Clinical Experience with the Use of Pulsatile Forces to Accelerate Treatment
Protracted treatment is one of the greatest challenges in orthodontics. As treatment lengthens, the patient is increasingly exposed to oral-health risks including root resorption, caries, and periodontal disease. Patient satisfaction may also decline as treatment is extended. Uribe and colleagues, evaluating the perceptions of parents, patients, and orthodontists on the need to accelerate treatment, found that 55% of adolescent patients felt their treatment was too long.1 Seventy percent of the responding orthodontists said they would be interested in clinical procedures that would reduce treatment time. The invasiveness of each procedure was inversely related to acceptance of that treatment for both orthodontists and patients.
The purpose of this article is to report the first extensive single-center experience with a new pulsatile force (PF) delivery device: AcceleDent*, a noninvasive accessory designed to accelerate orthodontic tooth movement.
Effects of Pulsatile Forces on Tooth Movement
Using a cranial-suture model developed by Meikle and colleagues,2 Kopher and Mao assessed PFs of 5N peak magnitude at 1Hz in rabbits,3 Peptan and colleagues evaluated PFs of 1N at 8Hz in rabbits,4 and Vij and Mao tested PFs of 300mN at 4Hz in rats.5 Taken together, these three studies indicated that PFs between 1Hz and 8Hz and forces ranging from .3N to 5N would increase sutural growth (a proxy for tooth movement), with efficacy increasing as the frequency increased. Rates of movement varied depending on the methodology, but increases of 2.5 times faster movement were commonly achieved with vibration. These studies were the basis for development of the AcceleDent device, which received a CE mark in 2009 and has been cleared by the U.S. Food and Drug Administration since 2012.
Similar articles from the archive:
In another study, Nishimura and colleagues measured the effects of vibration on tooth movement in rats.6 The subjects underwent "standard orthodontics" using a spring that applied force between the rat molars. Vibration at a frequency of 60Hz was delivered to the molars through a separate apparatus for 10 minutes on days 1, 7, and 14 of the 21-day experiment. Compared to the static-force group, the group that received vibration showed significantly faster tooth movement and a trend toward decreased root resorption.
Two recent studies by Liu further support the hypothesis that mechanical vibration enhances orthodontic tooth movement. In the first study, mice were divided into four groups: control, vibration only, orthodontic tooth movement, and orthodontic tooth movement plus vibration.7 The tooth movement was generated by an initial force of 20g; mechanical vibration was applied at a frequency of 4Hz for five minutes on days 0, 3, 6, 9, 12, 15, 18, and 21. Unlike any of the other groups, the orthodontics-plus-vibration group demonstrated 40% more tooth movement on the vibrated side vs. the non-vibrated side. In Liu's second study, mice were again divided into four groups: control, mechanical vibration, orthodontic tooth movement, and orthodontic tooth movement plus mechanical vibration.8 Force and frequency were applied in the same manner as in the initial study, but the evaluation period was increased to 27 days. Fluorescent markers were used to measure new bone formation. Results were similar to those of the first study: there was no difference in bone formation or resorption between the control and the vibration-only groups, but the orthodontics-plus-vibration group showed a 71% increase in the amount of bone formation compared to orthodontic tooth movement alone (p = .021).
Recent clinical studies have corroborated these results. Kau and colleagues, using an AcceleDent prototype in 14 patients, reported 2.1mm of tooth movement per month in the mandibular arch (twice the usual rate) and 3mm per month in the maxillary arch.9 Bowman observed a 30% reduction in treatment time for leveling and alignment in 30 adolescent Class II nonextraction patients treated with AcceleDent, compared to two control groups of 37 and 50 patients.10
Materials and Methods
Dr. Orton-Gibbs is the lead clinician of a relatively small private practice, treating 220-270 active patients with a full range of orthodontic appliances. In November 2009, the practice began introducing AcceleDent to a few patients. After the first six months, AcceleDent was offered at the initial consultation to any patient who met the following criteria:
A total of 117 patients opted to use AcceleDent as an adjunct to their treatment between November 2009 and May 2014. The following factors were recorded for each patient:
1. Age at start of treatment and sex.
2. Appliance type.
3. Acceptance rates for all patients offered AcceleDent during a three-month period, and also for all aligner patients and all surgical-orthodontic patients during the entire study period.
4. Preferred place of AcceleDent use.
5. Reduction in treatment time for fixed-appliance and aligner cases.
6. Need for refinement stages in aligner cases.
For all patients treated during this period, the expected treatment time was estimated before the clinician knew whether the patient wanted to use AcceleDent, based on more than 25 years of clinical experience. The accuracy of predicted treatment time in fixed-appliance patients without PF was verified by comparing actual against predicted treatment time in a consecutively treated control group matched to the PF group of patients, also consecutively treated.
Descriptive statistical methods were used to summarize the data. The level of statistical significance was set at p < .05. Mean differences between groups were determined using paired t-tests.
Results
1. Age and sex: The 117 patients accepting AcceleDent had a mean starting age of 31 years, six months (Fig. 1A). Sixty-four percent of the patients were female; 76% were adults.
2. Appliance type: Of the 117 patients, 52 (45%) chose to use ceramic brackets, 19 (16%) metal brackets, 19 (16%) lingual brackets, 16 (14%) clear aligners, and 11 (9%) removable expansion appliances (Fig. 1B).
