Evaluation of Mandibular Position for Splint Therapy Using a Virtual Articulator
To perform an accurate evaluation of occlusion, the clinician must guide the mandible into a correct position relative to the condyle.1,2 If there is an occlusal discrepancy between maximum intercuspation and the centric position of the condyle, the condylar position must first be assessed.1
If the occlusion and TMJ are unstable, some kind of splint therapy will be necessary before a diagnosis can be made. Previous studies have reported that a stabilization splint is more effective than a biteplane splint or anterior-positioning splint.3,4 A stabilizing splint causes fibroses of the TMJ retrodiscal tissue, forming a “pseudodisc” that allows the condyle to be positioned stably and function reliably, thus improving most of the patient’s related symptoms.5 The condyle will then be located in the uppermost position within the articular fossa, with the pseudodisc interposed in the upper part. Once the TMJ and condyle are functionally stable, the clinician can evaluate the patient’s proper TMJ position, make a diagnosis, and develop a treatment plan.6-8
The traditional analog articulator and facebow transfer used to confirm stability of the condyle during splint therapy can be complicated and cumbersome. Today’s digital technology offers an alternative approach.9-12 This article introduces a novel method of evaluating mandibular position before and after splint therapy with a virtual articulator, using a single cone-beam computed tomography (CBCT) image and successive intraoral scans.
Case Report
A 22-year-old female presented with the chief complaint of anterior protrusion. She had a skeletal Class II malocclusion with a hyperdivergent pattern, a convex profile, and multiple restorations. The lower left second and third molars were tilted mesially because of a missing lower left first molar. Bilateral condylar resorption was observed, and the left condylar cortical layer was thinned. A bilateral click of the TMJ was detected on opening and closing, and bilateral joint pain was reported with palpation in the lateral and posterior aspects of each TMJ. The patient could open her mouth 31mm without pain and 37mm with a forced opening. Because of the discrepancy between centric-related occlusion (CRO) and maximum intercuspal position (MIP) and the unstable occlusion, the mandibular position had to be stabilized with a splint before a proper jaw position could be determined and an orthodontic treatment plan established.
