CASE REPORT
Treatment in 41 Days Using a Customized Passive Self-Ligation System and the "Surgery First" Approach
The orthognathic “surgery first” approach introduced by Nagasaka and colleagues1 to correct skeletal dysplasias without presurgical orthodontic preparation has gained popularity in recent years. This method offers several advantages: the profile shows an immediate improvement without the need for decompensation, the functional orthognathic balance is restored early in treatment, and the regional acceleratory phenomenon (RAP) can potentially shorten treatment.1-7
Recent developments in three-dimensional technology have provided new options for more precise planning of interocclusal relationships and jaw movements. Cone-beam computed tomography can now be used to plan orthognathic surgery, and surgical splints can be fabricated with computer-aided design/computer-aided manufacturing (CAD/CAM) programs.8 Such a protocol eliminates dental impressions, simplifies the laboratory process, and reduces patient exposure to ionizing radiation.9-11 Custom digital design and manufacturing of bracket systems can also improve treatment efficiency.7,8,12
This report describes the integration of the Insignia* custom self-ligating bracket system with 3D virtual surgical planning and digitally manufactured surgical splints in a “surgery first” approach that can dramatically reduce treatment time.
Diagnosis and Treatment Plan
A 21-year-old male requested an enhanced chin projection to improve his occlusal relationship and facial esthetics (Fig. 1A and 1B).
Similar articles from the archive:
- The "Surgery First" Approach with Passive Self-Ligating Brackets for Expedited Treatment of Skeletal Class III Malocclusion June 2015
- THE CUTTING EDGE Treatment of Severe Facial Asymmetry Using Virtual Three-Dimensional Planning and a "Surgery First" Protocol August 2013
- CASE REPORT Nonextraction "Surgery First" Treatment of a Skeletal Class III Patient with Severe Maxillary Crowding May 2013
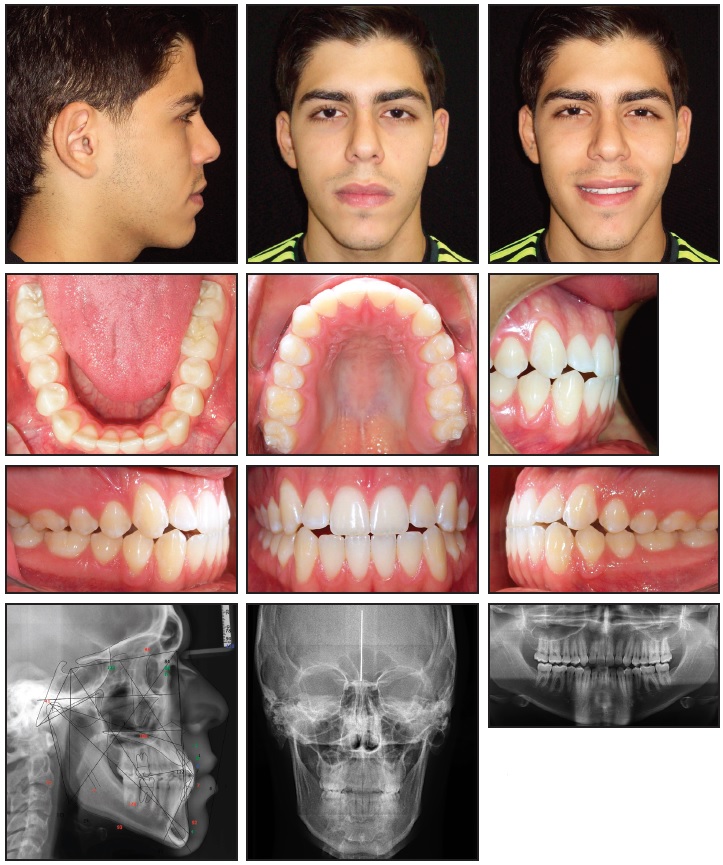
Fig. 1 21-year-old male patient with mild Class III malocclusion, minor crowding, long lower face, and mandibular macrognathism before treatment (continued on next image).
