Treatment of Snoring and Sleep Apnea with a Tongue Rehabilitation Device
Sleep is an essential physiological condition for vital bodily functioning. The two distinct types of sleep are non-rapid eye movement (NREM), which accounts for about two-thirds of sleep time over the course of the night, and rapid eye movement (REM), which makes up the remaining one-third. The stages of sleep occur in four to six cycles per night, with an average of 70-120 minutes per cycle.1-3
Snoring is a low-frequency, predominantly inspiratory noise caused by soft-tissue vibration in the pharynx during breathing.4 The prevalence ranges from 5% to 50% of the general population, increasing with age.2,5 Snoring may be a sign of other more serious respiratory sleep disorders, including apnea,6 and is the most common symptom of obstructive sleep apnea (OSA) syndrome, being present in nearly all cases.
OSA is characterized by recurring upper airway obstruction lasting about 10 seconds and occurring at least five to 10 times per hour of sleep.[ref]7-9[/ref] The American Academy of Sleep Medicine (AASM) classifies apneas as central, obstructive, or mixed. Risk factors include obesity, alcohol consumption, smoking, maxillofacial anomalies, enlarged tonsils, macroglossia, and sedative use.10,11
Nighttime OSA symptoms are resuscitative snoring, frequent awakening, pauses in breathing, suffocation, nocturia, excessive sweating, nightmares, insomnia, heartburn, regurgitation, and gagging. Daytime symptoms include excessive sleepiness, fatigue, non-restorative sleep, morning headaches, mood changes, difficulty in concentration, memory changes, and low libido.2,8,12,13
The physiopathology of OSA is related to airway obstruction, generally between the soft palate and epiglottis, and is also a function of negative diaphragmatic pressure.14 Assessment of genioglossus muscle activity at the onset of sleep shows that patients with OSA experience a far greater decline in activity, which may be associated with significantly reduced electromyographic activity and represent a loss of neuromuscular compensation during sleep. Even in non-symptomatic individuals, the geniohyoid muscle plays an important role in terms of upper airway strength and modulation of airway permeability.15
