JCO Interviews Dr. Charles J. Burstone on Orthodontic Force Control
DR. GOTTLIEB Understanding force systems is so important in orthodontics and yet most orthodontists find it hard to deal with the basic information. "As you increase the diameter of a round wire, you get an increase in force to the fourth power; so, if you double the diameter of a round wire, you get 16 times the force." They tune out that type of information.
DR. BURSTONE If that's true, all we can say is that they should not tune it out. That's part of the knowledge needed in order to make an intelligent decision about whether one should use an .014" arch or an .016" arch. Incidentally, an .016" wire will deliver almost twice (1.7x) as much force for the same activation as an .014" wire. So, that is a major factor in arriving at a decision on what wire an orthodontist should use. And, it's going to get more complicated, rather than simpler, because new alloys such as Nitinol and TMA have been introduced. The orthodontist wants to make a decision on whether he should use them, and have enough knowledge to select the correct alloy for his patient. No one can tell him how to design every last mechanism that will go into the treatment of every case. Part of the challenge of orthodontics is that an orthodontist is a designer and a bioengineer, and it requires the highest attributes of human thinking to pull all this knowledge together. We are shortchanging our patients, if orthodontics is carried out with a "cookbook" approach.
DR. GOTTLIEB You mention TMA. What is it?
DR. BURSTONE TMA, Titanium Molybdenum Alloy, is used in a new wire introduced into orthodontics by Jon Goldberg, a metallurgist at the University of Connecticut, and myself. It is a beta-titanium alloy, which is almost 80% pure titanium. The stability of the beta phase at room temperatures imparts its unique properties.
DR. GOTTLIEB In what way are its properties unique for orthodontists?
DR. BURSTONE In the development of TMA wire, we tried to create a balance of properties that the clinician needs--low stiffness, high maximum elastic deflection, formability, and ease of joining. A TMA wire delivers only 0.4 the force of a steel wire and may be deflected approximately twice as far without permanent deformation. This allows early placement of edgewise wires, and fuller bracket engagement than with smaller round wires. The high elastic deflection simplifies design and, in many instances, eliminates the need for loops in alignment procedures.
DR. GOTTLIEB Is the wire brittle?
DR. BURSTONE In the past, the wires with the best spring properties were the most brittle; because they were drawn to a high percent reduction, so that the yield strength would be higher.This was a mistake. It was our desire to produce a wire with balanced properties. TMA is very ductile. It can be bent and rebent, and formed into complicated configurations without fracture. It can be bent in very small radii of curvature. It is easily twisted to produce torque, yet springback is excellent, due to the high ductility. I believe that good ductility and freedom from fracture are very important. The orthodontist cannot afford fracture of the wire in his appliances.
DR. GOTTLIEB How are hooks placed on a TMA wire?
DR. BURSTONE TMA can be joined by welding alone. With proper welding, there is little reduction in the mechanical properties of the wire. I use the Rocky Mountain 506 Dial-A-Weld with a setting of #1 and a current level of #5 to #10 on the rheostat to weld wires. There is variation among welders, so each welder should be calibrated for best results.
DR. GOTTLIEB And you can weld round wire?
DR. BURSTONE The best welds are round to round, because of the point contact of the wire. Edgewise wire should be slightly rounded where a weld is needed. I recommend using the larger diameter or flat electrodes, so that the wires are better restrained during the welding process.
DR. GOTTLIEB You said the wires are joined by welding alone. No solder reinforcement is needed?
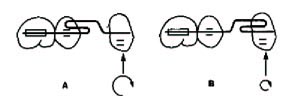
DR. BURSTONE No. Unlike steel, the weld will hold without solder. Furthermore, the spring properties are not lost. This means that auxiliaries for rotation, root movement, and space closure can be welded directly to an archwire (Fig. 1).
DR. GOTTLIEB Is it necessary to heat treat TMA wire?
DR. BURSTONE No. No heat treatment is required.
DR. GOTTLIEB How do you select the most desirable cross section of wire?
DR. BURSTONE It depends upon the application. Sometimes you would like teeth to move in all directions, for which it is probably best to use a round wire, because it has more uniform properties in each direction. On the other hand, if you would only like tooth movement in one plane, there are advantages in using rectangular wires, because in the thinner dimension these wires are much more flexible and deliver less force for a given activation. If you have a problem that is primarily occlusogingival, rectangular wire is fine. So, the cross section of the wire is dependent upon its application. Of course, it is more difficult, but possible, to produce torque with round wire.
