JCO INTERVIEWS
Charles J. Burstone, DDS, MS, Part 2: Biomechanics
Part 1 of this interview, on Facial Esthetics, is available in the February 2007 issue.
DR. NANDA You have often been called the father of biomechanics in orthodontics. How did you get interested in biomechanics?
DR. BURSTONE As a young clinical orthodontist treating patients and supervising graduate students, I was very careful to take progress records, including headfilms, on my patients. In more situations than I imagined, I was getting undesirable side effects. Even if the teeth were becoming well aligned, they were not oriented in space where I wanted them.
To begin with, I thought that I was not making the wires correctly, and then it dawned on me that I was making some basic errors in my biomechanics. The major problem was not poor wire fabrication or sloppy wires, but something much more fundamental. This caused me to go back and learn and relearn basic physics and engineering, so I could have a scientific basis for orthodontic biomechanics. In other words, I started as a clinician who saw problems and tried to understand why they occurred and what to do about them.
DR. NANDA You have done some classic research described in some seminal articles on the subject of biomechanics. Based on this research, why do you believe that a thorough grounding in biomechanics is necessary for the clinician?
DR. BURSTONE The bread and butter of orthodontic treatment is the application of forces and force systems to alter tooth positions or to produce bony changes. Therefore, the application of scientific biomechanics as we daily treat our patients can pay big dividends. The quality of treatment improves, and we work much more efficiently.
Similar articles from the archive:
DR. NANDA How does "scientific biomechanics" differ from biomechanics in general?
DR. BURSTONE The phrase "biomechanics" has been commonly misused in orthodontics. Sometimes it refers to techniques; other times it refers to clinical procedures such as wire bending. "Scientific biomechanics" relates forces and stresses to our orthodontic problems. It answers such questions as:
- What is the relationship between the appliance and the force system?
- What is the optimal force system to produce different centers of rotation?
- What is an optimal force? What is the relationship between stress and strain?
- What are the biological changes in the periodontal ligament and in the bone?
- What are the proper materials for optimal appliance design?17
DR. NANDA Can you give us an example of how scientific biomechanics can be a practical adjunct for the busy clinician?
DR. BURSTONE All of us would like to have controlled tooth movement. This is achieved by having a proper moment and force exerted from the bracket by means of a wire, using a multi-attachment appliance. Let's look at space closure as an example. The patient has incisors that we want to retract. In a loop arch for anterior retraction, lingual root torque is placed to prevent roots from being displaced forward. In early Tweed mechanics, labial root torque was placed. This was backward until we all learned that the tooth movement produced was not desirable. Lingual root torque is required to prevent incisor roots from displacing forward. Have we learned our lesson? In some straightwire appliances today, a flared incisor that requires retraction would produce labial root torque. It's the wrong force system--like going back 60 years (Fig. 8).
There is more to controlled tooth movement than some special bracket or bracket prescription. To gain control, we can slide teeth along the archwire, or we can build in the force system required for non-sliding mechanics. The basic force system is independent of technique or appliance.
DR. NANDA With all the refinements we now have in brackets and wires, are you saying that straight wires don't always work?
DR. BURSTONE If we place a straight wire into correctly placed brackets on crooked teeth, a resulting force system is inherently produced. Many times, this is exactly what we want, and we look like geniuses no matter what wires we use. At other times, we can produce a secondary malocclusion that could be more problematic than the original problem. Thus, a knowledgeable orthodontist will be able to differentiate those situations where straight wires work well and those situations where they will not work well. There are many examples of undesirable side effects during leveling. For instance, if the root of the cuspid is forward, leveling an arch will increase the deep overbite (Fig. 9). Other side effects include the development of open bites, canted occlusal planes, and crossbites during treatment.
