MANAGEMENT & MARKETING
Defining Starts and Status Codes for Actionable Analytics
This column is compiled by JCO Contributing Editor Robert S. Haeger, DDS, MS. Every few months, Dr. Haeger presents a successful approach or strategy for a particular aspect of practice management. Your suggestions for future topics or authors are welcome.
Understanding practice-management metrics is critical in facing up to the business challenges of corporate orthodontics and large insurance companies. Those who know what to measure, how to standardize their data, and how to interpret the numbers will be far better business managers of their offices.
In a previous column (JCO, November 2014), John McGill and I described how to standardize expense accounting with QuickBooks to create an ideal profit-loss statement. This month, I have teamed up with Paul Zuelke to take you through the essential process of standardizing practice-management data by defining patient starts, organizing status codes, and generating actionable metrics for better business management. Once you have established your reporting system with appropriate metrics, it is a simple matter to benchmark your figures to those of other offices and determine what areas need improvement. The resulting analytics will help you make the right strategic decisions to improve your profitability.
Future Management & Marketing articles will demonstrate how all this data coordination can be used to create metrics for managing employees and designing a strategic marketing plan.
RSH
Similar articles from the archive:
Defining Starts and Status Codes for Actionable Analytics
The first step in clarifying the status of patients is to determine exactly what constitutes a patient start.
Defining Starts
Doctors have defined starts in many different ways. Some count only full cases; others count both Phase I and Phase II. Some even tally retreated cases. Although continuing to count starts by your prior method might have some historical value, a more useful definition of a start is as follows: the first time you or your practice places a clinical appliance, of any kind and of any value, in the patient¢s mouth. Any placement after the first clinical appliance placed by you is not a start; it is simply an additional phase of orthodontic care. If a patient has already had a clinical appliance placed by another practice, the first time you place an appliance for that patient is a new start.
To further qualify this definition:
- Any individual patient can start only once in your practice.
- An early, limited treatment with a lingual holding arch is a new start; the placement of braces two years later is merely an additional phase of treatment for the same patient.
- Phase I treatment is a new start; Phase II treatment of the same patient is not.
- Phase II treatment of a patient who received Phase I treatment elsewhere is a new start.
- An adult who comes in for a replacement retainer and was not previously treated by you or your office is a start.
- A retreatment of a patient you have previously treated is neither an exam nor a start.
Each start is recorded with an exclusive procedure code at the bonding date or retainer delivery date. The same procedure codes should never be used for active, retreatment, or Phase II patients. These status codes allow you to run practice-management reports and calculate powerful metrics, as described below.
Defining Status Codes
Status codes for your practice can be divided into four major categories (Fig. 1):
1. Yet to start
- Exam yet to occur.
- Pending (you recommended treatment, and the patient is deciding whether to pursue it).
- Other treatment (the patient needs some kind of pre-orthodontic care from another office).
- Start scheduled.
2. In observation
- Pretreatment observation.
- Ready to start after the next appointment.
- Not ready to start after the next appointment.
- Between phases.
3. In active treatment
- Child patient (18 or younger) treated with holding arches and no active tooth movement.
- Phase I treatment (the patient is undergoing tooth movement in preparation for braces at a later stage).
- Phase II treatment (the patient had previous fixed appliances or a holding arch placed in your practice).
- Full treatment (the patient is in single-stage treatment involving full upper and lower tooth movement).
- Braces.
- Invisalign*.
- Limited treatment (a catch-all category for patients needing retainers to move teeth, patients needing retainers only to hold teeth in place, patients needing single-arch treatment, and transfer patients).
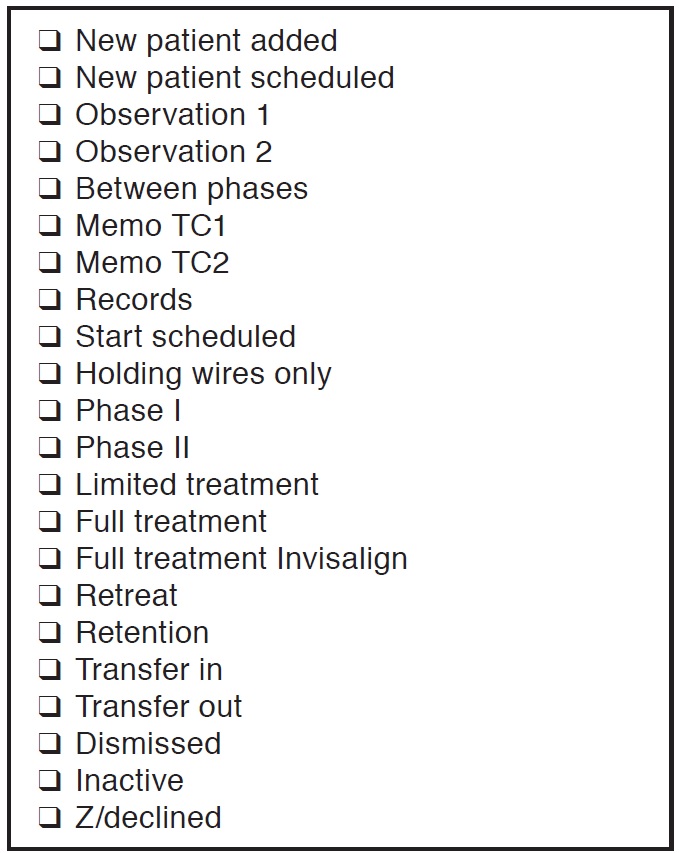
Fig. 1 Dr. Haeger’s customized status codes list, adapted from Dolphin** practice-management software.