A TRIOS* digital scanner was used to take intraoral scans of both arches in MIP and CRO (Fig. 1). For the CRO scan, the mandible was positioned in a musculoskeletally stable position using bilateral manual manipulation and a wax bite registration.** The intraoral scan data were imported into the OrthoAnalyzer*** software program and reprocessed as a stereolithographic (STL) file.
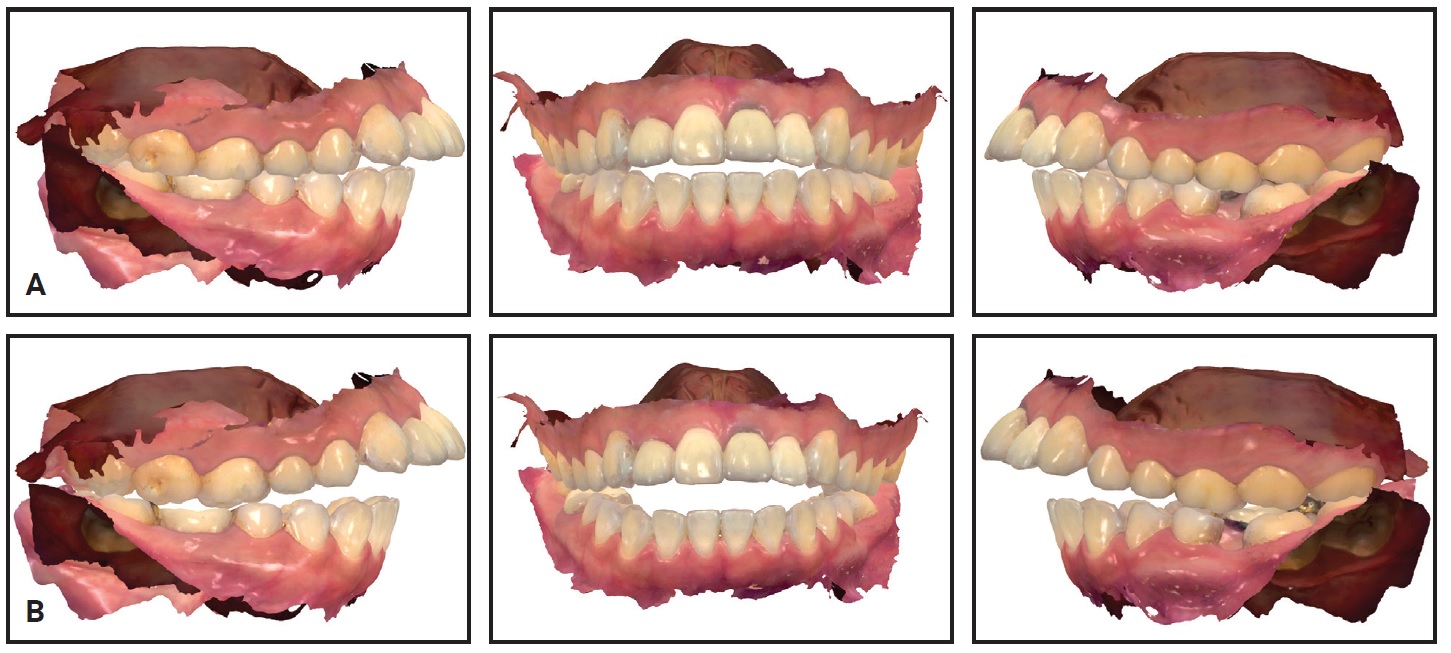
Fig. 1 Digital intraoral scans. A. Maximal intercuspal position (MIP). B. Centric-related occlusion (CRO).
A CBCT scanner† was set at 80kV and 5mA, with a voxel size of .39mm × .39mm × .39mm and a 200mm × 179mm field of view. The digital imaging and communication in medicine (DICOM) file obtained from the CBCT and model scan data were imported into the software program R2GATE,‡ version 2.0.0.
The maxillary model was registered on the CBCT scan in R2GATE. All anterior teeth and both second molars were included when the region of interest was selected, using the manual adjustment scale bar. The initial registration was performed by selecting three corresponding points on each model and the CBCT image; automatic fine registration was used to finish the process. The maxillary teeth in the CBCT scan were replaced with the maxillary teeth of the model scan data. Using the virtual facebow transfer function, a virtual articulator was imported and adjusted to the right and left condyle medial poles and right orbitale (Fig. 2). These data were exported and saved in an STL file format.

Fig. 2 Cone-beam computed tomography data imported into R2GATE‡ program and merged with intraoral scan data. Virtual articulator imported and adjusted to right and left condyle medial poles and right orbitale.
The mandibular position was evaluated by superimposing the STL file in both CRO and MIP. A quantitative measurement of the CRO-MIP discrepancy was obtained using the grid function (Fig. 3).