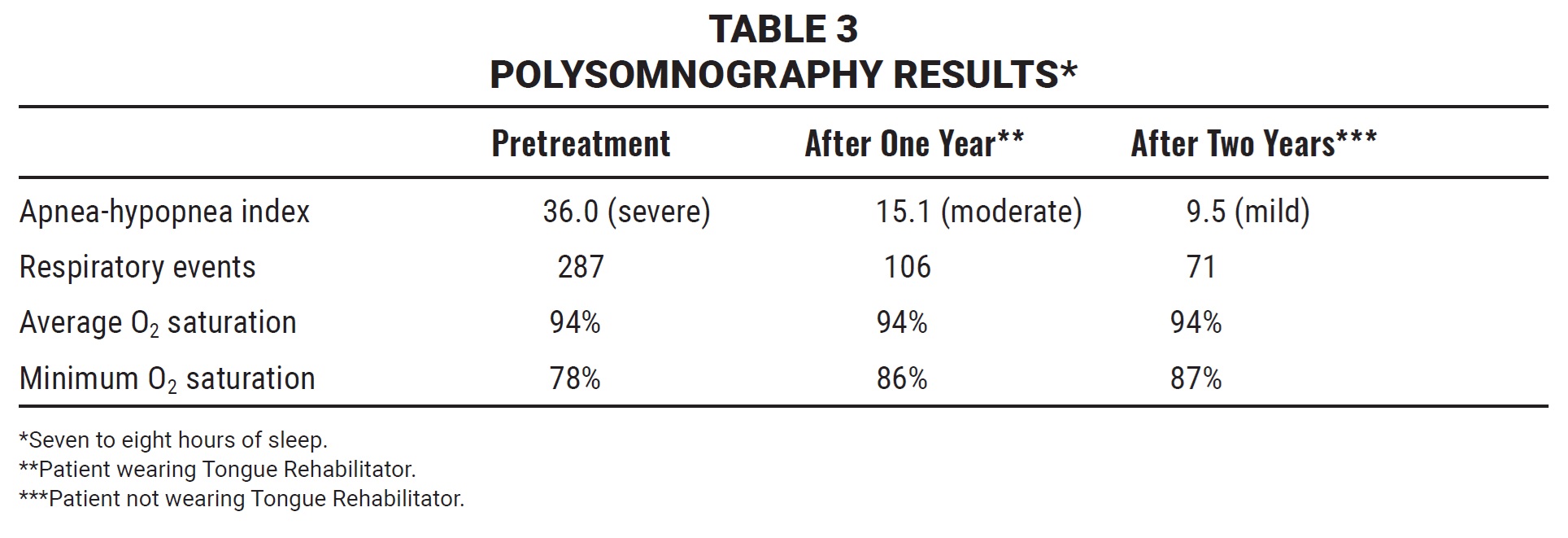
To evaluate for predisposition to OSA, an orthodontist should consider the patient’s Friedman classification, modified Mallampati score, Angle classification, oral cavity anatomy, questionnaire responses, and cephalometric analysis.12,16-18 In addition, an accurate diagnosis and assessment of severity will require a polysomnography test to measure the frequency of reduced airflow and number of obstructive events per hour of sleep.2,18 The AASM classifies OSA using the apnea-hypopnea index (AHI): the mild form involves five to 15 apneas or hypopneas per hour of sleep; moderate, 15-30; and severe, more than 30.19
Interdisciplinary treatment of OSA can incorporate intraoral devices, continuous positive airway pressure (CPAP), behavioral measures, or orthognathic surgery. The goals are to eliminate the obstruction of respiratory events and restore normal sleep patterns and arterial oxygenation, with the fewest possible risks and adverse side effects.12
Intraoral Appliances
Intraoral devices are indicated for treatment of patients with primary snoring and mild or moderate apnea and for some with more severe sleep disturbances who are intolerant of CPAP or refuse orthognathic surgery.13 Contraindications include severe TMD, active periodontal disease, predominantly central sleep apnea, extensive use of prostheses, lack of motivation, and a tendency to nausea or vomiting.9,12,20
The theoretical basis of these appliances is that gravity causes all tissue—including the tongue and jaw—to fall posteriorly when the patient lies in a supine position. Several intraoral devices work by opening the upper airway during sleep, often by repositioning the tongue, soft palate, or other anatomical parts that may be causing the obstruction.21 Repositioning and stabilizing the jaw and hyoid bone more anteriorly help avoid soft-tissue collapse during sleep. The concomitant increase in genioglossus muscle activity also inhibits relaxation of the tongue muscles.22
Mandibular advancement devices are designed to push the jaw forward and thus increase upper airway volume during sleep. Since this mechanism can also lead to patient discomfort,2,20,23-25 the objective is to achieve maximum results with minimum advancement.26 Mandibular advancers are widely used in OSA treatment, but few studies have been conducted to determine whether they may induce changes in occlusion, neuromuscular balance, or facial patterns, particularly when used for long periods.3