DR. GOTTLIEB Do you ever use a flat wire?
DR. BURSTONE If you have primarily first order problems, a ribbon wire could be useful. I happen to use .022" slots. Many times, for anterior alignment, I will use an .020" X .016" braided or TMA ribbon wire, recognizing that I want rigidity occlusogingivally and flexibility labiolingually, to correct rotations and labiolingual malalignment. In this way, we take advantage of preferential orientation.
DR. GOTTLIEB That would require that you use another wire for leveling. You couldn't expect that wire to level.
DR. BURSTONE That's right. Many times, the initial alignment can be done with a light round wire, either solid or braided. If second order problems are minimal, but a discrepancy exists in the first order direction, that's where a ribbon may be used. By segmenting, I am not depending on the alignment wire for the overall leveling of the arch, since a base arch is used, and I can be more selective in choosing a wire. With a continuous arch, one is stuck with the same cross section throughout.
DR. GOTTLIEB There is something about each wire that makes it suitable to move teeth readily during leveling--the smaller the diameter of a round wire, or the flatness of a ribbon wire, or the low modulus of elasticity of Nitinol and TMA.DR. BURSTONE There are a number of factors we should look at if we are trying to level teeth, if we disregard for the moment any side effects from having a continuous wire or continuous segment from bracket to bracket. One factor is the maximal elastic deflection or range of action. Most clinicians would like a wire that can be deflected into a bracket over a long distance without permanent deformation--a high maximal elastic deflection. Obviously, if the wire deforms, the teeth will not move.
DR. GOTTLIEB Is that the same thing as elastic limit, and are there other similar expressions?
DR. BURSTONE Engineers will speak about a yield point, a yield strength, a proportional limit, or an elastic limit. Elastic limit is the stress just before permanent deformation takes place. As clinicians, we don't think on the stress level. We think of activations and forces. So, we really shouldn't use the term "elastic limit': unless we are talking about stress--pounds per square inch. How far a wire can be deflected without permanent deformation is related to the elastic limit of the material. Everything else being the same, the maximum elastic deflection of an appliance varies linearly with the elastic limit. This is the range of action, or how far you can maximally activate an appliance without permanent deformation.
DR. GOTTLIEB How does the choice of wire alloy influence range of action?
DR. BURSTONE Two material properties determine range of action. One is the elastic limit or yield strength, and the other is the modulus of elasticity of the material. We would like to have the highest possible ratio between these two. The modulus of elasticity measures the stiffness of the material. The less stiff a material is, the easier it is to bend. Less force is produced for any activation. Some of the new materials that have been introduced into orthodontics, like Nitinol and TMA, can be deflected over long distances, because they have very high ratios between their elastic limit and their modulus of elasticity.
DR. GOTTLIEB It is not solely the modulus.
DR. BURSTONE That's right. You have to consider elastic limit, too. Nitinol has a very low modulus of elasticity, around 5 million PSI. Stainless steel might be around 25 million in the wires that we use. So, this means that for every millimeter of activation of similar size wires, Nitinol will give considerably smaller forces than stainless steel--approximately one-fifth the force. So, the clinician should know that if he uses the same cross section of wire, he may be getting a larger deflection, but also much less force. Sometimes that is good, particularly if he previously was using too much force in steel. But, it also can be bad, if he's not building up to the optimal force levels required. He might find that as the wire works out and the force drops, he may not have sufficient force to get full alignment of the teeth. So, we have to look at more than the range of action of a wire. We have to look at the forces the wire produces as well. If the wire produces too much force, we'll get pain and necrosis in the periodontal ligament. If there is not enough force, we may not get the rapidity of tooth movement that we want.
There are ways to increase the range of action other than in the choice of alloy. A large range of action could be obtained by reducing the cross section of the wire. Smaller wires can be deflected further. But, there is the disadvantage that if the wire is too small, it might permanently deform. Another way to increase the range of action is to increase the interbracket distance, or to use loops in the wire. The promising thing about the new materials is that you don't have to complicate your design so much, if you rely on the materials with good characteristics.