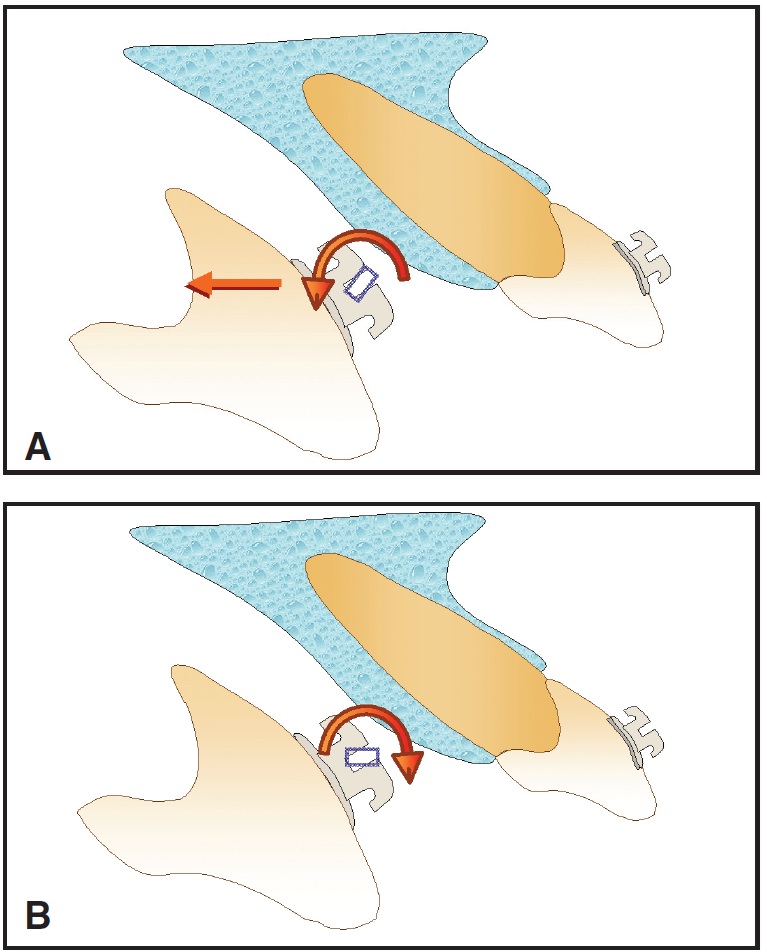
Fig. 8 A. Tipping central incisor lingually around center of rotation at its apex requires lingual force and lingual root torque. B. Straight wire produces labial root torque, which tends to displace root forward.
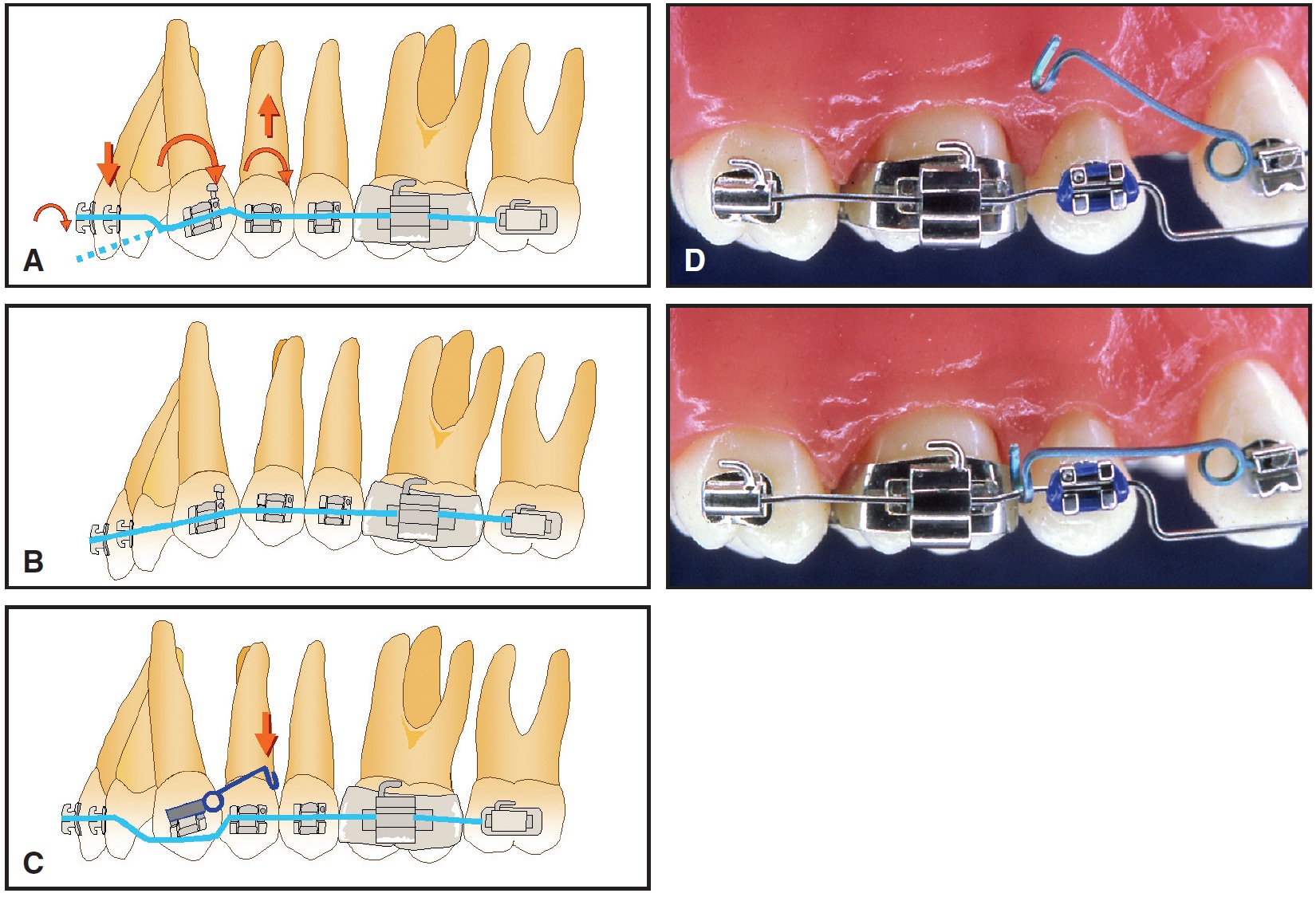
Fig. 9 A. Trying to use straight wire to level canine with its root inclined forward produces undesirable forces and moments. Occlusal force from archwire causes incisors to erupt, increasing deep overbite (dotted line shows that archwire would lie incisal to canine if not ligated to incisors). Intrusive force and clockwise moment on first premolar also tend to tip buccal segments mesially. B. Overall effect of this straight-wire force system tends to deepen overbite and produce reverse curve of Spee in upper arch. Additional wires and longer treatment time may be required to correct this secondary malocclusion. C. Unwanted side effects can be eliminated by using bypass arch—separate continuous arch stepped around canine—which makes use of full arch to control anchorage. Separate root spring is placed on canine to correct axial inclination. D. TMA* root spring before and after activation. Placing bypass arch occlusal to canine bracket allows canine extrusion. If no extrusion is needed, bypass arch should contact occlusal edge of canine bracket.
As the old statement says, there is no free lunch. Whatever we do must be grounded in sound physics and biomechanics. This includes the question of friction, which all clinicians should thoroughly understand. In any event, without the correct force system, we will not be happy with the result.
DR. NANDA We hear much about friction these days, and there is considerable interest in self-ligation with so-called "frictionless" brackets. How important is friction, and is the elimination of friction always desirable?
DR. BURSTONE Friction between wires and brackets can be both good and bad. During canine retraction, friction can reduce the force and minimize tipping movements. This could be good. Other times, friction can be so great as to minimize or prevent tooth movement. Friction in orthodontic appliances is complicated and involves many factors. I cannot give a simple answer other than to emphasize the importance of understanding all of the factors involved. These include the coefficients of friction of the materials involved and, particularly, the role of the applied force system. The force system is the primary determinant of the friction force; for example, if translation is required using sliding mechanics, friction will be very high. The idea of a friction-free bracket is a misnomer, unless the only type of tooth movement required is simple tipping (Fig. 10).
DR. NANDA What about anchorage control? How do you prevent mesial drift of posterior segments in extraction cases?
