CASE REPORT
Miniplate Anchorage for Correction of Skeletal Anterior Open Bite in an Adult
Anterior open bite has a multifactorial etiology, involving skeletal, dental, and functional factors as well as oral habits.1-8 It is also influenced by the facial growth pattern and by respiratory function.1,2,7
Oral habits are usually related to one another. For example, when an open bite is associated with fingersucking or pacifier use, the tongue will usually assume a lower position, between the upper and lower arches. The upper incisors will then be intruded and tipped labially, while the lower incisors are moved lingually; as a result, the lips will be interposed between the upper and lower incisors.1,2,7,9
A long-face syndrome is characterized by alveolar hyperplasia, as well as a clockwise mandibular rotation resulting from the excessive lower facial height.10 When combined with other factors, this growth pattern can aggravate an open-bite malocclusion.1-3,7,10,11
Obstruction of the nasal cavity by the adenoids, tonsils, or hypertrophic turbinates leads to an altered breathing pattern in which the oral cavity remains open most of the time. The tongue then assumes a lower and more anterior resting position to permit air passage, thus contributing to an anterior open bite.2,7 Moreover, when the tongue loses contact with the upper posterior teeth, these teeth are exposed to the action of the perioral muscle, causing palatal torque or even, in some cases, a posterior crossbite.2
Treatment depends partly on the age of the patient. In children, one option is simply to remove the causative factor and wait for self-correction.1,2,7 Treatment of anterior open bite is more challenging in adult patients, with a high rate of relapse. Although most studies of anterior open-bite treatment show good results, the real success of such therapy should be measured by its long-term stability.12
Similar articles from the archive:
- CASE REPORT Skeletal Open-Bite Correction with Mini-Implant Anchorage and Minimally Invasive Surgery September 2018
- CASE REPORT Treatment of Skeletal Class II Open Bite with the Triple Intrusion System August 2018
- CASE REPORT Nonsurgical Treatment of a Severe Skeletal Anterior Open Bite February 2017
This case report shows an adult patient with a skeletal anterior open bite that was corrected using extensive skeletal anchorage.
Diagnosis and Treatment Plan
A 27-year-old female presented for removal of lower fixed appliances after about seven years of prior orthodontic treatment (Fig. 1). Her chief complaint was a lack of vertical interincisinal contact.

Fig. 1 27-year-old female patient with skeletal Class I malocclusion and anterior open bite (lower fixed appliances remaining from previous treatment).
From a frontal view, the patient had normal symmetry and zygomatic projection; the lateral assessment found a straight profile with good zygomatic projection and a normal nasolabial angle and chin-neck line. Excessive lingual inclination of the upper posterior teeth was observed in smiling, but the upper incisor display was acceptable in smiling and at rest. The patient showed an anterior open bite, with extruded and lingually inclined upper posterior teeth and intruded lower anterior teeth. The lower right first premolar was missing. Darkened upper central incisors and gingival hyperplasia on the lower lateral incisors were also noted.
Cone-beam computed tomography (CBCT) using an extended field of view and the SYM Protocol (a systematic method of diagnosis and treatment planning based on tomography) indicated overall symmetry and a skeletal Class I malocclusion associated with an anterior open bite (Fig. 2).