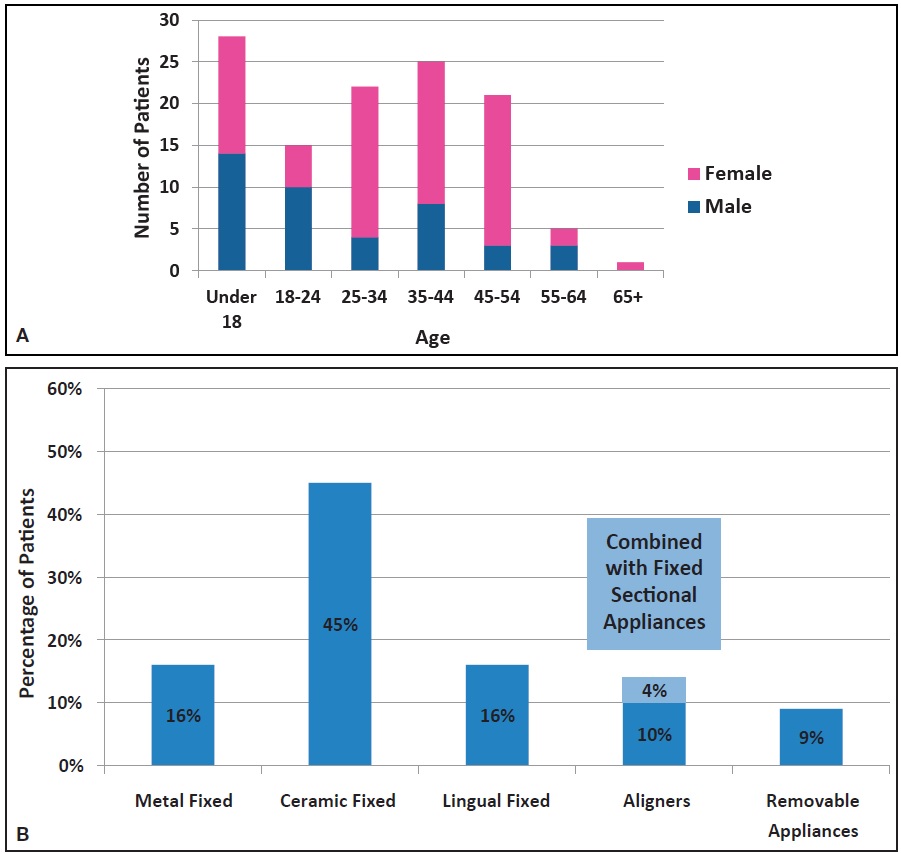
Fig. 1 Sample of 117 AcceleDent* patients. A. Age at start of treatment and sex. B. Appliance type.
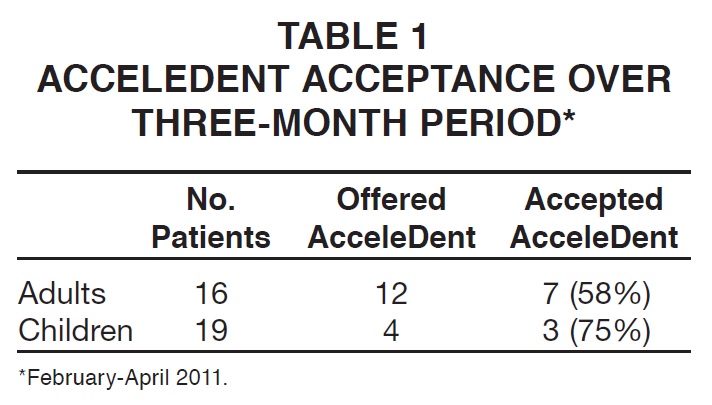
3. Acceptance rates: The acceptance of AcceleDent when recommended with orthodontic treatment was documented over a three-month period (February-April 2011). Of the 35 patients who accepted treatment during that time, AcceleDent was offered to 16 patients (45%) and accepted by 10, resulting in an overall 63% acceptance rate. Because of the selection criteria outlined above, AcceleDent was offered to a higher percentage of adults than of children (Table 1).
Between May 2010 and May 2014, 13 of 34 patients (38%) opting for aligner treatment chose to use AcceleDent and had completed treatment. Between September 2009 and March 2012, 15 of 18 patients (83%) needing orthodontics with orthognathic surgery chose to use AcceleDent.
4. Preferred place of use: The most popular place (47%) for using AcceleDent was while watching TV (Fig. 2). Although two respondents said they used AcceleDent while driving, the practice now recommends against using AcceleDent while driving because it may cause a distraction.
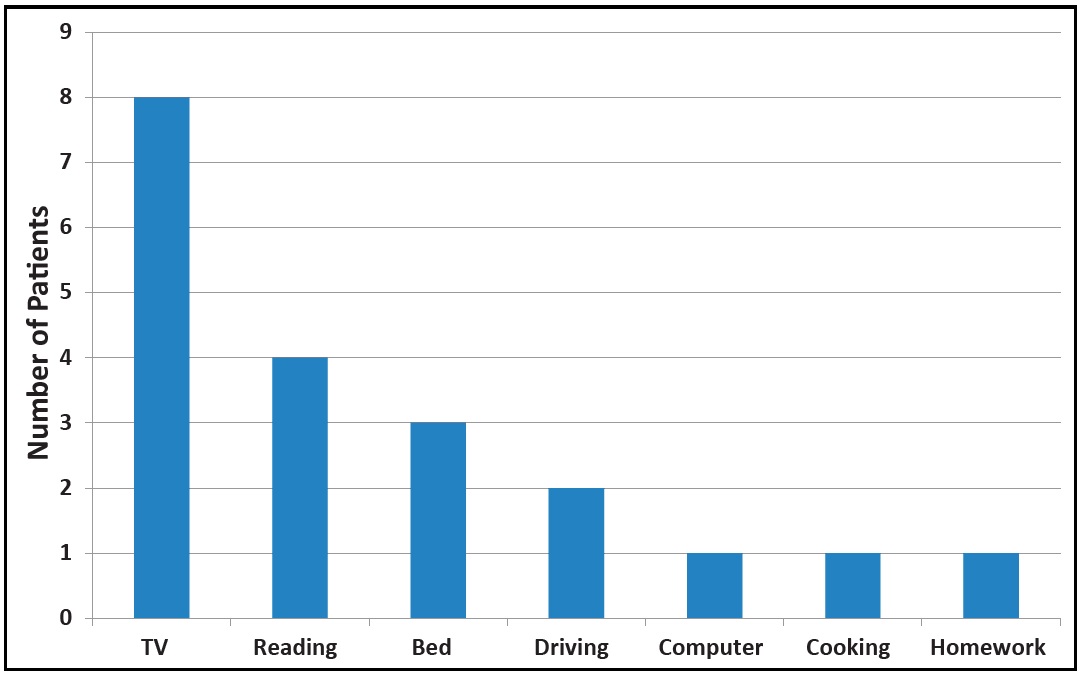
Fig. 2 Preferred place of AcceleDent use of first 22 patients (17 respondents, three of whom listed two preferred places).
