CASE REPORT
Orthodontic Eruption of an Impacted and Dilacerated Maxillary Central Incisor
Maxillary central incisors are the third most commonly impacted teeth, following third molars and maxillary canines.1 The etiology of tooth impaction is multifactorial, typically involving genetic and environmental factors such as lack of space in the dental arch, an abnormal frenulum, prolonged retention of deciduous teeth, ankylosis, supernumerary teeth, tumors, cysts, or trauma.2
Studies have shown that about 30% of children under age 7 have suffered injuries to one or more of their deciduous incisors,3,4 and that the most serious injuries to deciduous teeth occur between ages 1 and 3.5,6 Intrusion and avulsion are the most severe injuries that can affect developing tooth germs in children up to 2 years old.7 Intrusion of deciduous teeth can lead to a variety of pathologic alterations to the permanent teeth, including hypoplasia, crown dilaceration, root angulation or dilaceration, partial or complete arrest of root formation, sequestration of the permanent tooth germ, and disturbances in eruption.8
Impacted maxillary incisors in the early mixed dentition pose a clinical challenge to the orthodontist,9 especially when they are associated with crown or root dilacerations, because of their complex axial positions. This case report describes the orthodontic management of an impacted and dilacerated maxillary central incisor associated with a history of trauma in the deciduous dentition.
Diagnosis and Treatment Plan
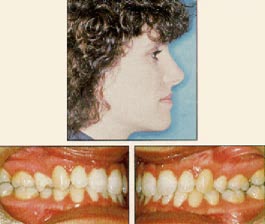
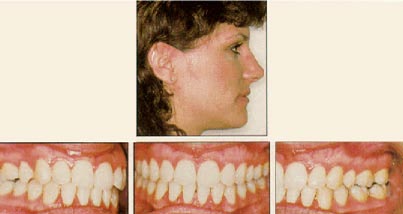
A 10-year-old female presented to the Department of Orthodontics, Federal University of Rio de Janeiro Dental School, with the chief complaint of a missing maxillary right central incisor and changes in adjacent tooth positions that had caused an unpleasant “aged Class III smile” (Fig. 1A). This unesthetic appearance had led to psychological issues due to bullying at school.
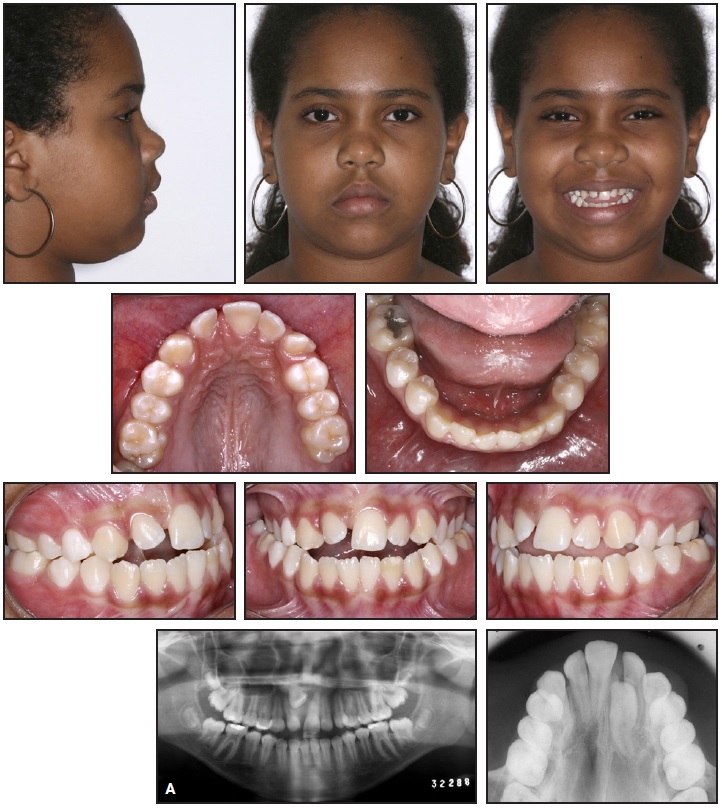
Fig. 1 A. 10-year-old female patient with missing maxillary right central incisor, anterior and posterior crossbite, and anterior open bite before treatment (continued in next image).
