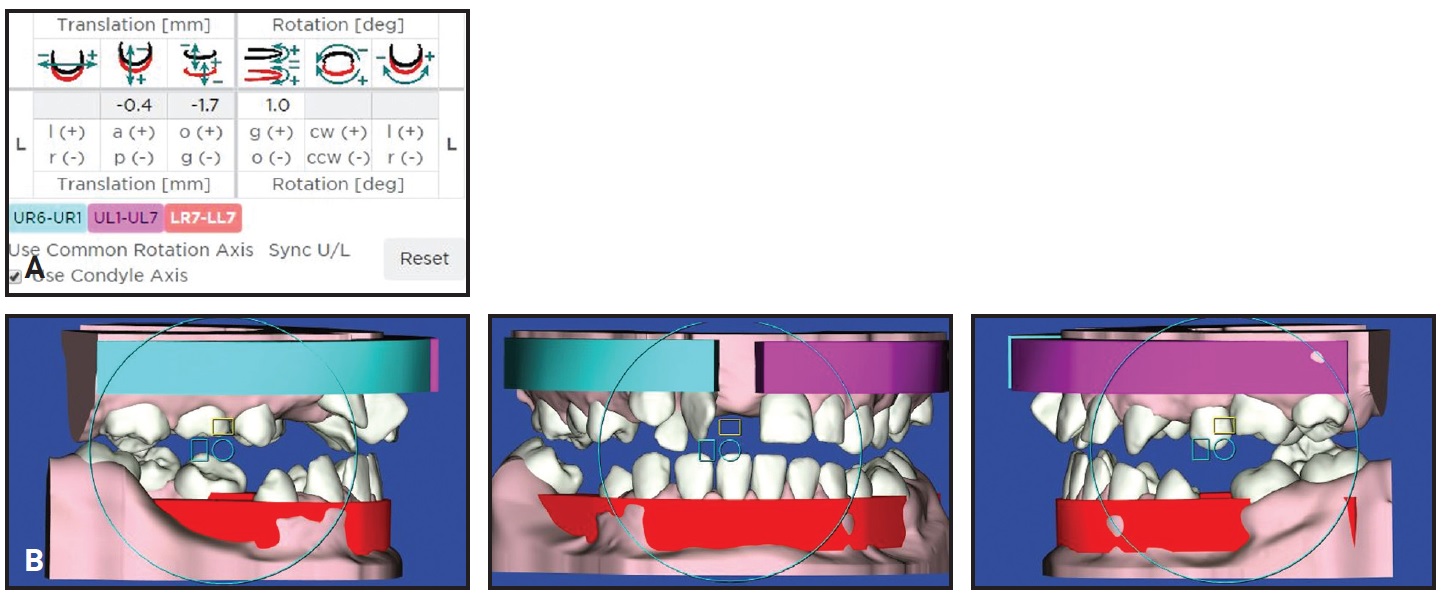
Fig. 7 Case 1. A. Six degrees of freedom (translation vector and rotation matrix) with surgical movements of mandible eliminated. B. STL file for intermediate splint obtained from this position.
The STL files were sent to the technician, who processed the images using Exocad‡‡‡ software. The surgical splints were designed to include holes for metal ligatures in the interproximal spaces. The software determines the thickness of resin needed to avoid fractures during surgery; if this minimum thickness is not achieved, the splint planning must be reevaluated. In the present case, the thickness was appropriate. The STL files with 3D images of the surgical splints were transferred to a DWS 020D§ prototyping machine, which printed the splints in Dental SG§§ surgical resin. The final splint was cut away in the area of the upper right permanent canine and retained deciduous canine to allow the programmed distalization of the permanent canine.
A few days before surgery, .018" MBT§§§ preadjusted appliances were bonded, and passive sectional .017" × .025" stainless steel wires were inserted in both arches. During surgery, a Le Fort I osteotomy was performed to advance the maxilla 6mm and expand it 3mm, a BSSO was performed with a slight setback of the mandible, and the deciduous upper right canine was extracted.
A few days after surgery, the passive sectional wires were removed. The patient wore the occlusal splint for six weeks; during this period, the permanent upper right canine was distalized with light elastomeric chain until it almost contacted the first premolar (Fig. 8).
After removal of the occlusal splint, the upper right canine was distalized without loss of anchorage. The space gained was sufficient for derotation of the upper right central incisor and proclination of the upper right lateral incisor.
In the subsequent orthodontic phase, the initial orthodontic brackets were replaced with more efficient low-friction .018" MBT-prescription appliances. The upper right central incisor was rotated with an .014" stainless steel auxiliary power arm attached to .014" and then .016" nickel titanium archwires. After 12 weeks, when we had obtained enough coronal space for the upper right lateral incisor, we increased the space between the upper right canine and central incisor at the apical level by repositioning the brackets to accentuate the distal root inclination of the canine and the mesial root inclination of the central incisor. Another 12 weeks later, after the necessary space was gained, the upper right lateral incisor was proclined and then uprighted with labial root torque, using an .014" Warren spring on an .018" stainless steel archwire (Fig. 9).
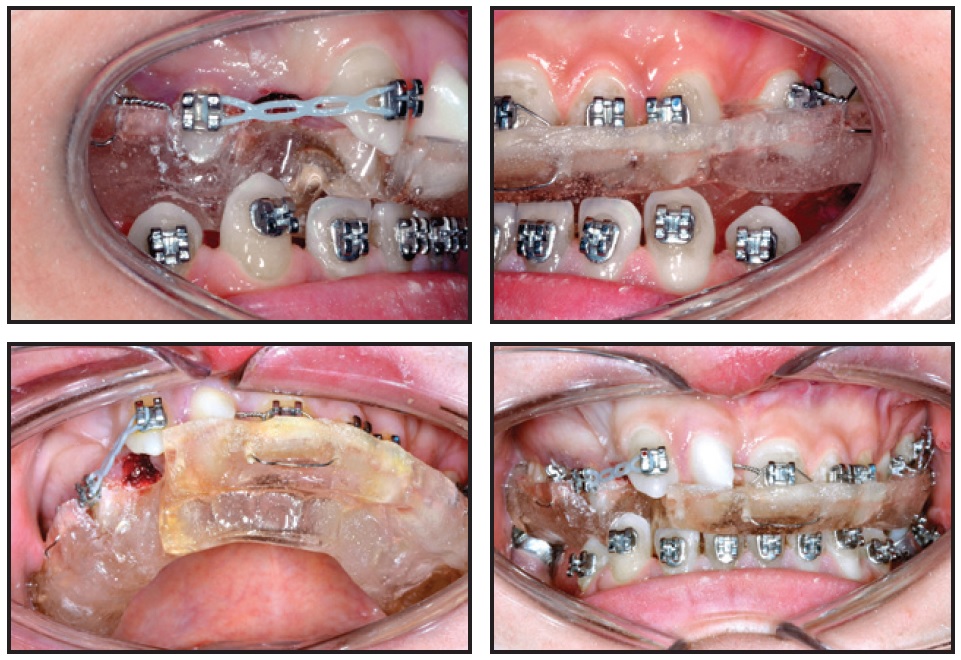
Fig. 8 Case 1. Orthodontic distalization of upper right canine after Le Fort I and bilateral sagittal split osteotomies, with patient still wearing final splint for six weeks.