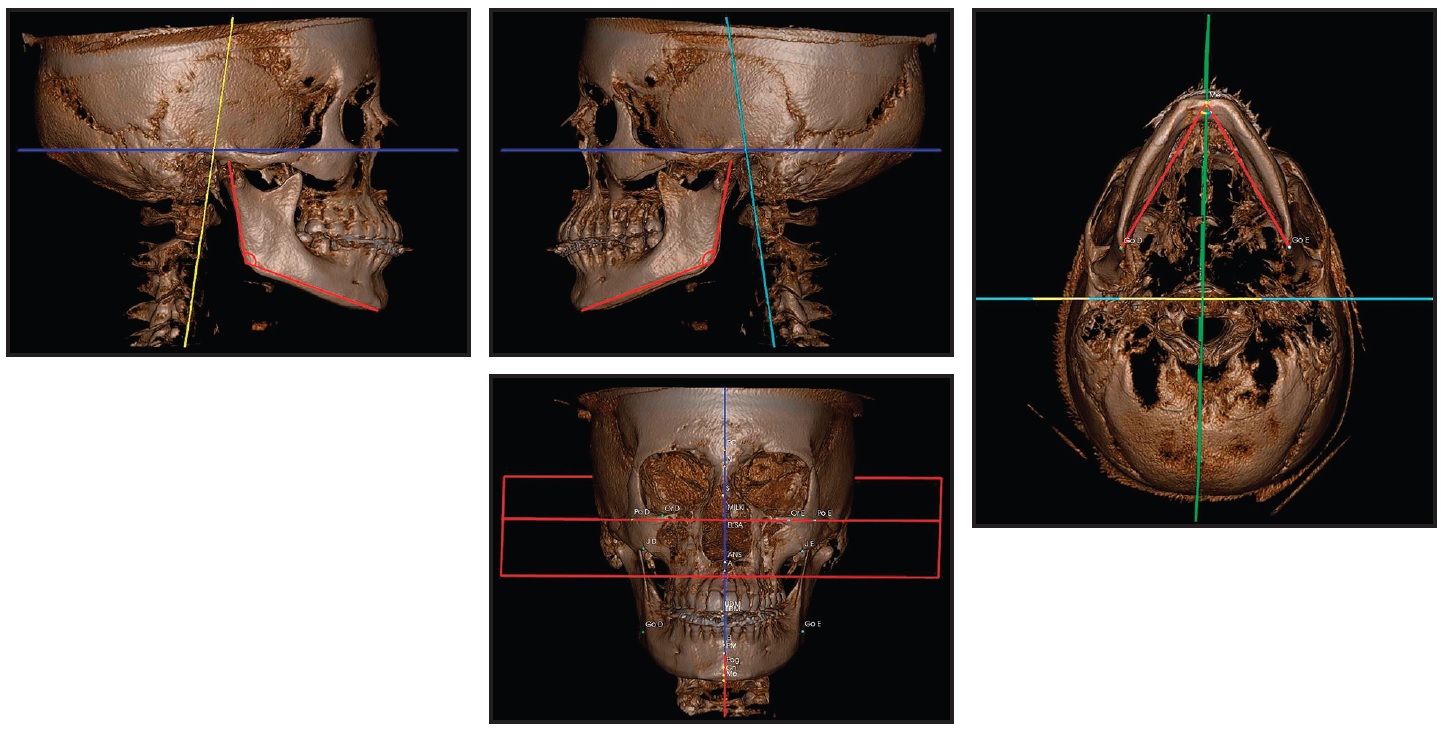
Fig. 2 Images created with cone-beam computed tomography (CBCT) and SYM Protocol.
A mesofacial growth pattern and good maxillomandibular positioning were observed in the three-dimensional side view. Anteroposterior and anteroinferior views confirmed facial symmetry and correspondence of the upper and lower dental midlines with the facial midline. The condyles were centered, with their cortical bones intact. A close-up view showed that upper incisors were properly positioned, but the lower incisors were tipped forward. The panoramic radiograph generated from the CBCT scan revealed mesially angulated lower teeth and a possible endodontic lesion at the apex of the lower left central incisor, which was confirmed with periapical radiographs.
The maxilla showed two distinct occlusal planes, one anterior and one posterior. This alteration of the occlusal plane was probably related to the patient’s habitual mouthbreathing during childhood and adolescence. Gravity had caused extrusion of the upper posterior teeth, which came into premature contact during closure, resulting in the anterior open bite. Because of the posterior extrusion, skeletal anchorage was considered essential to avoid premolar extractions or orthognathic surgery.
An interdisciplinary treatment plan was established, starting with periodontal treatment and endodontic evaluation of the upper central incisors. Four 2mm-thick, T-shaped miniplates (the same plates used for fixation in orthognathic surgery) would be installed to anchor intrusion of the upper and lower posterior segments and distalization of both arches (Fig. 3). In the upper arch, one miniplate would be inserted in each zygomatic pillar, between the first and second molars. Lower miniplates would be inserted in the external mandibular cortical bone on each side, also between the first and second molars.
Treatment Progress
The miniplates were inserted under local anesthesia. Surgery was performed through a linear incision followed by mucoperiosteal detachment and exposure of the target area (Fig. 4).