DR. GOTTLIEB You mean you don't have to put in loops?
DR. BURSTONE That's right, and you can work with smaller interbracket distances. However,there is another reason for putting loops in the wire, in addition to getting a larger range of action, and that is to obtain the desired force system with minimum side effects. New, superior alloys cannot solve this problem alone.
DR. GOTTLIEB Is the load-deflection rate the same as stiffness?
DR. BURSTONE Load-deflection rate measures the stiffness of an appliance component.
DR. GOTTLIEB How does the orthodontist know what size wires to select, since stiffness is determined by both size and material?
DR. BURSTONE In the past, we used only steel wires and all we had to worry about was cross section to vary load-deflection rates. Now we have new materials with different moduli of elasticity, and braids with apparent moduli. To make it simple, I am recommending that the orthodontic companies use a numbering system on their wire packages to let the clinician know its stiffness. For instance, the wire stiffness (Ws) for four different wires are:
[show_img]266-jco-img-t1.jpg[/show_img]To compare the stiffness or the load-deflection rate of the wires, one needs to ratio the wire stiffness numbers. For instance, .016" steel delivers 2.7 times the force of a .018" X .025" D-Rect wire (256/96.6 = 2.7). An .018" Nitinol is somewhat stiffer than a .018" X .025" D-Rect. Unlike the old world of appliances, now the largest wires can deliver lower forces.
DR. GOTTLIEB How does load-deflection rate enter into selecting and designing an archwire?
DR. BURSTONE There are a number of things we want to build into appliance design. One would be consistency of force. That means a low load-deflection rate. If the load-deflection rate were high, there would be a rapid dropoff in force values every time the tooth would move. Since we would ike to keep forces relatively constant as the tooth is moving, we want the lowest possible load-deflection rates. With a low load-deflection rate, you automatically get a large range of action. Most orthodontists want this, because it means they don't have to reactivate the appliance very often.
Although the alloy you select, the cross section of the wire, and the interbracket distance are factors in lowering the load-deflection rate, the most important consideration is the configuration that you put in the wire. Currently, there is a lot of interest in using simple configurations, like straight wire. There are limits to how far you can go with a simple configuration. With a straight wire, the force system is determined by the shape of the wire with respect to the brackets. If you analyze the force system carefully, you may not like what you have. It is true that sooner or later the teeth may straighten out, but they may not end up where you want them. For example, if you place a straight wire in an upper arch with a deep overbite in a Class II division 2 case, you could level the upper arch, but end up with an occlusal plane that is steepened, and with the upper incisors not intruded. That may not be what you want. So, there is more of orthodontics than just lining up teeth. The key to successful treatment is to line them up and to orient them correctly in space according to your original objectives.
DR. GOTTLIEB You mentioned earlier that there was more than one reason to put loops in the archwire. This might be a good time to expand on that point.
DR. BURSTONE If you want to control the force system by varying the magnitudes of the forces and moments on adjacent teeth, this can be done by placing loops between the brackets. I think the point is missed on why loops should be used. One reason is to lower the load-deflection rate and deliver a more constant force. Another reason is to increase the range of activation, to deflect the wire further without permanent deformation. But, these are not the major reasons for putting in a loop. The major reason for putting in a loop is to control the force system to the teeth on either side of the loop.
Let me give you an example of how a loop would make some difference. Let's suppose that I have an L loop placed between a bicuspid and a cuspid and that the cuspid is super-erupted in relation to the bicuspid. If I face the L loop backward, not only will there be an intrusive force on the cuspid, but there will be a large moment or torque which would displace the cuspid root forward (Fig. 2A). On the other hand, if I take the same wire and make an L loop facing forward, there would not be as much of an undesirable moment tending to move the cuspid root forward, but a larger torque or moment on the bicuspid (Fig. 2B). So, if I am clever enough in selecting proper loop configurations, I an alter the relative force system. On the other hand, if I just placed a straight wire between the bicuspid and cuspid, the wire would dictate the system, and I would have no control over it.
DR. GOTTLIEB Unless one were to use pretorqued and preangulated brackets with the straight wire.