This article introduces the Tongue Rehabilitator,* an appliance designed for orthodontic patients with snoring habits, sleep apnea, or open bites caused by lingual interposition. Unlike conventional devices that move the jaw forward, the Tongue Rehabilitator’s mechanism of action is based on raising the tongue and directing it to a physiological position, thereby strengthening it enough to enable a full lip seal (first valve). Tongue-to-palate contact (second valve) promotes opening of the oropharynx in a latero-lateral direction, and the tongue base then activates the third valve by initiating contact with the soft palate.
The device is made from .032" or .036" stainless steel wire, folded in the shape of a heart and attached to an acrylic palatal plate (Fig. 1).

Fig. 1 Tongue Rehabilitator* fabricated from .032" stainless steel wire.
It is placed sublingually to activate the genioglossus muscle and act as an orthosis during speech or swallowing, thus stimulating the intrinsic and extrinsic tongue muscles as well as the adjacent mucosa and glands. The Tongue Rehabilitator changes the muscle tone of the tongue, placing it in a more anterior and physiological position for its natural functions of swallowing and speaking while allowing normal arch growth (Fig. 2).
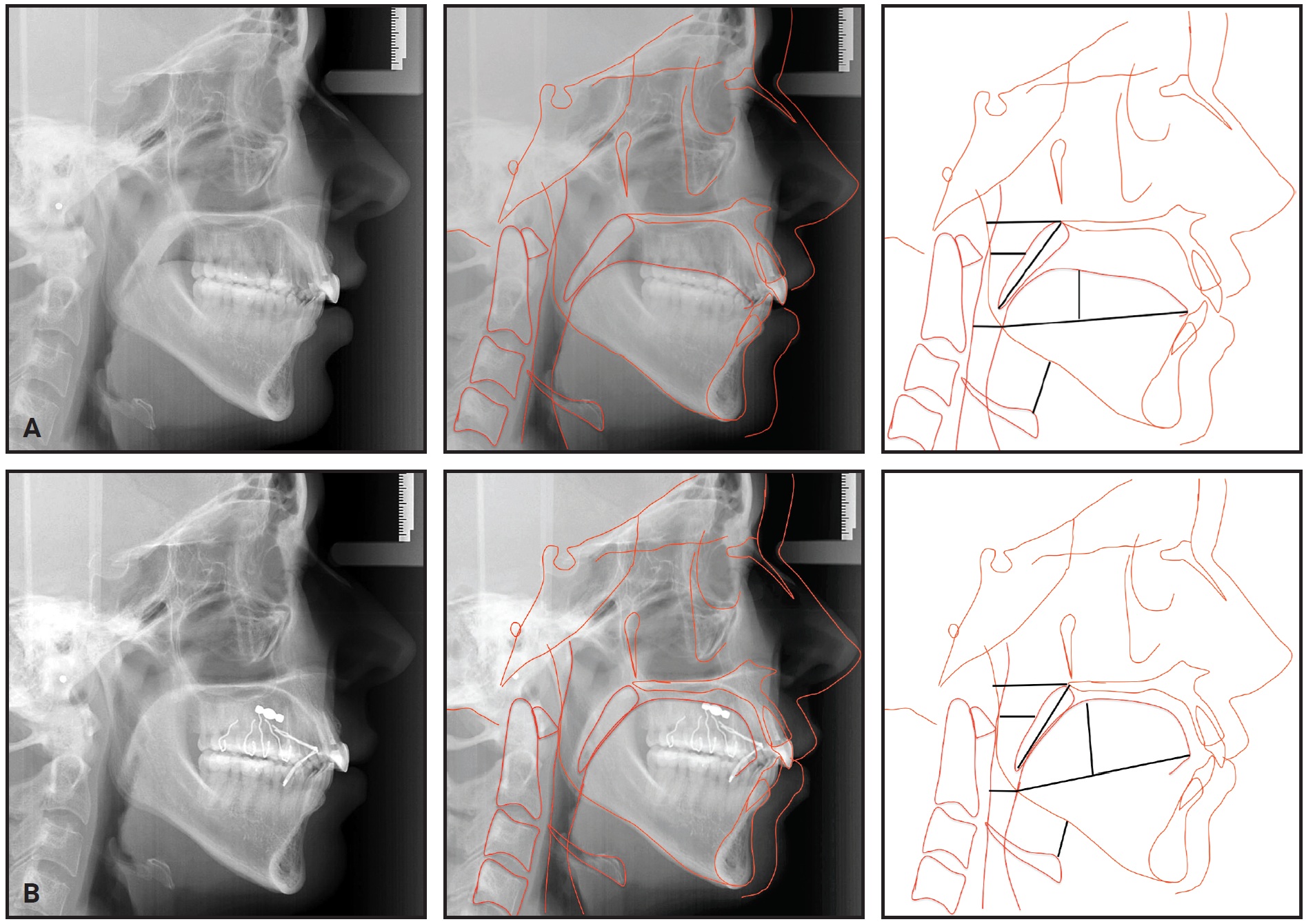
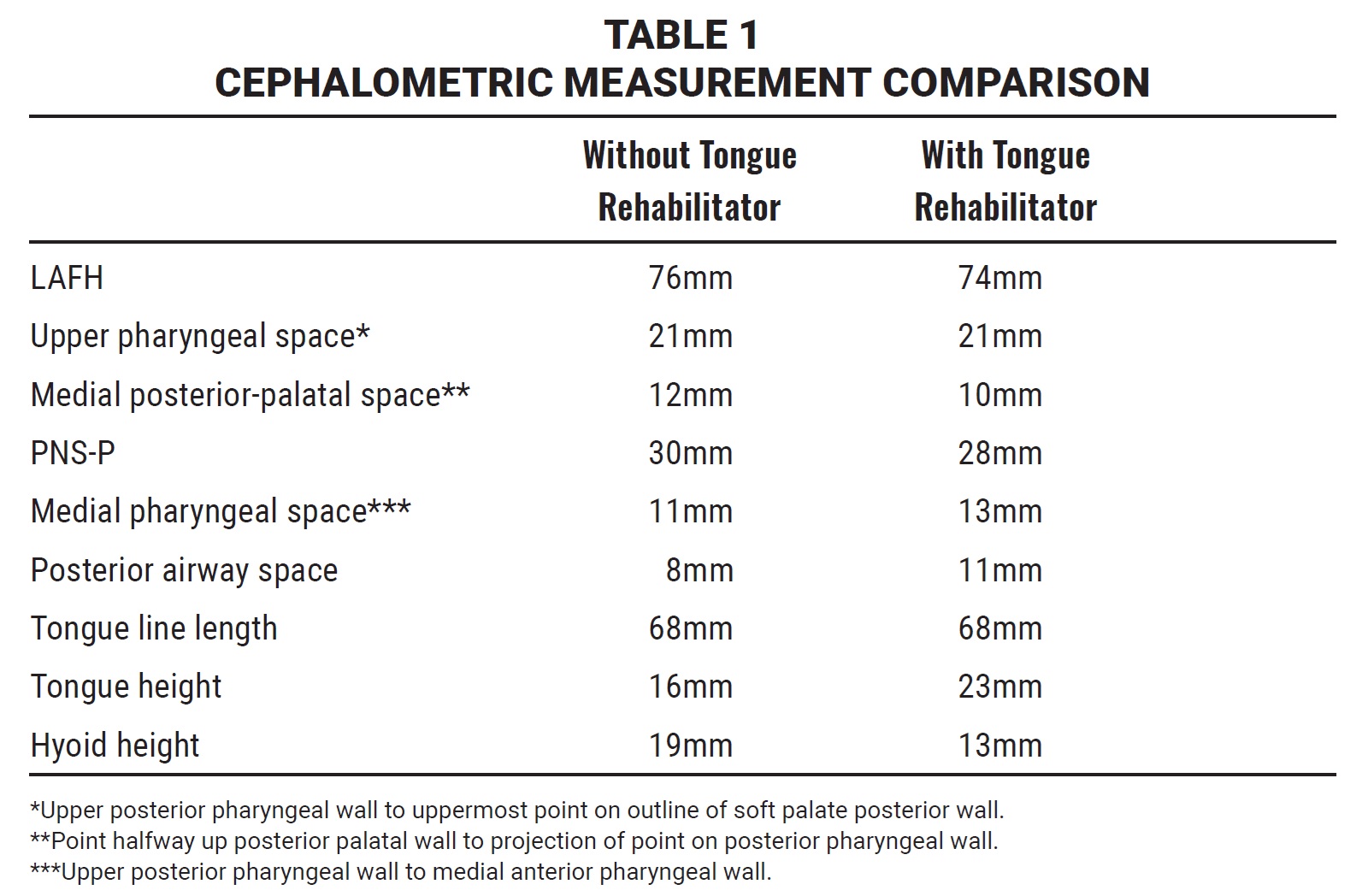
Fig. 2 38-year-old female patient without (A) and with (B) Tongue Rehabilitator in position.
In the patient shown here, with the appliance in place, the tongue was 7mm higher, the hyoid was 6mm lower, and the soft palate (PNS-P) was 2mm shorter ([table=1][Table 1[/table]). Projecting the tongue forward and upward promotes lip seal during swallowing, which helps open the posterior airway and reduce snoring to foster restorative sleep.
Case Report
A 49-year-old male sought treatment to improve tooth positioning for subsequent prosthetic rehabilitation (Fig. 3).

Fig. 3 49-year-old male patient with skeletal Class III malocclusion and history of snoring and breathing cessation during sleep.
