Digital Lab Appliances: The Time Has Come
Intraoral scanners are widely used today, and virtual models have replaced plaster casts in most orthodontic offices.1 Pretreatment scans can now be stored in the cloud. Most clinicians transmit digital models to their preferred clear-aligner provider, whether it’s a well-known firm or an in-house lab. Nevertheless, only a minority use digital scans for indirect bonding2 or for fixed retainers.3 Digital versions of traditional laboratory-
produced appliances are rarely presented in the literature, and when they are, they are labeled as experimental.4-6 When it comes to these appliances, most orthodontists stick to their old habits and rely on alginate impressions.
There is a vast unexploited potential in digital orthodontics. The way an average doctor uses a scanner is analogous to using a smartphone with a few basic apps. As orthodontists, we need to explore all our options for customized services and determine which will work best for our practices. It is a waste of resources to own a scanner and not use it for every step of orthodontic therapy, from interceptive treatment through retention.
This article provides an overview of current digital possibilities, with special attention to laboratory-made appliances.
Digital Bands
We use Ortho System* software for our digital design procedures. Many computer-aided design and manufacturing (CAD/CAM) software platforms are available, however, and each orthodontist or laboratory should choose programs according to their preferences. Considerations include user-friendliness of the design protocols, time involved in preparing the digital setups, and prices (annual fees or one-time purchases).
A digital band—the mainstay of lab-produced digital appliances—can be easily designed by contouring it to the edges of the tooth where it will be placed (Fig. 1). This may take as long as five minutes, depending on the complexity of the structure. We recommend a thickness of .6-.7mm (.024"-.028"). The band can be designed to extend to adjacent teeth in the form of a band, pad, or wire, according to the situation.
When the design is completed, it is usually sent to a laser-sintering6 or laser-melting center. The price of outsourced bands is reasonable, while the cost of these three-dimensional printers remains prohibitive for in-house production. Laser sintering and laser melting have different effects on the properties of the metal that must be taken into account. For example, laser-sintered metal should not be bent; even though it is strong and resistant, it is also brittle and prone to breakage because it is composed of melted powder. The band (or the “island” if it includes more than one tooth) is returned from the lab with a rough surface that needs to be polished on the side exposed to the mouth and sandblasted on the inner surface to enhance microretention.
Since digital bands do not extend between the contact points, they eliminate the need for preliminary separator elastics. This is a key advantage, considering that most patients perceive separators as the most painful aspect of orthodontic treatment.7 Digital bands also save money for the practice; because each band is custom-made on demand, different sizes do not have to be kept in inventory.
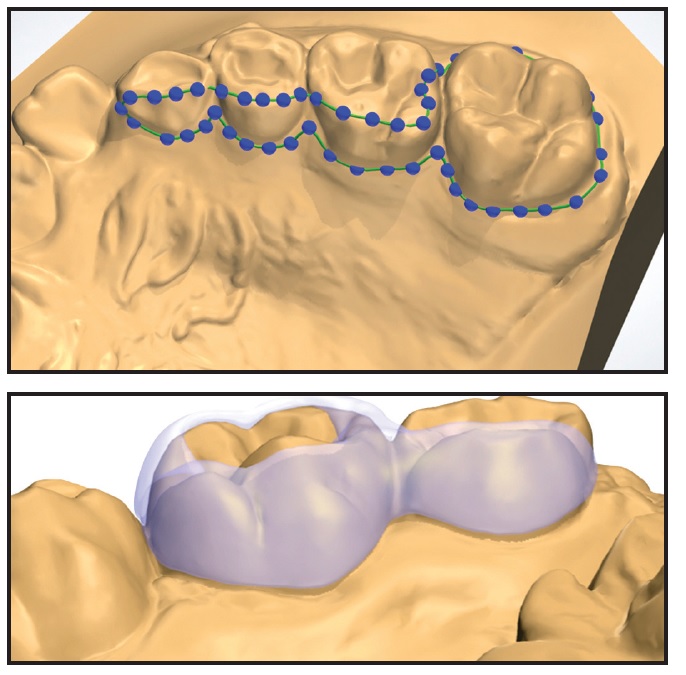
Fig. 1 A. Digital bands contoured to tooth surfaces. B. Pad extended to adjacent tooth.