DR. BURSTONE Then the straight wire and angled brackets would dictate the force system. Bends must be placed to avoid undesirable side effects in many clinical situations. Most of us are using undersized wires, particularly in the posterior segment, so the torques are not that critical. Still, I think it is highly desirable to build in as much as possible in our strapups. Pretorqued and preangulated brackets can help in placing finishing detail. It certainly makes it a lot easier to finish a case, if a relatively straight wire can be placed. It is particularly important that few second order bends have to be placed. Of course, there are inaccuracies even with the best strapups and variations in tooth size and shape, all of which have to be compensated for with bends. There could be a danger of too much prefabrication, if that means that everyone is given the same axial inclinations. There is great variation required in mesiodistal axial inclinations for a well-finished case.
DR. GOTTLIEB Do you individualize axial inclinations for each case?
DR. BURSTONE I use 45° headfilms as well as periapicals to determine axial inclinations. I want good dispersion of the roots along with good intercuspation of the crowns. If we want to treat roots as well as crowns, we can't use standardized axial inclinations. For this reason, I don't think that standard numbers can be used in the second order direction. With bonding, there is no reason why we can't give every patient what they really need in the way of axial inclination.
As far as third order is concerned, the lower incisors are quite variable in axial inclination. It depends on how far forward or backward you want them. A nonextraction case with flared anterior teeth has a different angle required in the brackets than a case with upright lower incisors. Also, there is a lot of variation in the buccolingual axial inclinations of the posterior teeth and the curve of Monson. So, we can't use standard angles with the idea that they will automatically give us what we want at the end of treatment. But, one advantage of using the averages with undersized wires is that you are apt to get into less trouble by starting with the average than if you started with just straight slots, using straight arches.
DR. GOTTLIEB You'd have to be willing to reband a lot of teeth if you start everyone with the average and then recognize that you needed to individualize to some extent. Either that or you have to bend the archwire. However, I don't think anyone, including Andrews, ever represented that it was an inviolate straight wire. It's a straight wire a percentage of the time.
DR. BURSTONE My point is that you do not have to rebracket if you use oriented radiographs to determine mesiodistal axial inclinations, rather than using crown morphology alone. Treatment planning includes determining the axial inclinations for the patient. Individualizing at the beginning will save time and effort in the long run. In a sense, I suppose I have always used a straight wire technique by angling my brackets in a second order direction. The "torques" weren't built in, but the object was a strapup that would permit finishing with as simple a wire as possible. Now I use brackets with built-in "torque". I have often said that the Segmented Arch technique can be a crooked arch technique, because we place the buccal segment wires early in treatment, and often just leave them. If you have a little discrepancy in your strapup--not that we recommend poor strapups--you don't have to keep reduplicating the bends in the wire. Even with the best strapups, the finishing wire is apt to have many little bends. A finishing arch may not look perfectly symmetrical, and the wire that makes the case look beautiful at the end of treatment may not look beautiful if placed on a flat ideal arch chart. Because of occlusal interferences or gingival impingement, brackets may have to be staggered and bends may be required. Just having the brackets in the right place, so that a straight wire will hold and aid in finishing procedures, has much to do with the major mechanics of treatment and treatment objectives. Although it is possible to place a wire in malaligned brackets and work your way up through eavier wires, and finally line up all the brackets and the teeth, this to me is not quality orthodontics, because it doesn't determine the position of the teeth in three-dimensional space. Because of the nature of the side effects produced, you can temporarily end up with teeth in poor positions and permanently not reach your objective, even if the brackets appear well-aligned. For example, if a maxillary cuspid at the beginning of treatment had a root forward, and we must angle our bracket to the occlusal plane. If you put a continuous straight wire into the angled cuspid bracket, the anterior teeth will erupt and produce a deep overbite. Now, you can wait for everything to level out again with the wire, or most likely other wires, but there will be no way to finally intrude the incisors and get them back towards the position that you wanted. The result is a level arch with a steep plane of occlusion. It is a fine idea to have a strapup as ideal as possible, but beyond that is where we have to design our mechanics to put teeth where we want them to be.
DR. GOTTLIEB You don't agree with the idea of tying in an entire arch from the start of treatment.
DR. BURSTONE You are referring to a continuous arch with ideal form. I think to blindly tie in a continuous arch and let the wire do our thinking for us can produce irreparable damage, and prevent us from reaching our objectives in a large percentage of our cases. You have to design your mechanics so that you are selectively moving teeth, without side effects.
