CASE REPORT
Guided Eruption of Multiple Impacted Teeth Using a Modified Miniplate
The etiology of impaction is multifactorial1; causes may include genetic predisposition, mesiodens or multiple supernumerary teeth in the anterior maxillary region,2,3 odontogenic tumors such as odontomas or cysts,4-6 alterations in the eruption path or formation of scar tissue due to trauma or premature loss of the primary incisors,7,8 abnormal root angulation or dilacerations,9 and inadequate arch space. The frequency of maxillary incisor impaction ranges from .06% to .2%.10 Treatment is especially challenging not only because of a diverse pattern of impaction, but because these teeth are significant from an esthetic point of view.
In this case report, we describe a technique for the management of multiple impacted teeth obstructed by a supernumerary.
Diagnosis and Treatment Planning
An 11-year-old male presented with the chief complaint of an unerupted upper left canine and central and lateral incisors (Fig. 1).
Similar articles from the archive:
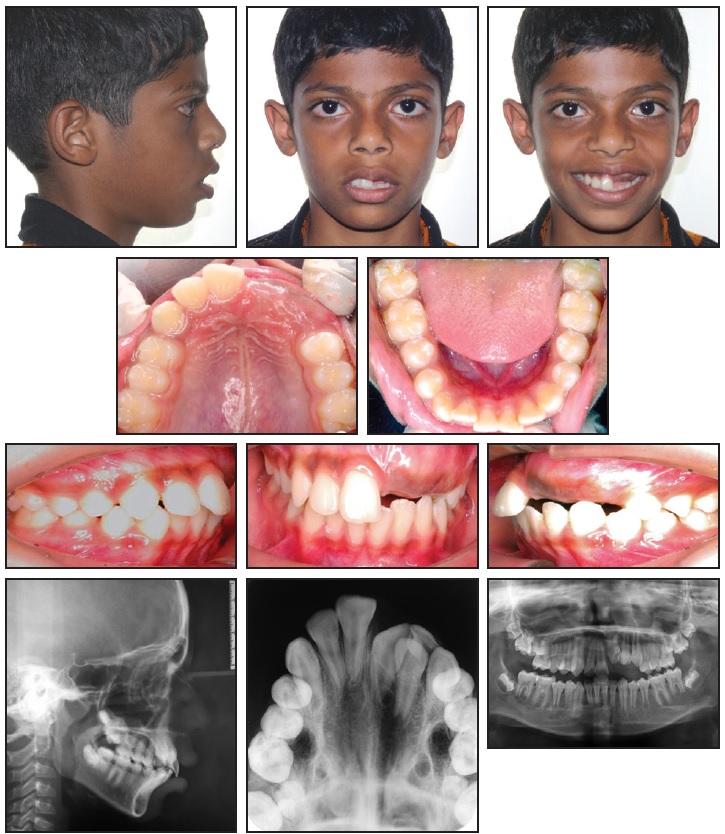
Fig. 1 11-year-old male patient with unerupted permanent upper left central and lateral incisors and canine, three impacted supernumerary teeth, shifted upper midline, and incompetent lips before treatment.
No history of trauma to the dental or facial region was reported, but the deciduous teeth had been extracted six years earlier due to caries. The patient had a symmetrical face and convex profile; the lips were incompetent, with an interlabial gap of 5mm. He was in the permanent dentition with Class I molar relationships on both sides and a Class I canine relationship on the right. The overjet was 4mm and the overbite 3mm, while the upper midline was shifted to the left by 2mm. We noted mild lower anterior crowding and supraeruption of the left lateral incisor and canine.