5. Reduction in treatment time: Predicted treatment times were estimated in the first 14 consecutively treated fixed-appliance cases with PF and 14 without PF. Each group included 14 skeletally mature patients who had completed growth (11 buccal and three lingual cases); each group included six orthognathic patients. Predicted treatment times were between 18 and 24 months, with no significant difference in predicted treatment time between the AcceleDent and control patients. In the control group (no PF), the predicted treatment time was accurate to within an average 1.6 months (7%). For the fixed appliance patients using AcceleDent, treatment took an average 12.4 months, 38.2% faster than the average predicted treatment time of 20.0 months (Fig. 3, Table 2). After adjusting for prediction error, the PF group finished 33.5% faster than predicted, saving an average 6.23 months of treatment time.
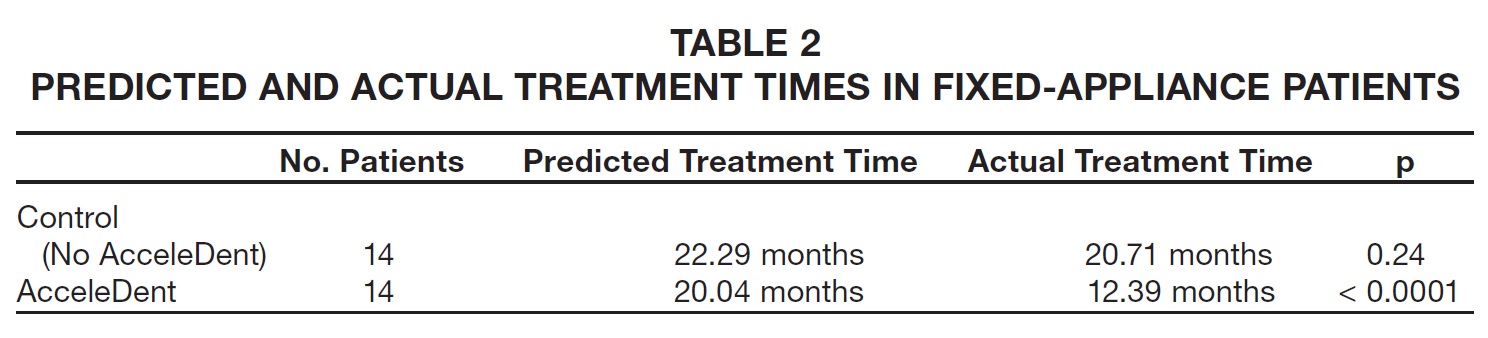
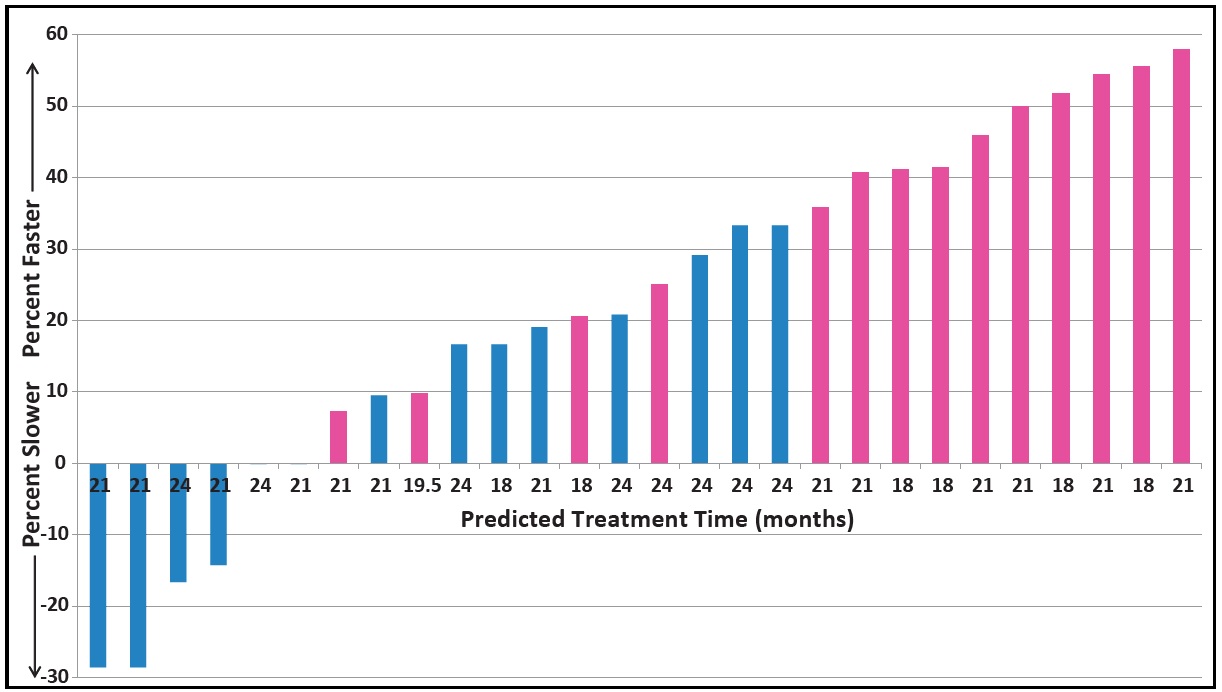
Fig. 3 Slower or faster than predicted treatment times for AcceleDent group (pink, N = 14) compared to control group without AcceleDent (blue, N = 14).
For each of the 13 completed aligner patients who chose to use AcceleDent between May 2010 and May 2014, the required number of aligners was determined, and the treatment time was estimated by multiplying that number by the customary two weeks per aligner. This is a conservative estimate because patients will sometimes use the same aligners longer than two weeks (for example, when on vacation), and appointments may not coincide exactly with aligner change dates, further lengthening treatment. Patients using PF were asked to change their aligners as they became passive, which they reported to be seven to 10 days. Treatment time was an average 37.2% faster than the conservative estimate for each case, with a range of 5-55% faster (Fig. 4).