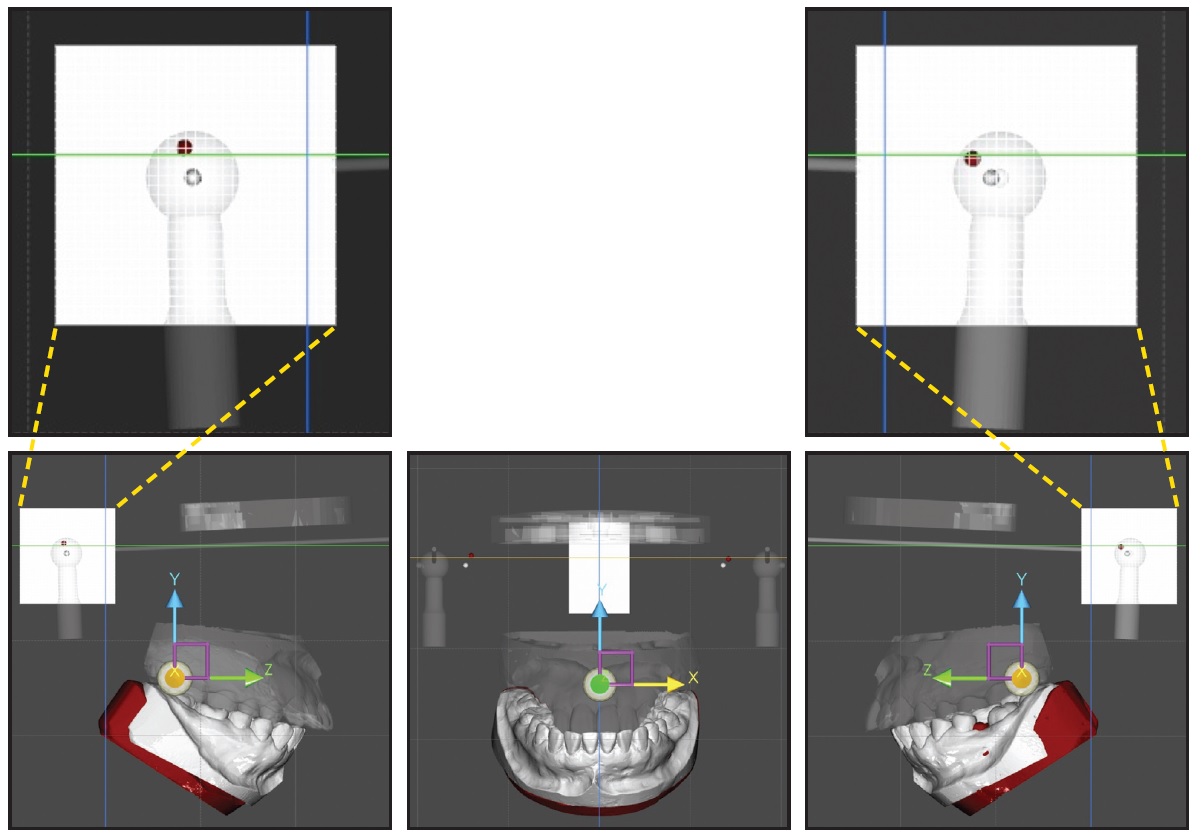
Fig. 3 Mandibular position in MIP (gray) and CRO (red). CRO-MIP discrepancy measured on grid.
The patient wore the splint for six months—the recommended period of stabilization before diagnosis and treatment planning.13 During this time, only intraoral scans (no further CBCT scans) were taken at each visit, and the virtual mounting process was repeated to confirm that the condyle was stable (Fig. 4).
