Upper Molar Distalization with Invisalign Treatment Accelerated by Photobiomodulation
Recent advances in the Invisalign* system allow predictable distalization of posterior teeth to facilitate treatment of Class II and Class III malocclusions.1-3 A sequential approach can be used to maximize anchorage, but requires a large number of aligner stages.4 Even with the weekly change protocol recently recommended by Align Technology, it may take 40-50 weeks to distalize the posterior teeth, depending on the amount of tooth movement needed.5,6 In a previous article, we demonstrated that the use of OrthoPulse** photobiomodulation (PBM) could accelerate bone remodeling and orthodontic tooth movement, allowing patients to change Invisalign aligners as often as every three days.7 This article shows how PBM can be applied to accelerate sequential distalization with the Invisalign system.
Photobiomodulation and Tooth Movement
Photobiomodulation, also known as low-level light therapy, employs near-infrared light (600-1000nm) from a low-level laser or light-emitting diode.8,9 At the cellular level, PBM is thought to activate the predominant mitochondrial photoacceptor, cytochrome c oxidase, thus increasing mitochondrial adenosine triphosphate production by means of an elevated proton concentration gradient across the inner mitochondrial membrane.10-13 This effect facilitates tissue repair and bone remodeling by raising metabolic activity in damaged areas.14 In addition, there is some evidence that PBM therapy can reduce pain because of its anti-inflammatory properties.15
Data from rat models have indicated that PBM can also accelerate tooth movement. One study reported increases in osteoclast numbers on the pressure side of the targeted molars and bone formation and cellular proliferation on the tension side.16 Clinical studies investigating orthodontic treatment with fixed appliances17 and clear aligners18,19 have found significantly increased tooth movement in the irradiated patients. A systematic review of five human trials and 11 animal studies concluded that a reasonable dose of PBM may reduce orthodontic treatment time20; an evaluation of 18 clinical trials found evidence supporting the efficacy of laser therapy and PBM.21