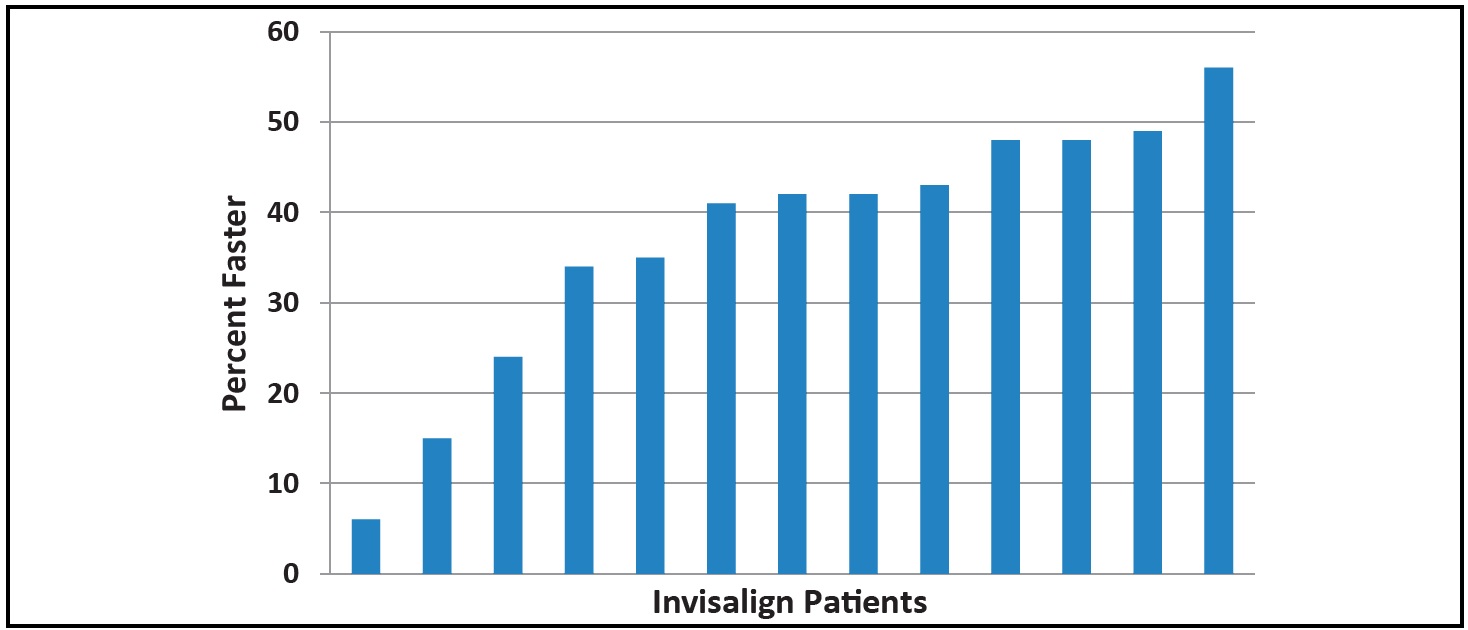
Fig. 4 Treatment times for Invisalign** patients with AcceleDent (N = 13) compared to conservative estimates.
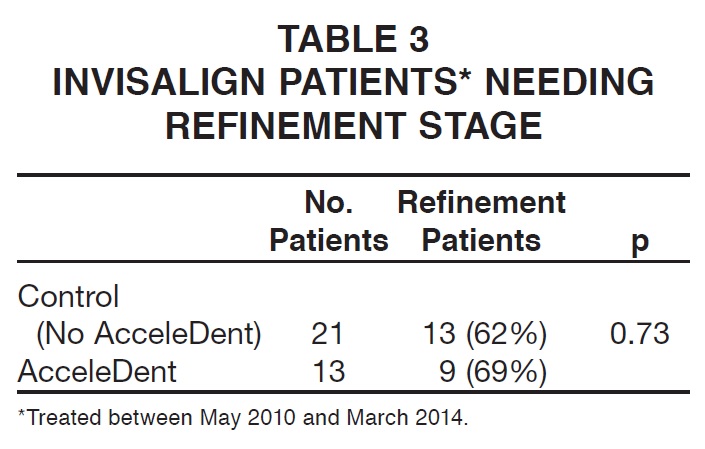
6. Need for refinement aligners: According to Fisher's exact test, there was no significant difference in the percentage of PF patients needing refinement aligners compared to those not using PF (Table 3).
Discussion
Age and acceptance rates: In our sample, the group most likely to choose AcceleDent was the surgical-orthodontic patients (83%). The practice does not automatically recommend AcceleDent to every patient; more adults than children are offered the device. If a patient with a relatively short estimated treatment time asks to use AcceleDent, the benefits are discussed. The extra cost of the unit and the required commitment need to be worth the potential reduction in treatment time. In our experience, when this device is given to patients rather than purchased, it is not valued as much and, therefore, cooperation is often poorer.
Appliance type: Even for patients using cosmetic appliances such as aligners or lingual appliances, speeding up treatment may be an attractive option. One unexpected consequence of offering AcceleDent was that some adults who had initially requested aligner treatment opted for ceramic braces with AcceleDent. This alternative is more cost-effective and more accurate than aligners, and treatment can be completed within a more manageable time frame of 10-16 months rather than 15-24 months.
Preferred place of use: Patients are more successful when they make using AcceleDent part of their daily routine.
Reduction in treatment time: Although the matched sample of fixed-appliance cases was relatively small (N = 14), the average savings of more than six months over a 20-month estimated treatment time was statistically significant (p < .0001).
For patients choosing to use aligners with PF, the 37% reduction in treatment time shown here would be a cautious estimate, since most patients without PF do not follow an exact biweekly aligner-change schedule. Some practitioners are currently prescribing aligners to be worn for less than two weeks even without PF; further clinical trials are needed to establish the optimal rate for aligner changes with and without AcceleDent.
Need for refinement aligners: A number of clinicians have reported in personal communications that their patients track better using AcceleDent, so that fewer case refinements are needed. We did not find that to be true in our sample. The practice asks every aligner patient, with or without PF, to bite for 10 minutes per day on a small flexible block (chewie) for the first day or two each time the aligners are changed. Clinicians who do not use this technique may see more positive effects from biting on the AcceleDent mouthpiece.
Clinical Management
The best bite profile (open, flat, or deep) should be chosen from the AcceleDent trial tray; it can be sterilized for reuse. With a more complex malocclusion, there may not be contact on every tooth at the beginning of treatment, but Liu and colleagues showed that the vibrations are transmitted through the archwire and alveolus.11
The mouthpiece may be too wide posteriorly for some patients. In that case, the end corners can be rounded off using a non-serrated scissor (Fig. 5A). The mouthpiece may also be too long for smaller patients (particularly younger children), so that the harder inner core may need to be shortened. Mauns wire cutters work well for cutting the inner core, and the softer outer layer can be trimmed with scissors (Fig. 5B).