The digital band does offer less mechanical retention than a traditional band. Any undercuts should be cleaned or filled by the technician before drawing the structure; otherwise, the band won’t fit because of its limited elasticity. The orthodontist can easily overcome this limitation by etching the enamel surface as required by the appliance design—generally for 30 seconds (or more for deciduous teeth) on the lingual side. A thin layer of cement (we prefer Transbond Plus** Light Cure Band Adhesive) is applied on the inner surface of the band, with no need for intermediate bonding agents. The appliance is then seated over the tooth surfaces, using only enough pressure to squeeze out the excess cement. Cotton swabs or cotton rolls can be used to remove the gross excess, and small tips, such as those used for bonding, to remove cement from the buccal grooves.
For easy removal, grab the gingival part of the band with a conventional band-removing plier. Squeeze the plier until you hear a sound indicating that the tooth-adhesive interface has been broken. Apply the same pressure on the lingual and buccal surfaces of each band until all surfaces except one are free, then apply a slightly stronger pressure on the last surface for appliance removal.
Removal of digital bands is generally easier and less painful for the patient than removal of conventional bands.
If the digital band is connected to pads extending over the lingual or buccal surfaces (not surrounding the entire tooth), it is generally not necessary to apply pressure to the pads. They will easily debond when pressure is applied to the main band. A typical example is a rapid maxillary expander (RME) with metallic islands. In an unusual case requiring multiple bands, a crown-cutting bur should be used to weaken or directly cut the connection between bands; otherwise, it would be extremely painful for the patient when multiple full bands are removed.
Unlike a traditional band, a digital band cannot extend under the gingival margin, which makes gingival inflammation less likely. Some questions have arisen about caries susceptibility because the band does not extend into the contact point. After delivering more than 800 digital appliances, we have not noticed an increased incidence of caries, and we have seen much less gingivitis.
Digital Fixed Appliances
Some types of appliances have to be fit on 3D-printed acrylic models. Although this approach is not as ecologically conservative, it is required for precise soldering of traditional metal components, such as active wires that need to be bent manually and laser-melted to two different islands. For fabrication of an RME—perhaps the most common digitally produced appliance—the islands with arms can be soldered directly to the screw (Fig. 2).
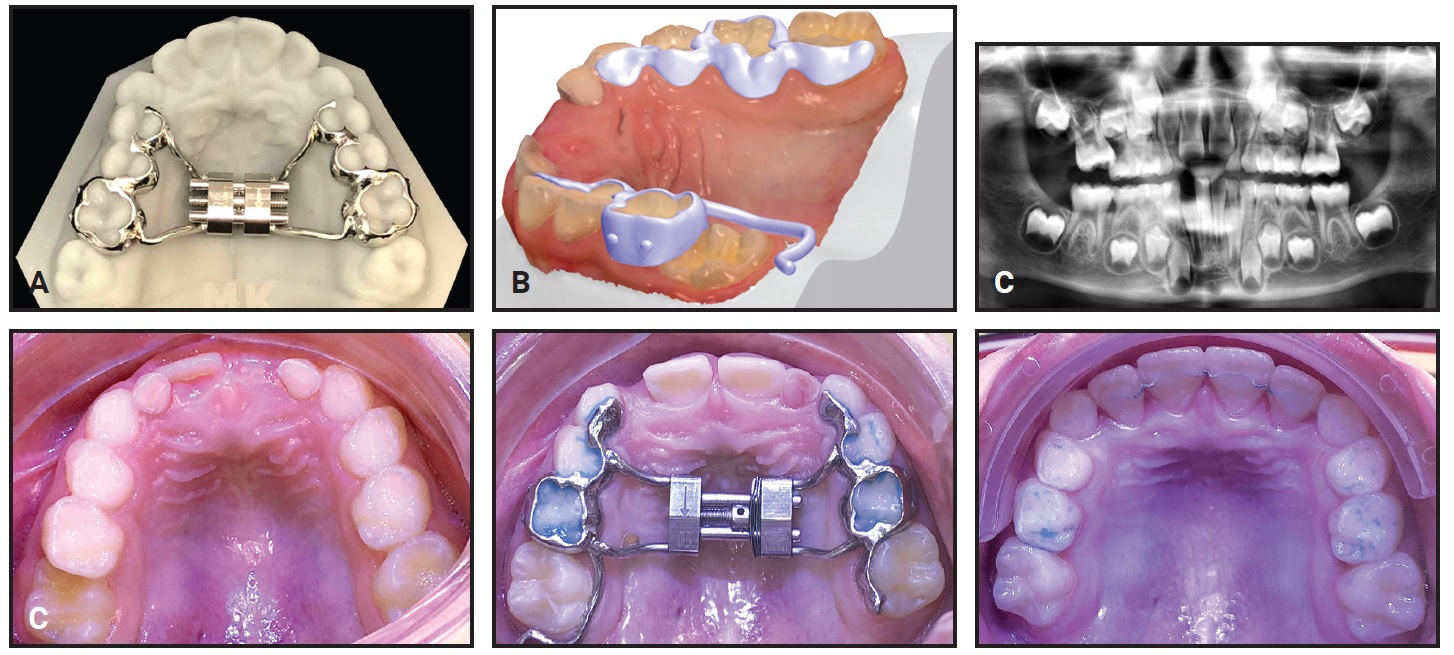
Fig. 2 A. Rapid maxillary expander (RME) connected to digitally designed “islands.” B. Modified Hyrax-Halterman RME design for de-impacting upper first molars. Small points on buccal side allow easier debonding. C. Modified RME design used in 7-year-old male patient to de-impact upper right first molar in 12 months.