The patient had a history of trauma to her maxillary deciduous incisors at age 2. Clinical examination found a convex profile and excessive lower facial height. She showed bilateral Class I canine and molar relationships, anterior and posterior crossbites, and an anterior open bite caused by a tongue-thrust habit. Overbite and overjet were −2mm and −1mm, respectively. The absence of the maxillary right central incisor had caused mesial displacement of the adjacent teeth and collapse of the maxillary anterior region, with the maxillary left central incisor deviated 3.7mm from the facial midline. Dental cast analysis revealed arch-length discrepancies of −10.9mm in the maxilla and −2.3mm in the mandible.
Pretreatment panoramic and occlusal radiographs indicated that the maxillary right central incisor was partly intraosseous and impacted. Cone-beam computed tomography (CBCT) showed that the root of the incisor was positioned horizontally, close to the floor of the nasal cavity and the maxillary right lateral incisor (Fig. 1B). In addition to ectopic eruption, the right central incisor presented dilaceration and shortening of the root. These alterations were attributable to displacement of the tooth germ from the trauma in the deciduous dentition.
Cephalometric analysis (Fig. 1C, Table 1) confirmed a skeletal Class I relationship (ANB = 4.4°) with a high mandibular plane angle (SNGoGn = 40.4°). The mandibular incisors were protruded and proclined (L1-NB = 8.3mm, 31.9°).
Treatment objectives were to recover space in the upper arch for the maxillary right central incisor, guide this tooth into its proper position, obtain good gingival attachment and a symmetrical gingival margin for the impacted tooth, correct the posterior and anterior crossbites and anterior open bite, and reduce the bimaxillary protrusion.
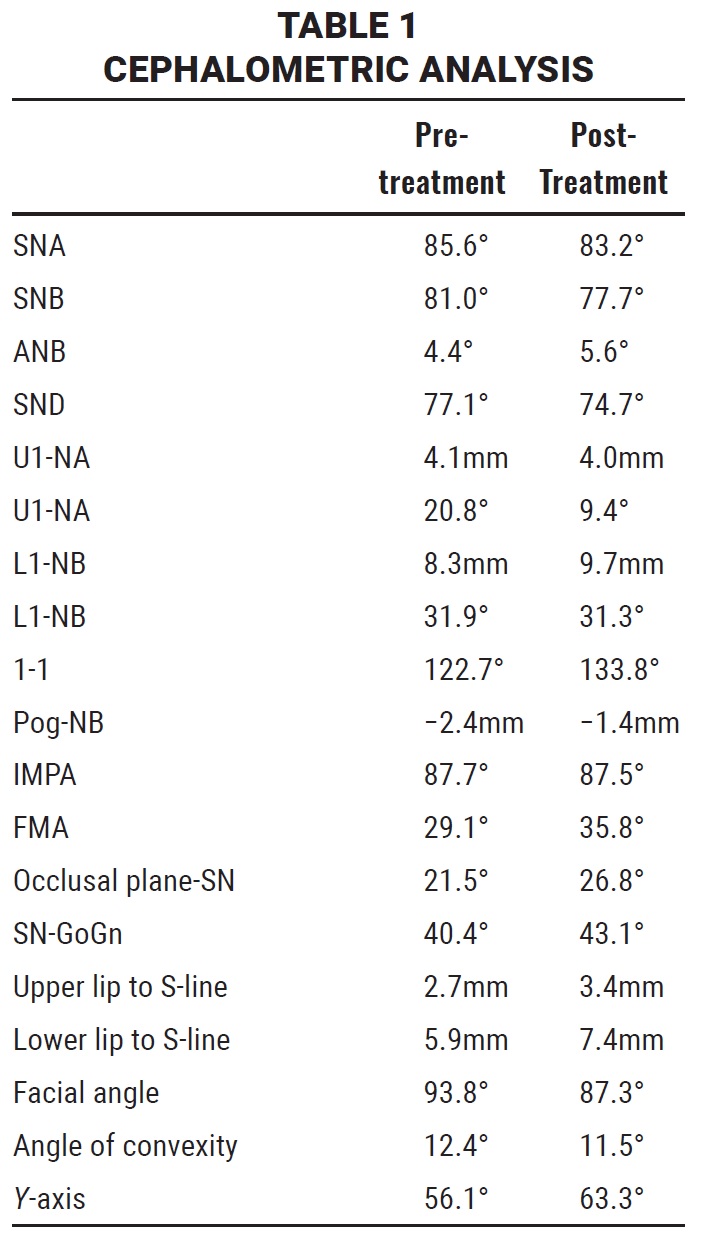
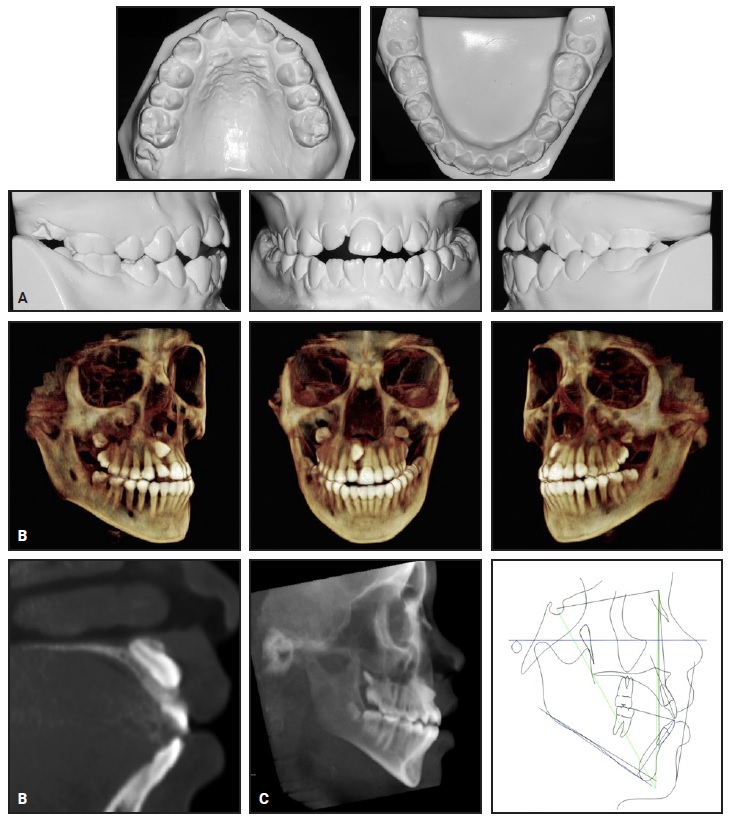
Fig. 1 (cont.) A. 10-year-old female patient with missing maxillary right central incisor, anterior and posterior crossbite, and anterior open bite before treatment. B. Cone-beam computed tomography (CBCT) reconstruction and sagittal slice indicating position of maxillary right central incisor. C. Pretreatment cephalometric analysis (black = Steiner, blue = Tweed, green = Downs).