He complained of snoring problems and stoppages of breathing during sleep. Clinical examination indicated a dolichocephalic pattern with adequate lip seal and a skeletal Class III malocclusion due to maxillary retrusion. The patient had a Class III subdivision left canine relationship (Table 2), a distally rotated upper right first premolar, and a missing upper right second premolar, upper left first molar, lower left first premolar and first molar, and lower right first molar. The tongue volume was Class III, according to both the modified Mallampati and Friedman indices (Fig. 4).
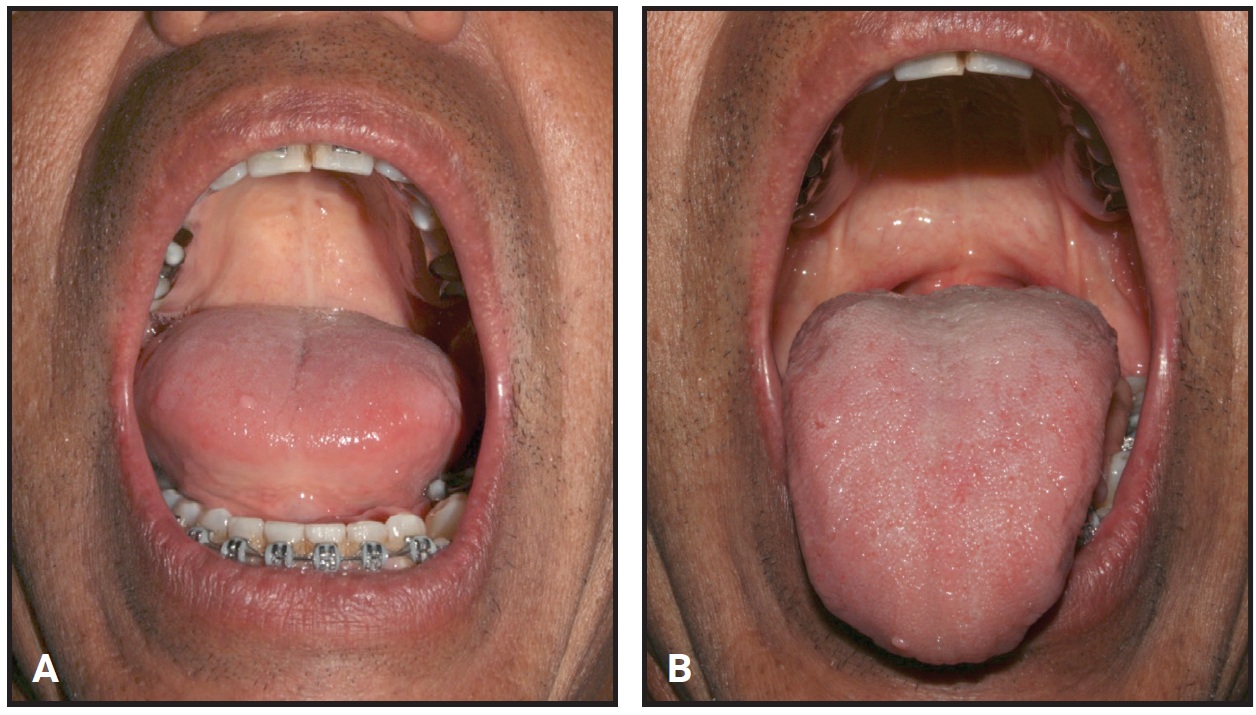
Fig. 4 Friedman (A) and modified Mallampati (B) scores indicate Class III tongue volume.
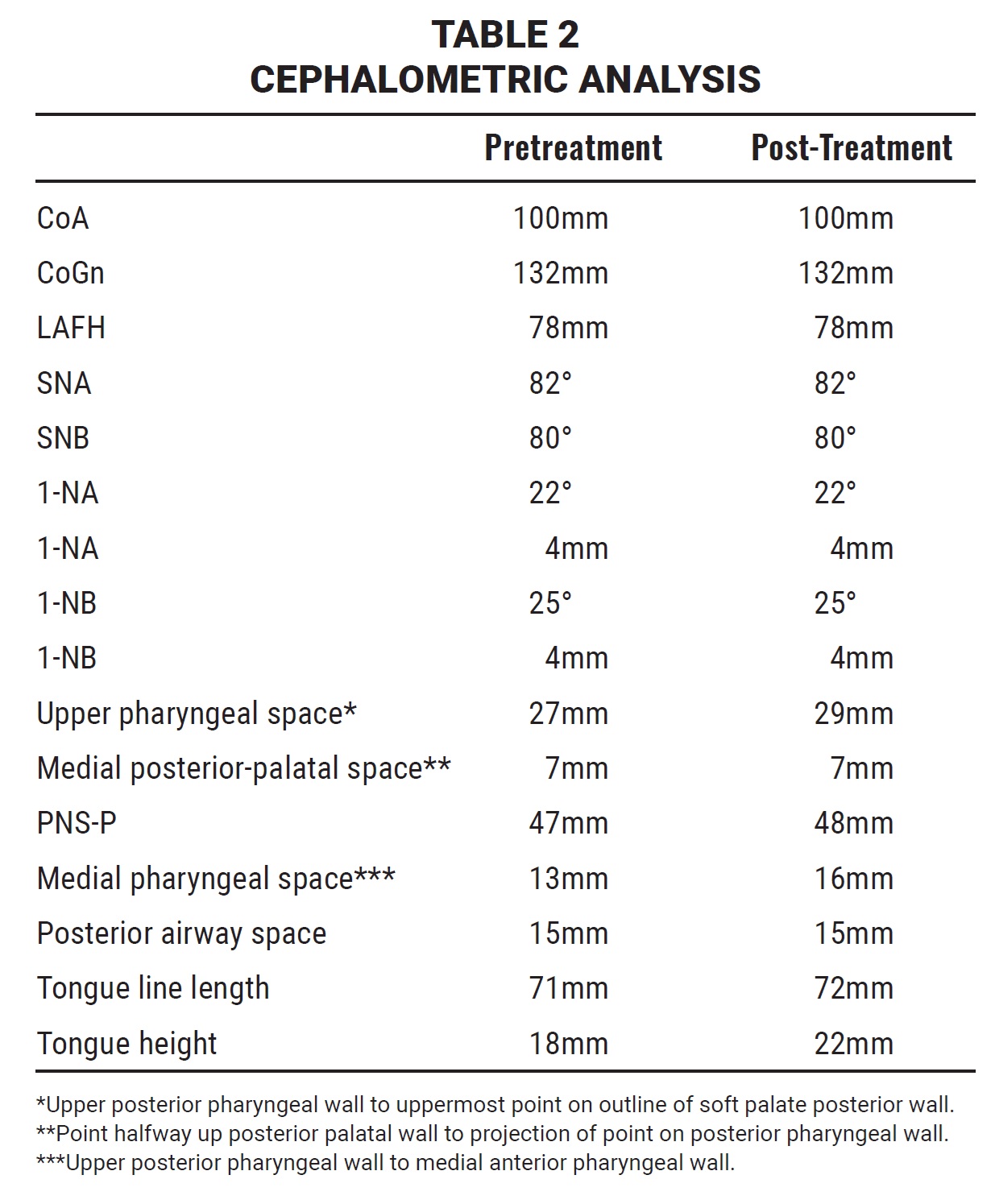
The patient was also being treated by an otorhinolaryngologist, who requested a polysomnography test (Table 3). This confirmed the diagnosis of severe OSA, recording a total of 287 respiratory events (0 central, 198 obstructive, and 89 mixed), for an AHI of 36 events per hour. The baseline O2 saturation was 97% and the average saturation was 94%, ranging from 78% to 99% over about eight hours of sleep.
