THE CUTTING EDGE
Invisalign Treatment Accelerated by Photobiomodulation
This column is compiled by JCO Technology Editor W. Ronald Redmond, DDS, MS. To help keep our readers on The Cutting Edge, Dr. Redmond will spotlight a particular area of orthodontic technology every few months. Your suggestions for future subjects or authors are welcome.
This month's Cutting Edge article describes accelerated orthodontic treatment using photobiomodulation (PBM), a low-level light therapy that has been shown to accelerate bone and connective-tissue metabolism for wound healing in medicine. One commercially available PBM device, OrthoPulse*, uses light-emitting diodes (LEDs) that produce 850 nanometers of light (very near the infrared spectrum), offering a safer mode of treatment than with laser light.
In the case presented here, OrthoPulse was used in combination with Invisalign** to treat a difficult malocclusion. Although the ClinCheck** was designed for the usual two-week aligner wear period, PBM allowed the aligners to be changed every three days. The patient was instructed to use the appliance for five minutes per arch each day; cooperation was monitored remotely using a unique app in the OrthoPulse charging base that communicates through the Internet with the doctor's office. The authors believe the patient's ability to change aligners every three days improved her compliance. Aligner fit was checked at each appointment to ensure the teeth were tracking properly. In this way, an Invisalign treatment originally planned for 92 weeks (46 sets of aligners) was completed in six months.
Similar articles from the archive:
I hope you find this article as professionally stimulating as I did.
WRR
Invisalign Treatment Accelerated by Photobiomodulation
Several methods have been proposed to accelerate orthodontic treatment and thus reduce treatment time. Surgical injury of the cortical bone through selective alveolar decortication, piezociususion,1 and corticision2 have been studied in animal models and human case reports, and vibrational forces have been investigated in case series.3-6 Although these methods have been found to increase the rate of tooth movement, some have also been associated with patient discomfort and other unfavorable effects.2 PBM is a noninvasive approach that has been shown to produce accelerated orthodontic tooth movement in animal7,8 and human models,9-14 with no root resorption or other adverse side effects.15
Also known as low-level light therapy, PBM is the application of visible-to-infrared light for the purpose of inducing biological stimulatory and inhibitory effects in target cells. It is generally accepted that PBM acts on mitochondria and is mainly mediated by cytochrome c oxidase (CCO), the terminal enzyme of the respiratory chain.16-18 As CCO absorbs light in the near-infrared range, photons excite wavelength-specific chromophores to initiate signaling pathways. The activation of CCO directly increases adenosine triphosphate (ATP) production.18 CCO has also been found to dissociate from inhibitory nitric oxide, a free radical and an important signaling molecule, to further increase ATP bioavailability.19 When released, nitric oxide participates in biological processes such as vasodilation and angiogenesis to provide analgesic effects.20,21 PBM has been shown to promote bone22-24 and connective tissue remodeling,25-27 probably due to the involvement of reactive oxygen species produced by mitochondria.
The OrthoPulse device utilizes PBM by directing continuous, near-infrared LEDs, at a wavelength of 850 nanometers, to the gingivae surrounding the dental roots. Compared to lasers, LEDs are non-coherent, safer, and less expensive.
The following case report demonstrates how PBM can be used to reduce treatment time in Invisalign patients.
Case Report
A 40-year-old female presented with an anterior open bite, a crossbite of the upper right lateral incisor, upper and lower anterior crowding, a V-shaped maxillary arch, a Class I malocclusion, and lip tension on closure (Fig. 1).

Fig. 1 40-year-old female patient with upper and lower anterior crowding, anterior open bite, and upper right lateral incisor in crossbite before treatment.
The ClinCheck simulation involved the use of 46 sets of aligners, including overcorrection by aligners 41-46 (Fig. 2A). With each pair of aligners planned for the usual two weeks of wear,28,29 the projected treatment time was 21 months.