The following treatment alternatives were considered:
1. Extraction of the impacted central incisor and space closure by moving the lateral incisor into its place, followed by prosthetic restoration.
2. Extraction of the impacted central incisor and orthodontic space opening for future restoration with an implant or bridge after the cessation of growth.
3. Extraction of the impacted central incisor and autotransplantation of a premolar to the region.
4. Surgical repositioning of the impacted central incisor.
5. Orthodontic space opening for the impacted central incisor, followed by surgical exposure and traction into the arch. Extraction of four premolars could be considered because of the patient’s vertical growth tendency and protrusive incisors.
After discussing the treatment alternatives and the uncertain prognosis, the parents and orthodontists decided in favor of traction of the impacted tooth into its proper position. The first stage of treatment would involve correction of the maxillary transverse deficiency and the posterior and anterior crossbites using a modified Haas expander. This would also provide space for the impacted tooth. The second stage would consist of surgical exposure of the impacted incisor and orthodontic traction into the arch. A final stage would involve the extraction of four premolars to obtain a better occlusal relationship.
Treatment Progress
A modified Haas expander10 was fabricated with two .028" helical springs contacting the mesial surfaces of the upper left central and right lateral incisors to obtain adequate space for the right central incisor (Fig. 2A). Composite was added to the lateral and central incisors to prevent disengagement of the springs during expansion. The Haas appliance was activated .25mm twice daily until the 11mm screw had completely opened. During activation, the coil springs naturally displaced the left central and right lateral incisors to open space for the impacted tooth.
After one month of palatal expansion, adequate anterior space had been created, and the posterior crossbite was corrected (Fig. 2B). Stainless steel edgewise brackets were then bonded to the upper left incisors, canine, and second premolar, and a segmented .016" nickel titanium archwire was inserted to initiate leveling and alignment (Fig. 3A).