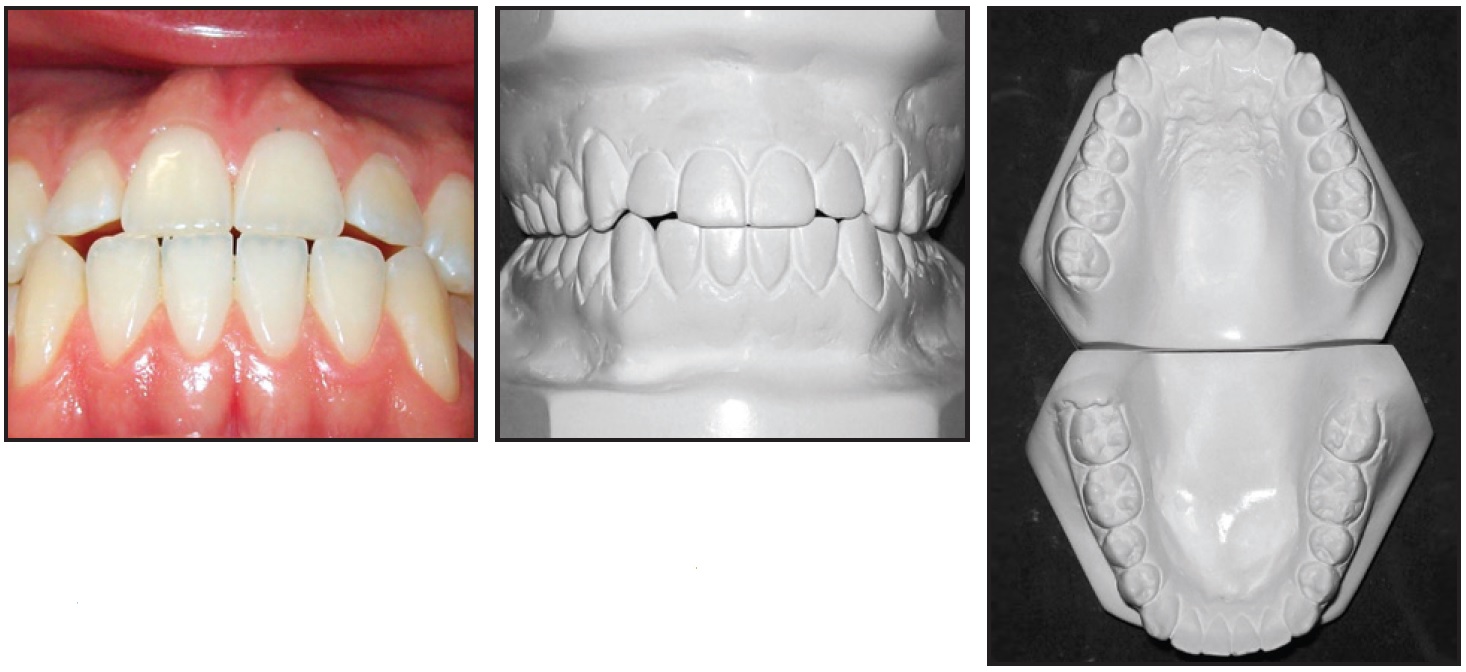
Fig. 1 (cont.) 21-year-old male patient with mild Class III malocclusion, minor crowding, long lower face, and mandibular macrognathism before treatment.
The patient had a straight profile with excessive lower facial height, a dental Class III malocclusion, minor crowding in both arches, edge-to-edge incisor relationships, and slightly proclined upper and lower incisors. Radiographic analysis indicated a mild skeletal Class III pattern and mandibular macrognathism. The panoramic radiograph showed adequate root integrity and anatomical symmetry.
Three treatment alternatives were presented. Orthodontic camouflage, suitable for patients with mild to moderate skeletal Class III malocclusions and acceptable facial esthetics, could improve the occlusal function in this case.13,14 Orthodontic treatment prior to maxillary advancement surgery and a vertical reduction mentoplasty would offer the advantage of moving the teeth into their ideal positions respective to the bones before surgery, but would also take more time.15,16 The third option was to use a “surgery first” procedure without presurgical orthodontics.