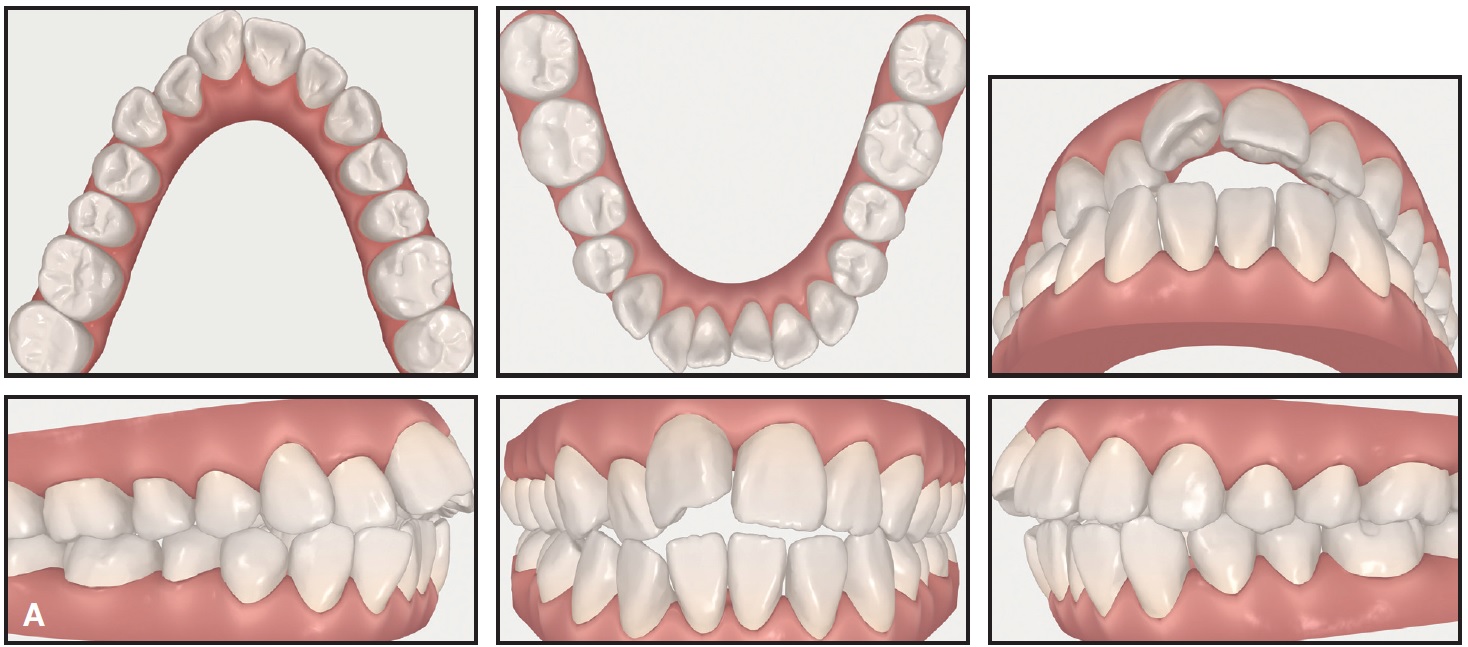
Fig. 2 ClinCheck** records. A. Pretreatment.