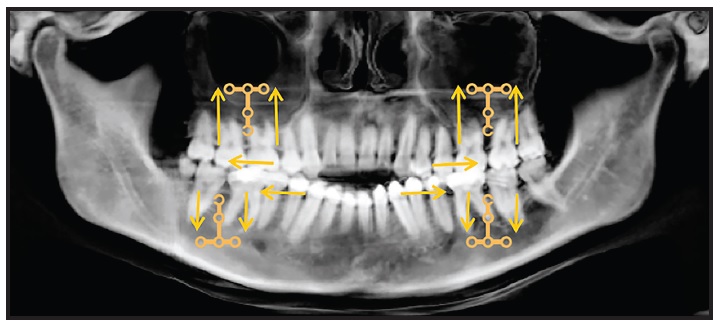
Fig. 3 Planning diagram showing direction of intended movement after placement of T-shaped miniplates: two upper miniplates in zygomatic pillars and two lower miniplates in external mandibular cortical bone.
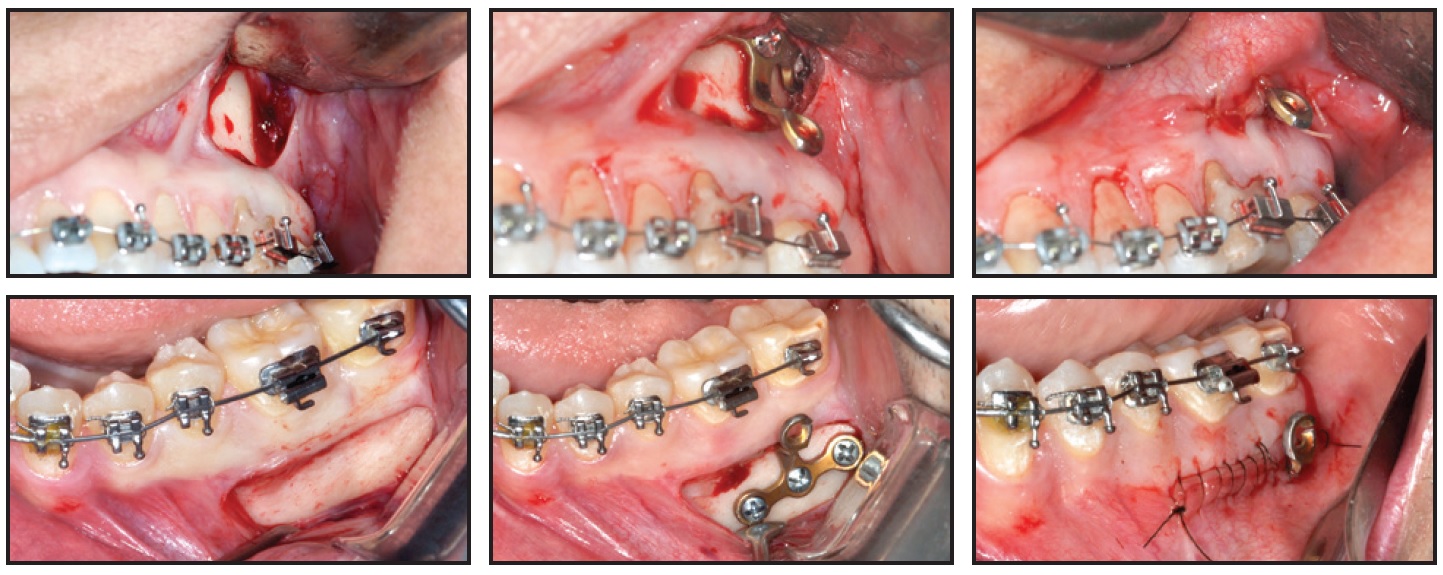
Fig. 4 Surgical procedure for installing T-shaped miniplates, which are bent to conform to patient anatomy and align with incision, keeping miniplates away from gingival margins and thus allowing proper hygiene.
Models made by rapid prototyping were used to facilitate adjustment of the miniplates, reducing the time required for surgery and thus minimizing postoperative edema. Each miniplate was bent to adapt to the patient’s anatomy and affixed using screws 2mm in diameter and 5mm in length. The region was then sutured, with one link of the miniplate left exposed for force attachment.
The upper left third molar and lower left and right third molars were extracted during the surgery, but the upper right third molar was maintained because the upper right first premolar had already been removed. Pre- and postsurgical analgesics and anti-inflammatory drugs were prescribed, and antibiotics were added after the procedure.