Because of the reported advantages of the “surgery first” approach and the patient’s expectations of immediate facial esthetic improvement and optimal functional occlusal results, we chose this alternative.1-7 It would avoid any worsening of facial esthetics from presurgical decompensation, and it would shorten treatment because of the activation of the RAP by surgery.
Treatment Progress
The surgeon decided to perform the correction in the maxilla because the midfacial soft-tissue hypoplasia, combined with the adequate distance between the throat and menton, contraindicated a mandibular setback. A 4mm maxillary advancement was planned by simulating the osteotomies in 3D using ProPlan CMF** software (Fig. 2).
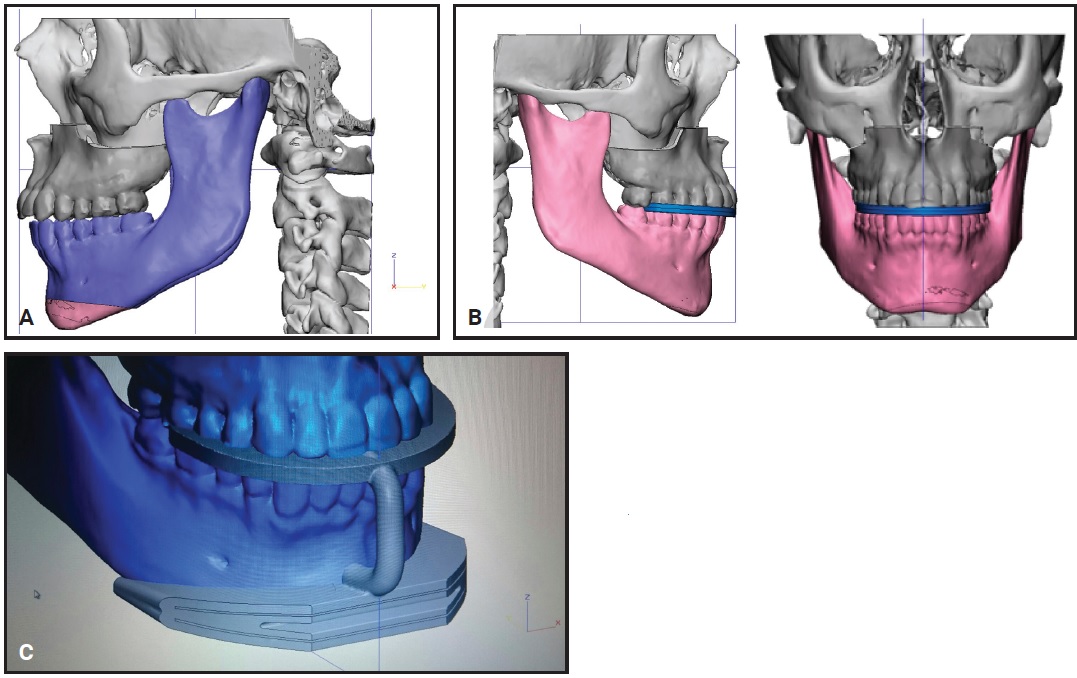
Fig. 2 A. Virtual surgical plan for maxillary advancement. B. Stereolithographic model of intermediate splint. C. Design of guide template for mentoplasty.
An intermediate splint and a guide template for the mentoplasty were designed digitally and fabricated on a Fortus 250mc*** printer. After polyvinyl siloxane impressions were taken and the photographic and radiographic records and preferences were loaded in the Approver Interface† software, the Insignia passive self-ligating brackets were designed (Fig. 3).