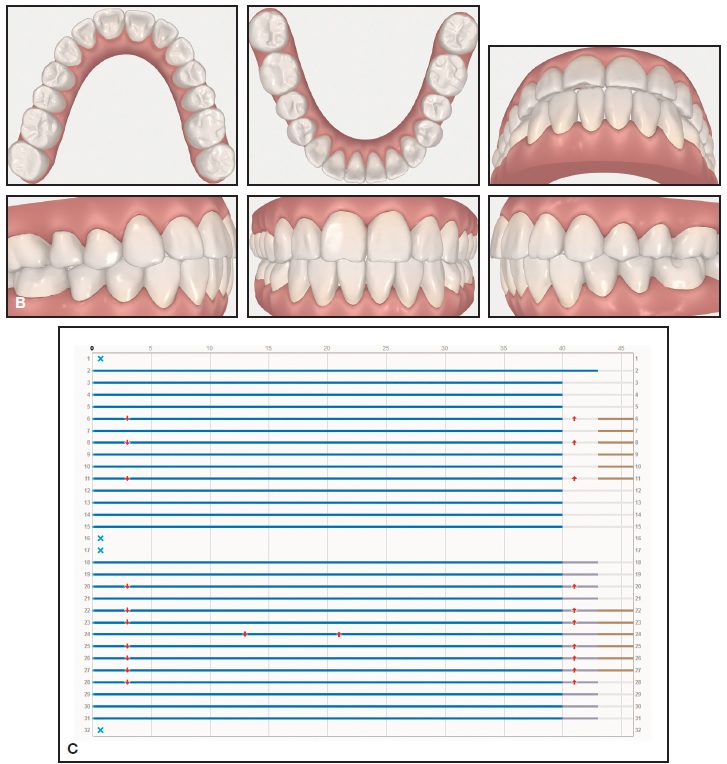
Fig. 2 (cont.) ClinCheck records. B. Projected post-treatment. C. Staging showing simultaneous movement of upper and lower arches with 46 sets of aligners over 21 months of treatment.
According to the treatment plan, interproximal reduction was performed first to alleviate crowding, adding .2mm of space at the upper second molars, .3mm at the upper first molars, .5mm at the upper second premolars, .7mm at the upper first premolars, and .6mm at the upper canines.
The patient wore the first and second sets of aligners for 14 days each (Fig. 3). When she was scheduled to receive her third aligners, we bonded attachments to optimize tooth movement and ensure that the aligners were closely compatible with the dentition, as is critical in this type of treatment (Fig. 4).

Fig. 3 Invisalign** fitting check at initial appointment.

Fig. 4 After 30 days of treatment, optimized attachments placed for third set of aligners.