On the same day as the miniplate installation, orthodontic treatment began with placement of .018" × .028" Ricketts-prescription fixed appliances and .012" nickel titanium archwires in both arches (Fig. 5). The first molars were anchored to the miniplates with elastomeric ligatures. The upper central and lateral incisors were not included in the archwires while endodontic treatment of the central incisors was still in progress.
After 21 days of leveling and alignment, .016" × .016" Titanol* thermoactivated archwires (80g) were placed, followed by .016" × .022" thermoactivated wires (120g) in both arches (Fig. 6).

Fig. 5 Fixed appliances bonded on day of surgery; .012" nickel titanium archwires inserted and first molars anchored to miniplates with elastomeric ligatures.

Fig. 6 After 21 days of leveling and alignment.
The premolars were included in these mechanics, supported by the miniplate anchorage. Because of the more superior positioning of the upper miniplates and the more inferior positioning of the lower miniplates, with both placed posteriorly on the vestibular side, bone remodeling was achieved in three planes of space, producing simultaneous intrusion, distalization, and labial tipping forces.
Correction of the anterior open bite, with a slightly positive vertical overjet, was observed after three months of treatment (Fig. 7).
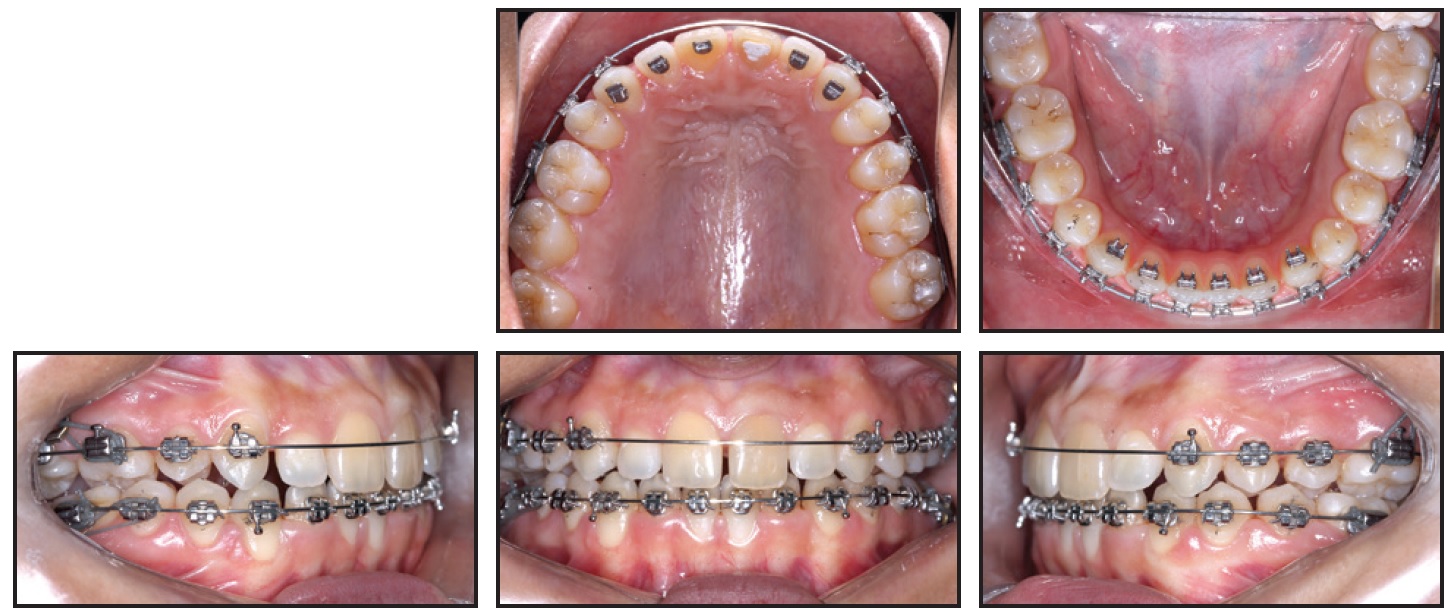
Fig. 7 After three months of treatment, showing correction of anterior open bite and buccal inclination of upper first molars as side effect of intrusive mechanics.