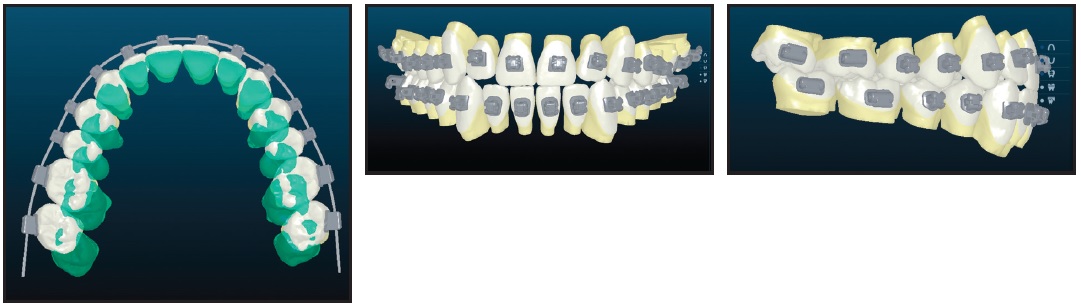
Fig. 3 Design of Insignia* custom brackets.
The brackets were placed one week before surgery without any archwires.2,4 To avoid interfering with the operating procedure or producing any tooth movement before the intermediate splint was placed during surgery, the initial .014" Copper NiTi‡ wires were placed in both arches immediately before the patient was intubated. Installation of the first superelastic wires in the operating room takes advantage of the RAP from the beginning of treatment and promotes gentle tooth movements rather than heavy occlusal contacts after surgery.
During the maxillary advancement, the maxilla was rigidly fixed in place with the intermediate splint (Fig. 4).
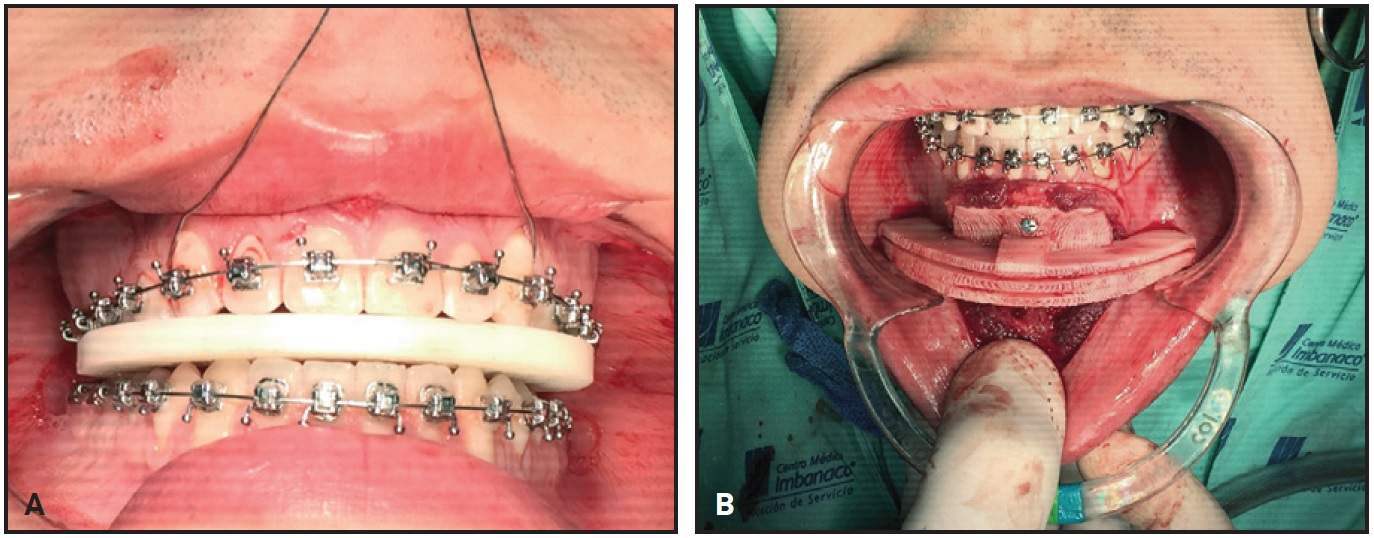
Fig. 4 A. Intermediate splint in position during maxillary advancement surgery. B. Digitally designed and fabricated template in position for mentoplasty.
A 5mm anterior vertical reduction mentoplasty was then performed using the surgical template. Instead of a final splint, the patient was stabilized with short intermaxillary elastics (³⁄16", 3.5oz) with Class III force vectors.