DR. BURSTONE There are a number of approaches to minimizing anchorage loss in the extraction patient. These could include headgears or other auxiliaries, but let's discuss the intraoral force system. There has been the suggestion of using Begg appliances for differential forcesheavy forces to slip anchorage and light forces to control anchorage. For many reasons, I'm not sure this is a practical and valid approach. What my research has pointed to is another concept: a differential moment-to-force ratio on the anterior and posterior teeth. The higher moment-to-force ratio on the posterior teeth can produce translation while the anterior teeth exhibit controlled tipping. The more uniform stresses of posterior teeth in the periodontal ligament enhance the anchorage. This principal is universal for both sliding and non-sliding mechanics, but is most easily applied using frictionless loops (Fig. 11).
DR. NANDA What do you think of using headgear to control anchorage? Most of our patients today are not well motivated to wear headgear.
DR. BURSTONE Headgears are certainly not obsolete. They can play a role, particularly in Class II patients to hold the upper teeth while the mandible is growing forward. However, I think it is a mistake to use sloppy mechanics that lose anchorage and expect the patient to cover up our mistakes by wearing a headgear. There is no question that scientific biomechanics can reduce patient compliance by minimizing anchorage loss and side effects.
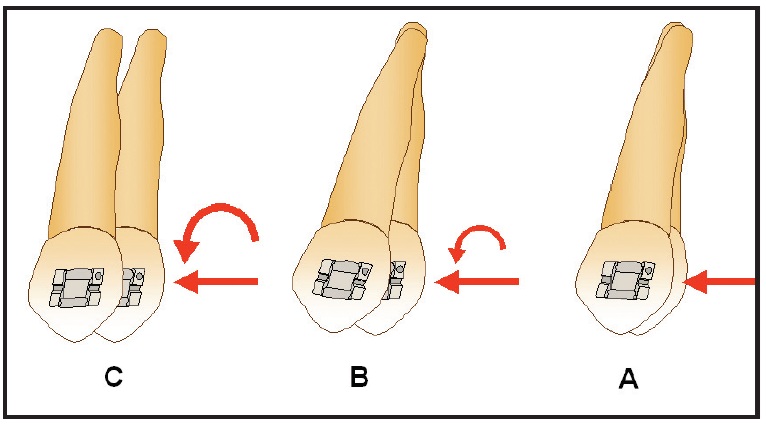
Fig. 10 When canine is retracted with sliding mechanics, archwire exerts moments to prevent tipping. These moments or couples produce vertical forces responsible for friction. A. With play between wire and bracket, tooth tips without friction. B. After archwire engages, friction begins and less tipping occurs. C. Greater moment is produced as tooth goes through translatory phase, when friction is highest.
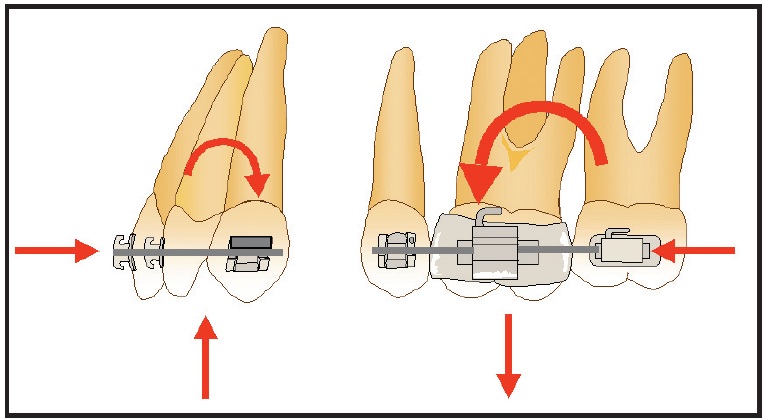
Fig. 11 Posterior anchorage can be controlled by using differential moments between anterior and posterior segments, pitting controlled tipping of anterior teeth against mesial translation of posterior teeth. No differential forces are created because forces are equal and opposite. Intrusive forces on incisors can be helpful in deep-bite patients.
DR. NANDA The orthodontist is bombarded with many new appliances, techniques, and brackets; can an understanding of biomechanics be helpful in selecting the best appliance for a patient?