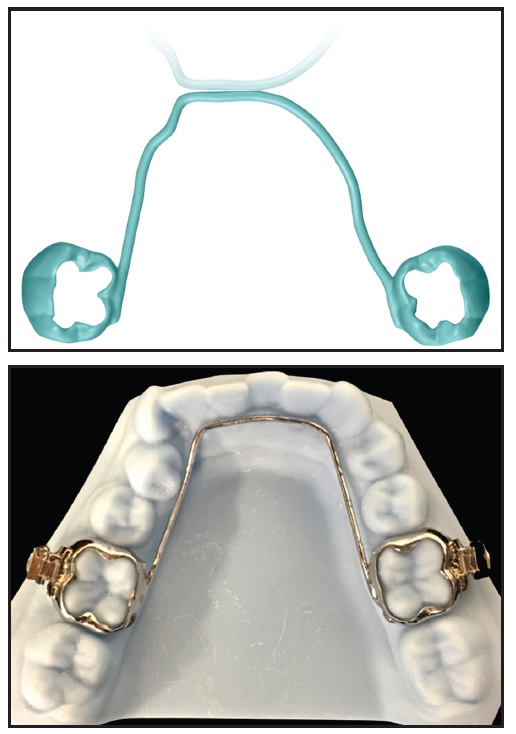
Fig. 3 Fully digital lingual arch (traditional tubes can be laser-soldered if needed).
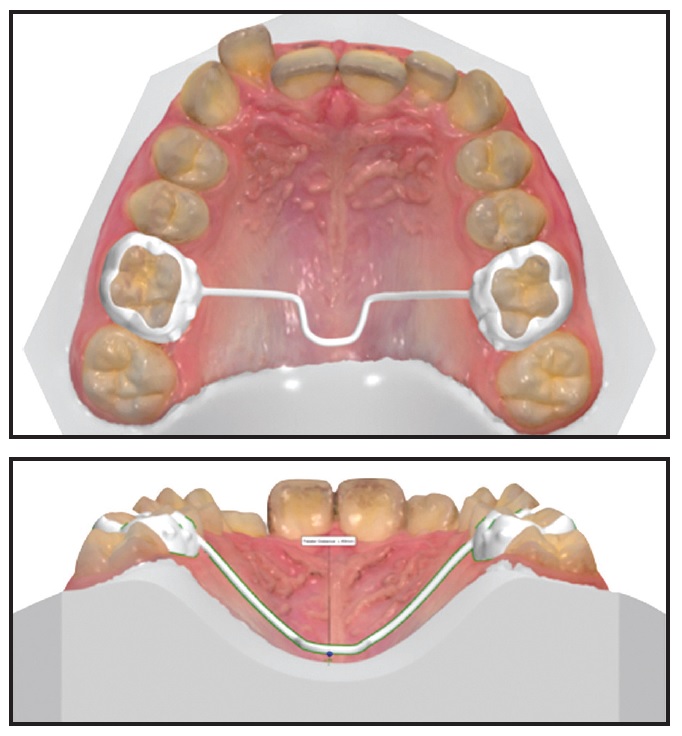
Fig. 5 Transpalatal arch (if fully digitally designed, cannot be activated and must be used passively).