Because of the minor crowding and the RAP response, the archwires could be changed every 11 days: .014" × .025" Copper NiTi wires were placed 11 days after surgery, followed by .018" × .025" Copper NiTi and .019" × .025" TMA* finishing wires (Fig. 5).
Treatment Results
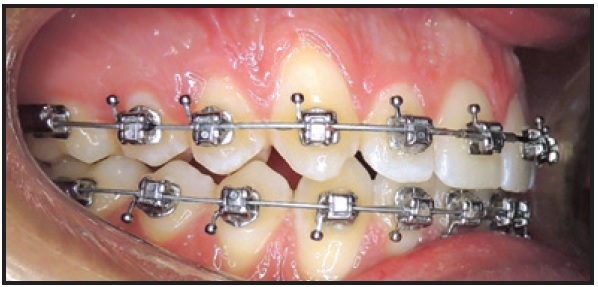
Fig. 5 Final .019" × .025" TMA* archwire in place.
The brackets were removed after only 41 days of orthodontic treatment, with a marked improvement in the vertical facial relationship and the occlusion (Fig. 6).
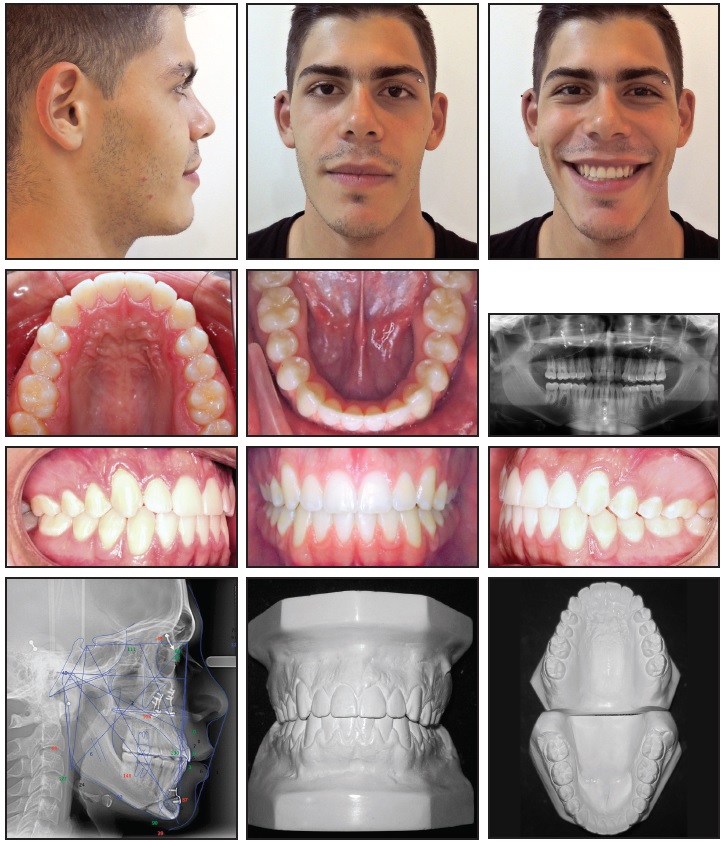
Fig. 6 Patient after 41 days of treatment.
Final photographs showed minor inflammation. Excellent stability was observed 24 months after treatment (Fig. 7A and 7B).
