CASE REPORT
Surgical-Orthodontic Management of Severe Sleep Apnea
Treatment of patients with complex anatomical deformities caused by trauma or congenital defects is extremely challenging. In addition to compromised esthetics, gross deformities also tend to be characterized by functional impairments.
Patients with craniomandibular deformities suffering from sleep apnea have been previously reported in the literature.1 The following report describes the treatment of such a patient.
Diagnosis
An 18-year-old male presented to the Department of Oral and Maxillofacial Surgery with problems including reduced mouth opening, loud snoring, excessive daytime somnolence, morning headaches, and an impaired ability to concentrate (Fig. 1). He had been treated for bilateral TMJ ankylosis with costochondral grafts 10 years previously and a bilateral coronoidectomy five years previously. He was referred to the Department of Orthodontics.
Similar articles from the archive:

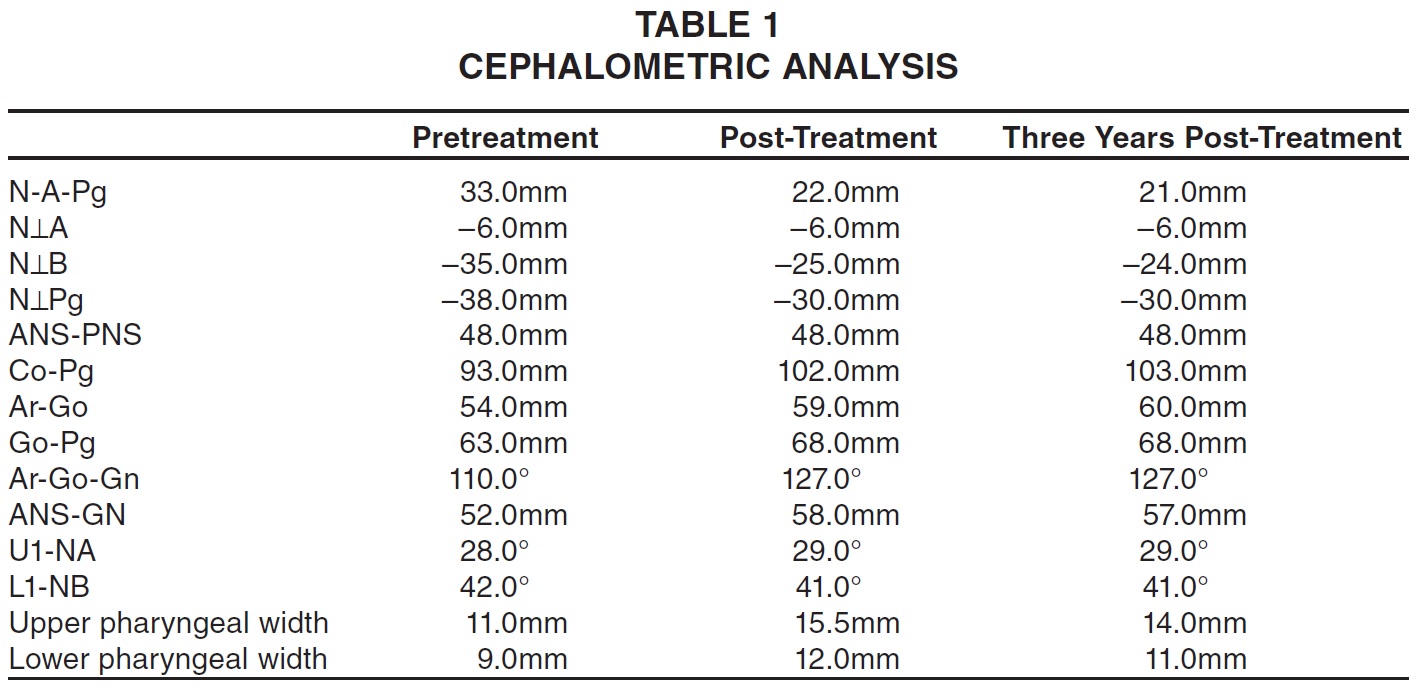
Fig. 1 18-year-old male patient with severe craniomandibular deformity, retrognathic mandible, facial convexity, and crowding in both arches before treatment.
On clinical examination, the patient exhibited excessive sleepiness, inability to focus and concentrate, reduced cognitive function, and a pale, sickly appearance. He was likely to doze off in the dental chair even when waiting for a few minutes. Extraoral examination showed facial asymmetry, with the chin deviated to the right. The profile was severely convex, and the lower jaw appeared severely retrognathic in both the horizontal and vertical dimensions. Mouth opening was limited to 15mm, making it difficult to take impressions.
Intraoral evaluation revealed proclination and crowding of the upper and lower anterior teeth, with an overjet of 12mm, an overbite of 5mm, a constricted upper arch with a tendency toward crossbite, and a buccal crossbite of the upper left second molar. The mandibular left lateral incisor was lingually displaced and was extruded well above the occlusal plane.