An OrthoPulse device was delivered, and the patient was instructed to change aligners every three days. The OrthoPulse was to be worn 10 minutes per day (five minutes per arch), with the patient biting down lightly on the device (Fig. 5). Even if the patient did not report to the practice, her compliance was monitored through the use of an accompanying app (Fig. 6).
Each Invisalign tray is programmed to move the teeth .25mm. If the teeth did not move as expected when the aligners were replaced every three days, we would have seen gaps between the aligners and teeth. This did not occur, and the patient did not report any pain or excessive pressure when changing aligners more frequently, indicating a good fit (Fig. 7).

Fig. 5 OrthoPulse* used for five minutes per arch each day.
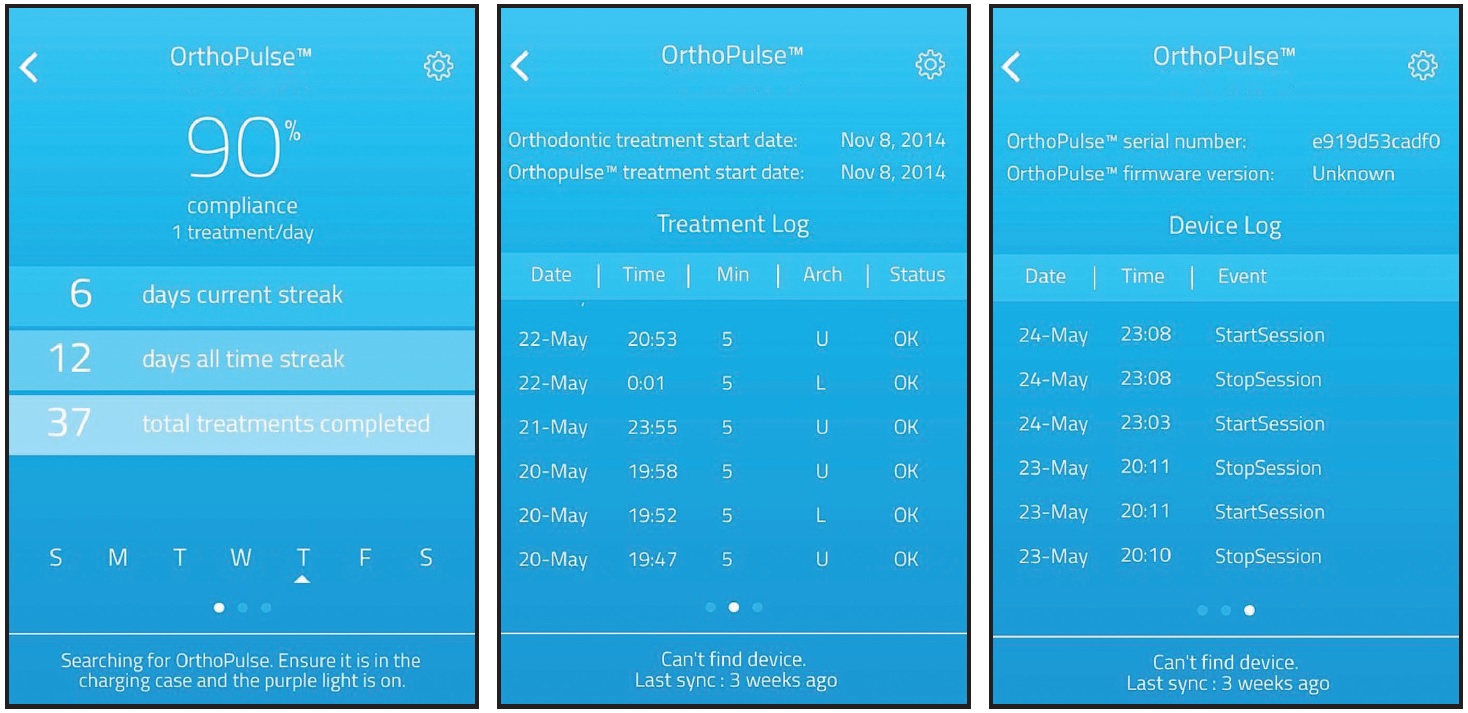
Fig. 6 OrthoPulse app used to monitor patient compliance remotely.
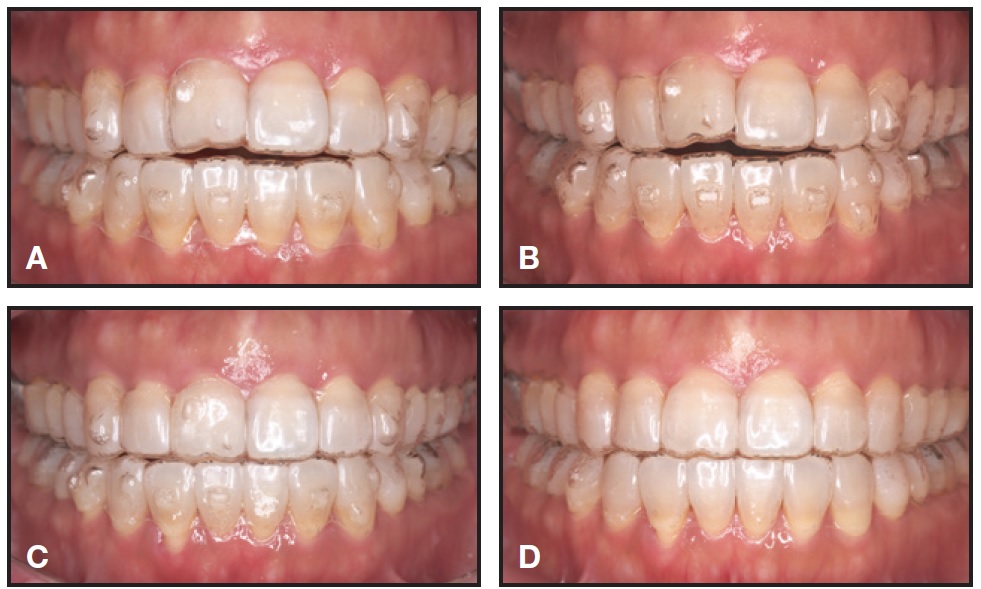
Fig. 7 A. After 51 days of treatment. B. After 109 days of treatment. C. After 139 days of treatment. D. Final overcorrection aligners, after 157 days of treatment.