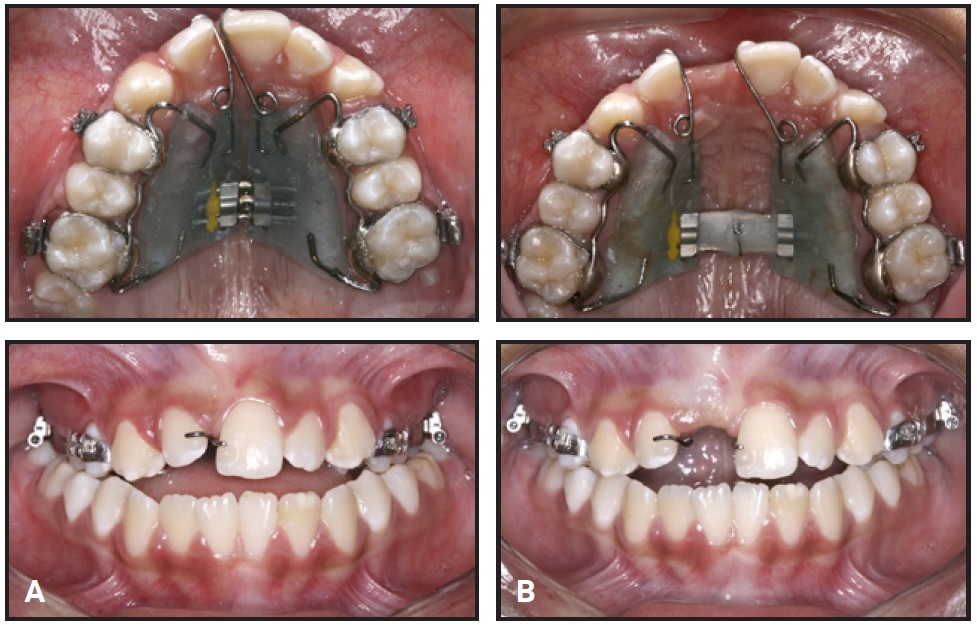
Fig. 2 A. Modified Haas expander. B. After one month of expansion.
One month later, brackets were bonded to the upper right lateral incisor, canine, and second premolar, enabling the insertion of continuous .016" nickel titanium (Fig. 3B) and .016" and .018" stainless steel archwires, successively. A lingual arch with spurs was placed to control the strong tongue-thrust habit during swallowing and speech. This was removed 12 months later, owing to constant breakage of the spurs, and replaced by cleats bonded to the lingual surfaces of the lower incisors. Four months after the start of leveling and alignment, a temporary resin crown was adapted to the maxillary right central incisor space by means of a bonded bracket, filling the opened space and thus improving smile esthetics (Fig. 3C).

Fig. 3 A. Edgewise appliance bonded for leveling and alignment of maxillary left segment with segmented .016" nickel titanium archwire. B. One month later, edgewise appliance bonded to maxillary right segment and continuous .016" nickel titanium archwire inserted. C. Three months later, temporary resin crown adapted to fit maxillary right central incisor space.
A continuous .021" × .025" stainless steel stabilizing archwire was then placed in all the brackets, and the maxillary teeth were tied together to improve anchorage during the orthodontic traction phase. The Haas appliance was removed 11 months later.
After 10 months of waiting for spontaneous eruption of the upper right central incisor, a closed-flap surgical exposure was performed from the labial side, and a bracket with a twisted ligature wire was bonded to the labial surface of the incisor. A stainless steel closed-coil spring with 80g of force was attached between the archwire and the twisted ligature wire (Fig. 4A). The force vector was initially oriented toward the distal to divert the tooth from an upper labial frenulum that was preventing the tooth from erupting. After this, multiple hooks were welded to the .021" × .025" stabilizing archwire, and the force vectors were redirected at every appointment, so that the tooth could be pulled down gradually and centered in the space (Fig. 4B).

Fig. 4 A. After surgical exposure of maxillary right central incisor, stainless steel closed-coil spring activated for incisor traction. B. Redirection of traction force vectors.
After six months of traction, an .016" stainless steel segmented archwire with a coil spring was welded to a hook attached to the .021" × .025" stainless steel main archwire (Fig. 5A). The segmented arch was adapted so that its active edge would fit passively in the right central incisor’s mesial bracket wing, away from the distal wing. The active edge was tied to the bracket slot to help correct the rotation of the right central incisor before it was guided into the occlusal plane. During this phase, we had to grind down the artificial crown to make room for the erupting tooth. Once the temporary crown was completely removed, a segment of elastomeric chain with 80g of force was connected between the right central incisor and hooks on the archwire to continue gradual traction (Fig. 5B).
After 11 months of incisor traction, when the incisal edge of the maxillary right central incisor was approaching the occlusal plane, an .012" stainless steel multiloop archwire was inserted to continue the leveling and rotation correction (Fig. 6A). The springs were placed to increase archwire flexibility, thus enabling the controlled forces to be transferred to the right central incisor.