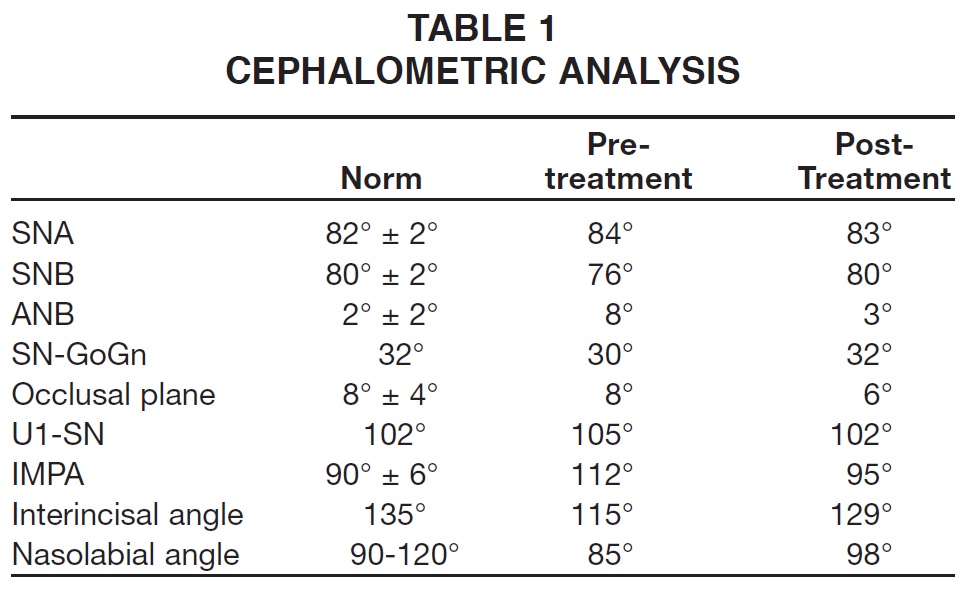
Radiographic evaluation confirmed the impaction of the three upper anterior teeth. Three impacted supernumerary teeth were also noted--one in the impacted anterior region and the other two between the upper first and second molars on each side. The impacted left central incisor was rotated. Cephalometric analysis showed a Class II skeletal pattern, with a normally inclined upper right central incisor and proclined lower incisors contributing to an acute interincisal angle (Table 1).
After the extraction of all supernumerary teeth and surgical exposure of the impacted upper left incisors and canine, we planned to use light orthodontic traction to bring these teeth into proper positions. The main treatment objectives were to provide adequate gingival attachment for the relocated teeth and symmetrical gingival margins while establishing an ideal overbite and overjet, a stable occlusion, and improved facial esthetics.
Two alternatives were considered for the impacted teeth. A "watch and wait" approach, after surgical flap repositioning, was not considered viable because the contralateral teeth had already erupted into the arch and there was inadequate space for natural eruption of the impacted teeth. The other option was to follow surgical exposure of the impacted teeth with orthodontic traction from temporary anchorage devices (TADs) in the opposing arch. A thorough survey of the literature indicated that miniplates had better stability (96%) compared to miniscrews (84- 86%).11-17 Although a miniplate system simplifies mechanics and reduces treatment time,16 however, it is more invasive and uncomfortable for the patient.
Potential benefits and risks of the treatment alternatives were explained to the patient and parents. The selected plan involved surgical exposure of the impacted teeth, followed by full fixed appliances with anchorage from a modified miniplate. After leveling and alignment, a space analysis would be performed before continuing treatment.
Treatment Progress
The three supernumerary teeth were extracted, and the impacted teeth were surgically exposed. After a full-thickness mucoperiosteal flap was raised for the central and lateral incisors, buttons were bonded to their labial surfaces for closed eruption. An apically repositioned flap was raised for the canine (Fig. 2A).
An "L"-shaped miniplate was modified by soldering it to an .035" stainless steel wire with hooks for attachment of elastics, then inserted into the lower anterior region below the root apices (Fig. 2B).17,18 An extrusive force of about 55g was applied to the incisors with 3/16" red elastics* (Fig. 2C). Six months later, when the teeth had erupted adequately, the upper and lower left anterior segments were bonded with .022" MBT**brackets and sectional wires were placed for alignment (Fig. 2D). Another 12 weeks later, elastic traction was added from the miniplate to the supraerupted lower left incisors and canine, applying an intrusive force of 15g (Fig. 2E).