Total treatment time was six months (Fig. 8). The upper anterior teeth were then recontoured using OptraPol*** (Fig. 9).

Fig. 8 A. Patient after six months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
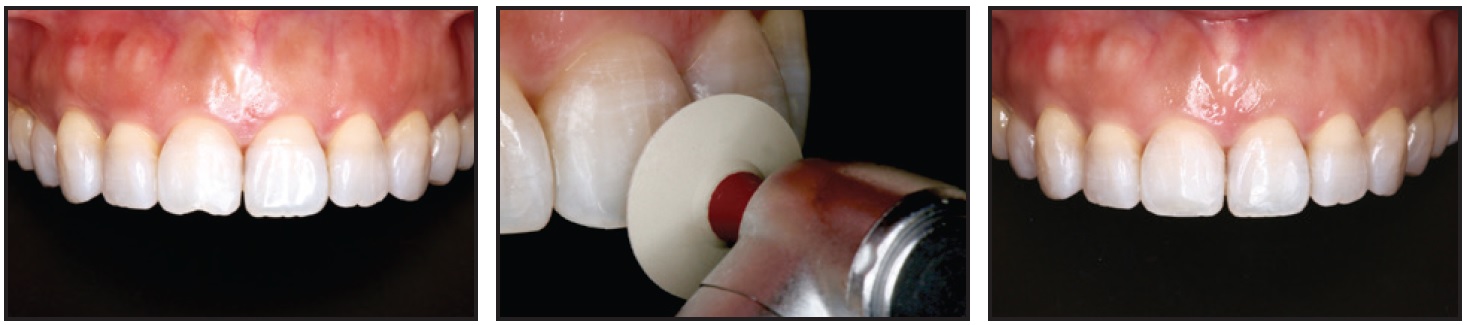
Fig. 9 Recontouring of upper anterior teeth after completion of treatment.
Discussion
The Invisalign system, originally intended for the resolution of mild crowding, is now being applied to more complex orthodontic cases.30-34 Although the company recommends that each set of aligners be worn for 14 days (at least 20 hours a day), an optimal period for aligner wear has yet to be established. Some clinicians may instruct their patients to change aligners more frequently - even without any attempt to accelerate treatment. The case shown here demonstrates the ability to maintain aligner tracking throughout treatment and reach a successful outcome while changing aligners every three days, by means of accelerated treatment with OrthoPulse.
Since clear aligners are removable, patient compliance is especially important. The use of a simple, non-invasive device such as OrthoPulse can help improve compliance, motivation, and satisfaction by accelerating orthodontic tooth movement. The orthodontist also benefits as more treatment time is freed up for accomplishing proper occlusal seating, minor rotations, and other adjustments during the final stage of treatment. The clinician's skill and experience in using accelerated-treatment methods will become increasingly important as we move into a new era of orthodontic correction.
FOOTNOTES
- *Registered trademark of Biolux Research Ltd., Vancouver, British Columbia, Canada; www.bioluxresearch.com.
- **Registered trademark of Align Technology, Inc., Santa Clara, CA; www.aligntech.com.
- ***Ivoclar Vivadent, Inc., Amherst, NY; www.ivoclarvivadent.us.
REFERENCES
- 1. Brugnami, F.; Caiazzo, A.; and Dibart S.: Lingual orthodontics: Accelerated realignment of the “social six” with piezocision, Compend. Cont. Ed. Dent. 34:608-610, 2013.
- 2. Camacho, A.D. and Velásquez Cujar, S.A.: Dental movement acceleration: Literature review by an alternative scientific evidence method, World J. Methodol. 4:151-162, 2014.