Radiographs showed the defective condylar joint and evidence of past surgery. All teeth were present except for the upper right and both lower third molars. The lower right second premolar was impacted. Cephalometric analysis confirmed a severe facial convexity, a retrognathic mandible, a deficient chin and lower facial height, and proclined upper and lower anterior teeth (Table 1).
Four-channel polysomnography revealed:
- Prolonged periods of apnea and hypopnea, with significant oxygen desaturation (64%).
- An apnea-hypopnea index (AHI) of more than 100.
- Resting tachycardia.
- These findings were indicative of severe obstructive sleep apnea (OSA) syndrome.2
Treatment Plan
The first priority in this case was to relieve the sleep apnea by mandibular advancement involving distraction osteogenesis (DO). The mandibular left lateral incisor was extracted prior to surgery since it was periodontally compromised, traumatic to the patient, and a probable source of occlusal interference. The surgical phase was to be followed by orthodontic treatment, with the objectives of creating a stable bite to maintain the mandibular position, alleviating the dental crowding, and achieving proper arch coordination.
Treatment Progress
A cephalogram and panoramic radiograph were used to evaluate the morphology of the mandible, the lengths of the ramus and body, and the locations of the inferior alveolar canal and tooth buds in the area of the osteotomy. Under general anesthesia, an oblique osteotomy of the angle of the mandible was performed, with cuts made distal to the second molars to achieve horizontal and vertical elongation. Two extraoral unifocal distractors were placed in an oblique orientation to promote both vertical and horizontal lengthening of the ramus and body (Fig. 2).
After one week of healing, the distractors were activated at a rate of .5mm twice a day for 25 days. The initial activation was bilateral; additional activation was then performed on the right side to correct the mandibular asymmetry. After a total activation of 15mm on the right side and 10mm on the left, the overjet and overbite had each been reduced to 1mm. The patient experienced little discomfort except for a mild skin rash that was quickly treated.
The distractors were left in place for another 12 weeks, to ensure adequate consolidation of the callus, and were then removed under local anesthesia. At the end of the distraction phase, the patient had a crossbite in the upper left quadrant (Fig. 3), but the convexity of the profile had been reduced considerably.

Fig. 2 Bilateral extraoral unifocal distractors in place.

Fig. 3 Distractors removed 12 weeks after end of 25-day activation period.
The patient could open his mouth an additional 3-4mm and was able to breathe more comfortably. Postsurgical polysomnography showed an AHI of 15 and a substantial increase in oxygen saturation (94%).
The upper and lower right first premolars were extracted before placement of orthodontic appliances. Full fixed appliances were bonded one week after removal of the distractors. Treatment was routine, requiring 20 months. A modified Hawley retainer with a lingual flange to hold the mandible in an advanced position was then prescribed.
Treatment Results
Post-treatment evaluation showed an improved profile with reduced convexity (Fig. 4A).
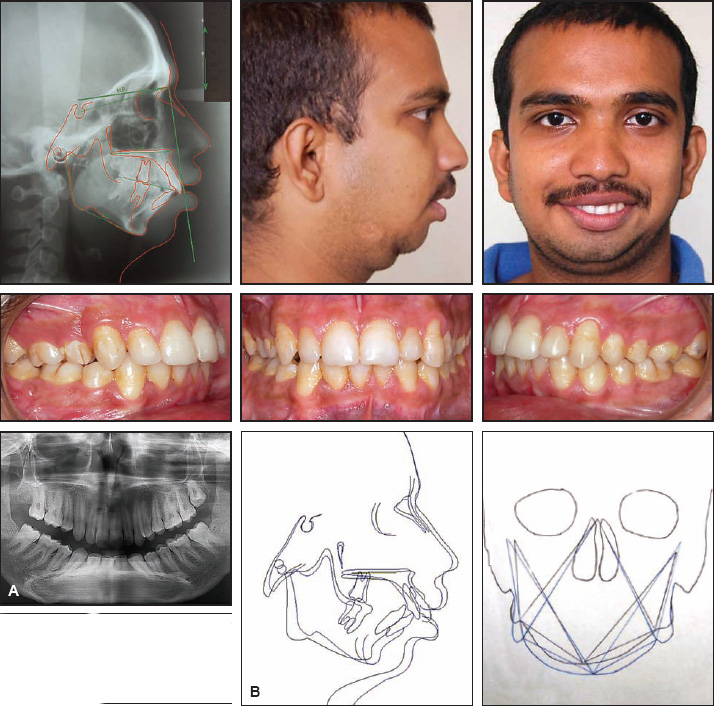
Fig. 4 A. Patient after 20 months of orthodontic treatment. B. Superimposition of pre- and post-treatment cephalometric and postero-anterior tracings.