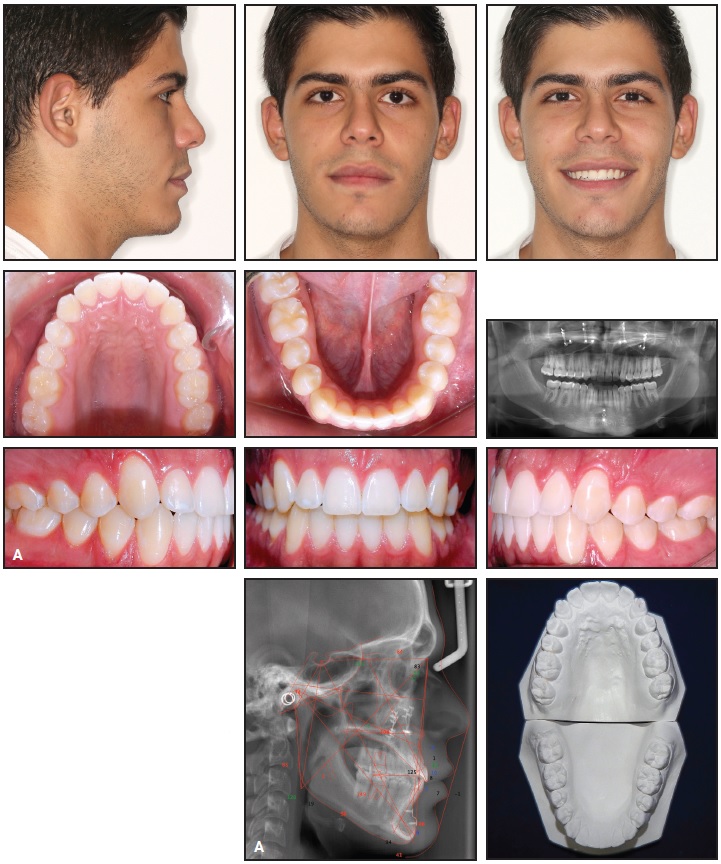
Fig. 7 A. Patient 24 months after treatment (continued on next image).
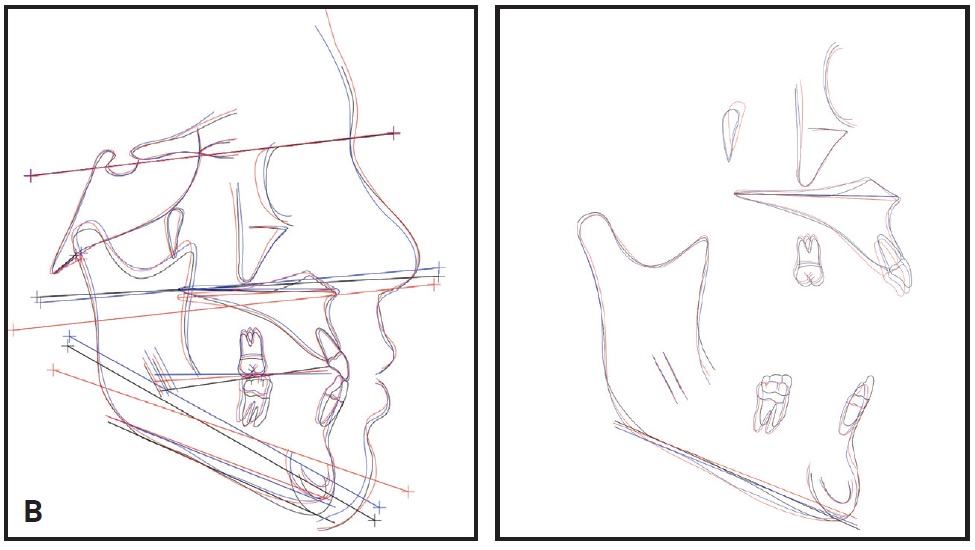
Fig. 7 (cont.) B. Superimposition of pretreatment (black), post-treatment (blue), and 24-month follow-up (red) cephalometric tracings.
Discussion
In a case of skeletal dysplasia, the “surgery-first” approach can improve treatment efficiency, providing greater patient and orthodontist satisfaction within a short period of time.3,4,6,17,18 In addition, “surgery first” treatment can now be planned with digital technology that allows the patient to see an immediate improvement in facial esthetics.
Uribe and colleagues reported a median treatment duration of 9.6 months with a “surgery first” approach.18 The shortest published treatment times for postsurgical orthodontics have been four months in a Class III patient with open bite and crowding19 and four and a half months in a patient with unilateral hyperplasia.20 Most authors have reported completion of treatment in six months to one year.1,2,4,20-24 To our knowledge, our patient’s total treatment time of 41 days is the shortest on record for a surgical-orthodontic case. These rapid results can be explained by a combination of digital diagnostic planning, customized appliances, and the RAP.