After being presented with several options, the patient agreed to orthodontic treatment that would involve improving the occlusion and redistributing the edentulous spaces for subsequent rehabilitation with implants and prostheses. Because he had a large tongue volume and no significant skeletal factors contributing to the upper airway obstruction, we decided to utilize the Tongue Rehabilitator along with fixed orthodontic appliances.
Stainless steel MBT**-prescription brackets*** were bonded in both arches. The initial archwires were .014" nickel titanium, progressing to .016" nickel titanium and .018" stainless steel. After 12 months of treatment, the alignment had improved enough to start treatment with the Tongue Rehabilitator.
Rectangular .019" × .025" stainless steel archwires were inserted to improve the occlusion over the next 12 months. During this stage, implants were placed in the edentulous sites of the lower left first premolar and first molar (Fig. 5).
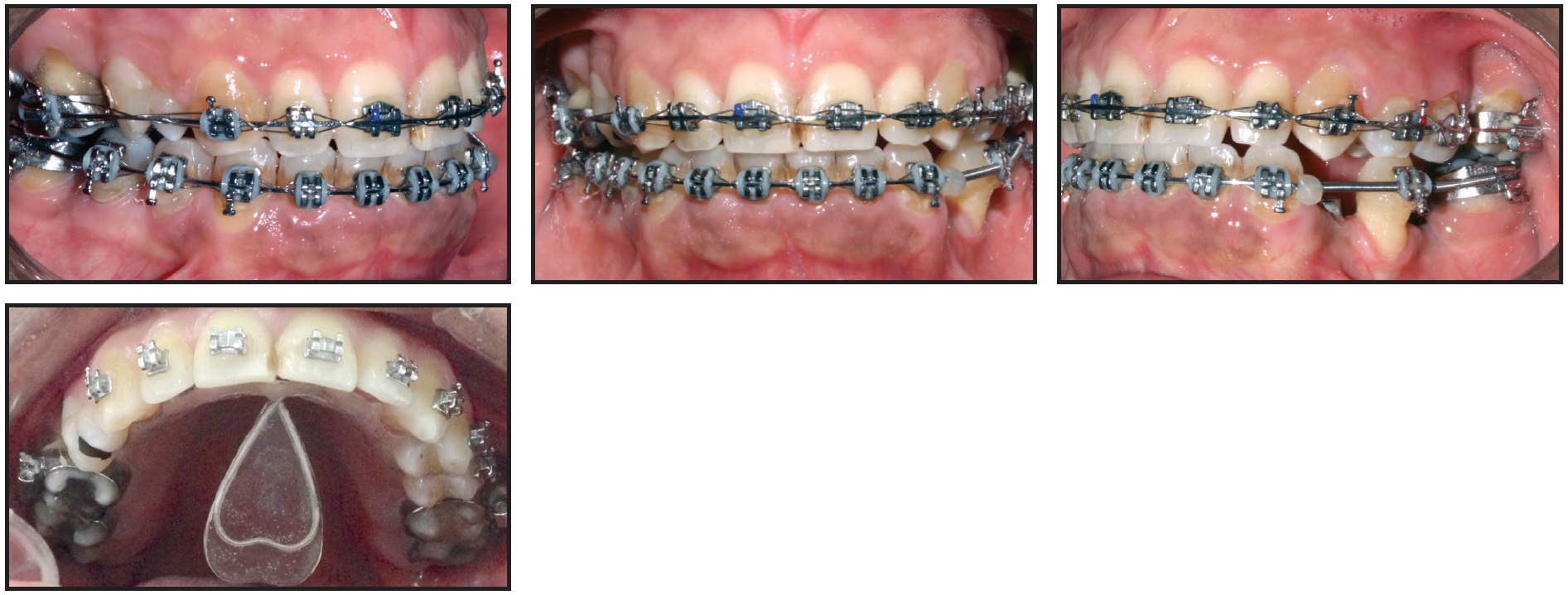
Fig. 5 After 20 months of treatment, including eight months with Tongue Rehabilitator.