DR. BURSTONE As clinicians, when a new appliance is presented, we have a number of alternatives. We can try it in our office. This is time-consuming and costly; furthermore, much of orthodontics requires long-term evaluation. It might be years before we recognize that the new procedure or appliance is not what is required. An understanding of biomechanics allows us to rationally analyze the appliance or technique and come to a valid conclusion about its efficacy. Orthodontic companies by necessity introduce many of the new appliances, and while most of these companies are genuinely interested in the profession, salespeople obviously have a conflict of interest when presenting these appliances.
DR. NANDA Can biomechanics also help us better utilize any appliance that we might currently be using?
DR. BURSTONE The nice thing about scientific biomechanics is that it is not dependent on any given appliance or technique. No matter what appliance you use, it allows you to use it better with more predictable results. Today, we have much too much commercialism in orthodontics; a healthy dose of science in understanding appliances and how they work is a good antidote. It is interesting to note that many of the new appliances that are suggested are nothing more than reinventions of old appliances.
DR. NANDA Do you have any advice for orthodontic researchers who are interested in evaluating the efficacy of different orthodontic appliances? Are there biomechanical considerations they must be aware of as they plan and carry out their research?
DR. BURSTONE Good epidemiologic studies are now being carried out to evaluate orthodontic appliances. The best ones are prospective, and the force systems used in these orthodontic appliances are a very important consideration. Even with well-designed sampling procedures, however, definitive conclusions may be hard to find because of all the variables. Let's suppose we want to compare the effects of headgear and a given functional appliance. It is not enough to say headgear alone or, more specifically, occipital headgear. Occipital headgear has many directions of pull, and even if the direction is given, there are many different points of force application in respect to the center of resistance of an arch or a molar. It is little wonder that there is so much inconclusive research appearing in our journals. Properly designed research must define the force system more completely; this should include moment and force magnitudes, moment-to-force ratios, force-deflection rates, and force direction. In addition, we also need good numerical methods to calibrate treatment changes.
DR. NANDA You've described appliances as being force- or shape-driven. What do you mean by that?
DR. BURSTONE Historically, orthodontic appliances were developed, described, and taught as shape-driven. In the era of shape-driven appliances, which is still with us, you were taught how to bend or twist a wire or how to properly position a bracket. That is all geometry--driven by shape. I think a better approach is to first determine your orthodontic goal--what you would like to do--and then determine the force system that is required to produce that result. Then, and then only, can you design your appliance. It is important to have a shape, but it is more important that the shape produces the desired force system. And of course, many times that shape will look nothing like an ideal or a straight wire. This does not mean that for every activation we have to know exactly every force; most of the time knowing the relative force system and the possible side effects can be more than adequate. Thus, as we train our modern orthodontists in graduate programs, a typodont course not only includes fabrication of the appliance, but also an explanation of the force system that goes with the appliance.
DR. NANDA I remember vividly a statement you made when I joined you in 1972, and I often repeat it in my lectures: "Orthodontics should not be driven by personalities." Well, it seems that no-thing has changed over the years, because our profession continues to associate names with techniques or brackets or other gadgets. What do you think is going on?
DR. BURSTONE It is much more common in art than in science to have different schools of thought associated with the names of respected leaders. We have seen this in psychiatry, where many schools of thought developed originally. As psychiatry became more of a science, there was no longer a need for different schools of thought and famous gurus. I hope that as orthodontics has matured, we can still respect our great teachers as well as the individual thinkers. It is a major responsibility of orthodontic departments and those of us who teach graduate students to make sure that every student has a good background in the science of orthodontics, especially biomechanics.
DR. NANDA What is the scientific basis for the field of orthodontic biomechanics?
DR. BURSTONE Biomechanics didn't originate with orthodontics. It is based upon the pioneers of physics like Galileo and Newton. More recently, it includes research in material science, mechanics of materials, beam theory, finite-element and computer science, etc. Those of us who do research in orthodontic biomechanics build on the foundation from the basic science of engineering and physics.
DR. NANDA It is not uncommon to hear lectures or to read articles in which the orthodontist develops his or her own system of biomechanics to explain what is happening. How do you feel about this?