Similar articles from the archive:
- Invisalign with Photobiomodulation: Optimizing Tooth Movement and Treatment Efficacy with a Novel Self-Assessment Algorithm March 2017
- THE CUTTING EDGE Invisalign Treatment Accelerated by Photobiomodulation May 2016
- A Three-Dimensional Finite Element Analysis of Upper-Canine Distalization with Clear Aligners, Composite Attachments, and Class II Elastics January 2017
Case Report
A 23-year-old female patient presented with the chief complaint of protrusive upper anterior teeth (Fig. 1A and B).

Fig. 1 A. 23-year-old female patient with Class II canine relationship, protrusive upper anterior teeth, and anterior open bite before treatment (continued in next image).
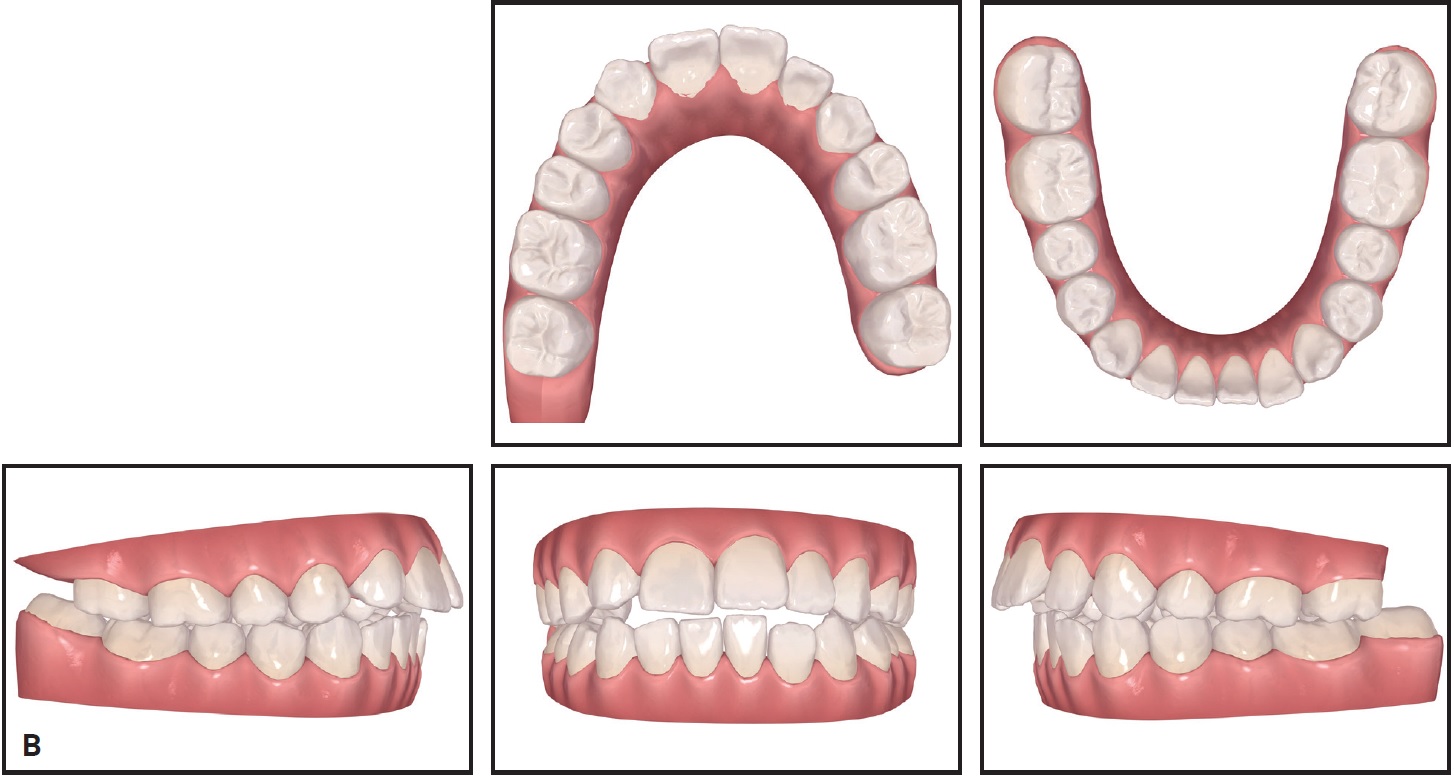
Fig. 1 (cont.) B. Initial ClinCheck* records.
The upper right lateral incisor was congenitally missing, and the upper left first premolar had been extracted at age 15, during previous orthodontic treatment with fixed appliances. An anterior open bite had resulted from a protrusive tongue habit acquired after that treatment. The canine relationship was Class II.
The patient requested an esthetic improvement using Invisalign clear aligners. Our treatment plan involved extraction of the lower left and both upper third molars, followed by distal movement of the upper molars. Because the patient lacked an upper right lateral incisor, the upper right first premolar would serve as the canine and the upper right canine would be recontoured as the lateral incisor after orthodontic tooth movement.
The patient was instructed to change her aligners every three days and to use an OrthoPulse PBM device twice a day for five minutes per arch. A modified OrthoPulse is currently in development to extend coverage to the first and second molars, allowing segmental PBM treatment of the molars and anterior teeth. For this case, a prototype OrthoPulse with a distal extension was used so as to affect only the molars during their distalization, thus maximizing anterior anchorage (Fig. 2).
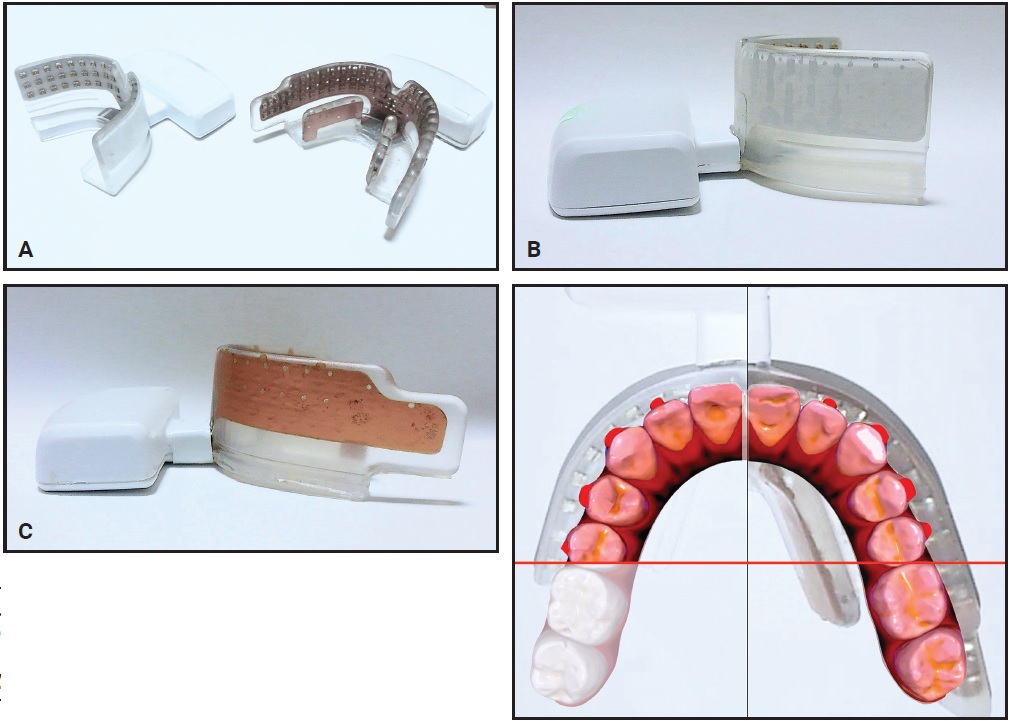
Fig. 2 A. Original OrthoPulse** (left) and modified prototype with distal extension (right). B. Original OrthoPulse. C. Distal extension applies photobiomodulation only to molar regions.