Advances in technology have led to the development of such systems as Insignia and SureSmile†† for designing customized brackets and wires.25 In the Insignia protocol, the occlusion and final alignment are created virtually with the interactive software, and the custom brackets and wires are made through reverse engineering with a CAD/CAM program. The brackets are then transferred to the patient for indirect bonding with conventional orthodontic adhesives.26 Reports have suggested that mean treatment times may be as much as eight months shorter with Insignia than with conventional fixed appliances.26-28
FOOTNOTES
- *Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- **Registered trademark of Materialise, Plymouth, MI; www.materialise.com.
- ***Trademark of Stratasys Ltd., Eden Prairie, MN; www.stratasys.com.
- †Ormco Corporation, Orange, CA; www.ormco.com.
- ‡Registered trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- ††Registered trademark of OraMetrix, Inc., Richardson, TX; www.suresmile.com.
REFERENCES
- 1. Nagasaka, H.; Sugawara, J.; Kawamura, H.; and Nanda, R.: “Surgery first” skeletal Class III correction using the Skeletal Anchorage System, J. Clin. Orthod. 43:97-105, 2009.
- 2. Villegas, C.; Uribe, F.; Sugawara, J.; and Nanda, R.: Expedited correction of significant dentofacial asymmetry using a “surgery first” approach, J. Clin. Orthod. 44:97-103, 2010.
- 3. Liou, E.J.W.; Chen, P.H.; Wang, Y.C.; Yu, C.C.; Huang, C.S.; and Chen, Y.R.: Surgery-first accelerated orthognathic surgery: Postoperative rapid orthodontic tooth movement, J. Oral Maxillofac. Surg. 69:781-785, 2011.
- 4. Aristizábal, J.F.; Martínez, R.; and Villegas, C.: The “surgery first” approach with passive self-ligating brackets for expedited treatment of skeletal Class III malocclusion, J. Clin. Orthod. 49:361-370, 2015.
- 5. Huang, C.S.; Hus, S.S.; and Chen, Y.R.: Systematic review of the surgery first approach in orthognathic surgery, Biomed. J. 37:184-190, 2014.
- 6. Peiró-Guijarro, M.A.; Guijarro-Martínez, R.; and Hernández-Alfaro, F.: Surgery first in orthognathic surgery: A systematic review of the literature, Am. J. Orthod. 149:448-462, 2016.
- 7. López, D.F.; Aristizábal, J.F.; and Martínez-Smit, R.: Condylectomy and “surgery first” approach: An expedited treatment for condylar hyperplasia in a patient with facial asymmetry, Dent. Press J. Orthod. 22:86-96, 2017.
- 8. Hernandez-Alfaro, F. and Guijarro-Martinez, R.: New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: An in vitro and in vivo study, Int. J. Oral Maxillofac. Surg. 42:1547-1556, 2013.
- 9. Hernandez-Alfaro, F.; Guijarro-Martınez, R.; and Peiro-Guijarro, M.A.: Surgery first in orthognathic surgery: What have we learned? A comprehensive workflow based on 45 consecutive cases, J. Oral Maxillofac. Surg. 72:376-390, 2014.
- 10. Uribe, F.; Janakiraman, N.; Shafer, D.; and Nanda, R.: Three-dimensional cone-beam computed tomography-based virtual treatment planning and fabrication of a surgical splint for asymmetric patients: Surgery first approach, Am. J. Orthod. 144:748-758, 2013.
- 11. Uribe, F.; Chugh, V.K.; Janakiraman, N.; Feldman, J.; Shafer, D.; and Nanda, R.: Treatment of severe facial asymmetry using virtual three-dimensional planning and a “surgery first” protocol, J. Clin. Orthod. 47:471-484, 2013.
- 12. Brown, M.W.; Koroluk, L.; Ko, C.C.; Zhang, K.; Chen, M.; and Nguyen, T.: Effectiveness and efficiency of a CAD/CAM orthodontic bracket system, Am. J. Orthod. 148:1067-1074, 2015.
- 13. Troy, B.A.; Shanker, S.; Fields, H.W.; Vig, K.; and Johnston, W.: Comparison of incisor inclination in patients with Class III malocclusion treated with orthognathic surgery or orthodontic camouflage, Am. J. Orthod. 135:146.e1-e9, 2009.