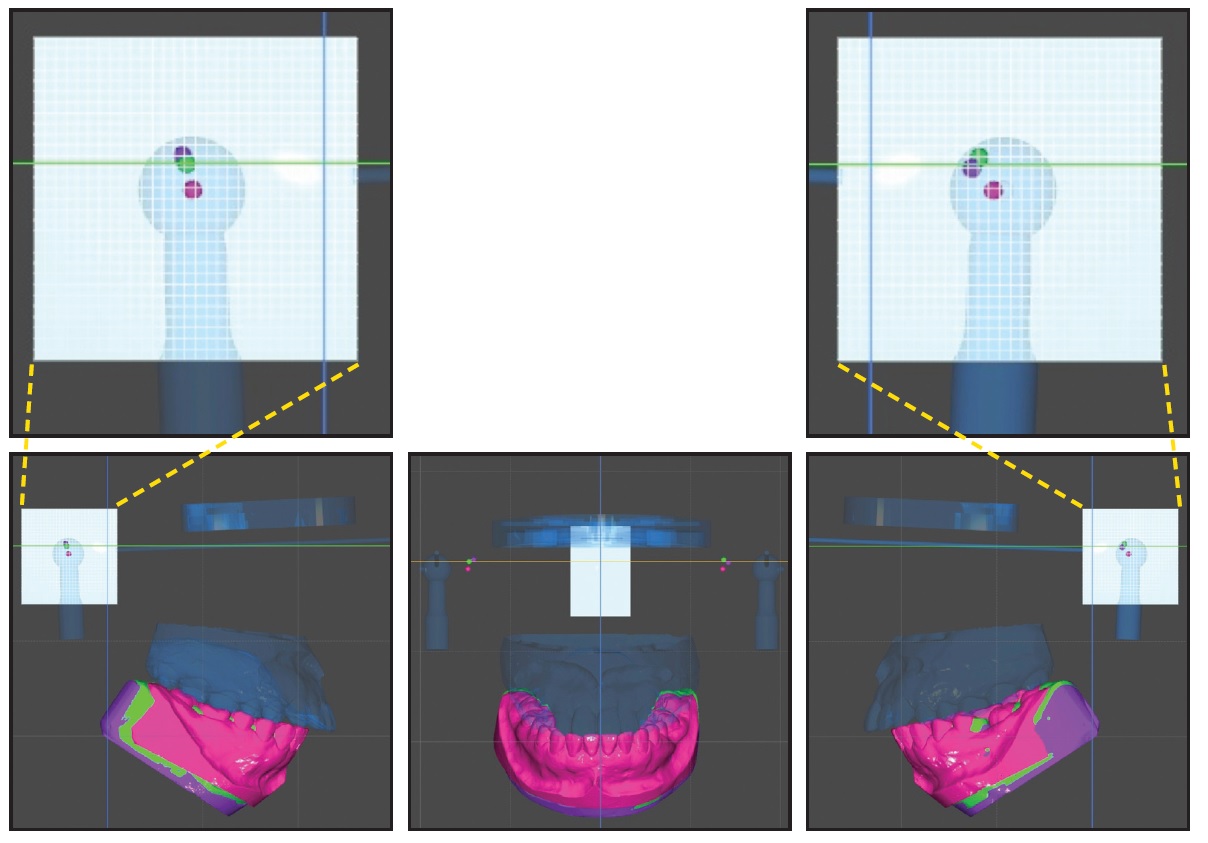
Fig. 4 Change in condylar position during splint stabilization treatment. Quantitative measurement of mandibular positional changes in MIP (pink) and CRO (green) and after stabilization (purple).
Cephalometric analysis showed that the mandible was rotated in a clockwise direction and the condyle was positioned in an upward direction compared with their initial positions (Fig. 5).
Discussion
A stabilization appliance can be used to treat muscle pain disorders14,15 by reducing the parafunctional activity that often accompanies periods of stress.16-19 When a patient presents with TMD related to muscle hyperactivity—such as bruxism—a stabilization appliance will help minimize the forces that can damage tissues, thus allowing more efficient healing.20,21 While the stabilization splint is worn, however, the protective co-contraction disappears and the position of the condyle changes, resulting in a change in occlusion. Therefore, the clinician should periodically adjust the splint to maintain an ideal functional occlusion. In addition, the positional changes of the condyle should be recorded at each visit using a device such as a mandibular position indicator. Once the position of the condyle has been kept constant for three months, the condyle can be considered stabilized.3,13
Our digital method allows sequential mandibular positions to be evaluated based on superimpositions of the initial CBCT data and the intraoral scans taken at each visit (Fig. 6).