Following our standard practice protocol, the patient wore two stages of aligners without attachments, so that she could adapt to wearing the aligners properly before more steps were added to her routine (Fig. 3).

Fig. 3 First Invisalign* set.
At this point, buttons were bonded to the lower first molars, and hooks were bonded directly to the upper right first premolar and left canine. The patient was instructed to use Class II elastics for 20 hours per day.20,22 During distalization of the upper molars, the occlusal coverage of the aligners reduced interference from opposing teeth and controlled the vertical position of the crowns.
After five weeks of treatment, the upper second molars had been distalized, and distal movement of the first molars was initiated (Fig. 4).
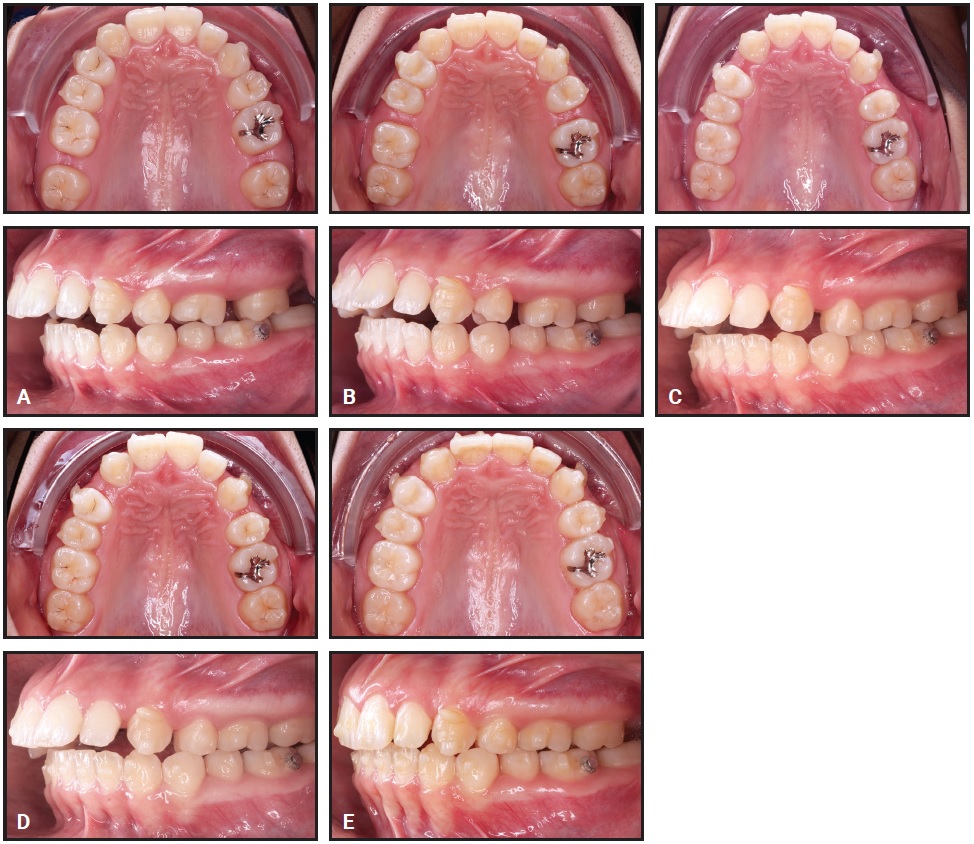
Fig. 4 Sequential distalization. A. Distalization of second molars completed after five weeks of treatment. B. Distalization of first molars completed after three months of treatment. C. Distalization of premolars completed after five months of treatment. D. Distalization of canines completed after seven months of treatment. E. Upper anterior retraction completed after 10 months of treatment.