An increased buccal tipping of the upper first molars was noted, with the palatal cusps contacting the buccal cusps of the lower left first molar and lower right second premolar and first molar—a side effect of the force produced by the miniplate attachment to the upper molar tubes. To control the molar tipping, an .016" × .022" Titanol Low-Force* archwire with a lower archform was inserted in the upper arch. The thicker wire, tied tightly with metallic ligatures, promoted slight compression of the upper arch and better torque control of the upper posterior teeth.
During this phase, the patient was referred for speech therapy evaluation. Nogueira** spurs were added to the lingual surfaces of the upper and lower incisors to help eliminate the tongue interpositioning habit.
After five months of treatment, when the endodontic therapy was complete, the upper incisors were bonded and incorporated into the archwire (Fig. 8). The upper posterior teeth were kept anchored to the miniplates using metallic wires coated with flowable resin for patient comfort.
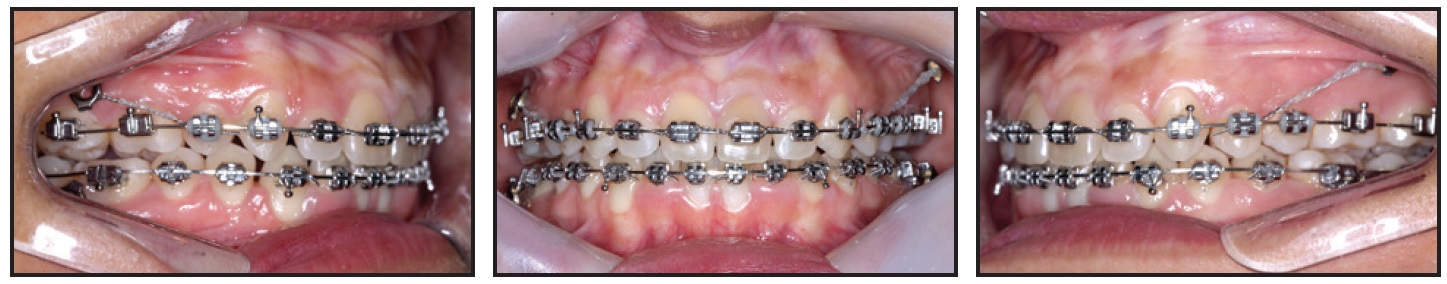
Fig. 8 After five months of treatment, upper incisors bonded and incorporated into archwire; metallic wires coated with flowable resin used to anchor upper posterior teeth to miniplates.
The upper posterior teeth were kept anchored to the miniplates using metallic wires coated with flowable resin for patient comfort.
After 12 months of treatment, the miniplates were removed under local anesthesia. An .016" × .022" Blue Elgiloy*** ideal upper archwire was adapted with inset bends for the upper lateral incisors and an offset bend for the upper left first molar (Fig. 9).
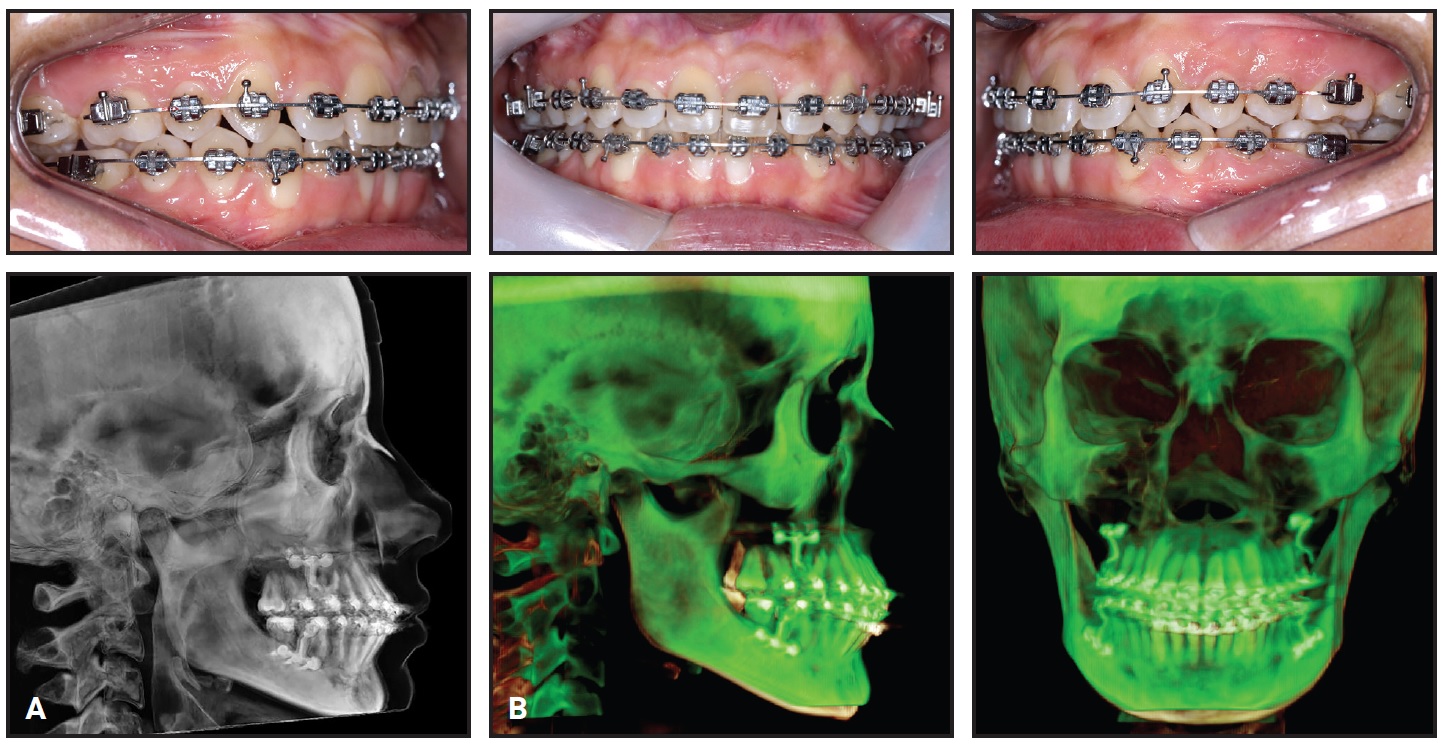
Fig. 9 A. Miniplates removed after 12 months of treatment (CBCT taken before removal). Blue Elgiloy*** ideal archwires inserted in both arches, from first molar to first molar, with inset bends for upper lateral incisors and upper right first molar and offset bends for upper left and lower first molars. B. Superimposition of CBCT images taken early in treatment and after 12 months of treatment.