A Class I molar and canine relationship was achieved, although the lower midline was compromised due to the extraction of a single mandibular lateral incisor. Chin projection and symmetry were improved, but some mandibular asymmetry was still present. The retropalatal passage (upper pharyngeal width) had widened by 4.5mm, and the retroglossal airway (lower pharyngeal width) by 3mm. Cephalometric analysis corroborated the clinical findings and also showed an increase in airway volume (Fig. 4B, Table 1).
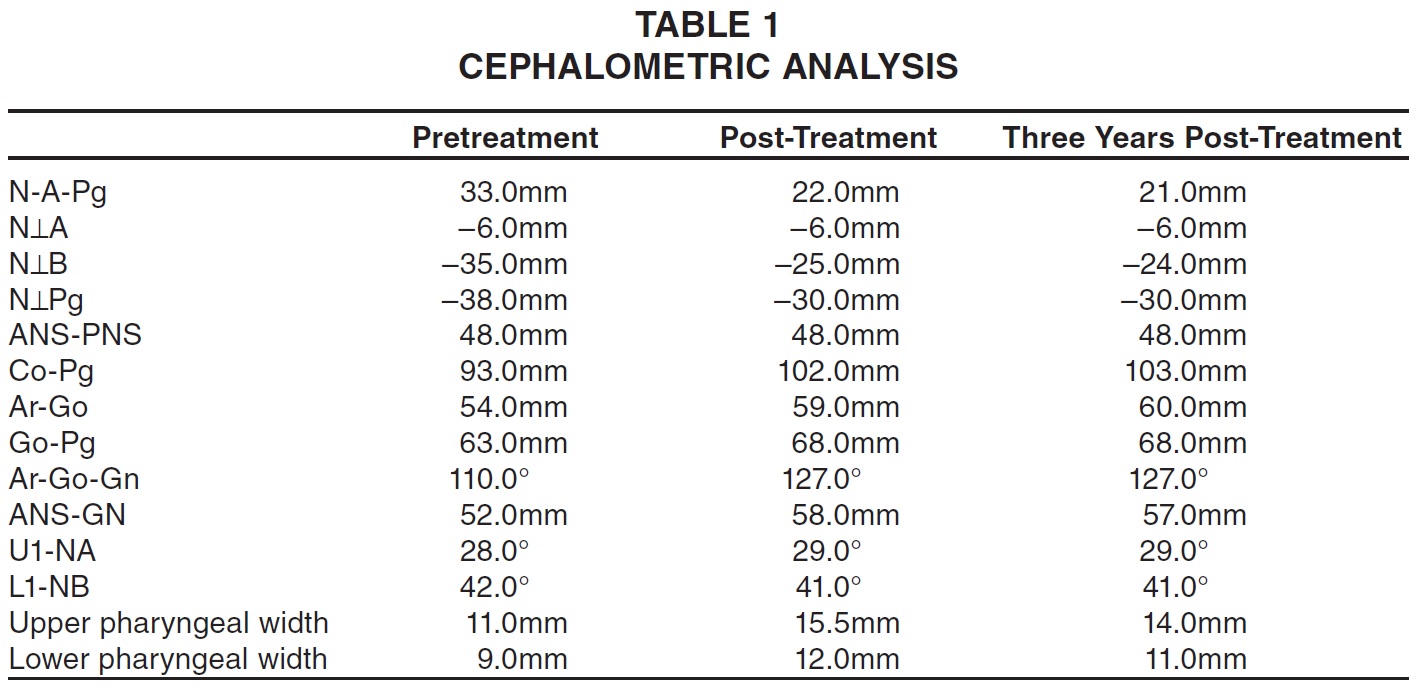
Most relapse occurs during the first year after mandibular DO, due to forces from the suprahyoid muscle complex.4 In this case, records taken three years after debonding confirmed the stability of the profile changes and the occlusion (Fig. 5).
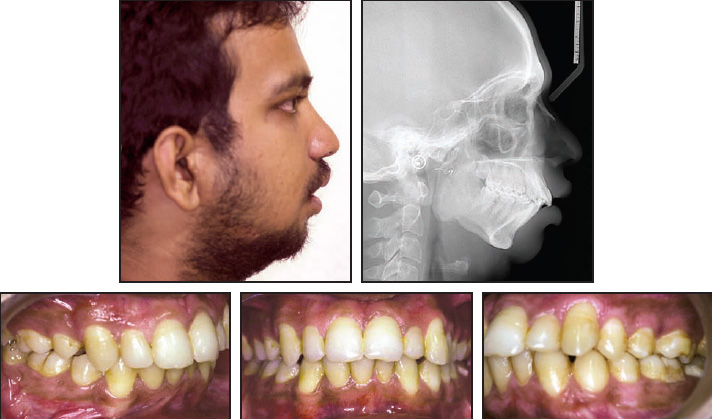
Fig. 5 Follow-up records taken three years after end of treatment.