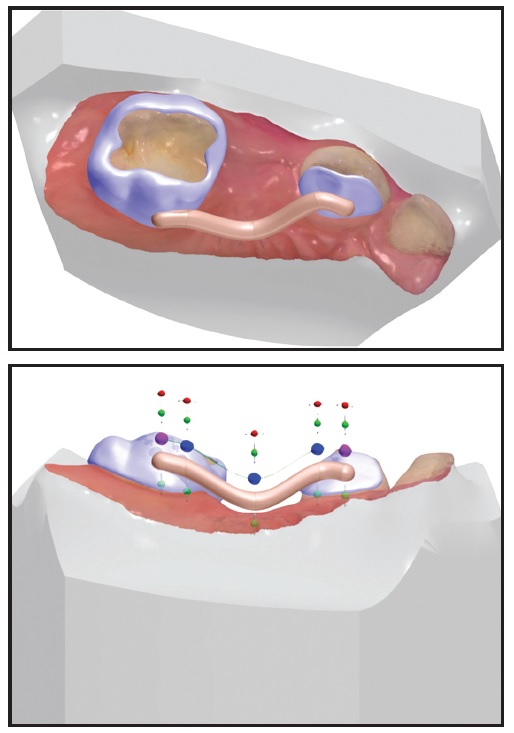
Fig. 4 Limited scan taken on young child to produce sectional space holder.
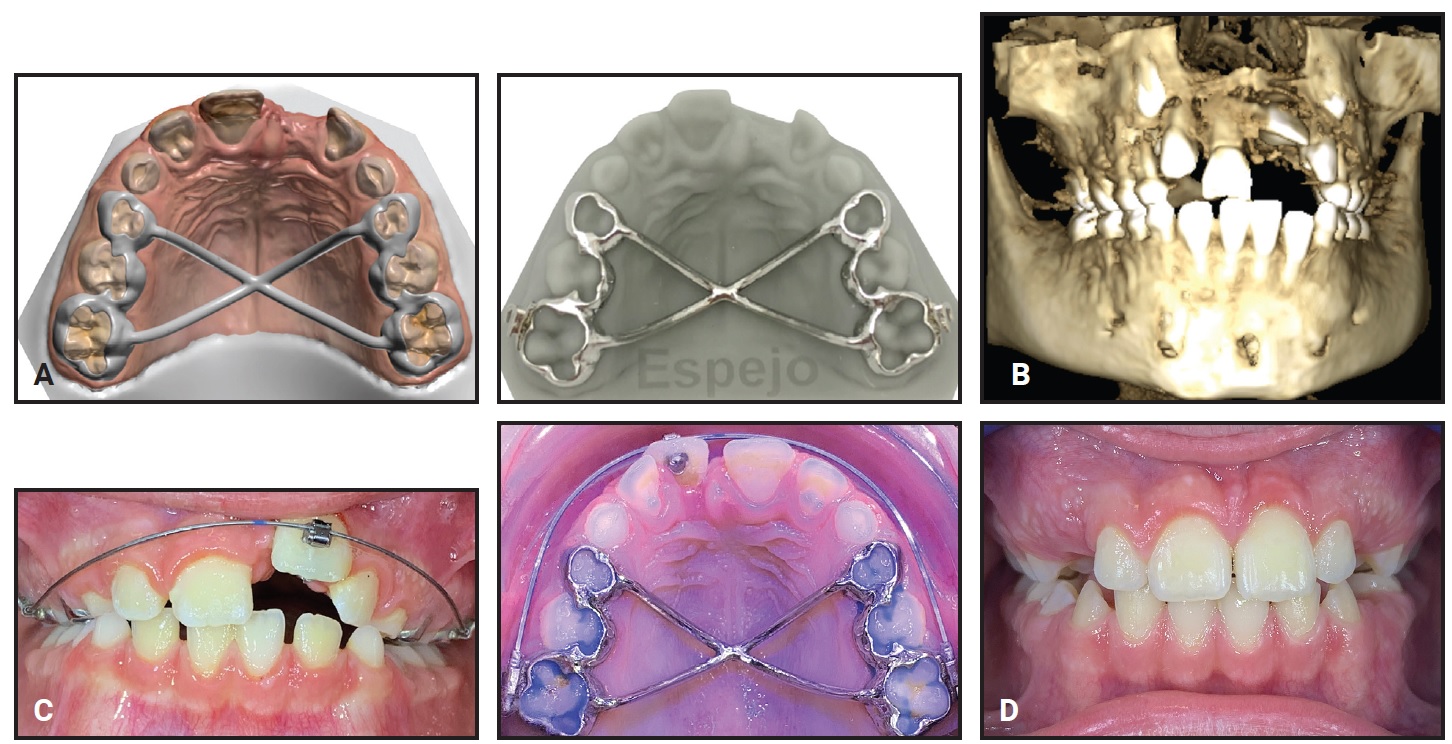
Fig. 6 A. Iron Cross palatal structure for strong anchorage. B. 8-year-old male patient with impacted upper left central incisor. C. Eruption guided by .018" × .025" nickel titanium archwire, anchored by digitally produced Iron Cross. D. After 15 months of treatment.