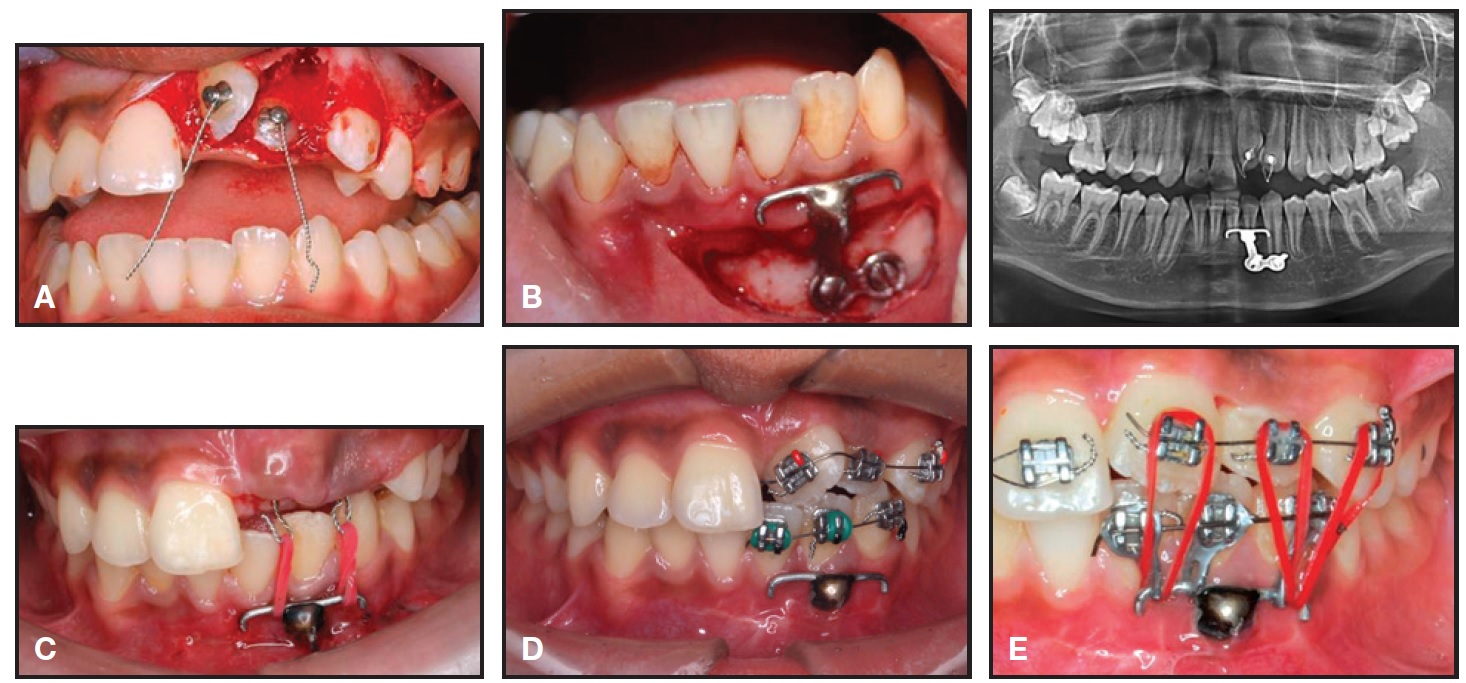
Fig. 2 A. Attachments bonded to surgically exposed incisors. B. Miniplate placed in lower anterior region below root apices. C. Traction of unerupted incisors using red elastics attached to “pigtail” hooks. D. After six months of traction and bonding of upper and lower left anterior teeth with sectional wires. E. Traction added to overerupted lower left incisors and canine.
After three more months of upper extrusion and lower intrusion, the remaining teeth were bonded to continue leveling and alignment. Twenty-four weeks later, records were taken and the patient was reevaluated to determine the remaining course of treatment (Fig. 3A). Based on cephalometric and clinical evaluation, all four first premolars were extracted (Fig. 3B). This was followed by retraction of the upper and lower anterior teeth (Fig. 3C) and the use of intermaxillary elastics for final settling (Fig. 3D). Overall active treatment time was 30 months.