- 3. Kau, C.H.; Nguyen, J.T.; and English, J.D.: The clinical evaluation of a novel cyclical force generating device in orthodontics, Orthod. Pract. U.S. 1:10-15, 2010.
- 4. Woodhouse, N.R.; DiBiase, A.T.; Johnson, N.; Slipper, C.; Grant, J.; Alsaleh, M.; Donaldson, A.N.; and Cobourne, M.T.: Supplemental vibrational force during orthodontic alignment: A randomized trial, J. Dent. Res. 94:682-689, 2015.
- 5. Orton-Gibbs, S. and Kim, N.Y.: Clinical experience with the use of pulsatile forces to accelerate treatment, J. Clin. Orthod. 49:557-573, 2015.
- 6. Bowman, S.J.: The effect of vibration on the rate of leveling and alignment, J. Clin. Orthod. 48:678-688, 2014.
- 7. Ekizer, A.; Uysal, T.; Güray, E.; and Akkuş, D.: Effect of LED-mediated-photobiomodulation therapy on orthodontic tooth movement and root resorption in rats, Lasers Med. Sci. 30:779-785, 2015.
- 8. Goulart, C.S.; Nouer, P.R.; Mouramartins, L.; Garbin, I.U.; and de Fátima Zanirato Lizarelli, R.: Photoradiation and orthodontic tooth movement: Experimental study on canines, Photomed. Laser Surg. 24:192-196, 2006.
- 9. Kau, C.H.; Kantarci, A.; Shaughnessy, T.; Vachiramon, A.; Santiwong, P.; de la Fuente, A.; Skrenes, D.; Ma, D.; and Brawn, P.: Photobiomodulation accelerates orthodontic alignment in the early phase of treatment, Prog. Orthod. 14:30, 2013.
- 10. Cruz, D.R.; Kohara, E.K.; Ribeiro, M.S.; and Wetter, N.U.: Effects of low-intensity laser therapy on the orthodontic movement velocity of human teeth: A preliminary study, Lasers Surg. Med. 35:117-120, 2004.
- 11. Genc, G.; Kocadereli, I.; Tasar, F.; Kilinc, K.; El, S.; and Sarkarati, B.: Effect of low-level laser therapy (LLLT) on orthodontic tooth movement, Lasers Med. Sci. 28:41-47, 2013.
- 12. Sousa, M.V.; Scanavini, M.A.; Sannomiya, E.K.; Velasco, L.G.; and Angelieri, F.: Influence of low-level laser on the speed of orthodontic movement, Photomed. Laser Surg. 29:191-196, 2011.
- 13. Limpanichkul, W.; Godfrey, K.; Srisuk, N.; and Rattanayatikul, C.: Effects of low-level laser therapy on the rate of orthodontic tooth movement, Orthod. Craniofac. Res. 9:38-43, 2006.
- 14. Youssef, M.; Ashkar, S.; Hamade, E.; Gutknecht, N.; Lampert, F.; and Mir, M.: The effect of low-level laser therapy during orthodontic movement: A preliminary study, Lasers Med. Sci. 23:27-33, 2008.
- 15. Nimeri, G.; Kau, C.H.; Corona, R.; and Shelly, J.: The effect of photobiomodulation on root resorption during orthodontic treatment, Clin. Cosmet. Investig. Dent. 6:1-8, 2014.
- 16. Karu, T.: Mitochondrial mechanisms of photobiomodulation in context of new date about multiple roles of ATP, Photomed. Laser Surg. 28:159-160, 2010.
- 17. Chung, H.; Dai, T.; Sharma, S.K.; Huang, Y.Y.; Carroll, J.D.; and Hamblin, M.R.: The nuts and bolts of low-level laser (light) therapy, Ann. Biomed. Eng. 40:516-533, 2012.
- 18. Karu, T.I. and Afanas’eva, N.I.: Cytochrome c oxidase as the primary photoacceptor upon laser exposure of cultured cells to visible and near IR-range light [in Russian], Dokl. Akad. Nauk 342:693-695, 1995.