Another six months later, after installation of the prosthetic crowns, the fixed appliances were removed.
A lingual 3-3 retainer was bonded in the lower arch, and a Hawley-type retainer was delivered for the upper arch. At bedtime, the Tongue Rehabilitator could be inserted into the telescopic tube of the retainer’s acrylic palatal plate. This approach fit well with the patient’s routine, since he worked with the public and his speech was affected when he was wearing the device.
Total orthodontic treatment time was 30 months (Fig. 6). At the three-month follow-up visit, we made slight adjustments to the retainer and Tongue Rehabilitator. The patient reported that his sleep quality had improved and he was waking up more refreshed, and that his wife also slept more comfortably.
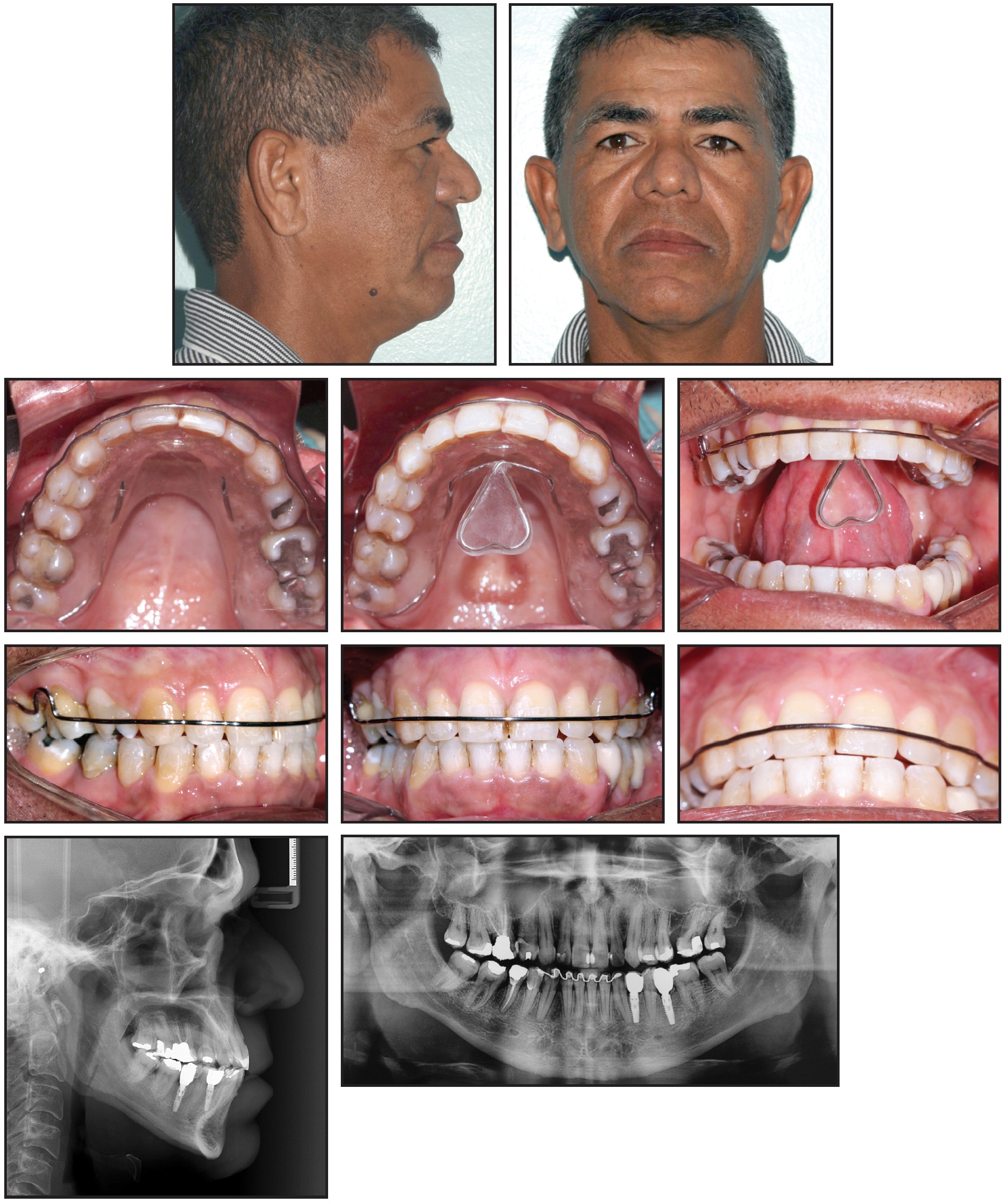
Fig. 6 Patient after 30 months of treatment.
To evaluate the efficiency of the Tongue Rehabilitator after one year of use, another polysomnography test was performed with the device in place (Table 3). The data confirmed a 58% reduction in AHI to 15.1 per hour of sleep, involving 106 respiratory events (0 central, 106 obstructive, and 0 mixed) over seven hours. The average O2 saturation was 94%, varying from 86% to 98%.