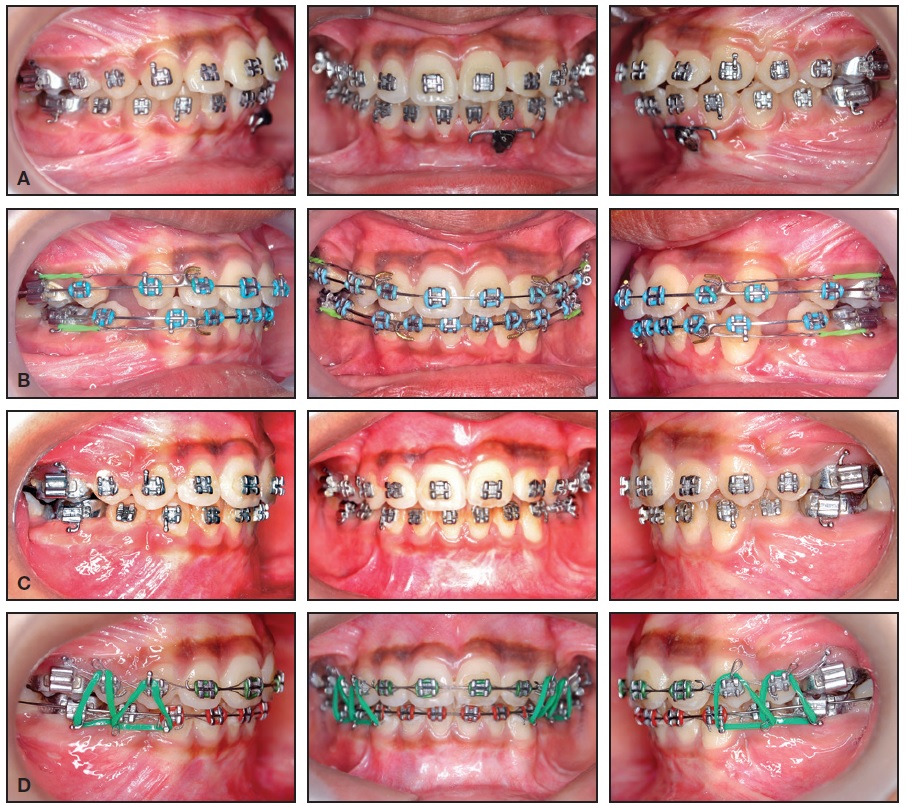
Fig. 3 A. Reevaluation after 12 months of traction. B. Three months later, next phase of treatment started after extraction of four first premolars. C. After six months of space closure. D. Intermaxillary elastics used in finishing stage.
Treatment Results
Ideal overbite and overjet relationships were established, with proper intercuspation and coincident upper and lower midlines (Fig. 4A). The final occlusion demonstrated proper interproximal contacts and root parallelism. Periodontal evaluation showed an acceptable gingival contour and adequate width of keratinized attached gingival tissue around the disimpacted teeth.
Superimposition of cephalometric tracings confirmed a consistent skeletal relationship and improved overjet and overbite, due to both treatment effects and favorable growth (Fig. 4B, Table 1).
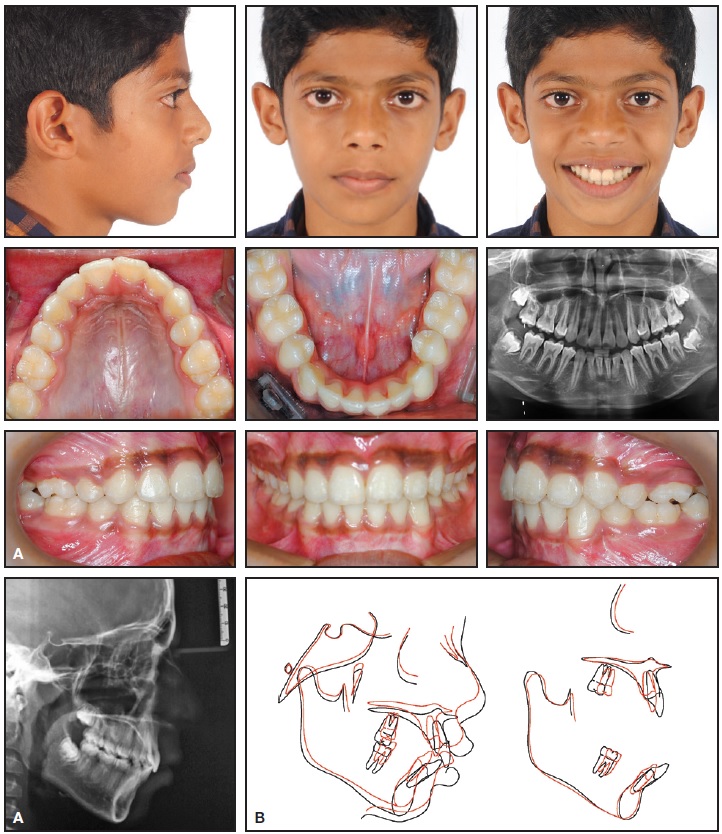
Fig. 4 A. Patient after 30 months of active treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
One year after orthodontic treatment, the occlusion and smile remained stable (Fig. 5).