An inset bend was also made for the upper right first molar, considering the Class II molar relationship distal to the missing upper right first premolar. The archwire was cut distal to the upper first molars, leaving the upper right second and third molars and upper left second molar free for physiological intercuspation. An .016" × .022" Blue Elgiloy ideal wire was also adapted in the mandibular arch, with offsets only at the lower first molars. The lower second molars were not included to allow physiological occlusion with their antagonists.
Treatment Results
Orthodontic appliances were removed after 14 months of treatment (Fig. 10). The objectives of this phase had been met with the achievement of a functional and balanced occlusion. The patient was referred for gingivoplasty, whitening, and faceting procedures on the upper central incisors.

Fig. 10 A. Patient after 14 months of treatment. B. After gingivoplasty, whitening, and faceting.
While provisional upper central incisor crowns were being made from bis-acryl composite resin (Fig. 11), the posterior intrusion resulting from bone remodeling in this region was evident. Smile esthetics were also notably improved, with good incisor display and correction of the negative torque on the upper posterior teeth.
The patient was checked every six months after treatment. Records taken three years post-treatment verified the stability of the occlusal relationships and facial harmony (Fig. 12).

Fig. 11 Provisional upper central incisor crowns made from bis-acryl composite resin.

Fig. 12 Patient three years after treatment.
Discussion
Several studies have demonstrated the superiority of CBCT imaging over traditional two-dimensional diagnostic methods.13,14 Because of the overlapping effect of lateral cephalograms, they cannot be used to identify the actual position of every tooth.13 Tomographic imaging, on the other hand, allows measurement of root resorption, evaluation of bone thickness, examination of the relationship between the alveolar crest and the teeth, and assessment of root anatomy, resulting in more accurate placement of skeletal anchorage and prediction of tooth movements.13 The SYM Protocol used in the present case facilitates the evaluation of true skeletal asymmetries and measurement of internal structures, providing precise values for orthodontic diagnosis15 (Fig. 2).