If the mouthpiece flanges are potentially impeding tooth movement, they can be trimmed with a non-serrated scissor (Fig. 5C). The palatal flange may need to be removed when anterior biteplanes are fitted (Fig. 5D). Both lingual flanges should be removed for orthognathic patients so they can insert the mouthpiece after surgery, even with limited opening.
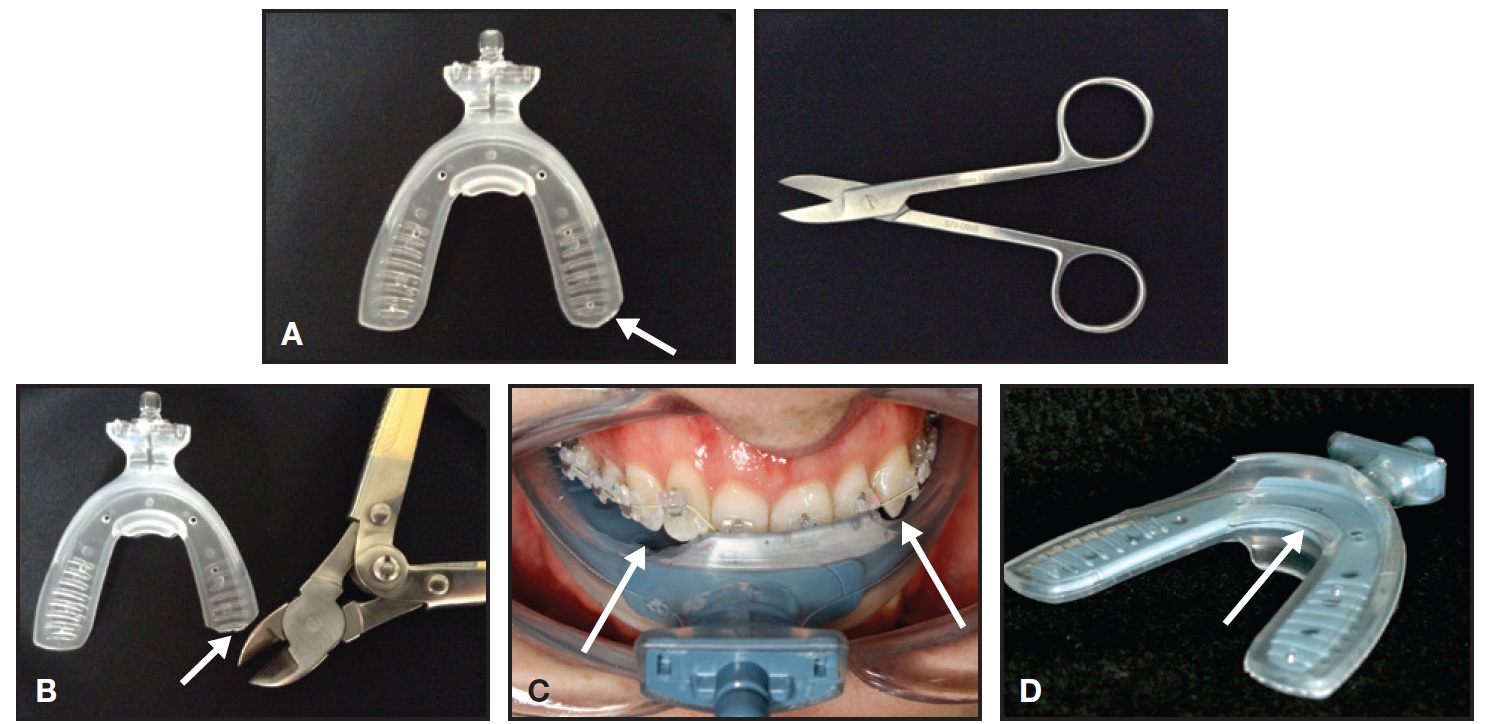
Fig. 5 Trimming of AcceleDent mouthpiece as required in some cases. A. Corner can be rounded off using non-serrated scissor. B. Solid inner core can be shortened with Mauns wire cutter for young patient. C. Buccal flange trimmed to avoid impeding tooth movement. D. Palatal flange trimmed to accommodate biteplanes on central incisors.
PF should be used concurrently with active force systems such as aligners, elastics, and removable appliances. The device should be used only 20 minutes per day; patients should be discouraged from using the device more frequently, because there is no evidence to support increased efficacy beyond that point.
Compliance is critical to success. Patient use can be monitored electronically at each appointment by connecting the AcceleDent Aura*** device to the computer with the integrated USB connector. Although cooperation is usually good, treatment objectives can be reviewed and adjusted based on the data. Encouragement should be given if needed, as with any treatment requiring patient compliance. The key for most patients is to incorporate the AcceleDent into a set time or activity each day, such as homework, watching TV, or reading in bed.
In fixed-appliance cases, the faster tooth movement achieved with AcceleDent will shorten the interval between visits for leveling and alignment, as well as in the detailing phase. During space closure, appointments can be maintained at normal intervals as the mechanics continue to be active. Table 4 shows a model for a simple 12 1/2-month leveling and alignment case, assuming full cooperation, good attendance, and no breakages. In this example, a typical 54-week case is reduced to 38 weeks with no difference in the total number of visits.
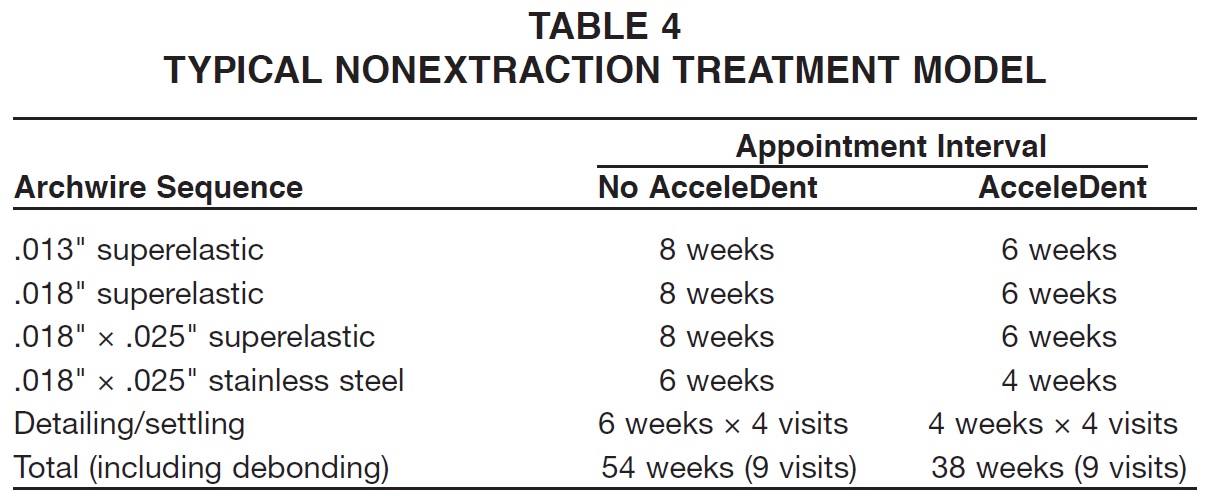
Table 5 shows a more complex model that would normally take 19 1/2 months (84 weeks) to complete. With AcceleDent, this is reduced to 58 weeks (13½ months), with two fewer visits needed (10 instead of 12), thus saving chairtime. These examples reflect the average time savings in our practice.