Fig. 5 Patient one year after debonding.
Discussion
Multiple impaction is a rare occurrence, often associated with conditions such as cleidocranial dysplasia, Gardner syndrome, Down syndrome, or Aarskog syndrome.18 In the present case, apart from the multiple impactions of permanent and supernumerary teeth, no other disorder was diagnosed.
It is important to properly inform the patient and parents of the risks involved before extensive treatment is undertaken to save severely impacted teeth.19,20 A multidisciplinary approach will require close cooperation of the orthodontist, the oral surgeon, and sometimes the pedodontist and periodontist. As soon as the impaction is detected, treatment should be initiated to remove any obstacle in the physiologic eruptive path.21 This will often result in spontaneous eruption. If surgical exposure of the impacted teeth is necessary, the choice of an open-eruption or closed-eruption technique22-25 should be determined after the evaluation of esthetic and functional sequelae such as gingival attachment, height, width, and scarring.26,27 In the case shown here, closed eruption was chosen for the impacted central and lateral incisors to ensure adequate gingival tissue around the teeth; a partial-thickness flap was raised and repositioned apically at the canine to prevent marginal bone loss and gingival recession.
Miniplates can withstand heavier and more dynamic forces than orthodontic miniscrews can. Moreover, the soft-tissue thickness is not critical,16 and even root contact or proximity will have little impact on successful stabilization. Our modified "L"-shaped miniplate--with a soldered .035" stainless steel wire arm for attachment of elastics-- also had the advantage of versatility in the application of forces with different vectors and levels, so that an extrusive force could be applied to the upper anterior teeth and an intrusive force to the lower anterior teeth. Because the force was dissipated through the entire arm, the miniplate was taxed to a lesser degree. Engaging the impacted teeth with a sectional wire eliminated the risk of unwanted movement of the adjacent teeth. This design also allowed the patient to change elastics and facilitated oral hygiene. Careful monitoring and a multidisciplinary approach led to a successful esthetic result, with a healthy periodontium and a functional occlusion.
FOOTNOTES
- *TP Orthodontics, Inc., LaPorte, IN; www.tportho.com.
- **Trademark of 3M Unitek, Monrovia, CA; www.3Munitek.com.
REFERENCES
- 1. Kokich, V.G. and Mathews, D.P.: Surgical and orthodontic management of impacted teeth, Dent. Clin. N. Am. 37:181-204, 1993.
- 2. Giancotti, A.; Grazzini, F.; De Dominicis, F.; Romanini, G.; and Arcuri, C.: Multidisciplinary evaluation and clinical management of mesiodens, J. Clin. Pediat. Dent. 26:233-237, 2002.
- 3. Ibricevic, H.; Al-Mesad, S.; Mustagrudic, D.; and Al-Zohejry, N.: Supernumerary teeth causing impaction of permanent maxillary incisors, J. Clin. Pediat. Dent. 27:327-332, 2003.
- 4. Batra, P.; Duggal, R.; Kharbanda, O.P.; and Parkash, H.: Orthodontic treatment of impacted anterior teeth due to odontomas: A report of two cases, J. Clin. Pediat. Dent. 28:289-294, 2004.
- 5. Kamakura, S.; Matsui, K.; Katou, F.; Shirai, N.; Kochi, S.; and Motegi, G.: Surgical and orthodontic management of compound odontoma without removal of the impacted permanent tooth, Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 94:540-542, 2002.
- 6. Morning, P.: Impacted teeth in relation to odontomas, Int. J. Oral Surg. 9:81-91, 1980.
- 7. Andreasen, J.O.; Sundstrom, B.; and Ravn, J.J.: The effect of traumatic injuries to primary teeth on their permanent successors, I. A clinical and histologic study of 117 injured permanent teeth, Scand. J. Dent. Res. 79:219-283, 1971.
- 8. Andreasen, J.O. and Ravn, J.J.: The effect of traumatic injuries to primary teeth on their permanent successors, II. A clinical and radiographic follow-up study of 213 teeth, Scand. J. Dent. Res. 79:284-294, 1971.
- 9. Stewart, D.J.: Dilacerated unerupted maxillary central incisors, Br. Dent. J. 145:229-233, 1978.
- 10. Grover, P.S. and Lorton, L.: The incidence of unerupted permanent teeth and related clinical cases, Oral Surg. Oral Med. Oral Pathol. 59:420-425, 1985.