The standard treatment for open bite in adult patients involves orthodontic therapy and orthognathic surgery.11,16,17 Another option is to reduce the vertical dimension by extracting teeth, but this has disadvantages including loss of anchorage and removal of teeth needed to balance the occlusion.18 Inability to control tooth movement in all three planes of space is a major limitation of conventional orthodontics. Skeletal anchorage has evolved in recent years to enable the achievement of better results with fewer side effects, thus optimizing orthodontic movements and allowing a significant reduction in treatment time.15,19 In adult patients with anterior open bites, the use of skeletal anchorage can often avoid the need for orthognathic surgery.10,16,18-22
The efficacy of temporary anchorage devices or mini-implants is restricted by proximity to root apices, limitations in anchoring complex orthodontic movements, the potential for fracture, and a relatively high failure rate during treatment.19,20,23,24 In contrast, miniplates can be inserted in areas with better bone quality, away from the root apices,8 and provide greater control of complex orthodontic movements in all three planes of space.15,19,22
A technique has been described using mini-implants in the infrazygomatic crest to anchor maxillary posterior intrusive mechanics for the correction of skeletal open bite.25,26 Even though the infrazygomatic crest is not located between the dental roots, however, it is close to the apices, and it requires sufficient bone volume for stable insertion. A miniplate inserted at the base of the zygomatic pillar allows the use of greater force and range of motion. In the adult open-bite case shown here, miniplate anchorage enabled more intrusion of the posterior segments and the use of more attachments providing simultaneous 3D forces. Optimal results were achieved without the need for premolar extractions or orthognathic surgery—either of which could have worsened the patient’s good facial profile. Disadvantages of miniplates include a higher cost and the need for surgical procedures for their installation and removal, involving the risk of infection.
One of the most important factors to consider in the treatment of open bite is long-term stability. Consolaro has proposed the term “tensegrity” to describe the stability of a system’s morphology.19 When balance is restored among the occlusion, articulation, and musculature, a new level of tensegrity is reached.19,20 In a case such as this one, therefore, it is important to integrate speech therapy and tongue spurs to retrain the tongue position and thus ensure greater stability.27 Poor tongue positioning may persist even after correction of a dentoalveolar discrepancy.2 In our patient, no tongue-containment device was needed to sustain the results of treatment and the new state of tensegrity.
FOOTNOTES
- *Trademark of Forestadent GmbH, Pforzheim, Germany; www.forestadent.com.
- **3M, São José, Brazil; www.3M.com.br.
- ***Registered trademark of Rocky Mountain Orthodontics, Denver, CO; www.rmortho.com.
REFERENCES
- 1. Almeida, R.R. and Ursi, W.J.S.: Anterior open bite: Etiology and treatment, Oral Health 80:27-31, 1990.
- 2. Almeida, R.R.; Santos, S.C.B.N.; Santos, E.C.A.; Insabralde, C.M.B.; and Almeida, M.R.: Anterior open bite: Considerations and a case report [in Spanish], Rev. Dent. Press J. Orthod. 3:17-29, 1998.
- 3. Artese, A.; Drummond, S.; Nascimento, J.M.; and Artese, F.: Criteria for the diagnosis and stable treatment of anterior open bite, Dent. Press J. Orthod. 16:136-161, 2011.
- 4. Dung, J.D. and Smith, R.J.: Cephalometric and clinical diagnoses of open bite tendency, Am. J. Orthod. 94:484-490, 1998.
- 5. Lopez-Gavito, G.; Wallen, T.R.; Little, R.M.; and Joondeph, D.R.: Anterior open-bite malocclusion: A longitudinal 10-year post-retention evaluation of orthodontically treated patients, Am. J. Orthod. 87:175-186, 1985.
- 6. Maciel, C.T.V. and Leite, I.C.G.: Etiological aspects of the anterior open bite and its implications for orofacial functions [in Portuguese], Pro. Fono. 17:293-302, 2005.
- 7. Subtelny, J.D. and Sakuda, M.: Open-bite: Diagnosis and treatment, Am. J. Orthod. 50:337-358, 1964.
- 8. Sugawara, J.: Temporary skeletal anchorage devices: The case for miniplates, Am. J. Orthod. 145:145-565, 2014.