Discussion
Sleep apnea is classified as obstructive, central, or mixed.5 Obstructive apnea is caused by a collapse of soft-tissue structures in the oropharynx or hypopharynx. Our patient's sleep apnea was attributable to mandibular retrognathia due to ankylosis of the TMJs and impeded growth. The severely micrognathic and retropositioned mandible likely caused the retropositioned tongue base to fall into the pharyngeal airway.6
OSA syndrome is characterized by repetitive episodes of upper airway obstruction during sleep, usually associated with a reduction in blood oxygen saturation. People with sleep apnea literally stop breathing during their sleep, often for a minute or longer, making this a potentially fatal condition. The severity of sleep apnea is determined by the AHI (also known as the respiratory distress index), which measures the number of abnormal respiratory events per hour of sleep. An AHI of 5-14 indicates mild OSA, 15-30 indicates moderate severity, and more than 30 indicates severe OSA.
OSA affects the quality of life, with consequences including excessive daytime somnolence, morning headaches, changes in personality, depression, difficulty in concentrating, and confusion.3 Many of these symptoms were seen in our patient, who had difficulty pursuing his daily routine and academic commitments as a college student.
Distraction osteogenesis has become a common treatment modality for maxillofacial disorders since its use by McCarthy to lengthen a congenitally hypoplastic mandible.7 The technique involves the manipulation of a healing bone, with an osteotomized area stretched before calcification has occurred to promote the formation of additional bone and investing soft tissue. Because greater movement is possible than with conventional orthognathic surgery, DO is recommended for mandibular deficiencies of more than 10-15mm (our patient presented with an overjet of 12mm). DO is the preferred approach when a short ramus cannot be lengthened by maxillofacial surgery, since the musculature of the pterygomandibular sling does not adapt to lengthening of the ramus.8 Distraction histogenesis allows better soft-tissue adaptation and thus can be used to enlarge the soft-tissue envelope.9
Although extraoral distractors can cause minor facial scarring and are highly visible and potentially uncomfortable during sleep, they were the most affordable option for our patient. Mandibular advancement with DO preceded orthodontic treatment partly because of the patient's limited ability to open his mouth, but mainly because our first priority was to advance the mandible and cure his sleep apnea. After distraction, the mandibular advancement could be perceived clinically, along with an improvement in chin projection, neck-throat profile, and labiomental sulcus definition and an increase in lower anterior facial height. More significantly, the retroglossal and retropalatal airway had been enlarged, as reflected in the post-operative polysomnography.
Our patient was cured of daytime somnolence and associated symptoms and reported remarkable improvement in his overall well-being and self-confidence.
REFERENCES
- 1. Jamieson, A.; Guilleminault, C.; Partinen, M.; and Quera-Salva, M.A.: Obstructive sleep apneic patients have craniomandibular abnormalities, Sleep 9:469-477, 1986.
- 2. Hosselet, J.; Ayappa, I.; Norman, R.G.; Krieger, A.C.; and Rapoport, D.M.: Classification of sleep-disordered breathing, Am. J. Respir. Crit. Care Med. 163:398-405, 2001.
- 3. Cote, E.F.: Obstructive sleep apnea: An orthodontic concern, Angle Orthod. 58:293-307, 1988.
- 4. Carlson, D.S.; Ellis, E. III; and Dechow, P.C.: Adaptation of the suprahyoid muscle complex to mandibular advancement surgery, Am. J. Orthod. 92:134-143, 1987.
- 5. Lowe, A.A.; Santamaria, J.D.; Fleetham, J.A.; and Price, C.: Facial morphology and obstructive sleep apnea, Am. J. Orthod. 90:484-491, 1986.
- 6. Young, T.; Palta, M.; Dempsey, J.; Skatrud, J.; Weber, S.; and Badr, S.: The occurrence of sleep disordered breathing among middle-aged adults, N. Engl. J. Med. 328:1230-1235, 1993.
- 7. McCarthy, J.G.; Schreiber, J.; Karp, N.; Thorne, C.H.; and Grayson, B.H.: Lengthening the human mandible by gradual distraction, Plast. Reconstr. Surg. 89:1-8, 1992.
- 8. Rubio-Bueno, P.; Villa, E.; Carreno, A.; Naval, L.; Sastre, J.; Manzanares, R.; and Diaz-Gonzales, F.J.: Intraoral mandibular distraction osteogenesis: Special attention to treatment planning, J. Craniomaxillofac. Surg. 29:254-262, 2001.
- 9. Rachmiel, A.; Levy, M.; and Laufer, D.: Lengthening of the mandible by distraction osteogenesis: Report of cases, J. Oral Maxillofac. Surg. 53:838-846, 1995.