- 11. Lu, P.C.; Wang, C.H.; Wang, H.C.; Lee, K.T.; Lee, H.E.; and Chen, C.M.: A study of the mechanical strength of miniscrews and miniplates for skeletal anchorage, J. Dent. Sci. 6:165-169, 2011.
- 12. Leung, M.T.; Rabie, A.B.; and Wong, R.W.: Stability of connected miniimplants and miniplates for skeletal anchorage in orthodontics, Eur. J. Orthod. 30:483-489, 2008.
- 13. Lai, E.H.H.; Yao, C.C.J.; Chang, J.Z.C.; Chen, I.; and Chen, Y.J.: Threedimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: Comparison of head gear, miniscrew, and miniplate skeletal anchorage, Am. J. Orthod. 134:636- 645, 2008.
- 14. Choi, B.H.; Zhu, S.J.; and Kim, Y.H.: A clinical evaluation of titanium miniplates as anchors for orthodontic treatment, Am. J. Orthod. 128:382-384, 2005.
- 15. Cornelis, M.A.; Scheffler, N.R.; Nyssen-Behets, C.; De Clerck, H.J.; and Tulloch, J.F.: Patients'and orthodontists' perceptions of miniplates used for temporary skeletal anchorage: A prospective study, Am. J. Orthod. 133:18-24, 2008.
- 16. Lee, S.J.; Lin, L.; Kim, S.H.; Chung, K.R.; and Donatelli, R.E.: Survival analysis of a miniplate and tube device designed to provide skeletal anchorage, Am. J. Orthod. 144:349-356, 2013.
- 17. Chung, K.R.; Jeong, D.M.; Kim, S.H.; Ko, Y.I.; and Nelson, G.: En-masse retraction dependent on a temporary skeletal anchorage device without posterior bonding or banding in an adult with severe bidentoalveolar protrusion: Seven years post treatment, Am. J. Orthod. 141:484-494, 2012.
- 18. Yalcin, S. and Gurbuzer, B.: Multiple impacted teeth in the maxilla, Oral Surg. Oral Med. Oral Pathol. 76:130, 1993.
- 19. Kolokitha, O.E. and Papadopoulou, A.K.: Impaction and apical root angulation of the maxillary central incisors due to supernumerary teeth: Combined surgical and orthodontic treatment, Am. J. Orthod. 134:153-160, 2008.
- 20. Pinho, T.; Neves, M.; and Alves, C.: Impacted maxillary central incisor: Surgical exposure and orthodontic treatment, Am. J. Orthod. 140:256-265, 2011.
- 21. Becker, A.: Early treatment for impacted maxillary incisors, Am. J. Orthod. 121:586-587, 2002.
- 22. Becker, A.; Brin, I.; Ben-Bassat, Y.; Zilberman, Y.; and Chaushu, S.: Closed-eruption surgical technique for impacted maxillary incisors: A postorthodontic periodontal evaluation, Am. J. Orthod. 122:9-14, 2002.
- 23. Chaushu, G.; Becker, A.; Zeltser, R.; Branski, S.; and Chaushu, S.: Patients' perception of recovery after surgical exposure of impacted teeth treated with a closed eruption surgical-orthodontic technique, Am. J. Orthod. 125:690- 696, 2004.
- 24. Chaushu, S.; Becker, A.; Zeltser, R.; Vasker, N.; and Chaushu, G.: Patients' perception of recovery after surgical exposure of impacted maxillary teeth treated with an open-eruption surgicalorthodontic technique, Eur. J. Orthod. 26:591-596, 2004.
- 25. Chaushu, S.; Becker, A.; Zeltser, R.; Branski, S.; Vasker, N.; and Chaushu, G.: Patients' perception of recovery after exposure of impacted teeth: A comparison of closed- versus open-eruption techniques, J. Oral Maxillofac. Surg. 63:323-359, 2005.
- 26. Brand, A.; Akhavan, M.; Tong, H.; Kook, Y.A.; and Zernik, J.H.: Orthodontic, genetic, and periodontal considerations in the treatment of impacted maxillary central incisors: A study of twins, Am. J. Orthod. 117:68-74, 2000.
- 27. Vanarsdall, R.L. and Corn, H.: Softtissue management of labially positioned unerupted teeth, Am. J. Orthod. 72:53-64, 1977.