After two years of using the Tongue Rehabilitator at night, the patient underwent a third polysomnography test without the device, resulting in an AHI of 9.5 per hour over eight hours of sleep. He experienced 71 respiratory events (0 central, 71 obstructive, and 0 mixed) and an average O2 saturation of 94%, ranging from 87% to 98%. The patient stopped wearing the Tongue Rehabilitator at this point.
Discussion
Treatment modalities for OSA aim to raise the pressure of the pharynx above obstructive pressure, reduce obstruction, or increase upper airway muscle activity and widen the pharyngeal airway, thereby allowing adequate ventilation during sleep.2,20,23,24
Behavioral management is indicated for patients with mild apnea.7,12,27 In cases of moderate or severe apnea, the American Sleep Disorders Association and others consider CPAP treatment to be the gold standard.1,26 Orthognathic surgery can also reduce AHI values to normal levels.2,28
Intraoral devices are generally recommended for patients with primary snoring and mild or moderate apnea, but they are also an option for severely apneic patients who refuse surgery or will not use CPAP therapy because of intolerance, refusal, or contraindications.7,8,10,13,20 Comparisons of various intraoral appliances have found that the mandibular advancement devices can cause effects such as mandibular protrusion, maxillary retrusion, and TMD, resulting in considerable patient discomfort.9,12,23
In contrast, the Tongue Rehabilitator was designed to protrude the tongue and stimulate neural receptors, thus sealing the valves during swallowing and opening the posterior airway. The tongue is a strong muscular organ responsible for a significant portion of pharyngeal obstruction during sleep. When it is placed in an anterior position, the genioglossus muscle stimulates the suprahyoid muscles, which in turn move the hyoid bone forward, opening the hypopharynx even more.11,15
This device may be contraindicated in patients prone to retching. On the other hand, it can be used in patients with TMD because the contraction of lateral pterygoid muscles causes the jaw to follow the protrusive movement of the tongue, thus moving the articular disk into a more anteriorized position and widening the space of the mandibular fossa.
The Tongue Rehabilitator can be adapted to a number of different orthodontic appliances, as seen here. In our patient, it not only opened the airway, but served as a primary tongue educator. After two years of use, the patient’s AHI was reduced from severe (36) to mild (9.5). This device can also be used with expansion plates to treat open bites in the mixed dentition.
Dentistry plays an important role in interdisciplinary treatment of OSA; in particular, orthodontists should be closely involved in identifying OSA and treating it with intraoral devices. Although the Tongue Rehabilitator has shown promising results in our practice, further studies are needed to provide additional scientific evidence of the functionality of this new device, especially compared with mandibular advancement appliances, in the treatment of snoring and sleep apnea.[ref]21,22[/ref]
ACKNOWLEDGMENT: The authors would like to thank Genilda Paes for the design and manufacture of the Tongue Rehabilitator used in this work.
FOOTNOTES
- *Nilton Coelho, DDS, National Institute of Industrial Property Patent PI1102400-3 A2; niltonrosacoelhorc@gmail.com.
- **Trademark of 3M, Monrovia, CA; www.3M.com.
- ***Morelli, Sorocaba, Brazil; www.morelli.com.br.
REFERENCES
- 1. Caldas, S.G.F.R.; Ribeiro, A.A.; Santos-Pinto, L.; Martins, L.P.; and Matoso, R.M.: The effectiveness of mandibular advancement intraoral appliances in the treatment of the snoring and obstructive sleep apnea and hypopnea syndrome (OSAHS): Systematic review, Rev. Dent. Press Ortod. Ortop. Facial 14:74-82, 2009.
- 2. Ito, F.A.; Ito, R.T.; Moraes, N.M.; Sakima, T.; Bezerra, M.L.S.; and Meirelles, R.: Obstructive sleep apnea and hypopnea syndrome (OSAHS) and snoring: Treatment strategies with focus in mandibular advancement device (MAD-ITO), Rev. Dent. Press Ortod. Ortop. Facial 10:143-156, 2005.
- 3. Leite, F.G.J.; Rodrigues, R.C.S.; Ribeiro, R.F.; Eckeli, A.L.; Regalo, S.C.H.; Sousa, L.G.; Fernandes, R.M.F.; and Valera, F.C.: The use of a mandibular repositioning device for obstructive sleep apnea, Eur. Arch. Otorhinolaryngol. 271:1023-1029, 2014.
- 4. Kahwage Neto, S.: Snoring (in Portuguese), Rev. Paraense Med. 21:79-80, 2007.
- 5. Haddad, F. and Bittencourt, L.: Guidelines: Recommendations for the Diagnosis and Treatment of Obstructive Sleep Apnea Syndrome in Adults (in Portuguese), Associação Brasileira do Sono, São Paulo, Brazil, 2013.
- 6. Cançado, R.H.; Valarelli, F.P.; Freitas, K.M.S.; Neves, L.S.; and Guimarães Júnior, C.H.: Using the Twin Force Bite Corrector (TFBC) appliance in the treatment of Class II malocclusion, Orthod. Sci. Pract. 24:431-447, 2013.
- 7. Chaves Júnior, C.M.; Dal-Fabbro, C.; Bruin, V.M.S.; Tufik, S.; and Bittencourt, L.R.A.: Brazilian consensus on snoring and sleep apnea: Aspects of interest to orthodontists (in Portuguese), Dent. Press J. Orthod. 16:1-10, 2011.