Class II elastics were continued to prevent anchorage loss. Distalization of the first molars required nine weeks, followed by eight weeks for the premolars and five weeks for the canines. After 10 months of treatment, when anterior retraction was complete, a gingivoplasty was performed in the upper right anterior region to achieve esthetic symmetry of the gingival margins, and the upper right canine was recontoured to simulate a lateral incisor (Fig. 5).
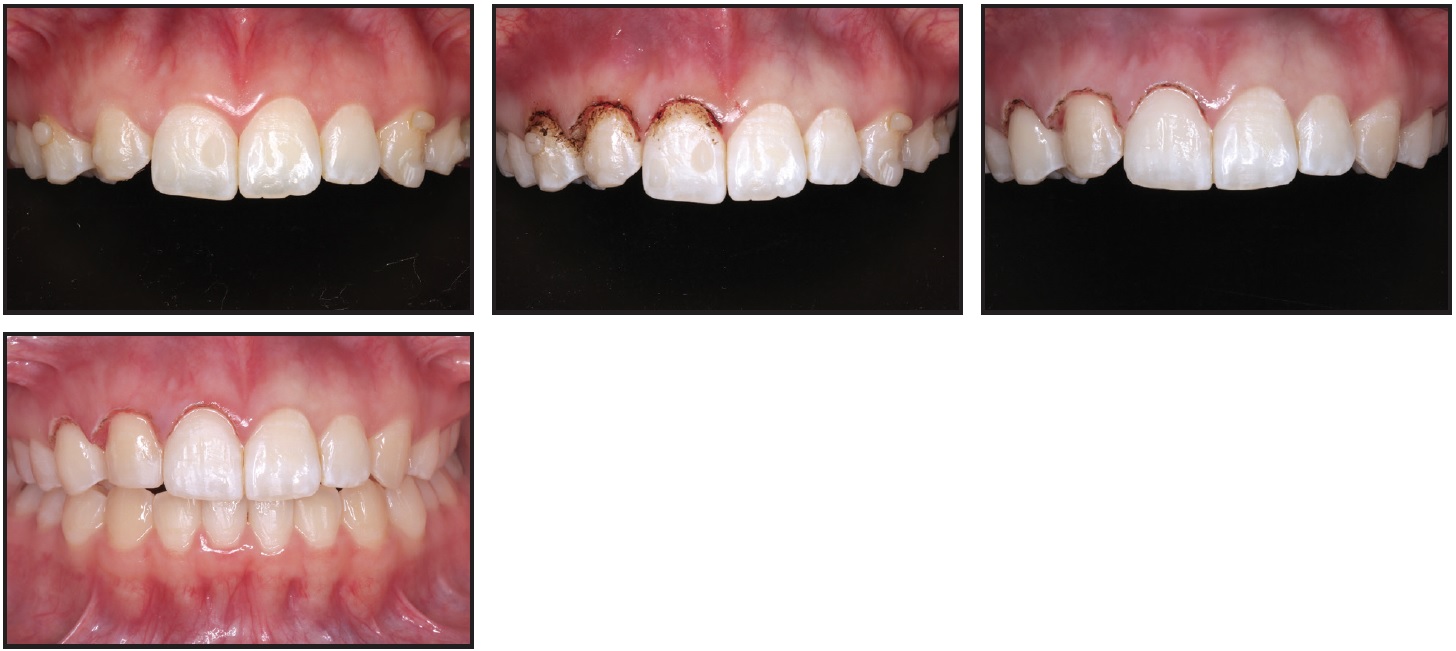
Fig. 5 With upper retraction complete, gingivoplasty performed in upper right anterior region to lengthen crowns and improve gingival margins; upper right canine recontoured to simulate lateral incisor.
Treatment was completed in 11 months, using 111 sets of aligners ([img=6A]Fig. 6A, B[/img) and C.