4. Not in active treatment
- Declined treatment (the patient had an exam but did not follow through with treatment).
- Retention (the patient is in retainers and will return to your office for follow-up appointments).
- Inactivated (the patient has finished the active retention phase and will call your office for any future care).
Prospective patients who declined treatment should be tallied separately from inactivated patients, because some of them do end up starting. You may also want to target this group for occasional marketing.
Generating Actionable Metrics
Once you have organized your starts and status codes, you can produce a number of actionable metrics to help manage your practice.
Percentage of child starts: This is a critical metric because the age breakdown of your patients will impact your practice marketing plan. Offices with high percentages of adults require more marketing to referring dentists, while those with high percentages of children get more starts from siblings and observation pools.
Collections per start: This is a good metric for assessing your proportion of limited-treatment starts and your conversion of Phase I patients to Phase II.
Number of observation patients awaiting their first treatment: This is a great predictor of future starts, since a healthy practice will get 30-35% of its starts from the observation pool. By tracking this number over the years, you can get an early indication of increases or decreases in your patient base, letting you know when it¢s time to consider another location or step up your external marketing.
Number of Invisalign starts; percentage of adult starts using Invisalign: Following these numbers over time allows you to determine whether a scanner would be a wise investment. It also helps you evaluate the Invisalign lab component of overhead and how it relates to your practice capacity. Invisalign treatment requires less chair-time and is more profitable when your office is at full capacity; at less than capacity, the lab cost will exceed your cost of bands, brackets, and retainers.
Percentages of exams that start, go to observation, decline treatment, are still pending a decision, or had no treatment recommended: Practices with low percentages of Phase I cases typically start about 41-43% of their child exams, while those with high Phase I percentages are generally around 52-55%, with some as high as 75%.
Overall conversion rate (starts/exam): This provides a great picture of general practice health, taking into account your numbers of current exams, treatment-coordinator conversions, and observation patients. On the other hand, because the overall rate includes so many components, it can make it difficult to identify the source of any conversion problems. The rate can be accurately calculated only if you define starts as outlined above. If you count a single patient twice, your conversion rate will become distorted and meaningless.
Conversion rate minus patients going to observation and those for whom no treatment was recommended: To calculate this percentage, divide the number of current-year exams by the number of patients for whom you recommended treatment. As a conversion rate for a specified time period, it is a good way to assess the effectiveness of your practice¢s initial phone calls and treatment coordinators. A healthy practice will convert around 75- 78% of children and 42-46% of adults.
Percentage of starts from exams: This is a key metric for understanding the importance of child exams and your observation program. If the percentage of starts from exams goes up, it often means that the number of patients in pretreatment observation is declining. This number will help you decide whether to focus your marketing efforts more on internal or external activities.
Ratio of active Phase II patients to active Phase I patients: If 85% of your Phase I patients proceed into Phase II, and Phase II treatment takes six months longer than Phase I, this ratio should be between 1.1:1 and 1.3:1. If the ratio is too low, it means either that your Phase I treatments are too long or that you are not converting enough Phase I patients to Phase II.
Percentage of child starts in Phase I: Monitoring this percentage will help you determine how to market your practice to dentists. If your Phase I starts are low, you will need to encourage dentists to refer patients early, even if you don't typically start them at that time. Dentists will quickly learn when you like to start patients and adjust their referral patterns accordingly. If they begin referring too late, however, you will end up being too dependent on exams for your starts because your observation pool will shrink. You should therefore emphasize to your referring dentists that you always want to see child patients in the middle mixed dentition.
Training Staff to Use Status Codes
Proper use of status codes and metrics will not only provide you with strategic information about your practice, but can also help you avoid significant loss of profits. Consider the following three scenarios, all of which actually occurred in orthodontic offices and all of which could easily have been avoided.
One practice saw its Phase II case starts decline by 47% from the same period a year earlier, costing the office more than $160,000 in lost production (and revenue). A bit of investigation revealed that an employee had been routinely changing the status code of finished Phase I patients to "Retention" instead of "Between Phases". As a result, those patients were no longer reported as needing recall appointments.
Another office could not figure out why it was showing more case starts than exams. The chairside assistants were posting procedure codes for all patients seen in the clinic (a common practice). Unfortunately, these assistants had not been properly trained: every time they bonded a bracket or delivered a set of aligners, they were using the procedure codes for new case starts.
Yet another doctor discovered that one of his treatment coordinators was intentionally changing the status codes of "Pending" patients to "Inactive"because she "didn't like doing follow-up work". She knew the doctor used the list of "Pending" patients to monitor whether treatment coordinators were following up on patients, so the "Inactive" status code kept her patients off that list. The lack of proper follow-up cost this practice 15-20 case starts.
These three doctors all believed their statistics were accurate, and that they could count on their reports to give them accurate information about their practices' well-being. It took a financial emergency for each of them to see the importance of proper staff training.
Conclusion
The crucial point to remember is that any individual patient can start only once in your practice--the first time he or she undergoes a treatment you have recommended. A start could involve placing a holding wire or active retainer, beginning either Phase I or full treatment, or providing a retainer for a patient treated by a different office. First-time starts must have specific procedure codes that are never used for active patients.
Proper use of status codes will organize your patient base for actionable metrics and benchmarking. The resulting analytics will help you create a strategic marketing plan, monitor various conversion rates, prevent the loss of patient starts, and increase your profitability. Take the time to educate your entire staff (including chairside assistants) on how posting correct status codes will help the practice grow.