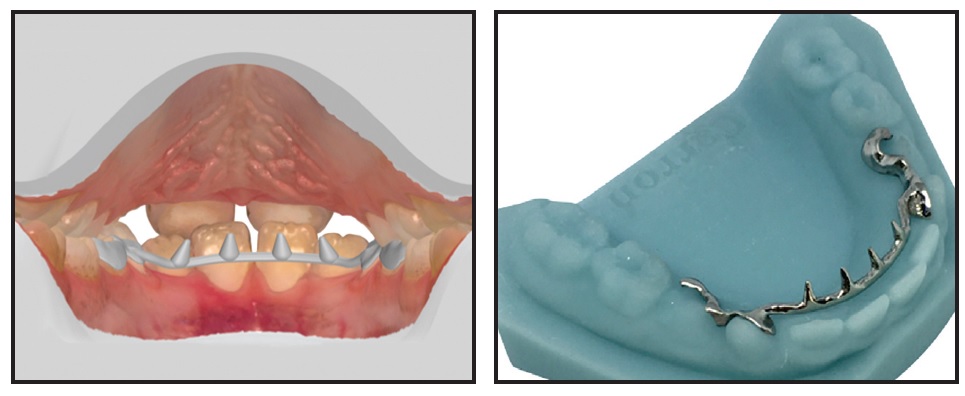
Fig. 7 Customized lingual tongue spurs used to correct tongue-thrust habit.
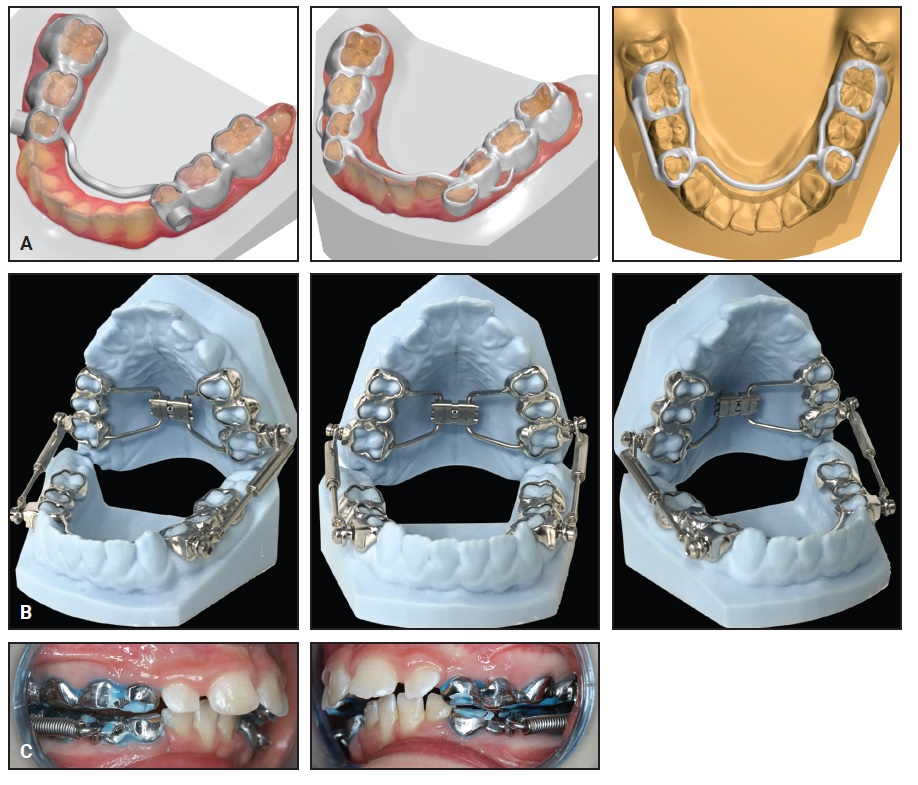
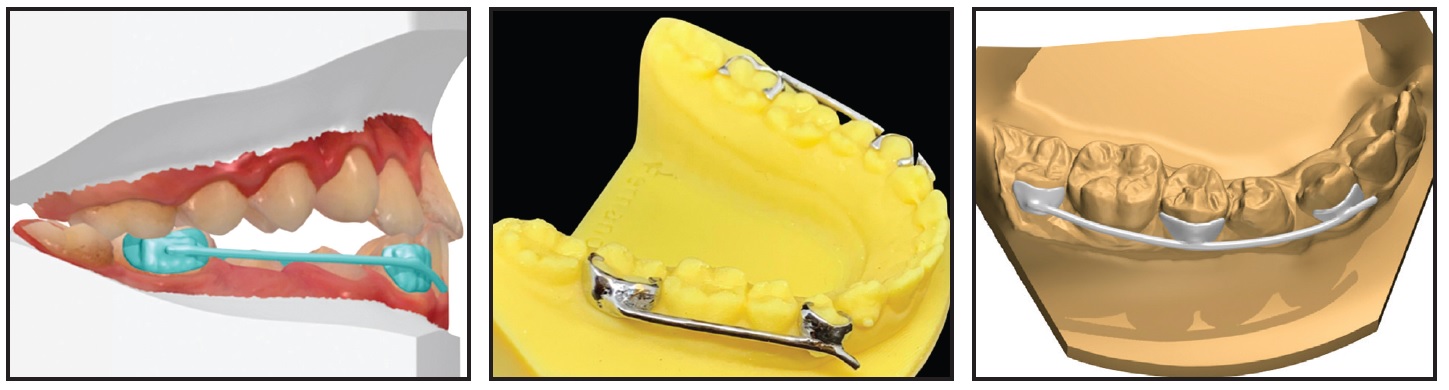
Fig. 9 Customized Class III appliance (based on Carriere Motion† appliance) designed with or without intermediate pad, depending on clinical need.
Digital Removable Appliances
The most common removable appliances are vacuformed retainers. An acrylic model is still needed to form a plastic retainer or aligner, but the 3D printing industry is working on a process for printing plastic of the same quality without the need for thermoforming.
Functional appliances can also be made from digital models. Bite registration in an advanced mandibular position allows the technician to employ a natural articulator—the patient’s maxillomandibular relationship. A wax mini-jig can be fitted to the incisors to register the bite in a forward position. The scanner is used to record the occlusion of the molars and premolars, and the software will then couple the arches in the therapeutic bite-jumping position. The technician uses this position to virtually design the acrylic structure, according to the clinician’s instructions. The scanner’s bite registration is so precise that little or no adaptation is required during appliance delivery.
If Adams clasps, labial arches, or other features are needed, appropriate holes are set into the acrylic structure (Fig. 10).
Acrylic can be 3D-printed, but milling is a good alternative for fabricating these appliances. After milling, the acrylic will have a matte finish and must be polished to become clear.
Michigan splints can also be produced with the highest precision (Fig. 11). The clinician can choose to leave a flat surface for the opposing arch or incorporate indentations to enhance mandibular stability during sliding movements.
Tongue educators for dynamic lingual training can be digitally designed and fabricated by 3D printing (Fig. 12). Digital versions of traditional tongue positioners, such as the Enveloppe Linguale Nocturne,†† are designed to adhere to the palatal vault by suction.