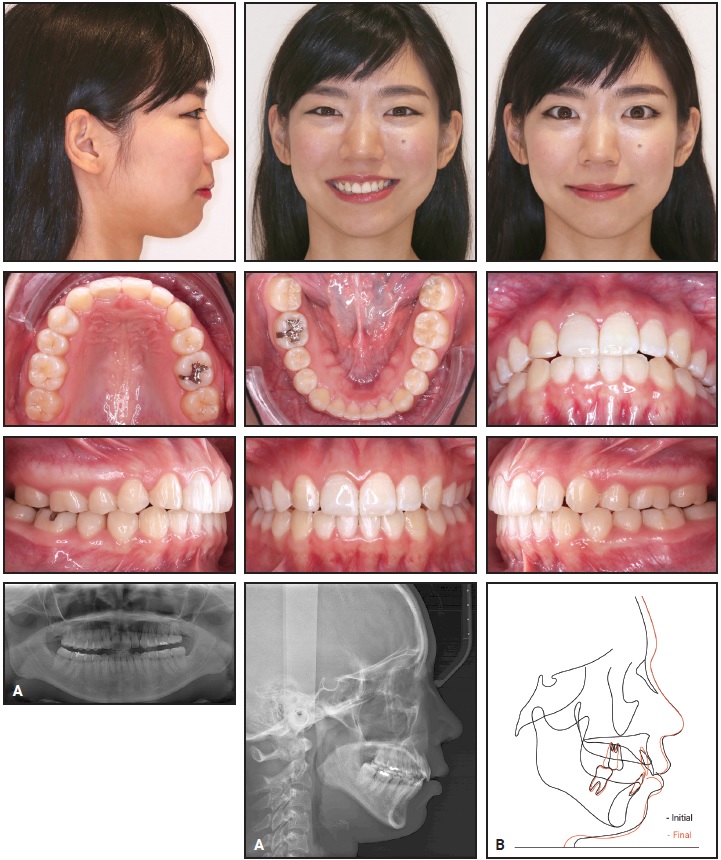
Fig. 6 A. Patient after 11 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings (continued in next image).
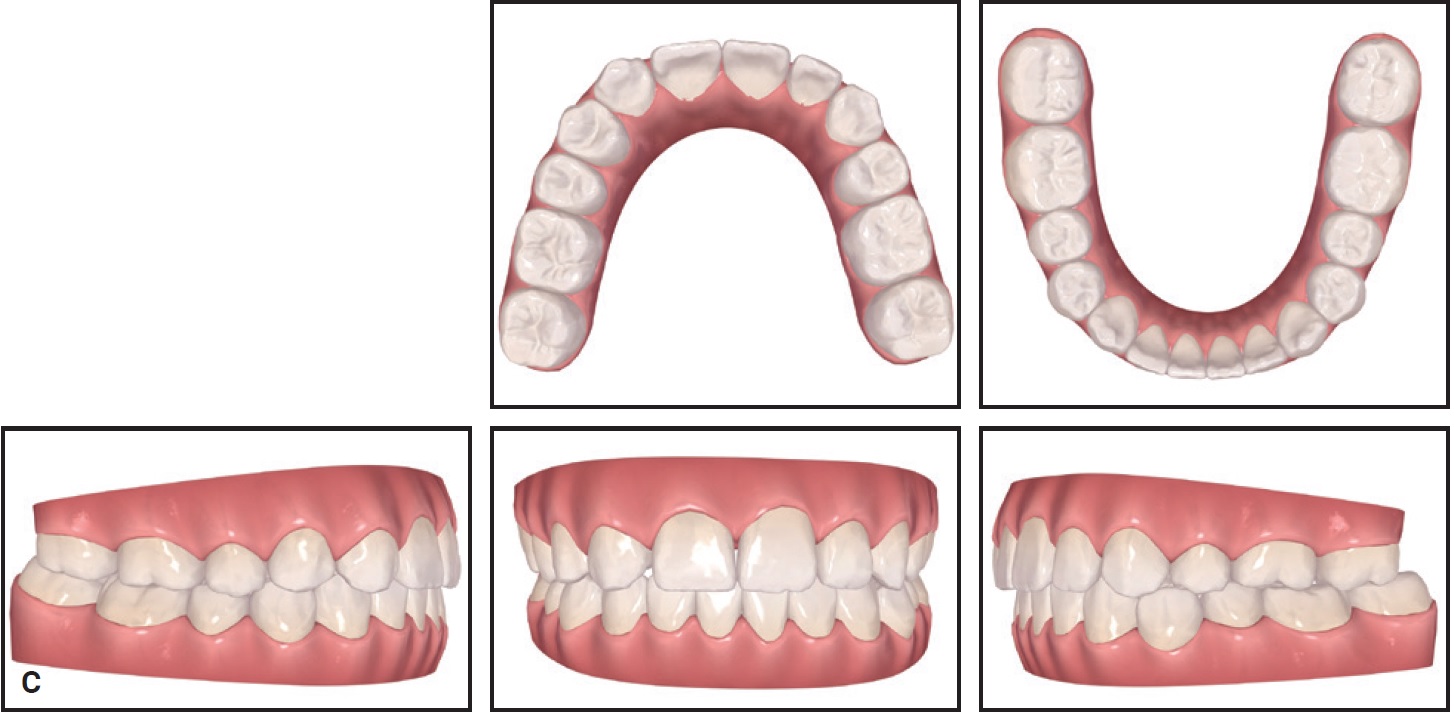
Fig. 6 (cont.) C. Post-treatment ClinCheck records.