- 19. Karu, T.I.; Pyatibrat, L.V.; Kolyakov, S.F.; and Afanasyeva, N.I.: Absorption measurements of a cell monolayer relevant to phototherapy: Reduction of cytochrome c oxidase under near IR radiation, J. Photochem. Photobiol. B. 81:98-106, 2005.
- 20. Karu, T.I.; Pyatibrat, L.V.; and Afanasyeva, N.I.: Cellular effects of low power laser therapy can be mediated by nitric oxide, Lasers Surg. Med. 36:307-314, 2005.
- 21. Poyton, R.O. and Ball, K.A.: Therapeutic photobiomodulation: Nitric oxide and a novel function of mitochondrial cytochrome c oxidase, Discov. Med. 11:154-159, 2011.
- 22. Pinheiro, A.L. and Gerbi, M.E.: Photoengineering of bone repair processes, Photomed. Laser Surg. 24:169-178, 2006.
- 23. Bouvet-Gerbettaz, S.; Merigo, E.; Rocca, J.P.; Carle, G.F.; and Rochet, N.: Effects of low-level laser therapy on proliferation and differentiation of murine bone marrow cells into osteoblast and osteoclasts, Lasers Surg. Med. 41:291-297, 2009.
- 24. Lirani-Galvão, A.P.; Jorgetti, V.; and da Silva, O.L.: Comparative study of how low-level laser therapy and low-intensity pulsed ultrasound affect bone repair in rats, Photomed. Laser Surg. 24:735-740, 2006.
- 25. Chen, A.C.; Arany, P.R.; Huang Y.Y.; Tomkinson, E.M.; Sharma, S.K.; Kharwal, G.B.; Saleem, T.; Mooney, D.; Yull, F.E.; Blackwell, T.S.; and Hamblin, M.R.: Low-level laser therapy activates NF-kB via generation of reactive oxygen species in mouse embryonic fibroblasts, PLoS One 6:e22453, 2011.
- 26. Almeida-Lopes, L.; Rigau, J.; Zãngaro, R.A.; Guidugli-Neto, J.; and Jaeger, M.M.: Comparison of the low level laser therapy effects on cultured human gingival fibroblasts proliferation using different irradiance and same fluence, Lasers Surg. Med. 29:179-184, 2001.
- 27. Hawkins, D.; Houreld, N.; and Abrahamse, H.: Low level laser therapy (LLLT) as an effective therapeutic modality for delayed wound healing, Ann. N.Y. Acad. Sci. 1056:486-493, 2005.
- 28. Bowman, S.J.; Celenza, F.; Sparaga, J.; Papadopoulos, M.A.; Ojima, K.; and Lin, J.C.: Creative adjuncts for clear aligners, Part 3: Extraction and interdisciplinary treatment, J. Clin. Orthod. 49:249-262, 2015.
- 29. Ojima, K.; Dan, C.; Nishiyama, R.; Ohtsuka, S.; and Schupp, W.: Accelerated treatment with Invisalign, J. Clin. Orthod. 48:487-499, 2014.
- 30. Schupp, W.; Haubrich, J.; and Neumann, I.: Treatment of anterior open bite with the Invisalign system, J. Clin. Orthod. 44:501-507, 2010.
- 31. Boyd, R.L.; Miller, R.J.; and Vlaskalic, V.: The Invisalign system in adult orthodontics: Mild crowding and space closure cases, J. Clin. Orthod. 34:203-212, 2000.
- 32. Schupp, W.; Haubrich, J.; and Neumann, I.: Class II correction with the Invisalign system, J. Clin. Orthod. 44:28-35, 2010.
- 33. Castroflorio, T.; Garino, F.; Lazzaro, A.; and Debernardi, C.: Upper-incisor root control with Invisalign appliances, J. Clin. Orthod. 47:346-351, 2013.
- 34. Vlaskalic, V. and Boyd, R.: Orthodontic treatment of a mildly crowded malocclusion using the Invisalign System, Aust. Orthod. J. 17:41-46, 2001.