Treatment with Invisalign** can be highly satisfying for patients using PF; the most compliant patients are finding they can change aligners every seven days instead of every two weeks, halving their treatment time. Ojima and colleagues reported a patient who changed aligners every five days, reducing her predicted treatment time of 30 months to 18 months,12 but we have not seen any patients who can change aligners faster than every seven days.
Case Reports
Case 1 was a 27-year-old female who presented 13½ months before her wedding with a moderate Class II, division 2 relationship, mild crowding in the lower arch, and moderate crowding in the upper right quadrant (Fig. 6).

Fig. 6 Case 1. 27-year-old female patient with moderate Class II, division 2 relationship, mild crowding in lower arch, and moderate crowding in upper right quadrant before treatment. Estimated treatment time: 18 months.
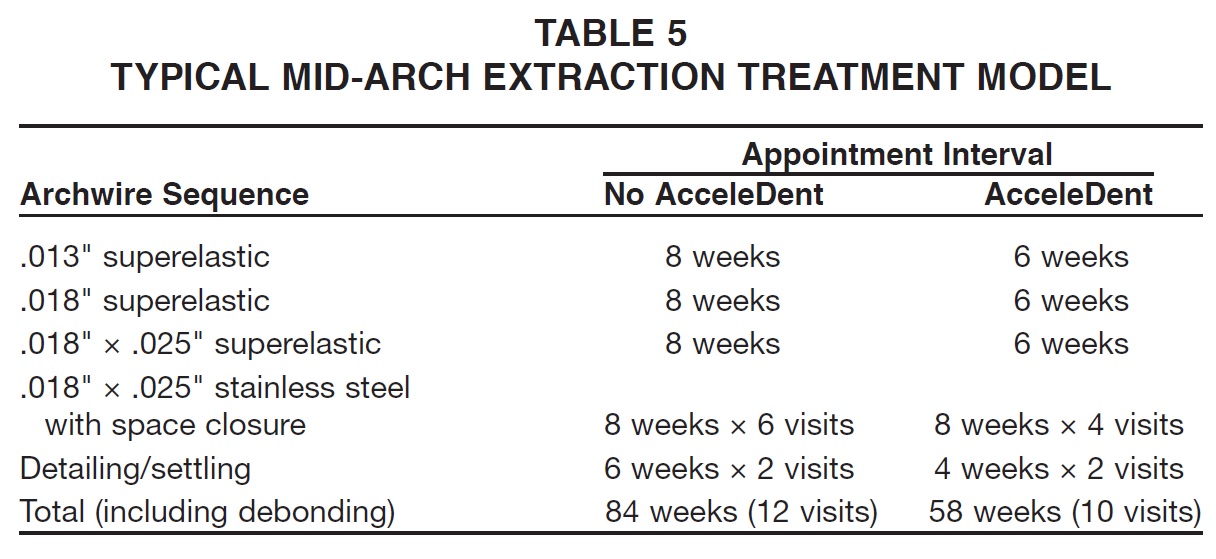
Estimated treatment time was 18 months without PF. The patient chose to use AcceleDent, and nonextraction treatment was planned. Class II elastics were worn to correct the buccal relationship on the right side (Fig. 7).
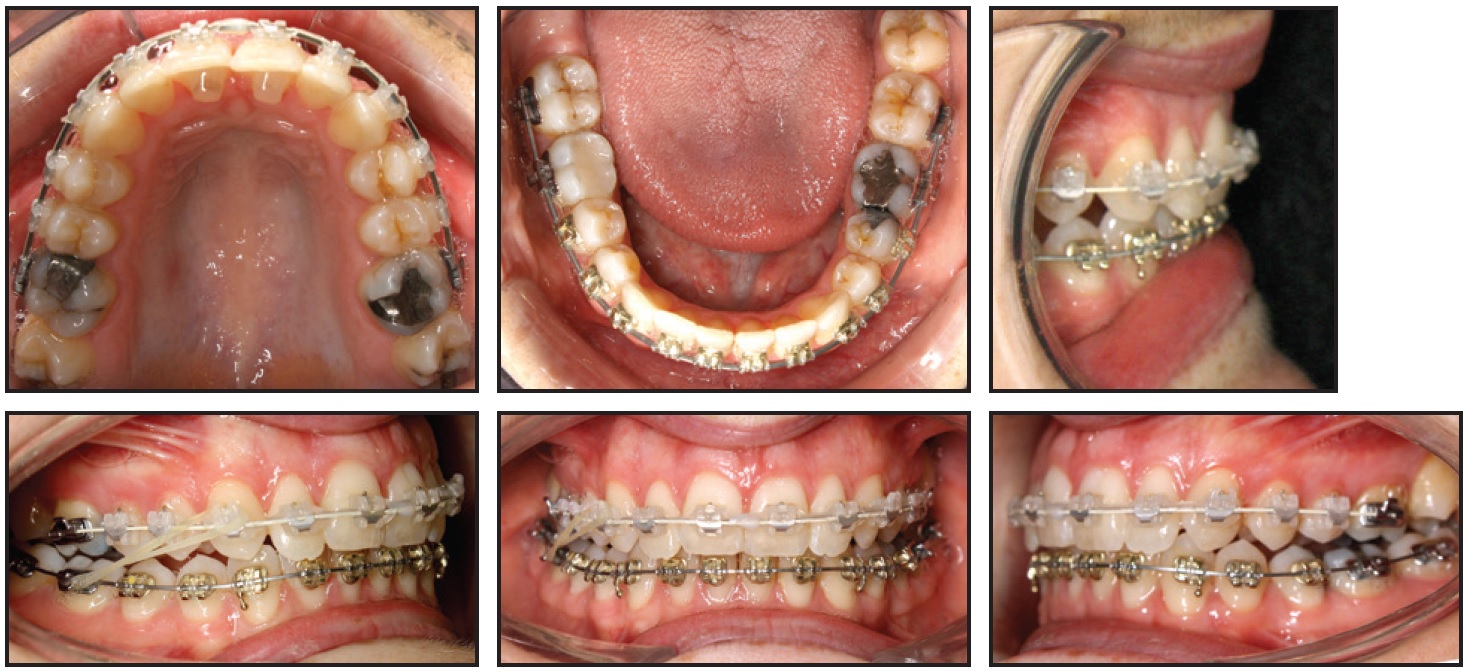
Fig. 7 Case 1. After four and a half months of treatment.