Fig. 9 Case 1. Seven months after surgery, upper right lateral incisor proclined and uprighted with labial root torque, using .014" Warren spring on .018" stainless steel archwire; lower incisors proclined and molars uprighted using .016" × .022" Elgiloy**** Blue archwire with steps at edentulous spaces.
Leveling of the lower arch was initiated with .012" nickel titanium sectional wires and an .016" × .016" Elgiloy**** Blue overlay wire between the central and lateral incisors. One month later, the lower incisor proclination and molar uprighting were begun using an .016" × .022" Elgiloy Blue utility arch and then an .016" × .022" Elgiloy Blue continuous archwire with steps at the edentulous spaces (Fig. 9), along with .014" and .016" nickel titanium piggyback wires.
After 11 months of treatment, the lower anterior spaces were closed by mesializing the lower canines and premolars. Finishing archwires were .016" × .022" and .017" × .025" nickel titanium in the upper arch and .016" × .022" Elgiloy and .017" × .025" stainless steel in the lower arch.
Total treatment time was 15 months (Fig. 10).
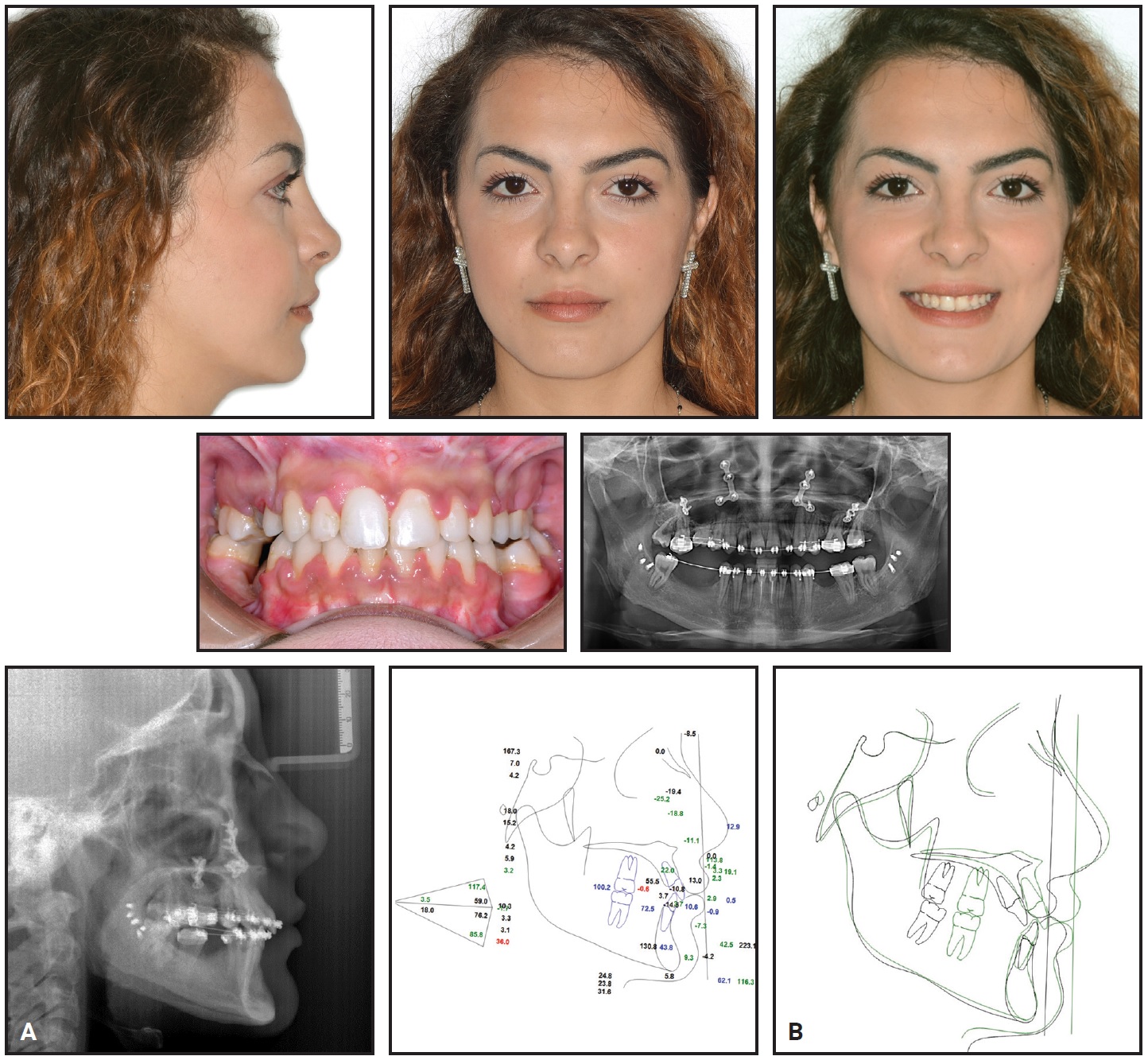
Fig. 10 Case 1. A. Patient after 15 months of treatment. (Radiographs taken one week before debonding.) B. Superimposition of pre- and post-treatment cephalometric tracings.
A satisfactory occlusion was achieved, with normal overjet and overbite, and a Class I canine relationship was attained. There was a noticeable improvement in facial esthetics, mainly because of the postero-anterior increase in the middle facial third. The black corridors disappeared in smiling, and the lip line and smile arc were refined. Cephalometric tracings confirmed the skeletal and occlusal improvements, although transverse issues remained because the patient decided to stop treatment for personal reasons.
Thermoformed retainers were delivered for both arches, and the patient was sent back to the surgeon for preprosthetic treatment prior to implant placement (Fig. 11).
Case 2
A 42-year-old female presented with no prior history of orthodontic treatment (Fig. 12). Facial esthetic analysis42-48 indicated a symmetrical face with the maxillary and mandibular dental midlines deviating from the facial midline. The facial proportions were generally good, but there was a slight vertical excess of the lower facial third, and the nasolabial fold and the angular area of the labial rim showed signs of a mildly retrusive middle facial third. Smile analysis found a commissural smile with a smile index49,50 of 50. In smiling, the lip line was at the gingival margin of the incisors, but there was 5mm of exposed gingiva at the premolars. The upper lip was festooned. The profile was nearly normal, with a slightly excessive facial angle (174°), a nasolabial angle of 92°, a proper lip position, and a normal chin-throat distance.

Fig. 11 Case 1. Patient after implant-prosthetic rehabilitation.

Fig. 12 Case 2. 42-year-old female with skeletal Class III malocclusion, retrusive maxilla, and protrusive mandible before treatment.
Intraoral examination found a narrow upper arch and a slightly retroclined upper left first molar. The lower arch was ovoid-shaped. Agenesis of all four permanent second premolars was noted, with retained deciduous second premolars. Periodontal defects at the level of the upper and lower incisors, hypoplastic upper lateral incisors, and triangular tooth shapes were also observed. The lower midline was shifted 2mm to the left, and the upper midline was shifted 1.5mm to the right. The molar relationship was Class III. No signs or symptoms of TMD were present.