Discussion
By using the extended OrthoPulse device, the patient was able to change aligners every three days without any loss of tracking. A major advantage of PBM is that the clinician can review treatment progress in a compressed time period, allowing any necessary refinement or midcourse correction to be performed earlier.23,24 A disadvantage of a faster aligner progression is that loss of tracking could occur sooner. That makes it even more crucial for the patient to understand aligner fit and to advance to the next stage only if the current aligners are fitting well.
In the case shown here, segmental PBM treatment improved aligner tracking by enhancing anterior anchorage while accelerating molar movement. Shortening the time required for Invisalign treatment can prevent the typical decline in patient compliance25 and avoid any deterioration in oral hygiene and consequent issues such as dental caries, periodontal problems, or root resorption.26,27
FOOTNOTES
- *Registered trademark of Align Technology, Inc., San Jose, CA; www.aligntech.com.
- **Trademark of Biolux Research Ltd., Vancouver, BC, Canada; www.bioluxresearch.com.
REFERENCES
- 1. Schupp, W.; Haubrich, J.; and Neumann, I.: Class II correction with the Invisalign system, J. Clin. Orthod. 44:28-35, 2010.
- 2. Ravera, S.; Castroflorio, T.; Garino, F.; Daher, S.; Cugliari, G.; and Deregibus, A.: Maxillary molar distalization with aligners in adult patients: A multicenter retrospective study, Prog. Orthod. 17:12, 2016.
- 3. Pagani, R.; Signorino, F.; Poli, P.P.; Manzini, P.; and Panisi, I.: The use of Invisalign system in the management of the orthodontic treatment before and after Class III surgical approach, Case Rep. Dent. 2016:9231219, 2016.
- 4. Weir, T.: Clear aligners in orthodontic treatment, Austral. Dent. J. 62:58-62, 2017.
- 5. Giancotti, A.; Garino, F.; and Mampieri, G.: Lower incisor extraction treatment with the Invisalign technique: Three case reports, J. Orthod. 42:33-44, 2015.
- 6. Bowman, S.J.; Celenza, F.; Sparaga, J.; Papadopoulos, M.A.; Ojima, K.; and Lin, J.C.: Creative adjuncts for clear aligners, Part 3: Extraction and interdisciplinary treatment, J. Clin. Orthod. 49:249-262, 2015.
- 7. Ojima, K.; Dan, C.; Kumagai, Y.; and Schupp, W.: Invisalign treatment accelerated by photobiomodulation, J. Clin. Orthod. 50:309-317, 2016.
- 8. Domínguez, A. and Velásquez, S.A.: Effect of low-level laser therapy on pain following activation of orthodontic final archwires: A randomized controlled clinical trial, Photomed. Laser Surg. 31:36-40, 2013.
- 9. Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; and Brawn, P.: Photobiomodulation accelerates orthodontic alignment in the early phase of treatment, Prog. Orthod. 14:30, 2013.
- 10. Rojas, J.C. and Gonzalez-Lima, F.: Low-level light therapy of the eye and brain, Eye Brain 3:49-67, 2011.