Treatment was completed in 12 1/2 months (Fig. 8).

Fig. 8 Case 1. Completion of treatment in 12½ months.
Case 2 was a 13-year-old male with a deep overbite, bimaxillary retroclination, and insufficient space for the lower left canine to erupt (Fig. 9).

Fig. 9 Case 2. 13-year-old male patient with deep overbite, bimaxillary retroclination, reduced upper-incisor display, and lack of space for lower left canine before treatment. Estimated treatment time: 24 months.
He had a short face with a reduced upperincisor display. Treatment aims included extrusion of the upper incisors, space creation for the lower left canine, and correction of the overbite and occlusion. Estimated treatment time was 24 months without PF. The patient chose to use AcceleDent, and he wore a removable expander with an anterior biteplane for three and a half months to help increase lower facial height and reduce the overbite. Lower fixed appliances were added two weeks into treatment, and upper fixed appliances three months into treatment, by which time the lower left canine space had been fully opened (Fig. 10). Total treatment time was 12 months (Fig. 11).
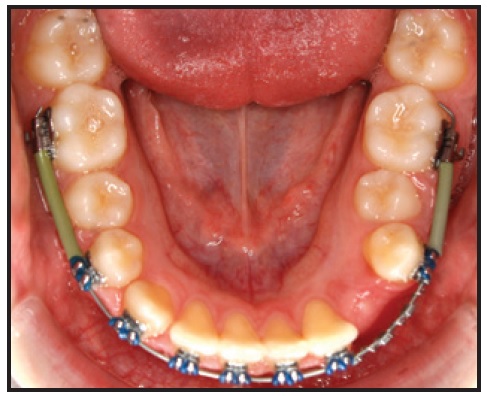
Fig. 10 Case 2. Space creation for lower left canine after two and a half months of lower fixed-appliance wear.

Fig. 11 Case 2. Completion of treatment in 12 months.
Case 3 was a 37-year old female with narrow arches, crowding on a skeletal Class II base, lingually inclined buccal segments, and excessive vertical proportions before treatment (Fig. 12).

Fig. 12 Case 3. 37-year-old female patient with narrow arches, skeletal Class II base, and excessive vertical proportions before treatment. Estimated treatment time: 18 months.
Her estimated treatment time was 18 months. Because she wanted a quick and esthetically discreet option, she chose Invisalign with AcceleDent. We performed 1.3mm of interproximal reduction in the upper anterior region and .6mm of reduction around the lower incisors to create space and prevent gingival spacing. Using 21 sets of aligners, changed weekly, the buccal segments were uprighted to create further space for alignment. The patient reported that she went on vacation for 10 days during treatment and did not take her AcceleDent with her. She tried to change the aligners at the usual weekly interval, but was unable to do so because her teeth hurt too much in the new trays. Total treatment time was five months (Fig. 13).

Fig. 13 Case 3. Completion of treatment in five months, using 21 aligners changed weekly.
Case 4 was a 45-year-old male patient with bimaxillary retroclination, the upper right second premolar in crossbite, and moderate upper and lower crowding (Fig. 14).
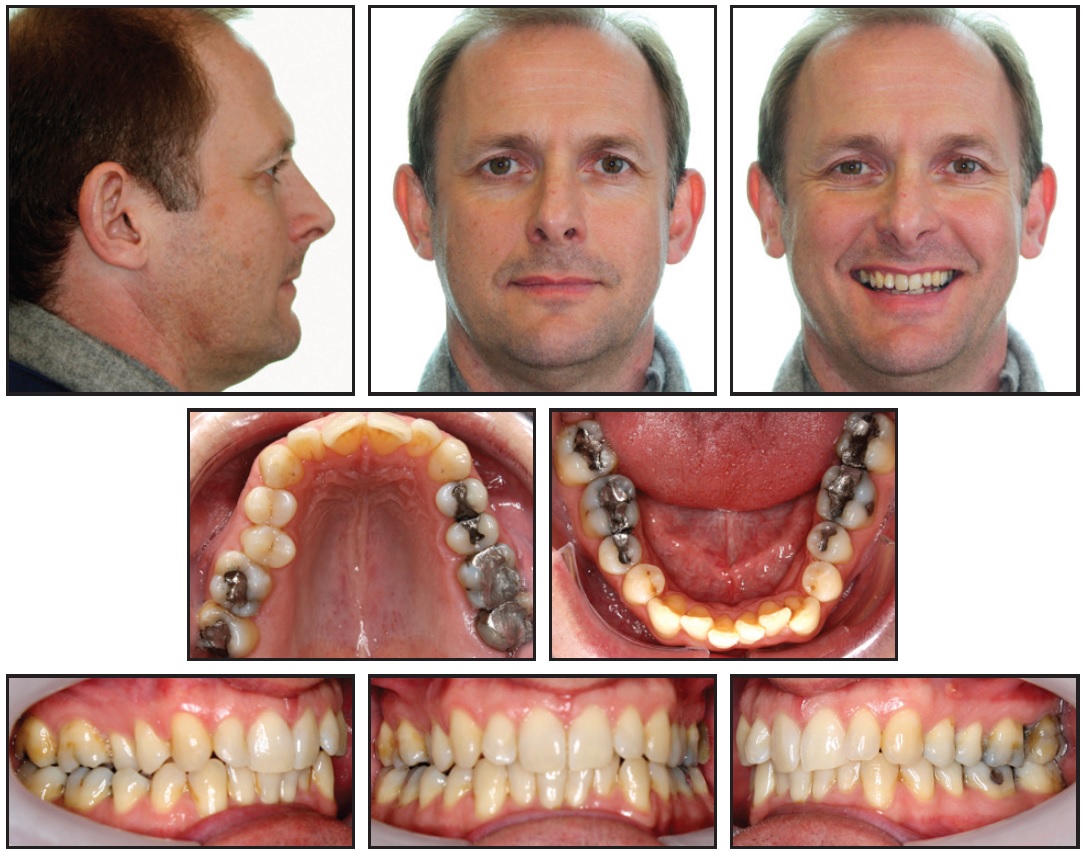
Fig. 14 Case 4. 45-year-old male patient with bimaxillary retroclination, upper right premolar in crossbite, and moderate upper and lower crowding before treatment. Estimated treatment time: 18-24 months.