Cephalometric analysis confirmed a skeletal Class III malocclusion (ANB = −2.6°) with a retrusive maxilla (SNA = 79°), a protrusive mandible (81°), and a hyperdivergent facial type (facial axis = 85°). The upper incisors were slightly retroclined (U1-OP = 62°); the lower incisors were retroclined (L1-OP = 80.5°). An overjet of −1.4mm and an overbite of −.2mm were measured. Projections to the TVL were normal except for soft-tissue pogonion (3.5mm), which was protrusive.
After considering the advantages and disadvantages of conventional surgical-orthodontic treatment and the “surgery first” approach, the patient elected “surgery first” treatment. The surgery would include a Le Fort I osteotomy for a 4.8mm advancement, 1.5mm anterior impaction, 3.5mm posterior impaction, 1.5mm left rotation, and 3mm transverse expansion of the maxilla. A BSSO would be performed to achieve a 2.6mm pogonion setback, 5mm elevation, and midline correction of the mandible.
Orthodontic treatment objectives were to normalize the overjet and overbite, align and procline the upper incisors, and achieve a Class I canine relationship and a Class II molar relationship (because of the missing upper second premolars). We also planned to align the lower incisors and perform interproximal reduction (IPR) of .3mm at each contact to avoid excessive proclination and to reduce the excessive Bolton Index.
As in Case 1, two visual treatment simulations were drawn using Dolphin software (Fig. 13). Dental casts were mounted on a SAM 2 articulator, and model surgery was performed (Fig. 14). Analysis of the model surgery indicated occlusal instability in the transitional malocclusion,21 due to interferences between the right canines and left molars. The occlusal interference on the right side was created by a 45° rotation of the upper canine; on the left side, the interference was caused by retroclination of the upper first molar.
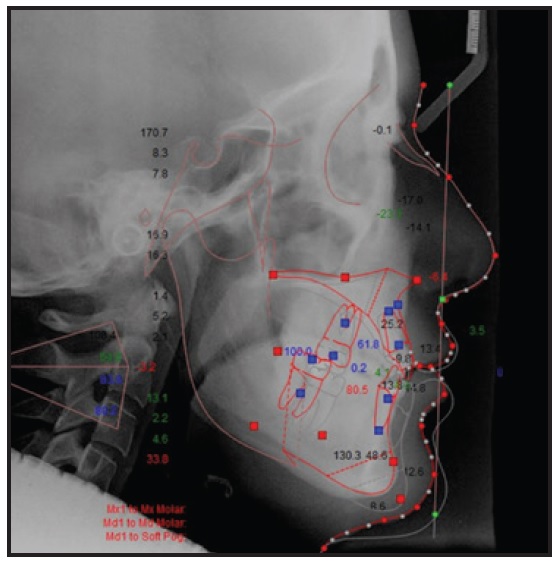
Fig. 13 Case 2. 2D visual treatment simulation for “surgery first” approach.
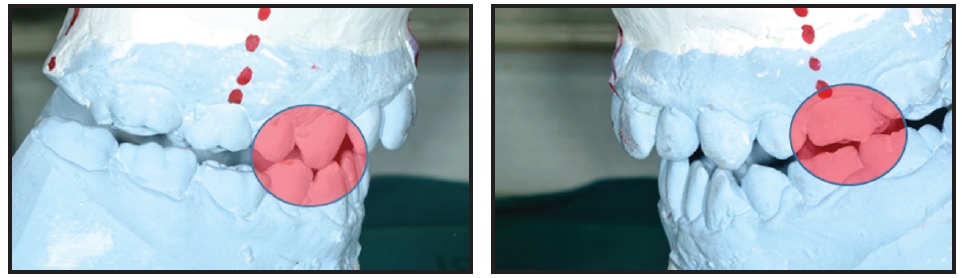
Fig. 14 Case 2. Model surgery showing evidence of occlusal instability (red circles) in transitional malocclusion.
The transverse expansion of the maxilla from the median osteotomy would require about 40 days of postsurgical stabilization with an occlusal splint. We decided to utilize segmental mechanics to move the upper right canine and left first molar into proper positions during the early postoperative stage, thus eliminating the occlusal interferences while the patient wore the final splint. The prescription for the upper arch therefore involved 1.5mm expansion of the left molar and 15% rotation of the right canine.
About three weeks before surgery, SmartClip§§§ .018" MBT-prescription appliances were bonded in both arches, and an intraoral TRIOS scan was taken. The 3D files of the bracketed arches were combined with the patient’s CBCT images using SureSmile** software. After the planned surgical movements were reproduced on the virtual 3D model (Fig. 15), a virtual orthodontic setup was performed. The prescription of five robotized custom arches began with .017" × .025" copper nickel titanium archwires to be placed the day before surgery; these wires would be passive on all teeth except the upper right canine and left first molar (Fig. 16).
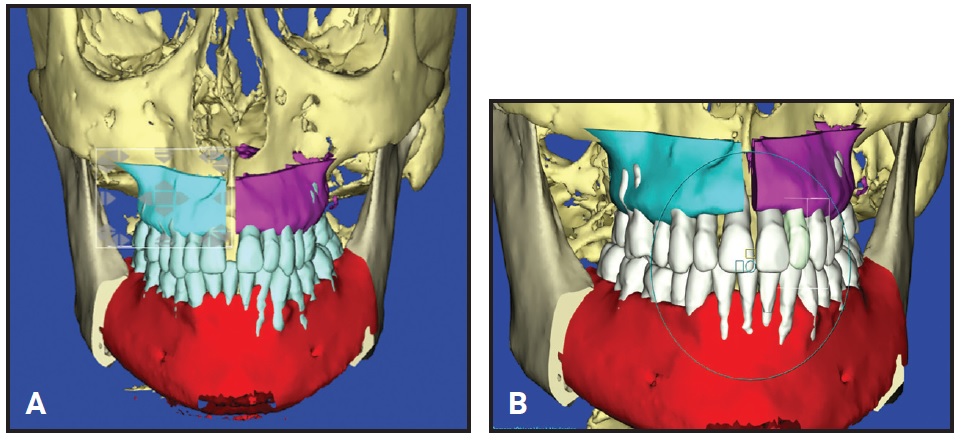
Fig. 15 Case 2. A. 3D plan of skeletal surgical movements and postsurgical occlusion. B. 3D plan of final occlusion following orthodontic treatment.
The CBCT images were then processed using ProPlan CMF software, as in Case 1. Referring to the 2D visual simulations, the postoperative occlusion was visualized, providing virtual images of the intermediate and final splints.
Using the 3D SureSmile software, the upper jaw movements were first carried out, working in all six degrees of freedom (Fig. 17).
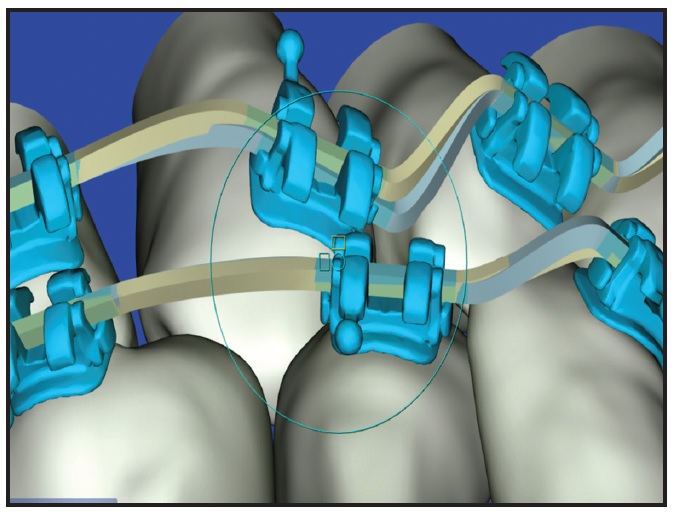
Fig. 16 Case 2. .017" × .025" copper nickel titanium customized SureSmile archwire, passive on all teeth except upper right canine and left first molar, to be placed one day before surgery.