Twenty-four months later, a full fixed edgewise appliance was bonded in the lower arch, and a sequence of .012", .014", .016", .018", and .017" × .025" stainless steel archwires was used for leveling and alignment and correction of buccolingual axial inclinations (Fig. 6B). The lingual root torque of the upper right central incisor was carefully individualized until the root was properly situated in the alveolar bone.
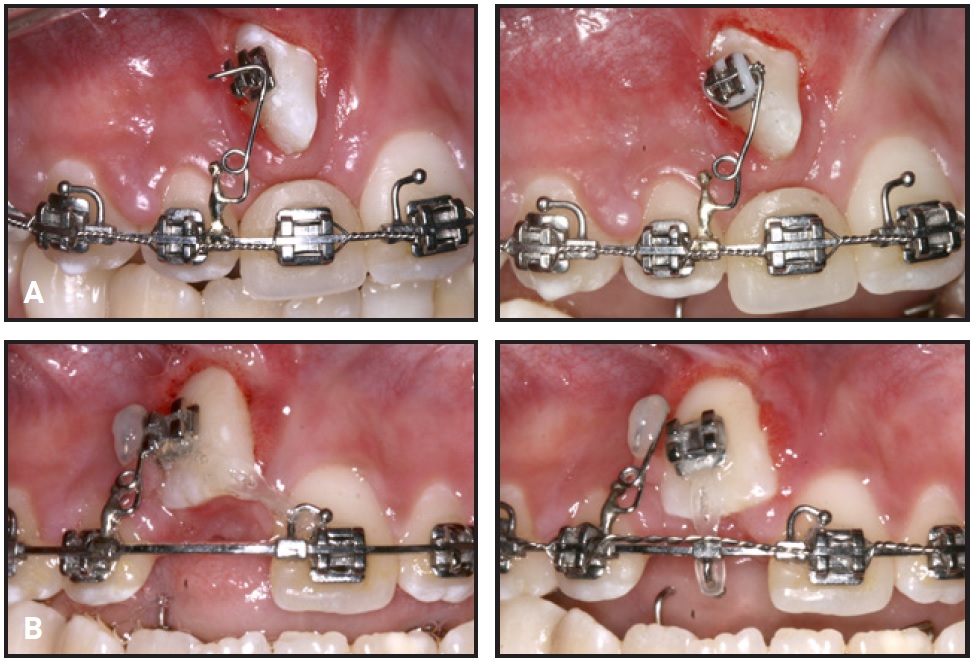
Fig. 5 A. After six months of incisor traction, segmented .016" stainless steel archwire with coil spring welded to hook on .021" × .025" stainless steel archwire. B. Traction of maxillary right central incisor with elastomeric chain after removal of temporary crown.
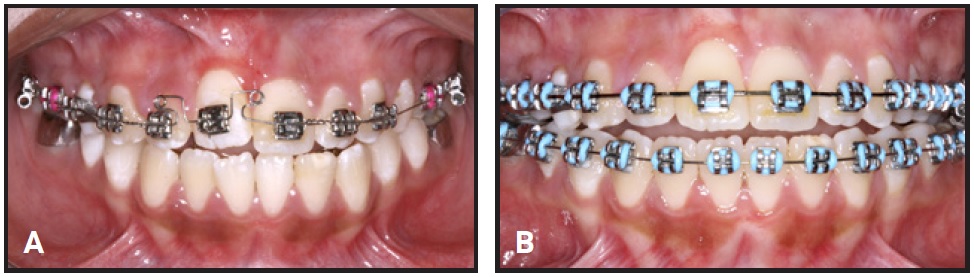
Fig. 6 A. After 11 months of incisor traction, multiloop .012" stainless steel archwire placed for further leveling and rotation correction. B. 24 months later, mandibular arch bonded and .012" stainless steel archwires inserted.
After reviewing the case, we opted to extract four second premolars. We felt it would be too risky to extract the first premolars and possibly have to retract the entire maxillary anterior segment, considering the dilaceration of the right central incisor and the patient’s history of trauma. Therefore, we planned for anchorage loss with free mesial movement of the posterior teeth to enable closure of the mandibular plane and correction of the anterior open bite. Continuous .018" × .025" stainless steel archwires were inserted, and a long elastomeric chain exerting light force was tied from the first premolars to the first molars. Four months later, when two-thirds of the extraction space had been closed, .018" × .025" retraction arches with teardrop loops were activated to complete space closure and slightly retract the incisors (Fig. 7A). At this time, the patient requested removal of the orthodontic appliances because she was already satisfied with the outcome achieved. We negotiated with the patient to replace the stainless steel edgewise appliances with MBT* monocrystalline ceramic brackets, as an incentive that would allow us to properly finish the orthodontic treatment (Fig. 7B). At the end of treatment, upper 2-2 and lower 4-4 lingual retainers were bonded, and an upper Essix** retainer was delivered.