He was starting treatment 16 months before a major sporting event that he was organizing. The estimated treatment time was 18-24 months, so he chose to use AcceleDent with Invisalign. Treatment goals included improving the inclination of the incisors. To correct the crossbite, a sectional fixed appliance was worn for three months in the upper right quadrant, placing the archwire below the bracket for intrusion of the upper right second premolar while the crossbite was corrected (Fig. 15). Total treatment time was 16 months, including the sectional fixed appliance, impressions for both initial and refinement aligners, and the ClinCheck** process (Fig. 16). A total of 33 aligners were needed.
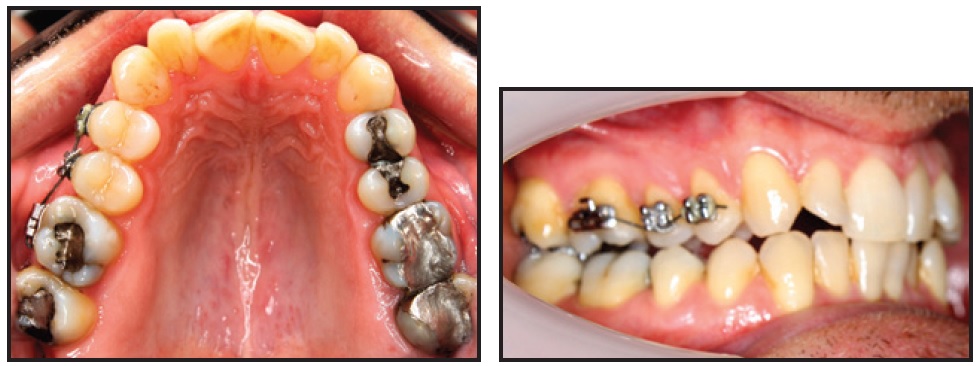
Fig. 15 Case 4. Sectional appliance used to correct crossbite of upper right second premolar.

Fig. 16 Case 4. Completion of treatment in 16 months.
Conclusion
This article demonstrates that the successful incorporation of AcceleDent into an orthodontic practice can significantly reduce treatment time, making it an attractive adjunct for both patients and clinicians. Because this is a new technique, further studies and randomized controlled trials are needed to better understand the optimal use of the device. Prospective studies will be challenging, however, as they need to be adequately designed to accommodate variations in treatment, patient compliance, and individual physiological response.
ACKNOWLEDGMENTS: We would like to acknowledge the help of Shelagh Foster in the preparation of this paper and Sheri Smith for the statistical analysis.
FOOTNOTES
- *Registered trademark of OrthoAccel Technologies, Bellaire, TX; www.acceledent.com.
- **Registered trademark of Align Technology, Inc., Santa Clara, CA; www.aligntech.com.
- ***OrthoAccel Technologies, Bellaire, TX; www.acceledent.com.
REFERENCES
- 1. Uribe, F.; Padala, S.; Allareddy, V.; and Nanda, R.: Patients', parents' and orthodontists' perceptions of the need for and costs of additional procedures to reduce treatment time, Am. J. Orthod. 145:S65-S73, 2014.
- 2. Meikle, M.C.; Reynolds, J.J.; Sellers, A.; and Dingle, J.T.: Rabbit cranial sutures in vitro: A new experimental model for studying the response of fibrous joints to mechanical stress, Calcif. Tissue Int. 28:137-144, 1979.
- 3. Kopher, R.A. and Mao, J.J.: Suture growth modulated by the oscillatory component of micromechanical strain, J. Bone Miner. Res. 18:521-528, 2003.
- 4. Peptan, A.L.; Lopez, A.; Kopher, R.A.; and Mao, J.J.: Responses of intramembranous bone and sutures upon in vivo cyclic tensile and compressive loading, Bone 42:432-438, 2008.
- 5. Vij, K. and Mao, J.J.: Geometry and cell density of rat craniofacial sutures during early postnatal development and upon in vivo cyclic loading, Bone 38:722-730, 2006.
- 6. Nishimura, M.; Chiba, M.; Sato, M.; Shimizu, Y.; Igarashi, K.; and Mitani, H.: Periodontal tissue activation by vibration: Intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats, Am. J. Orthod. 133:572- 583, 2008.
- 7. Liu, D.: Acceleration of orthodontic tooth movement by mechanical vibration, IADR Annual Meeting, Washington, DC, 2010, http://iadr.confex.com/iadr/2010dc/webprogram/Paper129765.html, accessed July 23, 2014.
- 8. Liu, D.: Histomorphometric study of orthodontic tooth movement under mechanical loading, J. Dent. Res. 90(spec. iss. A):1337, 2011.
- 9. Kau, C.H.; Nguyen, J.T.; and English, J.D.: The clinical evaluation of a novel cyclical force generating device in orthodontics, Orthod. Pract. U.S. 1:10-15, 2010.
- 10. Bowman, S.J.: The effect of vibration on the rate of leveling and alignment, J. Clin. Orthod. 48:678-688, 2014.
- 11. Liu, D.; Dai, Z.; and Royston, T.J.: Transmission of mechanical vibration from AcceleDent to dentition and skull, J. Dent. Res. 92(spec. iss. A):1773, 2013.
- 12. Ojima, K.; Dan, C.; Nishiyama, R.; Ohtsuka, S.; and Schupp, W.: Accelerated extraction treatment with Invisalign, J. Clin. Orthod. 48:487-499, 2014.