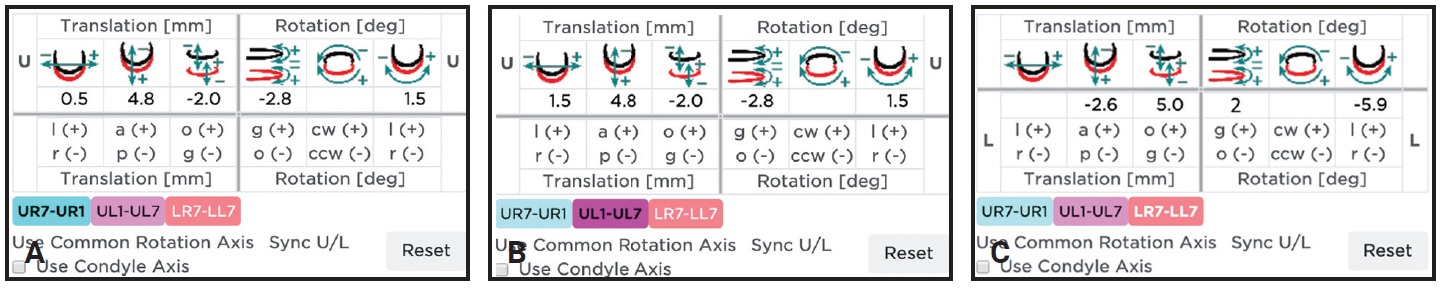
Fig. 17 Case 2. Six degrees of freedom (translation vector and rotation matrix). A. Osteotomized right hemimaxilla. B. Osteotomized left hemimaxilla. C. Osteotomized mandibular segments.
Once the mandible was repositioned, the required surgical expansion of the maxilla was added to ensure a stable occlusion. This position was then used to obtain the STL file for the virtual final splint (Fig. 18).
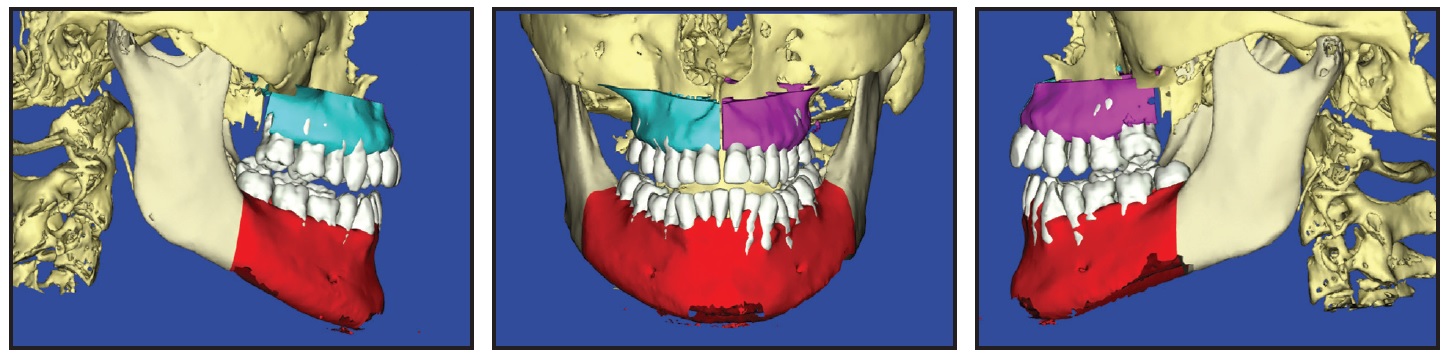
Fig. 18 Case 2. Planned postsurgical occlusion used to obtain STL file of virtual final splint.
Planning of the final splint in this case showed premature contacts of the upper right canine and left first molar, requiring an occlusal correction by means of a 2° rotation of the jaw on its hinge axis. Therefore, the planned postsurgical occlusion appeared to be Class II with an increased overjet. Once the interference of the upper right canine and left first molar were removed during the postsurgical stage, the mandible would rotate counterclockwise, correcting the apparent Class II relationship.
All movements relative to the lower jaw were eliminated to obtain the STL file for the intermediate splint (Fig. 19).
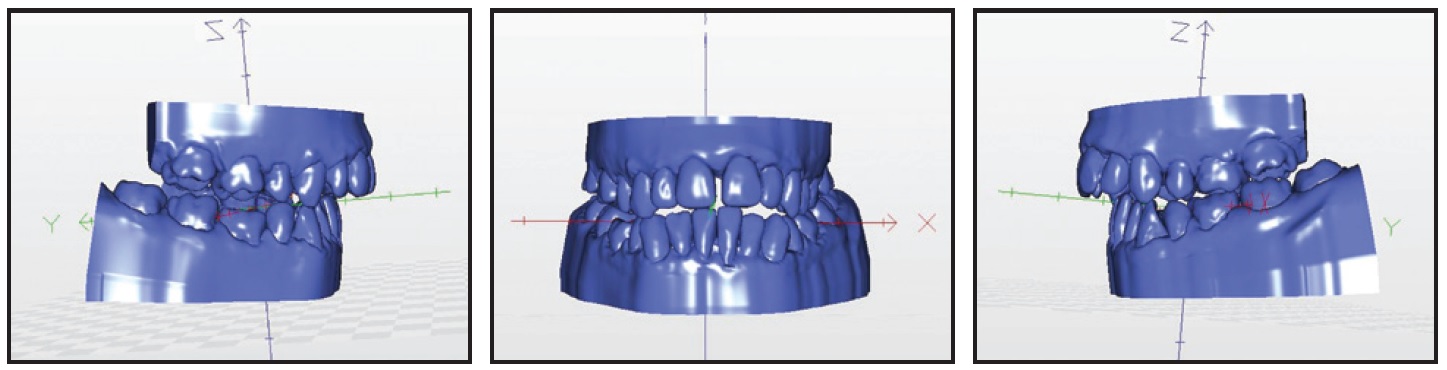
Fig. 19 Case 2. Surgical movements of mandible eliminated to obtain STL file of intermediate splint.
The STL files were sent to the technician, who processed the images using Exocad software, as in Case 1 (Fig. 20).