- 11. Eells, J.T.; Wong-Riley, M.T.; VerHoeve, J.; Henry, M.; Buchman, E.V.; Kane, M.P.; Gould, L.J.; Das, R.; Jett, M.; Hodgson, B.D.; Margolis, D.; and Whelan, H.T.: Mitochondrial signal transduction in accelerated wound and retinal healing by near-infrared light therapy, Mitochondrion 4:559-567, 2004.
- 12. Watanabe, H.; Bohensky, J.; Freeman, T.; Srinivas, V.; and Shapiro, I.M.: Hypoxic induction of UCP3 in the growth plate: UCP3 suppresses chondrocyte autophagy, J. Cell. Physiol. 216:419-425, 2008.
- 13. Masha, R.T.; Houreld, N.N.; and Abrahamse, H.: Low-intensity laser irradiation at 660 nm stimulates transcription of genes involved in the electron transport chain, Photomed. Laser Surg. 31:47-53, 2013.
- 14. Wakabayashi, H.; Hamba, M.; Matsumoto, K.; and Tachibana, H.: Effect of irradiation by semiconductor laser on responses evoked in trigeminal caudal neurons by tooth pulp stimulation, Lasers Surg. Med. 13:605-610, 1993.
- 15. Kawasaki, K. and Shimizu, N.: Effects of low-energy laser irradiation on bone remodeling during experimental tooth movement in rats, Laser Surg. Med. 26:282-291, 2000.
- 16. Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; and Brawn, P.: Photobiomodulation accelerates orthodontic alignment in the early phase of treatment, Prog. Orthod. 14:30, 2013.
- 17. Shaughnessy, T.; Kantarci, A.; Kau, C.H.; Skrenes, D.; Skrenes, S.; and Ma, D.: Intraoral photobiomodulation-induced orthodontic tooth alignment: A preliminary study, BMC Oral Health 16:3, 2016.
- 18. Nahas, A.Z.; Samara, S.A.; and Rastegar-Lari, T.A.: Decrowding of lower anterior segment with and without photobiomodulation: A single center, randomized clinical trial, Lasers Med. Sci. 32:129-135, 2017.
- 19. Carvalho-Lobato, P.; Garcia, V.J.; Kasem, K.; Ustrell-Torrent, J.M.; Tallón-Walton, V.; and Manzanares-Céspedes, M.C.: Tooth movement in orthodontic treatment with low-level laser therapy: A systematic review of human and animal studies, Photomed. Laser Surg. 32:302-309, 2014.
- 20. Houle, J.P.; Piedade, L.; Todescan, R. Jr.; and Pinheiro, F.H.: The predictability of transverse changes with Invisalign, Angle Orthod. 87:19-24, 2017.
- 21. Gkantidis, N.; Mistakidis, I.; Kouskoura, T.; and Pandis, N.: Effectiveness of non-conventional methods for accelerated orthodontic tooth movement: A systematic review and meta-analysis, J. Dent. 42:1300-1319, 2014.
- 22. Simon, M.; Keilig, L.; Schwarze, J.; Jung, B.A.; and Bourauel, C.: Treatment outcome and efficacy of an aligner technique—Regarding incisor torque, premolar derotation and molar distalization, BMC Oral Health 14:68, 2014.
- 23. Genc, G.; Kocadereli, I.; Tasar, F.; Kilinc, K.; El, S.; and Sarkarati, B.: Effect of low-level laser therapy (LLLT) on orthodontic tooth movement, Lasers Med. Sci. 28:41-47, 2013.
- 24. Sousa, M.V.; Scanavini, M.A.; Sannomiya, E.K.; Velasco, L.G.; and Angelieri, F.: Influence of low-level laser on the speed of orthodontic movement, Photomed. Laser Surg. 29:191-196, 2011.
- 25. Pratt, M.C.; Kluemper, G.T.; and Lindstrom, A.F.: Patient compliance with orthodontic retainers in the postretention phase, Am. J. Orthod. 140:196-201, 2011.
- 26. Schaefer, I. and Braumann, B.: Halitosis, oral health and quality of life during treatment with Invisalign and the effect of a low-dose chlorhexidine solution, J. Orofac. Orthop. 71:430-431, 2010.
- 27. Nimeri, G.; Kau, C.H.; Corona, R.; and Shelly, J.: The effect of photobiomodulation on root resorption during orthodontic treatment, Clin. Cosmet. Investig. Dent. 6:1-8, 2014.