- 8. Guimarães, M.L.R.; Oliveira, J.J.M.; and Azevedo, P.G.: PLP appliance for treatment of snoring and obstructive sleep apnea, Orthod. Sci. Pract. 8:113-117, 2015.
- 9. Godolfim, L.R.: Intra-oral devices in the treatment of snoring and sleep apnea (in Portuguese), in Nova Visão em Ortodontia e Ortopedia Funcional dos Maxilares, ed. E. Sakai, F.A. Cotrim-Ferreira, and N.D.S. Martins, Santos Publishing, São Paulo, Brazil, 2002, pp. 507-513.
- 10. Couto, F.F.; Renz, F.B.; and Grossi, M.L.: Use of interocclusal splint in the treatment of sleep apnea/hypopnea syndrome (OSAHS): A systematic review, Rev. Grad. PUCRS 2:1-9, 2009.
- 11. Silveira, M.A.: The sleep apnea syndrome, the snore and its treatment with Apnout appliance (in Portuguese), J. Bras. Ortod. Ortop. Facial 6:201-203, 2001.
- 12. Diagnosis and Treatment of Obstructive Sleep Syndrome (OSAS): Practical Guide (in Portuguese), ed. L.A. Bittencourt, LMP Publishing, São Paulo, Brazil, 2008.
- 13. Poluha, R.L.; Stefaneli, E.A.B.; and Terada, H.H.: Dentistry in obstructive sleep apnea syndrome: Diagnosis and treatment (in Portuguese), Rev. Bras. Odontol. 24:87-90, 2015.
- 14. Colombini, N.: Facial Surgery: Functional and Aesthetic Interpretation (in Portuguese), Theime Revinter Publicações, Rio de Janeiro, 2001, p. 591.
- 15. Johal, A.; Gill, G.; Ferman, A.; and McLaughlin, K.: The effect of mandibular advancement appliances on awake upper airway and masticatory muscle activity in patients with obstructive sleep apnoea, Clin. Physiol. Funct. Imaging 27:47-53, 2007.
- 16. Dekon, S.F.C.; Goiato, M.C.; Amaral, T.P.C.; Alves, T.M.; Quintino, N.V.; and Viana, L.P.: Surgeon’s role in primary dentist treatment of snoring and obstructive sleep apnea (in Portuguese), Rev. Odont. Araçatuba 36:70-74, 2015.
- 17. Rodrigues, M.M.; Dibbern, R.S.; Goulart, C.W.K.; and Palma, R.A.: Correlation between the Friedman classification and the apnea-hypopnea index in a population with OSAHS, Braz. J. Otorhinolaryngol. 76:557-560, 2010.
- 18. Silva, A.D.L.; Catão, M.H.C.V.; Costa, O.C.; and Costa, I.R.R.S.: Multidisciplinary in sleep apnea: A literature review, Rev. CEFAC 16:1621-1626, 2014.
- 19. Epstein, L.; Kristo, D.; Strollo Júnior, P.; Friedman, N.; Malhotra, A.; Patil, S.; Ramar, K.; Rogers, R.; Schwab, R.; Weaver, E.; and Weinstein, M.: Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults, J. Clin. Sleep Med. 5:263-276, 2009.
- 20. Caixeta, A.C.P.; Jansen, W.C.; and Caixeta, E.C.: Intra oral devices for the treatment of obstructive sleep apnea and hypopnea syndrome (in Portuguese), Arq. Bras. Odontol. 6:38-44, 2010.
- 21. Conley, R.S.: Management of sleep apnea: A critical look at intra-oral appliances, Orthod. Craniofac. Res. 18:83-90, 2014.
- 22. Kurtulmus, H.; Cotert, S.; Bilgen, C.; On, Y.; and Boyacioglu, H.: The effect of a mandibular advancement splint on electromyographic activity of the submental and masseter muscles in patients with obstructive sleep apnea, Int. J. Prosthod. 22:586-594, 2009.
- 23. Almeida, M.A.O.; Texeira, O.B.; Vieira, L.S.; and Quintão, C.C.A.: Treatment of obstructive sleep apnea and hipoapnea syndrome with oral appliances, Braz. J. Otorhinolaryngol. 72:699-703, 2006.
- 24. Abi-Ramia, L.B.P.; Carvalho, F.A.R.; Coscarelli, C.T.; and Almeida, M.A.O.: Increase in airway volume in patients with obstructive sleep apnea using a mandibular advancement device, Dent. Press J. Orthod. 15:166-171, 2010.
- 25. Monteiro, T.A.S.; Martins, O.F.M.; and Costa, D.M.C.: Intraoral appliances in the treatment of obstructive sleep apnea syndrome: A literature review (in Portuguese), Rev. Interdicip. NOVAFAPI 4:66-71, 2011.
- 26. Vinha, P.P.; Santos, G.P.; Brandão, G.; and Fagnani Filho, A.: Snoring and sleep apnea: Presentation of a new oral device and treatment protocol (in Portuguese), Rev. Gaúcha Odontol. 58:515-520, 2010.
- 27. Engelke, W.; Engelhardt, W.; Gartner, M.M.; Deccó, O.; Barrirero, J.; and Knosel, M.: Functional treatment of snoring based on the tongue-repositioning manoeuvre, Eur. J. Orthod. 32:490-495, 2010.
- 28. Prado, B.N.; Fernades, E.G.; Moreira, T.C.A.; and Gavranich Júnior, J.: Obstructive sleep apnea: Diagnosis and treatment, Rev. Odontol. UNICID 22:233-239, 2010.




COMMENTS
.