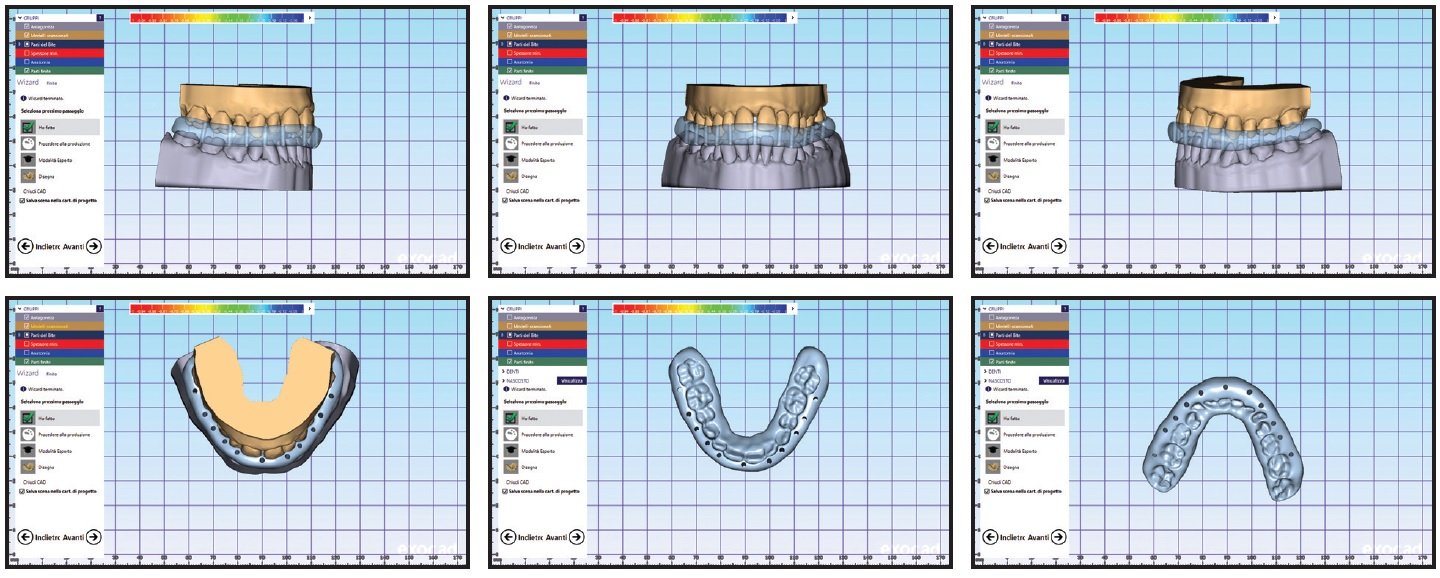
Fig. 20 Case 2. Design of intermediate splint using Exocad‡‡‡ software.
The data were transferred to the DWS 020D prototyping machine, and the two surgical resin splints were printed. The final splint was cut away in the areas of the upper right canine and left first molar to allow the initial movements programmed into the customized arches (Fig. 21).
During the postsurgical period, the anticipated occlusal interferences were eliminated using heavy .017" × .025" copper nickel titanium wires, while the patient wore the final splint (Fig. 22). Forty days after surgery, the occlusion was stable enough to proceed, and the splint was discontinued.

Fig. 21 Case 2. Dynamic final splint cut away in areas of upper right canine and left first molar to allow planned tooth movements.

Fig. 22 Case 2. Postsurgical occlusion with final splint and customized .017" × .025" copper nickel titanium archwires for elimination of occlusal interferences from upper right canine and left first molar.
The programmed SureSmile sequence of archwires continued with .016", .016" × .016", and .016" × .022" copper nickel titanium and .017" × .025" stainless steel for alignment. Triangle elastics (³⁄16", 3.5oz) were worn between the upper and lower canines and lower first premolars to maintain the correct occlusion, and vertical elastics were worn for about two months before debonding to improve intercuspation. Thermoformed retainers were delivered for both arches.
Total treatment time was 15 months (Fig. 23). All treatment objectives were achieved, including an optimal occlusion with good intercuspation, normal overjet and overbite, and Class I canine and Class II molar relationships. Facial esthetics showed a marked improvement resulting from the reduced vertical dimension, the sagittal increase in the middle facial third, and the setback of pogonion with its “anti-aging” effect. This result was enhanced by the correction of maxillary hypoplasia, with consequent esthetic improvement of the nasolabial folds and labial commissures. The lip line was refined, and the gummy smile at the premolars was eliminated. Cephalometric tracings confirmed the skeletal and occlusal improvements.
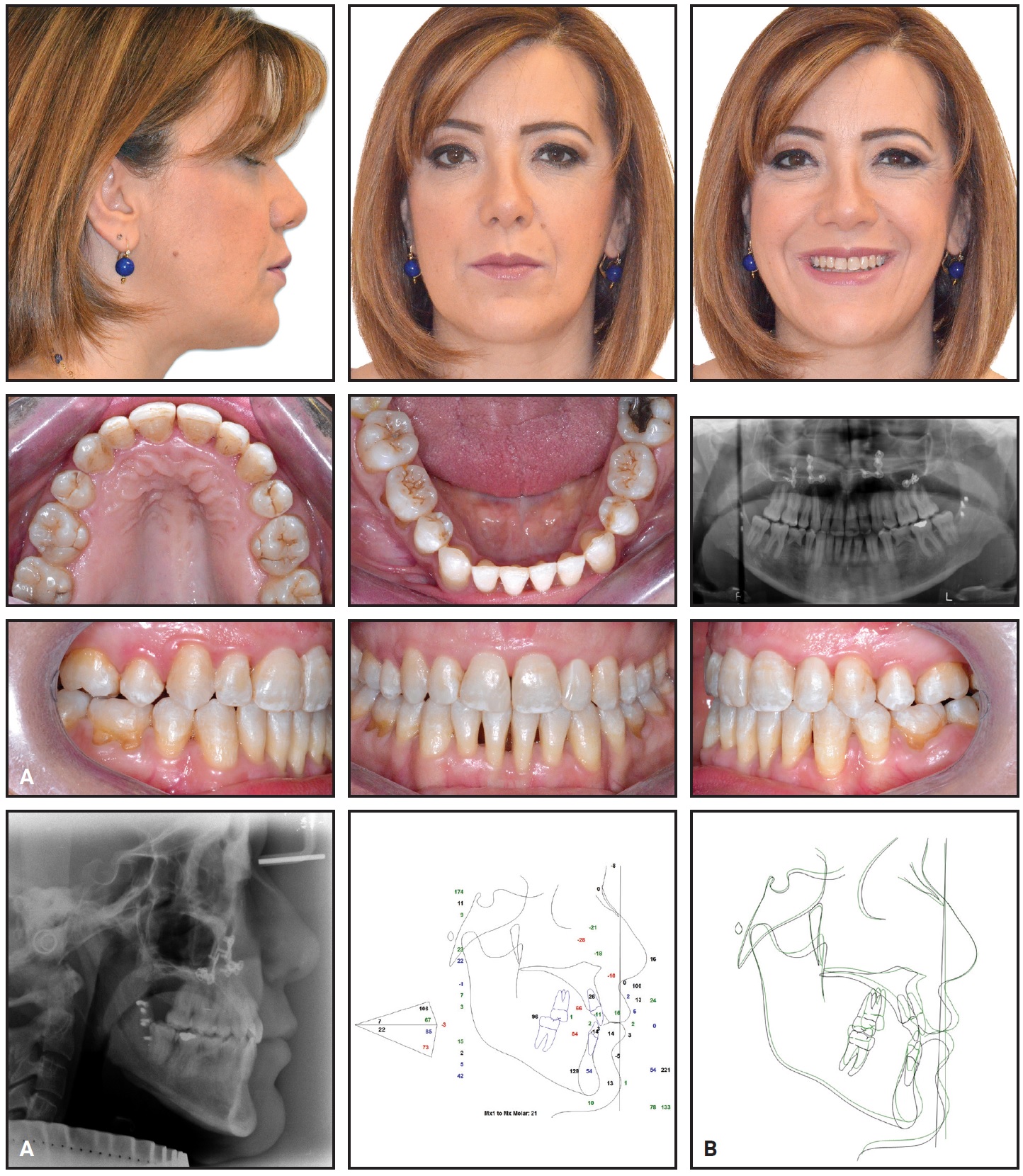
Fig. 23 Case 2. A. Patient after 15 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
The level of the papillae was preserved, without loss of attachment or bone support. Although periodontal problems were noted before treatment, the impression of dark triangles in the lower arch was concealed by the crowding and the retroclined lower incisors. Dark triangles appeared after treatment when the incisors were proclined and aligned, despite the planned IPR in this region. Periodontal therapy was performed during orthodontic treatment to mitigate the patient’s existing conditions.