Fig. 7 A. After 36 months of treatment (four months after extraction of four second premolars), .018" × .025" retraction arch with teardrop loops placed to complete space closure and slightly retract incisors. B. MBT* monocrystalline ceramic brackets bonded to finish treatment.
Treatment Results
The total active treatment period was 42 months, not including the 10-month waiting period. Post-treatment records demonstrated Class I molar and canine relationships, resolution of the posterior crossbite, and harmonious dental arches (Fig. 8A). The impacted maxillary right central incisor was successfully aligned and presented an acceptable gingival contour.

Fig. 8 A. Patient after 42 months of treatment (continued in next image).
Although the orthodontic traction was carried out carefully and with controlled force, the panoramic radiograph and CBCT showed moderate to pronounced root resorption of the right central incisor and periodontal bone loss on its labial surface (Fig. 8B). The root dilaceration was attributable to the previous trauma, but every effort was made to prevent cortical bone fenestration.
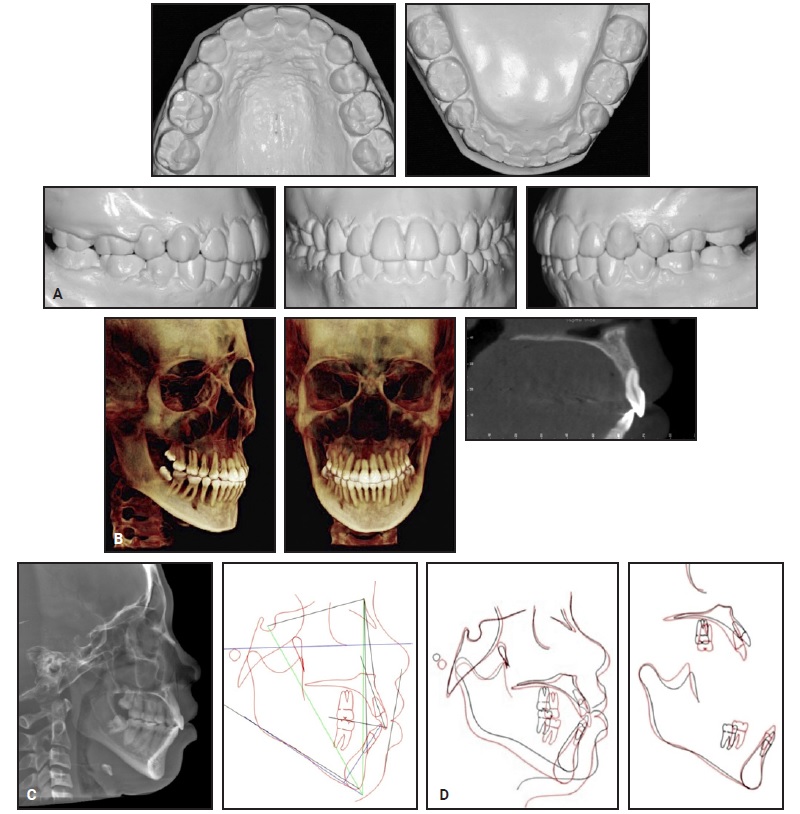
Fig. 8 (cont.) A. Patient after 42 months of treatment. B. CBCT reconstruction and sagittal slice indicating position of maxillary right central incisor. C. Post-treatment cephalometric analysis (black = Steiner, blue = Tweed, green = Downs). D. Superimposition of pretreatment (black) and post-treatment (red) cephalometric tracings.
Despite the patient’s vertical mandibular growth tendency (Fig. 8C,D), the anterior open bite was corrected by mesial movement of the posterior teeth and by resolution of the tongue-thrust habit with the aid of a speech therapist. Treatment results have been stable, as observed during a three-year follow-up period (Fig. 9).