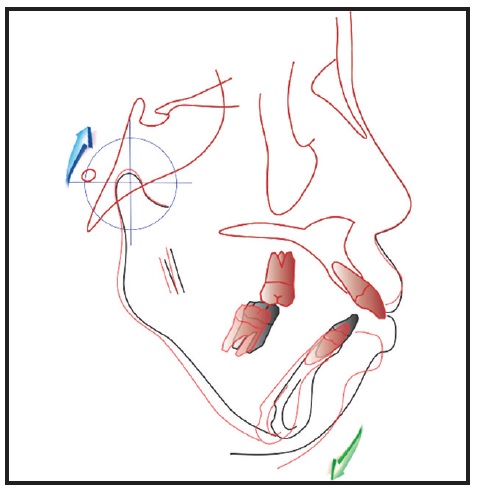
Fig. 5 Superimposition of pretreatment (black) and post-stabilization (red) cephalometric tracings after six months of splint stabilization.
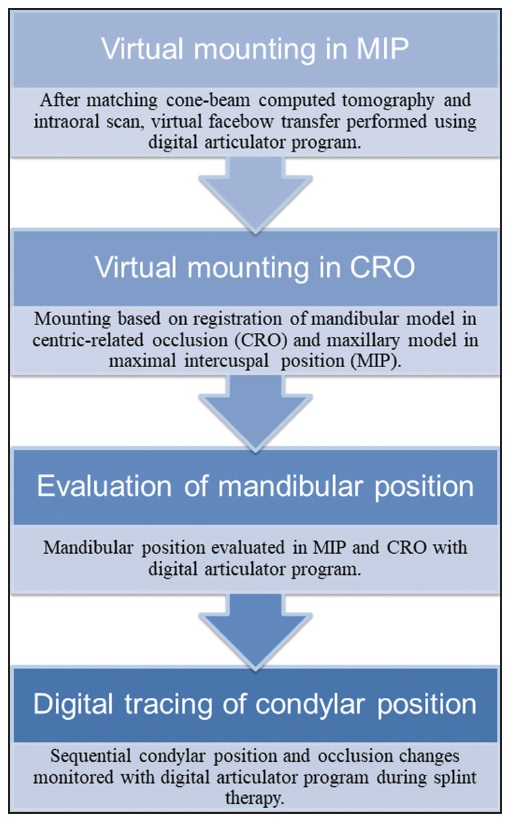
Fig. 6 Digital workflow for evaluation of condylar position using virtual articulator.
This technique reduces chairtime and avoids complicated and costly laboratory work during splint therapy.
For bite scanning, the digital scanner manufacturer recommends taking only partial scans of the premolar and molar areas. In CRO registration, however, unlike MIP, the upper and lower posterior teeth do not contact each other, potentially causing errors in the algorithm for stitching bite scans onto the maxillary and mandibular scans.22 Therefore, an additional adjustment is needed for accurate CRO registration. In this case, we used a surface-based registration from computer-aided design (CAD) software in addition to the normal bite registration provided by the manufacturer.
FOOTNOTES
- *Registered trademark of 3Shape, Copenhagen, Denmark; www.3shape.com.
- **Almorewax, Almore International Inc., Beaverton, OR; www.almore.com.
- ***Trademark of 3Shape, Copenhagen, Denmark; www.3shape.com.
- †Alphard Vega, Asahiroentgen, Kyoto, Japan; www.asahi-xray.co.jp/global.
- ‡Trademark of MegaGEN Implant Co., Ltd., Seoul, Korea; www.r2gate.com.
REFERENCES
- 1. Okeson, J.P.: Management of Temporomandibular Disorders and Occlusion, 7th ed., Elsevier/Mosby, St. Louis, 2013.
- 2. Okeson, J.P.: Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future, Am. J. Orthod. 147:S216-S223, 2015.
- 3. Kazumi, I.: Stabilization of the TMJ, in TMJ 1st Orthodontics Concepts, Mechanics, and Stability, ed. I. Kazumi, Topnotch Kikaku Ltd., Tokyo, 2014, pp. 85-94.
- 4. Schmitter, M.; Zahran, M.; Duc, J.M.; Henschel, V.; and Rammelsberg, P.: Conservative therapy in patients with anterior disc displacement without reduction using 2 common splints: A randomized clinical trial, J. Oral Maxillofac. Surg. 63:1295-1303, 2005.