DR. BURSTONE This is part of the problem. I'm sure that we have many intelligent orthodontists; however, they are not in the same genius category as Newton. It is not only more valid to build on accepted scientific principles, but it has the added advantage of allowing us to use terminology that can be understood and respected by all scientific specialties. A perusal of our orthodontic journals can show many unusual notations, funny words, signs and symbols, diagrams not in equilibrium, and imaginary or impossible force systems.
DR. NANDA So how do we get our fellow orthodontists to be more knowledgeable about scientific biomechanics?
DR. BURSTONE It must start with the training of our graduate students. In addition to courses in basic sciences, cephalometrics, techniques, appliance fabrication, treatment planning, dental materials, etc., they need a solid course in scientific biomechanics. This course should include how to handle resultants and components of forces acting on a body or a point, equivalent force systems, the biomechanics of tooth movement, equilibrium, equilibrium diagrams, mechanics of appliance design, force systems produced by straight or bent wires, and other applications for headgears and functional appliances. Of course, this material is much harder to teach than the technical aspects of orthodontics, which can be more quickly learned. The challenge is there and must be met by our orthodontic programs.
DR. NANDA There has been a lot of interest recently in "evidence-based orthodontics". Do you think we can practice orthodontics like medicine and surgery, where clear evidence is available regarding the efficacy of one procedure over another?
DR. BURSTONE There seems to be general acceptance in the field of medical epidemiology of the importance of a hierarchy of evidence. At the lowest level, one finds anecdotal evidence, and at the highest level, one finds a systematic review of many studies or a meta-analysis. This is a good framework to start from, since orthodontics has always suffered from a pluralism of individual opinions, from the individual orthodontist to the orthodontic guru. However, there are some problems with evidence-based orthodontics. First, unlike medicine, we are not dealing with disease or diseased tissues. We all establish individualized treatment goals and procedures. To obtain these goals, our mechanical procedures can be very different for any given patient; hence, unlike medicine, the endpoint may not be clear. For example, if there is an arch-length inadequacy, one orthodontist might decide to extract, and another orthodontist might solve the problem by expansion. Thus, an epidemiologic study may not be comparing the same endpoints. Nevertheless, the basic approach of evidence-based orthodontics is a goal that we should aim for.
DR. NANDA But are there good enough studies to establish meaningful protocols for treatment?
DR. BURSTONE This is the problem. Many of the studies that are quoted in the literature have major deficiencies, either in sampling or in method. Thus, they do not reach the level of quality for a meta-analysis to be performed. Medicine has the advantage, as I pointed out, of dealing with more definitive endpoints. The patient lives or dies. Longevity can be measured. The disease is cured. What is the endpoint for a successfully treated Class III? Protruded upper incisors? Retruded lower incisors? Growth alteration?
DR. NANDA Whatever the methodology, many orthodontists are reluctant to accept evidence-based approaches to treatment. They claim that their clinical experience and judgment are the basis for their treatment, rather than a bunch of dusty old articles.
DR. BURSTONE We all certainly learn a lot from our clinical experience; however, this does not make evidence. Unlike medical practitioners, most of us practice in isolation, and thus, there is little feedback from the rest of the profession on what were doing. We can harbor these beliefs even if there is no validity to them.
DR. NANDA Let's take the example of Class II treatment. By my recent count, there are at least 20 different appliances available to move a maxillary molar distally. Most of the appliances have been introduced without any evidence-based research. How do you feel about this?
DR. BURSTONE Most of these appliances use the principal of the Nance button for anchorage control during distalization. There is good evidence that these appliances can move molars distally, primarily by tipping, during the initial phase of treatment. Unfortunately, the premolars come forward; that is anchorage loss. The best studies show that the centers of resistance of the molars move back the same amount as the center of resistance of the premolars moves forward. Fifty percent of anchorage loss is not very impressive. During an intermediate second phase, bicuspids are supposed to drift distally. Unfortunately, the drift is minimal, and the molars come forward. Then there is a question of the overall effect. Many of these patients are also treated with Class II elastics, and therefore the studies do not show if the Class II correction is due to molar distalization or to holding of the upper molars, with mandibular growth accounting for the occlusal change. In other words, in successful Class II correction, has the orthodontist distalized the molars and held them back, or is the correction mainly due to favorable growth?