Root resorption of the second permanent molars, as seen in this patient’s post-treatment radiographs, is common in orthodontic cases. The resorption of the deciduous second premolars was physiological, caused by the application of orthodontic brackets. The patient was advised that those teeth would probably need to be replaced by implants at some point.
Discussion
These two patients, whose surgery was performed by Dr. Pelo, demonstrate how occlusal splints can play a crucial therapeutic role, allowing us to solve problems that many authors would exclude from a “surgery first” approach.
Case 1 exhibited severe overcrowding that required an extraction and relative space closure without loss of anchorage. In Case 2, occlusal instability caused by the premature contacts of two teeth was anticipated after surgery. Both cases required maxillary expansion. Some authors recommend a “surgery early” or “surgery late” approach for such patients, involving preliminary surgically assisted expansion.9,10,14,19 Others maintain that if the surgical maxillary expansion does not exceed 3-4mm, it can be performed with a median palatal osteotomy at the same time as the Le Fort I surgical procedure.13,20 In that scenario, the patient should wear a splint continuously for four to six weeks, until the skeletal segments have stabilized.13,20
In Case 1, we decided to distalize the permanent upper right canine (after extraction of the deciduous upper right canine) while the patient wore the occlusal splint. This approach offers many advantages, including:
- The splint maintains anchorage, so there is no loss of space during the distalization.
- The movement can be started immediately after surgery, taking advantage of the RAP.51-54
- With appropriate cutouts, the splint offers a programmed path for tooth movement.
- The traction can be programmed on the palatal side to avoid spontaneous rotation.
- The overall treatment time is reduced.
Case 2 presented a clear problem related to postsurgical occlusal instability. Various authors recommend at least three occlusal stops in the transitional malocclusion.14,16,18,20 Liao and Lo advised maintaining five or six occlusal contacts, not necessarily distributed among three sectors; they suggested that two sectors of contact—or even one if located in the anterior region—can provide enough stability.55 We agree with Liao and Lo: an ideal postoperative occlusion is characterized by five or six bilateral contacts that do not create an imbalance between the right and left sides. To be viable, the occlusal stops must avoid crossbites, edge-to-edge contact, and scissor or Brodie bite. They must be located bilaterally in the posterior regions, and they must occur simultaneously on the left and right sides.
In Case 2, the two contacts were distributed on both sides, but not symmetrically. The cusp-to-cusp contacts appeared inadequate to guarantee a stable position of the mandible. Therefore, the sources of occlusal instability were removed during the postsurgical phase while the patient wore the final splint. This segmental tooth movement was carried out with the aid of robotically manufactured custom archwires, using the SureSmile system. The ability to achieve individual tooth movements made it possible to transform a “surgery early” case into a “surgery first” case. Thus, the period of splint wear was not a static phase of treatment, but a dynamic phase.
The application of elastics and early orthodontic activation in the immediate postoperative period could allow removal of the final splint one or two days after surgery, according to some authors, even in the presence of deflecting precontacts. Thus, a source of patient discomfort is eliminated, and the therapeutic potential of the RAP is fully exploited. The elastics also perform the function of guiding the required mandibular positioning after surgery.
In our analysis of the literature, six articles reported the use of CAD/CAM splint manufacturing.13,19,34,37,39,40 Gateno and colleagues found a high degree of accuracy with CAD/CAM-generated splints as compared with conventional splints.56 A pilot study of CAD/CAM-generated surgical splints by Xia and colleagues indicated that the surgical results did not differ significantly from the planned outcomes, either statistically or clinically.57 These authors concluded that the computer-generated splints had a high degree of accuracy, with a fit similar to that of conventional splints.
Conclusion
Orthognathic splints are useful stabilization systems that can provide certainty for the surgeon. To date, however, few reports on the use of splints in the “surgery first” approach have been published. As our literature review demonstrated, there is no uniformity in the recommended duration of final splint wear based on the type of surgery performed.
This overview has described four types of occlusal splints for use with the “surgery first” approach:
- A repositioning splint can be used in a TMD patient before orthognathic surgery. During surgery, it maintains the asymptomatic condylar position.
- An intermediate splint should always be used for bimaxillary surgery. It can be avoided in “maxilla first” procedures when only simple movements are planned, but is mandatory in “mandible first” procedures.
- A final splint should always be used during surgery. In cases requiring segmental osteotomies or transverse maxillary expansion, or in patients with occlusal instability due to deflecting precontacts, the final splint should be worn for three weeks after surgery.
- A dynamic splint can sometimes turn a “surgery early” case into a “surgery first” case. The dynamic splint can also be used as an occlusal build-up to avoid interferences after surgery. Further investigation is required to verify its clinical efficacy.
FOOTNOTES
- *Trademark of 3dMD, Atlanta, GA; www.3dmd.com.
- **Registered trademark of Denstply Sirona, York, PA; www.dentsplysirona.com.
- ***Dolphin Imaging and Management Solutions, Chatsworth, CA; www.dolphinimaging.com.
- †Registered trademark of SAM Präzisionstechnik GmbH, Gauting, Germany; www.sam-dental.de.
- ‡Registered trademark of Materialise, Plymouth, MI; www.materialise.com.
- ††i-CAT FLX V17, Kavo Dental, Brea, CA; www.kavo.com/en-us.
- ‡‡Registered trademark of 3Shape, Copenhagen, Denmark; www.3shape.com.
- †††Trademark of OraMetrix, Inc., Richardson, TX; www.elemetrix.com.
- ‡‡‡Denseo GmbH, Aschaffenburg, Germany; www.denseo.de.
- §DWS, Thiene, Italy; www.dwssystems.com.
- §§Registered trademark of Formlabs, Inc., Somerville, MA; www.formlabs.com.
- §§§Trademark of 3M, Monrovia, CA; www.3M.com.
- ****Registered trademark of Rocky Mountain Orthodontics, Denver, CO; www.rmortho.com.
REFERENCES
- 1. Proffit, W.R. and Fields, H.W. Jr.: Combined surgical and orthodontic treatment, in Contemporary Orthodontics, 3rd ed., Mosby, St. Louis, 1999, pp. 674-709.