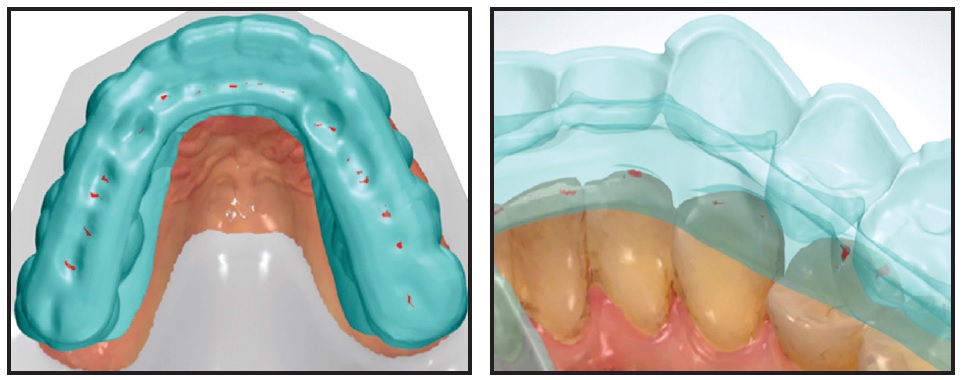
Fig. 11 Digitally designed Michigan splint (with indentations), requiring no adaptation in mouth.

Fig. 12 E-Tongue educator (digital version of Enveloppe Linguale Nocturne††) adheres to palate by suction. (Photo courtesy of NutisLab, Biarritz, France.)
Discussion
We all need to become aware of the possibilities of implementing laboratory appliance production into our digital workflows. In much the same way that some orthodontists now present themselves as Digital Smile Designers, the orthodontic technician will soon evolve into a Lab Designer.
The impact of technology in the laboratory will be disruptive. Fewer people may be needed to perform the same amount of work, since an expert technician can design a band or an island in five minutes or less. On the other hand, a plaster-free profession will produce less pollution and thus will have a positive impact on the environment.
If 3D printing technology continues to evolve rapidly and U.S. Food and Drug Administration approval keeps pace, every orthodontic office may soon have its own 3D printer remotely connected with the appliance designer. After approval of the design, the technician will be able to launch production from a remote location, and same-day appliance delivery—as is now possible with immediately loaded mini-implants8—will be a reality.
FOOTNOTES
- *Trademark of 3Shape, Copenhagen, Denmark; www.3shape.com.
- **Trademark of 3M, Monrovia, CA; www.3M.com.
- ***Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- †Registered trademark of Henry Schein Orthodontics, Melville, NY; www.henryscheinortho.com.
- ‡Trademark of Protec Dental Laboratories Ltd., Vancouver, BC, Canada; www.protecdental.com.
- ††Registered trademark of NutisLab, Biarritz, France; www.nutislab.com.
REFERENCES
- 1. Keim, R.G.; Gottlieb, E.L.; Vogels, D.S. III; and Vogels, P.B.: 2015 JCO Orthodontic Practice Study, Part 1: Trends, 49:625-639, 2015.
- 2. Breuning, K.H.: Efficient tooth movement with new technologies for customized treatment, J. Clin. Orthod. 45:257-262, 2011.
- 3. Kravitz, N.D.; Grauer, D.; Schumacher, P.; and Yong-Min, J.: Memotain: A CAD/CAM nickel-titanium lingual retainer, Am. J. Orthod. 151:812-885, 2017.
- 4. Farronato, G.; Santamaria, G.; Cressoni, P.; Falzone, D.; and Colombo, M.: The digital-titanium Herbst, J. Clin. Orthod. 45:263-267, 2011.
- 5. Graf, S.; Cornelis, M.A.; Hauber Gameiro, G.; and Cattaneo, P.M.: Computer-aided design and manufacture of Hyrax devices: Can we really go digital? Am. J. Orthod. 152:870-874, 2017.
- 6. Graf, S.; Vasudavan, S.; and Wilmes, B.: CAD-CAM design and 3-dimensional printing of mini-implant retained orthodontic appliances, Am. J. Orthod. 154:877-882, 2018.
- 7. Pal Singh Sandhu, G.; Kanase, A.; Naik, C.; Pupneja, P.; and Sudan, S.: Separation effect and perception of pain and discomfort from three types of orthodontic separators, J. Ind. Orthod. Soc. 47:6-9, 2013.
- 8. Maino, B.G.; Paoletto, E.; Lombardo, L.; and Siciliani, G.: From planning to delivery of a bone-borne rapid maxillary expander in one visit, J. Clin. Orthod. 51:198-207, 2017.





COMMENTS
.