DR. NANDA The FDA requires different phases for verification of an appliance in medicine. Do we need a regulatory body to validate the claims of the various orthodontic manufacturers?
DR. BURSTONE I'm not sure that we want to ask the FDA to have more stringent requirements for appliances that are not placed into tissues. I'm not sure that the AAO is in a position to serve as a regulatory body. Orthodontic companies can do more; they can at least have research demonstrating the efficacy of their appliances. But fundamentally, it is the intelligent, well-trained orthodontist who must be responsible for evaluating the appliances and materials that he or she uses.
DR. NANDA Over the years, many orthodontists have discussed with you some of their failures and problematic patients. Based on what they've told you, what do you consider the most difficult problems?
DR. BURSTONE Leaving out problems of patient cooperation, I would have to pick the treatment of asymmetries. There are extreme skeletal discrepancies that can be treated with orthognathic surgery, and in these cases, the orthodontics is simple. The difficult patients are a subset: the nonsurgical treatment of asymmetries. Some of these patients are not too difficult because they involve mandibular shifts, and fairly simple symmetrical mechanics can lead to an excellent end result. But other patients can have small skeletal asymmetries or even developmental dental asymmetries that are hard to treat. Treatment may lead to failure if symmetrical mechanics are used. Since no mandibular shift is present in these patients, the malocclusion can only be corrected with well-planned asymmetrical mechanics. This is much more challenging than the use of symmetrical mechanics. The use of a lot of intermaxillary elastics, such as Class II, Class III, or criss-cross elastics, may not lead to a stable correction. There must be differential tooth movement between the right and left sides to obtain the correction. These asymmetries are challenging because they require good planning, mechanics, and execution.18
DR. NANDA How is treatment planning for the asymmetrical patient different from our typical symmetrical situations?
DR. BURSTONE A good example is the so-called midline discrepancy associated with a small mandibular asymmetry. These are patients where the asymmetry is not great enough to suggest orthognathic surgery. Typically, a midline is established first. One could connect midpoints such as soft-tissue nasion, subnasale, and pogonion. This is valid and easy to do if all points coincide, but with an asymmetry, they do not. Picking two points such as nasion and subnasale to establish an upper facial midline may not be the best choice. I think in terms not of a midline, but of a "mid-arc", which is a reasonable fit of a curve going through key midpalatal plane structures. This simplifies treatment, since less incisor root movement is required, and a better esthetic result is achieved. In this view, the concept of a facial midline is a fallacy. We should be thinking more in terms of curvatures (Fig. 12).
Another example is an apical midline discrepancy. If an apical base discrepancy is recognized, it might be better to angle the incisor brackets for compensation. A small axial inclination difference will not be noted by the patient, and treatment then becomes much simpler. This avoids the use of asymmetrical intermaxillary elastics, such as anterior criss-cross elastics, that can alter the plane of occlusion, producing unsightly canting.
DR. NANDA You have been a role model to hundreds of orthodontic residents, and thousands of orthodontists have benefited from your contributions to the profession. Where do you see the profession at present?
DR. BURSTONE I am very positive about orthodontics in general and about orthodontic education today. The quality of our graduate students is excellent; the best of the best are electing to go into orthodontics. The overall quality of graduate training has never been better. There is more uniformity between programs, so that graduate students from any university can obtain an excellent education. Of course, I would like to see more biomechanics in the curriculum. This continues to be a major problem that is not easily resolved. Scientific biomechanics requires teachers with a fundamental knowledge of physics and engineering, which is not a common background for orthodontic graduates. In addition, it is important that graduate students have time and proper supervision to study their patients in depth. Although it is necessary for orthodontic departments to earn money to support their programs, an overload of patients can be counterproductive to learning.