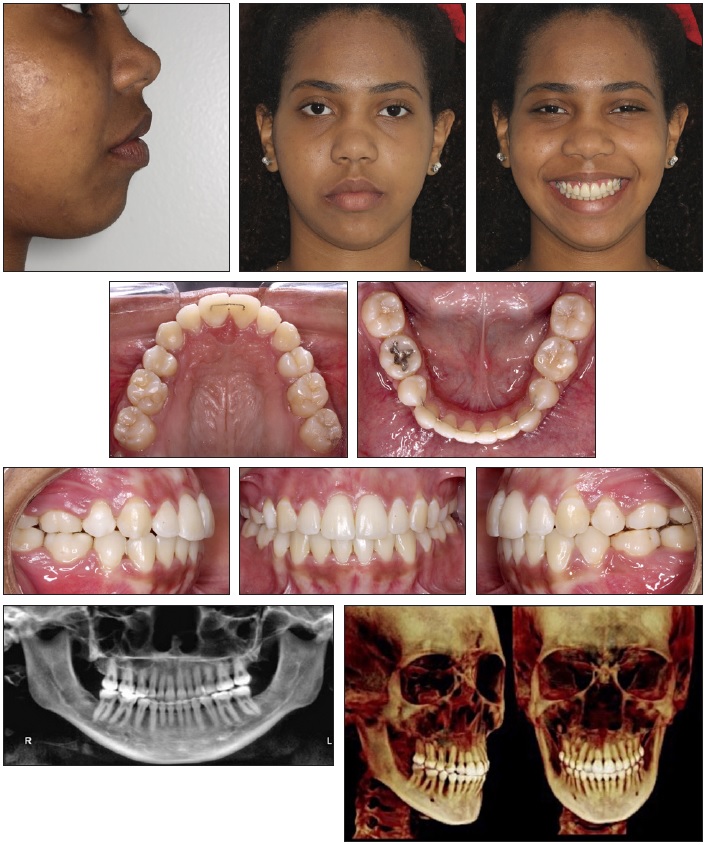
Fig. 9 Patient three years after treatment.
Discussion
Conservative treatment of impacted maxillary incisors unquestionably represents a significant clinical challenge, since it requires close collaboration between the orthodontist and the oral surgeon, not to mention skillful management of predominantly younger patients.11 Periodontal and orthodontic treatment of an impacted central incisor is especially sensitive because of its esthetic position. Careful soft-tissue management is required to ensure a good long-term esthetic outcome.12 It is important to inform the patient and parents clearly of the possibility of failure and the unpredictability of results before extensive measures are undertaken to save a severely impacted tooth.1 Even successfully treated patients may exhibit irregular root formation13 or an unesthetic gingival margin after alignment.14 Impaction of a permanent tooth is rarely diagnosed in the mixed dentition and is usually corrected during orthodontic treatment of the permanent dentition. The notable exception is the maxillary central incisors,15 which are typically diagnosed as impacted in the early mixed dentition, between ages 8 and 10.16
The first step in treatment of an impacted upper central incisor is to determine whether the tooth can be successfully aligned in its proper axial position, based on its location and orientation, amount of root formation, and degree of root dilaceration.13 It is important to plan when and how the impacted tooth will be moved, as determined by the positions of adjacent teeth and intermaxillary relationships. Another detail to consider is the placement of a temporary resin crown as soon as enough space has been created, followed by adjustments to the crown during orthodontic traction. In the case shown here, as soon as the temporary incisor crown was placed, the patient’s confidence and self-esteem improved dramatically.
In this case, orthodontic traction was carefully planned so that the orientation and intensity of the force vectors would enable gradual tooth movement, promoting esthetic gingival contours and minimizing root resorption. Apical resorption of the right central incisor’s dilacerated root provided a beneficial periodontal effect because it attenuated labial cortical bone fenestration. Cases of severe dilaceration may call for surgical endodontics, endodontic treatment, or apicoectomy procedures.17
Considering the high impaction of the maxillary right central incisor and its proximity to the upper labial frenulum, we decided not to excise a soft-tissue window and create an apically positioned flap, which would have risked gingival scarring and increased the clinical crown length.18,19 Any rotation of an impacted maxillary incisor should be corrected before guiding the impacted tooth into the occlusal plane, as was done here. Other factors contributing to the successful periodontal outcome included individualized lingual root torque, good quality of the gingival tissue, and patient compliance with oral hygiene.
It may sometimes be impossible to erupt an impacted central incisor orthodontically because of ankylosis and external root resorption.1 Alternative approaches might involve extraction of the impacted tooth followed by multidisciplinary treatment. Extraction of an impacted maxillary incisor should be considered a last resort, however, since the development and maintenance of the premaxilla depend on the development and eruption of the upper incisors.