- 2. Bell, W.H. and Creekmore, T.D.: Surgical orthodontic correction of mandibular prognathism, Am. J. Orthod. 63:256-270, 1973.
- 3. Worms, F.W.; Isaacson, R.J.; and Speidel, T.M.: Surgical orthodontic treatment planning: Profile analysis and mandibular surgery, Angle Orthod. 46:1-25, 1976.
- 4. Hernández-Alfaro, F. and Guijarro-Martínez, R.: On a definition of the appropriate timing for surgical intervention in orthognathic surgery, Int. J. Oral Maxillofac. Surg. 43:846-855, 2014.
- 5. Proffit, W.R.; Fields, H.W. Jr.; and Sarver, D.M.: Contemporary Orthodontics, 4th ed., Mosby, St. Louis, 2007, pp. 710-713.
- 6. Grubb, J. and Evans, C.: Orthodontic management of dentofacial skeletal deformities, Clin. Plast. Surg. 34:403-415, 2007.
- 7. Epker, B.N. and Fish, L.: Surgical-orthodontic correction of open-bite deformity, Am. J. Orthod. 71:278-299, 1977.
- 8. Peiró-Guijarro, M.A.; Guijarro-Martínez, R.; and Hernández-Alfaro, F.: Surgery first in orthognathic surgery: A systematic review of the literature, Am. J. Orthod. 149:448-462, 2016.
- 9. Huang, C.S.; Hsu, S.S.; and Chen, Y.R.: Systematic review of the surgery-first approach in orthognathic surgery, Biomed. J. 37:184-190, 2014.
- 10. Jeong, W.S.; Choi, J.W.; Kim, D.Y.; Lee, J.Y.; and Kwon, S.M.; Can a surgery-first orthognathic approach reduce the total treatment time? Int. J. Oral Maxillofac. Surg. 46:473-482, 2017.
- 11. Luther, F.; Morris, D.O.; and Hart, C.: Orthodontic preparation for orthognathic surgery: How long does it take and why? A retrospective study, Br. J. Oral Maxillofac. Surg. 41:401-406, 2003.
- 12. Liao, Y.F.; Chiu, Y.T.; Huang, C.S.; Ko, E.W.; and Chen, Y.R.: Presurgical orthodontics versus no presurgical orthodontics: Treatment outcome of surgical-orthodontic correction for skeletal class III open bite, Plast. Reconstr. Surg. 126:2074-2083, 2010.
- 13. Hernandez-Alfaro, F.; Guijarro-Martınez, R.; and Peiró-Guijarro, M.A.: Surgery first in orthognathic surgery: What have we learned? A comprehensive workflow based on 45 consecutive cases, J. Oral Maxillofac. Surg. 72:376-390, 2014.
- 14. Kim, C.S.; Lee, S.C.; Kyung, H.M.; Park, H.S.; and Kwon, T.G.: Stability of mandibular setback surgery with and without presurgical orthodontics, J. Oral Maxillofac. Surg. 72:779-787, 2014.
- 15. Nagasaka, H.; Sugawara, J.; Kawamura, H.; and Nanda, R.: “Surgery first” skeletal Class III correction using the Skeletal Anchorage System, J. Clin. Orthod. 43:97-105, 2009.
- 16. Kim, J.H.; Mahdavie, N.N.; and Evans, C.A.: Guidelines for “surgery first” orthodontic treatment, in Orthodontics—Basic Aspects and Clinical Considerations, ed. F. Bourzgui, InTechOpen, London, 2012.
- 17. Pelo, S.; Gasparini, G.; Garagiola, U.; Cordaro, M.; Di Nardo, F.; Staderini, E.; Patini, R.; de Angelis, P.; D’Amato, G.; Saponaro, G.; and Moro, A.: Surgery-first orthognathic approach vs traditional orthognathic approach: Oral health-related quality of life assessed with 2 questionnaires, Am. J. Orthod. 152:250-254, 2017.
- 18. Huang, S.; Chen, W.; Ni, Z.; and Zhou, Y.: The changes of oral health-related quality of life and satisfaction after surgery-first orthognathic approach: A longitudinal prospective study, Head Face Med. 12:2, 2016.
- 19. Hernández-Alfaro, F.; Guijarro-Martínez, R.; Molina-Coral, A.; and Badía-Escriche, C.: “Surgery first” in bimaxillary orthognathic surgery, J. Oral Maxillofac. Surg. 69:e201-207, 2011.
- 20. Baek, S.H.; Ahn, H.W.; Kwon, Y.H.; and Choi, J.Y.: Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: Evaluation of surgical movement and postoperative orthodontic treatment, J. Craniofac. Surg. 21:332-338, 2010.
- 21. Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; and Chen, Y.R.: Surgery-first accelerated orthognathic surgery: Orthodontic guidelines and setup for model surgery, J. Oral Maxillofac. Surg. 69:771-780, 2011.
- 22. Wei, H.; Liu, Z.; Zang, J.; and Wang, X.: Surgery-first/early- orthognathic approach may yield poorer postoperative stability than conventional orthodontics-first approach: A systematic review and meta-analysis, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 126:107-116, 2018.
- 23. Soverina, D.; Gasparini, G.; Pelo, S.; Doneddu, P.; Todaro, M.; Boniello, R.; Azzuni, C.; Grippaudo, C.; Saponaro, G.; D’Amato, G.; Garagiola, U.; and Moro, A.: Skeletal stability in orthognathic surgery with the surgery first approach: A systematic review, Int. J. Oral Maxillofac. Surg. 48:930-940, 2019.
- 24. Uribe, F.; Agarwal, S.; Shafer, D.; and Nanda, R.: Increasing orthodontic and orthognathic surgery treatment efficiency with a modified surgery-first approach, Am. J. Orthod. 148:838-848, 2015.
- 25. Akamatsu, T.; Hanai, U.; Miyasaka, M.; Muramatsu, H.; and Yamamoto, S.: Comparison of mandibular stability after SSRO with surgery-first approach versus conventional ortho-first approach, J. Plast. Surg. Hand Surg. 50:50-55, 2016.
- 26. Aymach, Z.; Sugawara, J.; Goto, S.; Nagasaka, H.; and Nanda, R.: Nonextraction “surgery first” treatment of a skeletal Class III patient with severe maxillary crowding, J. Clin. Orthod. 47:297-304, 2013.
- 27. Kim, J.W.; Lee, N.K.; Yun, P.Y.; Moon, S.W.; and Kim, Y.K.: Postsurgical stability after mandibular setback surgery with minimal orthodontic preparation following upper premolar extraction, J. Oral Maxillofac. Surg. 71:1968.e1-1968.e11, 2013.
- 28. Kochar, G.D.; Chakranarayan, A.; Londhe, S.M.; Varghese, B.; Jayan, B.; Chopra, S.S.; Mitra, R.; and Verma, M.: Management of skeletal Class II malocclusion by surgery-first approach, J. Craniofac. Surg. 28:e40-e43, 2017
- 29. Sugawara, J.; Aymach, Z.; Nagasaka, D.H.; Kawamura, H.; and Nanda, R.: “Surgery first” orthognathics to correct a skeletal Class II malocclusion with an impinging bite, J. Clin. Orthod. 44:429-438, 2010.