- 9. Vela-Hernandez, A.; Lopéz-García, R.; García-Sanz, V.; Paredes-Gallardo, V.; and Lasagabaster-Latorre, F.: Nonsurgical treatment of skeletal anterior open bite in adult patients: Posterior build-ups, Angle Orthod. 87:33-40, 2017.
- 10. Schendel, S.A.; Eisenfeld, J.; Bell, W.H.; Epker, B.N.; and Mihelevich, D.J.: The long face syndrome: Vertical maxillary excess, Am. J. Orthod. 70:398-408, 1976.
- 11. Cardoso, M.A.; Bertoz, F.A.; Capelozza Filho, L.; and Reis, S.A.B.: Cephalometric characteristics of the long face pattern [in Portuguese], Rev. Dent. Press Ortod. Ortop. Facial 10:29-43, 2005.
- 12. Huang, G.J.: Long-term stability of anterior open-bite therapy: A review, Semin. Orthod. 8:162-172, 2008.
- 13. Consolaro, A. and Freitas, P.Z.: Volumetric tomography (dental) versus helical (medical) in orthodontic planning and in the diagnosis of tooth resorption [in Portuguese], Rev. Clín. Ortod. Dent. Press 6:108-111, 2007.
- 14. Ludlow, J.B.; Gubler, M.; Cevidanes, L.; and Mol, A.: Precision of cephalometric landmark identification: Cone-beam computed tomography vs. conventional cephalometric views, Am. J. Orthod. 136:312-313, 2009.
- 15. Silva, E.; Meloti, F.; Pinho, S.; Cardoso, M.A.; and Consolaro, A.: Biomechanics with mini plates, Rev. Clín. Ortod. Dent. Press 17:17-34, 2018.
- 16. Kuroda, S.; Sakai, Y.; Tamamura, N.; Deguchi, T.; and Takano-Yamamoto, T.: Treatment of severe anterior open bite with skeletal anchorage in adults: Comparison with orthognathic surgery outcomes, Am. J. Orthod. 132:599-605, 2007.
- 17. Reichert, I.; Figel, P.; and Winchester, L.: Orthodontic treatment of anterior open bite: A review article—Is surgery always necessary? Oral Maxillofac. Surg. 18: 271-277, 2014.
- 18. Sugawara, J. and Nishimura, N.: Minibone plates: The skeletal anchorage system, Semin. Orthod. 11:47-56, 2005.
- 19. Consolaro, A.: Miniplates and mini-implants: Bone remodeling as their biological foundation, Dent. Press J. Orthod. 20:16-31, 2015.
- 20. Consolaro, A.: Mini-implants and miniplates generate sub-absolute and absolute anchorage [in Portuguese], Dent. Press J. Orthod. 19:20-23, 2014.
- 21. De Clerck, H.J.; Cornelis, M.A.; Cevidanes, L.H.; Heymann, G.C.; and Tulloch, C.J.F.: Orthopedic traction of the maxilla with miniplates: A new perspective for treatment of midface deficiency, J. Oral Maxillofac. Surg. 67:2123-2129, 2009.
- 22. Umemori, M.; Sugawara, J.; Mitani, H.; Nagasaka, H.; and Kawumura, H.: Skeletal anchorage system for open-bite correction, Am. J. Orthod. 115:166-174, 1999.
- 23. Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.M.; and Takano-Yamamoto, T.: Root proximity is a major factor for screw failure in orthodontic anchorage, Am. J. Orthod. 13:68-73, 2007.
- 24. Papageorgiou, S.N.; Zogakis, I.P.; and Papadopoulos, M.A.: Failure rates and associated risk factors of orthodontic miniscrew implants: A meta-analysis, Am. J. Orthod. 142:577-595, 2012.
- 25. Chen, C.; Lee, A.; Chang, C.; and Roberts, W.E.: Convex, Class II, deepbite, gummy smile and lingually tipped incisors: Conservative correction with bone screws and a crown lengthening procedure, Int. J. Orthod. Implantol. 45:60-81, 2017.
- 26. Lin, C.; Wu, I.; Chang, C.; and Roberts, E.: Simplified mechanics for gummy smile correction, Int. J. Orthod. Implantol. 47:72-91, 2017.
- 27. Garret, J.; Araujo, E.; and Baker, C.: Open-bite treatment with vertical control and tongue reeducation, Am. J. Orthod. 149:269-276, 2016.







COMMENTS
.