ACKNOWLEDGMENT: The authors express their gratitude to Dr. Teresa Cristina Pereira de Oliveira for contributing to this manuscript. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior–Brasil (CAPES)– Finance Code 001.
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
- **Registered trademark of Dentsply Sirona Orthodontics Inc., Sarasota, FL; www.essix.com.
REFERENCES
- 1. Brand, A.; Akhavan, M.; Tong, H.; Kook, Y.A.; and Zernik, J.H.: Orthodontic, genetic, and periodontal considerations in the treatment of impacted maxillary central incisors: A study of twins, Am. J. Orthod. 117:68-74, 2000.
- 2. Fardi, A.; Kondylidou-Sidira, A.; Bachour, Z.; Parisis, N.; and Tsirlis, A.: Incidence of impacted and supernumerary teeth: A radiographic study in a North Greek population, Med. Oral Patol. Oral Cir. Bucal. 16:56-61, 2011.
- 3. Boorum, M.K. and Andreasen, J.O.: Sequelae of trauma to primary maxillary incisors, I: Complications in the primary dentition, Dent. Traumatol. 14:31-44, 1998.
- 4. Glendor, U.: Epidemiology of traumatic dental injuries: A 12 year review of the literature, Dent. Traumatol. 24:603-611, 2008.
- 5. Rocha, M.J. and Cardoso, M.: Survival analysis of endodontically treated traumatized primary teeth, Dent. Traumatol. 23:340-347, 2007.
- 6. Altun, C.; Cehreli, Z.C.; Güven, G.; and Acikel, C.: Traumatic intrusion of primary teeth and its effects on the permanent successors: A clinical follow-up study, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 107:493-498, 2009.
- 7. Andreasen, J.O.; Andreasen, F.M.; and Andersson, L.: Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed., Wiley-Blackwell, Hoboken, NJ, 2007.
- 8. Diab, M. and elBadrawy, H.: Intrusion injuries of primary incisors, Part III: Effects on the permanent successors, Quintess. Int. 31:377-384, 2000.
- 9. Lin, Y.T.J.: Treatment of an impacted dilacerated maxillary central incisor, Am. J. Orthod. 115:406-409, 1999.
- 10. Sant’Anna, E.F.; Marquezan, M.; and Sant’Anna, C.F.: Impacted incisors associated with supernumerary teeth treated with a modified Haas appliance, Am. J. Orthod. 142:863-871, 2012.
- 11. Chaushu, S.; Becker, T.; and Becker, A.: Impacted central incisors: Factors affecting prognosis and treatment duration, Am. J. Orthod. 147:355-362, 2015.
- 12. Chandhoke, T.K.; Agarwal, S.; Feldman, J.; Shah, R.A.; Upadhyay, M.; and Nanda, R.: An efficient biomechanical approach for the management of an impacted maxillary central incisor, Am. J. Orthod. 146:249-254, 2014.
- 13. Tanaka, E.; Hasegawa, T.; Hanaoka, K.; Yoneno, K.; Matsumoto, E.; Dalla-Bona, D.; Yamano, E.; Suekawa, Y.; Watanabe, M.; and Tanne, K.: Severe crowding and a dilacerated maxillary central incisor in an adolescent, Angle Orthod. 76:510-518, 2006.
- 14. Chaushu, S.; Brin, I.; Ben-Bassat, Y.; Zilberman, Y.; and Becker, A.: Periodontal status following surgical-orthodontic alignment of impacted central incisors with an open-eruption technique, Eur. J. Orthod. 25:579-584, 2003.
- 15. Becker, A.: Early treatment for impacted maxillary incisors, Am. J. Orthod. 121:586-587, 2002.
- 16. Crawford, L.B.: Impacted maxillary central incisor in mixed dentition treatment, Am. J. Orthod. 112:1-7, 1997.
- 17. McNamara, T.; Woolfe, S.N.; and McNamara, C.M.: Orthodontic management of a dilacerated maxillary central incisor with an unusual sequela, J. Clin. Orthod. 32:293-297, 1998.
- 18. Boyd, R.L.: Clinical assessment of injuries in orthodontic movement of impacted teeth, II: Surgical recommendations, Am. J. Orthod. 86:407-418, 1984.
- 19. Vanarsdall, R.L. and Corn, H.: Soft-tissue management of labially positioned unerupted teeth (July 1977), Am. J. Orthod. 125:284-293, 2004.











COMMENTS
.