- 5. Pereira, F.J. Jr.; Lundh, H.; and Westesson, P.L.: Age-related changes of the retrodiscal tissues in the temporomandibular joint, J. Oral Maxillofac. Surg. 54:55-61, 1996.
- 6. Roth, R.H. and Rolfs, D.A.: Functional occlusion for the orthodontist, Part II, J. Clin. Orthod. 15:100-123, 1981.
- 7. Dyer, E.H.: Importance of a stable maxillomandibular relation, J. Prosth. Dent. 30:241-251, 1973.
- 8. Arnett, G.W.; Milam, S.B.; and Gottesman, L.: Progressive mandibular retrusion-idiopathic condylar resorption, Part II, Am. J. Orthod. 110:117-127, 1996.
- 9. Solaberrieta, E.; Garmendia, A.; Minguez, R.; Brizuela, A.; and Pradies, G.: Virtual facebow technique, J. Prosth. Dent. 114:751-755, 2016.
- 10. Kalman, L.; Chrapka, J.; and Joseph, Y.: Digitizing the facebow: A clinician/technician communication tool, Int. J. Prosthod. 29:35-37, 2016.
- 11. He, S.; Kau, C.H.; Liao, L.; Kinderknecht, K.; Ow, A.; and Saleh, T.A.: The use of a dynamic real-time jaw tracking device and cone beam computed tomography simulation, Ann. Maxillofac. Surg. 6:113-119, 2016.
- 12. Petre, A.; Drafta, S.; Stefanescu, C.; and Oancea, L.: Virtual facebow technique using standardized background images, J. Prosth. Dent. 121:724-728, 2019.
- 13. Dawson, P.E.: Adapted centric posture, in Functional Occlusion: From TMJ to Smile Design, ed. P.E. Dawson, Mosby/Elsevier, St. Louis, 2007, pp. 69-73.
- 14. Wahlund, K.; List, T.; and Larsson, B.: Treatment of temporomandibular disorders among adolescents: A comparison between occlusal appliance, relaxation training, and brief information, Acta Odontol. Scand. 61:203-211, 2003.
- 15. Ekberg, E. and Nilner, M.: Treatment outcome of appliance therapy in temporomandibular disorder patients with myofascial pain after 6 and 12 months, Acta Odontol. Scand. 62:343-349, 2004.
- 16. Fuchs, P.: The muscular activity of the chewing apparatus during night sleep: An examination of healthy subjects and patients with functional disturbances, J. Oral Rehab. 2:35-48, 1975.
- 17. Clark, G.T.; Rugh, J.D.; and Handelman, S.L.: Nocturnal masseter muscle activity and urinary catecholamine levels in bruxers, J. Dent. Res. 59:1571-1576, 1980.
- 18. Sheikholeslam, A.; Holmgren, K.; and Riise, C.: A clinical and electromyographic study of the long-term effects of an occlusal splint on the temporal and masseter muscles in patients with functional disorders and nocturnal bruxism, J. Oral Rehab. 13:137-145, 1986.
- 19. Okeson, J.P.: The effects of hard and soft occlusal splints on nocturnal bruxism, J. Am. Dent. Assoc. 114:788-791, 1987.
- 20. Kurita, H.; Kurashina, K.; and Kotani, A.: Clinical effect of full coverage occlusal splint therapy for specific temporomandibular disorder conditions and symptoms, J. Prosth. Dent. 78:506-510, 1997.
- 21. Dos Santos, J.D. Jr. and de Rijk, W.G.: Vectorial analysis of the equilibrium of forces transmitted to TMJ and occlusal biteplane splints, J. Oral Rehab. 22:301-310, 1995.
- 22. Iwaki, Y; Wakabayashi, N.; and Igarashi, Y: Dimensional accuracy of optical bite registration in single and multiple unit restorations, Oper. Dent. 38:309-315, 2013.






COMMENTS
.