- 30. Villegas, C.; Uribe, F.; Sugawara, J.; and Nanda, R.: Expedited correction of significant dentofacial asymmetry using a “surgery first” approach, J. Clin. Orthod. 44:97-103, 2010.
- 31. Choi, S.H.; Hwang, C.J.; Baik, H.S.; Jung, Y.S.; and Lee, K.J.: Stability of pre-orthodontic orthognathic surgery using intraoral vertical ramus osteotomy versus conventional treatment, J. Oral Maxillofac. Surg. 74:610-619, 2016.
- 32. Choi, S.H.; Yoo, H.J.; Lee, J.Y.; Jung, Y.S.; Choi, J.W.; and Lee, K.J.: Stability of pre-orthodontic orthognathic surgery depending on mandibular surgical techniques: SSRO vs IVRO, J. Craniomaxillofac. Surg. 44:1209-1215, 2016.
- 33. Hsu, S.S.; Singhal, D.; Xia, J.J.; Gateno, J.; Lin, C.; Huang, C.; Lo, L.; Ko, E.W.; and Chen, Y.: Planning the surgery-first approach in surgical-orthodontic treatment with a computer aided surgical simulation (CASS) planning protocol, J. Taiwan Assoc. Orthod. 24:24-37, 2012.
- 34. Janakiraman, N.; Feinberg, M.; Vishwanath, M.; Nalaka Jayaratne, Y.S.; Steinbacher, D.M.; Nanda, R.; and Uribe, F.: Integration of 3-dimensional surgical and orthodontic technologies with orthognathic “surgery-first” approach in the management of unilateral condylar hyperplasia, Am. J. Orthod. 148:1054-1066, 2015.
- 35. Kim, J.Y.; Jung, H.D.; Kim, S.Y.; Park, H.S.; and Jung, Y.S.: Postoperative stability for surgery-first approach using intraoral vertical ramus osteotomy: 12 month follow-up, Br. J. Oral Maxillofac. Surg. 52:539-544, 2014.
- 36. Park, K.R.; Kim, S.Y.: Park, H.S.; and Jung, Y.S.: Surgery-first approach on patients with temporomandibular joint disease by intraoral vertical ramus osteotomy, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 116:e429-436, 2013.
- 37. Uribe, F.; Janakiraman, N.; Shafer, D.; and Nanda, R.: Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: Surgery first approach, Am. J. Orthod. 144:748-758, 2013.
- 38. Uribe, F.; Adabi, S.; Janakiraman, N.; Allareddy, V.; Steinbacher, D.; Shafer, D.; and Villegas, C.: Treatment duration and factors associated with the surgery-first approach: A two-center study, Prog. Orthod. 16:29, 2015.
- 39. Pelo, S.; Saponaro, G.; De Angelis, P.; Gasparini, G.; Garagiola, U.; and Moro, A.: Effect of surgery first orthognathic approach on the temporomandibular joint, J. Craniofac. Surg. 29:671-675, 2018.
- 40. Hernández-Alfaro, F.; Nieto, MJ.; Ruiz-Magaz, V.; Valls-Ontañón, A.; Méndez-Manjón, I.; and Guijarro-Martínez, R.: Inferior subapical osteotomy for dentoalveolar decompensation of class III malocclusion in surgery-first and surgery-early orthognathic treatment, Int. J. Oral Maxillofac. Surg. 46:80-85, 2017.
- 41. Choi, J.W.; Lee, J.Y.; Yang, S.J.; and Koh, K.S.: The reliability of a surgery-first orthognathic approach without presurgical orthodontic treatment for skeletal Class III dentofacial deformity, Ann. Plast. Surg. 94:333-341, 2015.
- 42. Rufenacht, C.R.: Fundamentals of Esthetics, Quintessence Publishing Co., Hanover Park, IL, 1990.
- 43. Arnett, G.W. and Gunson, J.G.: Facial planning for orthodontists and oral surgeons, Am. J. Orthod. 126:290-295, 2004.
- 44. Arnett, W.G. and Bergman, R.T.: Facial keys to orthodontic diagnosis and treatment planning: Part I, Am. J. Orthod. 103:299-312, 1993.
- 45. Arnett, W.G. and Bergman, R.T.: Facial keys to orthodontic diagnosis and treatment planning: Part II, Am. J. Orthod. 103:395-411, 1993.
- 46. Arnett, G.W.; Jelic, J.S.; Kim, J.; Cummings, D.R.; Beress, A.; Worley C.M. Jr.; Chung, B.; and Bergman, R.: Soft tissues cephalometric analysis: Diagnosis and treatment planning of dentofacial deformity, Am. J. Orthod. 116: 239-253, 1999.
- 47. Sarver, D.M. and Ackerman, M.B.: Dynamic smile visualization and quantification, Part 1: Evolution of the concept and dynamic records of the smile capture, Am. J. Orthod. 124:4-12, 2003.
- 48. Sarver, D.M. and Ackerman, M.B.: Dynamic smile visualization and quantification, Part 2: Smile analysis and treatment strategies, Am. J. Orthod. 124:116-127, 2003.
- 49. Ackerman, J.L.; Ackerman, M.B.; Brensinger, C.M.; and Landis, J.R.: A morphometric analysis of the posed smile, Clin. Orthod. Res. 1:2-11, 1998.
- 50. Ackerman, M.B.: Digital video as a clinical tool in orthodontics: Dynamic smile design in diagnosis and treatment planning, in 29th Annual Moyers Symposium, vol. 40, University of Michigan, Ann Arbor, MI, 2003.
- 51. Frost, H.M.: The biology of fracture healing: An overview for clinicians, Part I, Clin. Orthop. Relat. Res. 248:283-293, 1989.
- 52. Frost, H.M.: The biology of fracture healing: An overview for clinicians, Part II, Clin. Orthop. Relat. Res. 248:294-309, 1989.
- 53. Wilcko, M.T.; Wilcko, W.M.; Pulver, J.J.; Bissada, N.F.; and Bouquot, J.E.: Accelerated osteogenic orthodontics technique: A 1-stage surgically facilitated rapid orthodontic technique with alveolar augmentation, J. Oral Maxillofac. Surg. 67:2149-2159, 2009.
- 54. Liou, E.J.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; and Chen, Y.R.: Surgery-first accelerated orthognathic surgery: Postoperative rapid orthodontic tooth movement, J. Oral Maxillofac. Surg. 69:781-785, 2011.
- 55. Liao, Y.F. and Lo, S.H.: Surgical occlusion setup in correction of skeletal Class III deformity using surgery-first approach: Guidelines, characteristics and accuracy, Sci. Rep. 8:11673, 2018.
- 56. Gateno, J.; Xia, J.; Teichgraeber, J.F.; Rosen, A.; Hultgren, B.; and Vadnais, T.: The precision of computer-generated surgical splints, J. Oral Maxillofac. Surg. 61:814-817, 2003.
- 57. Xia, J.J.; Gateno, J.; Teichgraeber, J.F.; Christensen, A.M.; Lasky, R.E.; Lemoine, J.J.; and Liebschner, M.A.K.: Accuracy of the computer aided surgical simulation (CASS) system in the treatment of patients with complex craniomaxillofacial deformity: A pilot study, J. Oral Maxillofac. Surg. 65:248-254, 2007.




COMMENTS
.