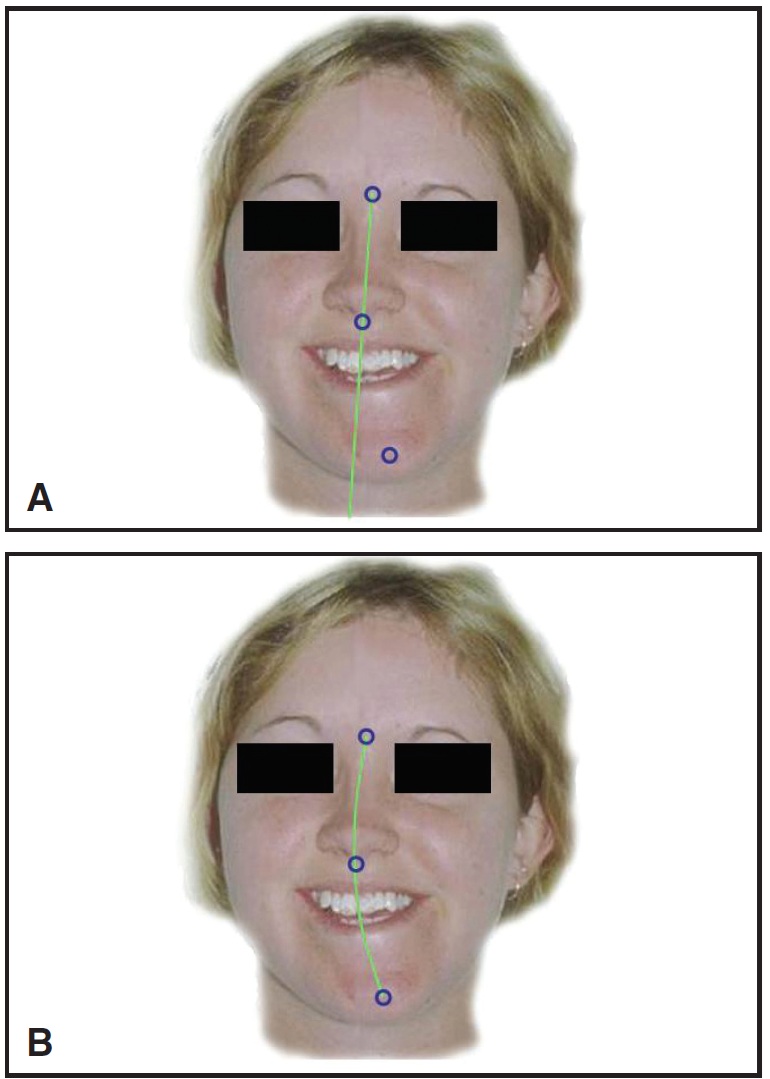
Fig. 12 A. Establishing upper facial midline between nasion and subnasale would require considerable upper incisor translation in any nonsurgical treatment of this patient with marked mandibular asymmetry. B. Smooth arc forming midline curvature is better fit for skeletal discrepancy, as seen at both incisors and skeletal landmarks. Whenever facial symmetry will not be corrected surgically, tooth positions should fit curve rather than straight line.
DR. NANDA The reason often given for the current shortage of teachers is a disparity in income, but we had this disparity when we both embarked on our educational careers. Why do you think the problem is so acute now?
DR. BURSTONE It is important that we do everything we can to increase and maintain competitive salaries for our best faculty. The AAO, the AAO Foundation, and alumni have all been helpful and should continue their efforts. It is also important that the universities maintain a happy, creative, and stimulating environment for their faculty.
In my career, I've always enjoyed every day. Nowadays, there can be too much pressure on faculty members for increased clinical production or promotion, which can create an unproductive atmosphere.
In addition, part-time faculty members who are clinicians in practice have to increase their contributions to orthodontic programs. We all have to give back something to a wonderful profession. This is not only valuable to the programs, the graduate students, and the profession, but as many part-time faculty members will tell you, it is a positive experience for them. Overall, if we, the academicians and the practitioners, pull together, we can look forward to a positive future for orthodontics.
DR. NANDA On behalf of the readers of JCO, I want to thank you for this interview.
REFERENCES
- 17. Burstone, C.J.: Application of bioengineering to clinical orthodontics, in Orthodontics: Current Principles and Techniques, ed. T.M. Graber, R.L. Vanarsdall, Jr., and K.W.L. Vig, 4th ed., Mosby, St. Louis, 2005, pp. 293-330.
- 18. Burstone, C.J. and Marcotte, M.R.: Problem Solving in Orthodontics: Goal-Oriented Treatment Strategies, Quintessence, Chicago, 2000.