- 14. Lin, J. and Gu, Y.: Preliminary investigation of nonsurgical treatment of severe skeletal Class III malocclusion in the permanent dentition, Angle Orthod. 73:401-410, 2003.
- 15. Uribe, F.; Agarwal, S.; Shafer, D.; and Nanda, R.: Increasing orthodontic and orthognathic surgery treatment efficiency with a modified surgery-first approach, Am. J. Orthod. 148:838-848, 2015.
- 16. Ko, E.W.; Hsu, S.S.; Hsieb, H.Y.; Huang, C.S.; and Chen, Y.R.: Comparison of progressive cephalometric changes and postsurgical stability of skeletal Class III correction with and without presurgical orthodontic treatment, J. Oral Maxillofac. Surg. 69:1469-1477, 2011.
- 17. Yu, H.B.; Mao, L.X.; Wang, X.D.; Fang, B.; and Shen, S.G.: The surgery-first approach in orthognathic surgery: A retrospective study of 50 cases, Int. J. Oral Maxillofac. Surg. 44:1463-1467, 2015.
- 18. Uribe, F.; Adabi, S.; Janakiraman, N.; Allareddy, V.; Steinbacher, D.; Shafer, D.; and Villegas, C.: Treatment duration and factors associated with the surgery-first approach: A two-center study, Prog. Orthod. 16:29, 2015.
- 19. Yu, C.C.; Chen, P.H.; Liou, E.J.W.; Huang, C.S.; and Chen, Y.R.: A surgery-first approach in surgical-orthodontic treatment of mandibular prognathism: A case report, Chang Gung Med. J. 33:699-705, 2010.
- 20. Wang, Y.; Ko, E.W.; Huang, C.S.; Chen, Y.R.; and Takano-Yamamoto, T.: Comparison of transverse dimensional changes in surgical skeletal Class III patients with and without presurgical orthodontics, J. Oral Maxillofac. Surg. 68:1807-1812, 2010.
- 21. Liao, Y.F.; Chiu, Y.T.; Huang, C.S.; Ko, E.W.; and Chen, Y.R.: Presurgical orthodontics versus no presurgical orthodontics: Treatment outcome of surgical-orthodontic correction for skeletal class III open bite, Plast. Reconstr. Surg. 126:2074-2083, 2010.
- 22. Baek, S.H.; Ahn, H.W.; Kwon, Y.H.; and Choi, J.Y.: Surgery-first approach in skeletal class III malocclusion treated with 2-jaw surgery: Evaluation of surgical movement and postoperative orthodontic treatment, J. Craniofac. Surg. 21:332-338, 2010.
- 23. Hernández-Alfaro, F.; Guijarro-Martínez, R.; Molina-Coral, A.; and Badía-Escriche, C.: “Surgery first” in bimaxillary orthognathic surgery, J. Oral Maxillofac. Surg. 69:e201-e207, 2011.
- 24. Sugawara, J.; Aymach, Z.; Nagasaka, D.H.; Kawamura, H.; and Nanda, R.: “Surgery first” orthognathics to correct a skeletal Class II malocclusion with an impinging bite, J. Clin. Orthod. 46:429-438, 2010.
- 25. Aldrees, A.M.: Do customized orthodontic appliances and vibration devices provide more efficient treatment than conventional methods? Kor. J. Orthod. 46:180-185, 2016.
- 26. Weber, D.J. II; Koroluk, L.D.; Phillips, C.; Nguyen, T.; and Proffit, W.R.: Clinical effectiveness and efficiency of customized vs. conventional preadjusted bracket systems, J. Clin. Orthod. 47:261-266, 2013.
- 27. Scholz, R.P. and Sarver, D.M.: Interview with an Insignia doctor: David M. Sarver, Am. J. Orthod. 136:853-856, 2009.
- 28. Sarver, D.M. and Ackerman, M.B.: Dynamic smile visualization and quantification, Part 1: Evolution of the concept and dynamic records for smile capture, Am. J. Orthod. 124:4-12, 2003.



COMMENTS
.