DR. GOTTLIEB You divide appliances into active and reactive portions. Please define these.
DR. BURSTONE Every archwire we put in not only has an active force system that we use to move the teeth that we would like to move, but also has a reactive force system, which relates to what we commonly call anchorage. It is easy sometimes to design an appliance to give the active force system, but what really challenges an orthodontist is to provide a reactive force system which is less apt to disturb the anchor teeth. There are many ways that this can be accomplished. One of the weaknesses of continuous arch mechanics is that the anchor tooth is just the adjacent tooth. Weare pitting one tooth against the next, and the wire does our thinking for us. In segmented arch technique, we use lingual arches, which dissipate the forces across the arch. Also, bypassing teeth avoids pitting adjacent teeth against each other. The magnitude of the force is critical in anchorage control. The reactive forces are less apt to disturb anchorage, if you keep the magnitudes low enough so that only the active teeth move.
DR. GOTTLIEB Do you band progressively at times?
DR. BURSTONE Yes. In an extraction case in the permanent dentition, I might retract cuspids first, until there was room for alignment of the anterior teeth, and only at that point bond the anteriors. Generally, I like to get onto the anteriors early in treatment, to intrude and correct deep overbite, and start en masse space closure.
DR. GOTTLIEB Do you ever bypass cuspids and bicuspids by not bracketing them?
DR. BURSTONE Usually, I try to band or bond all the teeth that are present in the mouth for control. If, for instance, we are using a base arch to the anteriors for intrusion, I like the security of knowing that I have a bicuspid in place attached to a buccal segment, which adds to the anchorage. Without all the teeth present, we could have some steepening of the occlusal plane. Using an auxiliary tube to the molar provides all the advantages of bypass. The point of departure off the buccal segments from an auxiliary tube means that the wire for retraction or intrusion does not have to come from the most anterior tooth in the segment, i.e., the bicuspid. If I am separately intruding incisors, I may not immediately bracket the cuspid.
DR. GOTTLIEB Could careless mechanics result in the rotation of the entire reactive segment?
DR. BURSTONE If intrusion is desired, too high forces produce large moments on the posterior teeth, which rotates or steepens the plane of occlusion of the maxillary arch. The roots of the posterior teeth are displaced forward. People talk about careless mechanics, and sometimes wires not fabricated carefully, but I think it is the concept that is more frequently careless. Most of the undesirable side effects can be predicted ahead of time. For example, in a first bicuspid extraction case, if we want to retract either the cuspids or all six anterior teeth as a unit, it is predictable that the buccal segments, as viewed from the occlusal, will want to rotate, since you are putting an anterior force on the posterior teeth buccal to the center of resistance. The bicuspid will move lingually and the first and second molars buccally. To me that's not sloppy wires. It is sloppy concept, because it can be avoided by placing a removable lingual arch, as we do.
In retracting the cuspid, the mesial force on the buccal segment causes the buccal segment to tip into the extraction site. That should be anticipated and there should be a large enough moment or torque or tipback to prevent that. The more closely you are able to calibrate your force system, the fewer surprises you are going to have. For example, in some techniques you can compensate for rotation by placing tipbacks, toe-ins, and expansion; but, the activations are imprecise and must be monitored carefully. With an appliance that can give you a predictable force system, there should be no surprises as space closure proceeds.
DR. GOTTLIEB How would you describe the appliance with the predictable force system?
DR. BURSTONE The approach that I have used for delivering predictable force systems is to develop assemblies or components that have been calibrated in the laboratory. For example, the Segmented Arch anterior retraction assembly has a spring and a base arch, but the whole assembly attaches at just two points--an auxiliary tube on the molar and a vertical tube on the cuspid. In this force system, we are not worried about a lot of reactions tooth-to-tooth, because we have just two points of attachment. Since the springs have been calibrated, we know how many millimeters of activation to place and how much of a tipback to place in the posterior region. For instance, a typical activation for en masse space closure with a 6mm spring might be 7mm of activation to deliver 250 grams of force, a tipback of 30° in the posterior region, an anti-tip moment in the anterior region of 90.° When this is placed, the anteriors should tip back with the center of rotation close to the apex of the incisors and the posterior teeth should not tip into the extraction site. If they move at all, they would translate forward. This is an example of a controlled force system. The force system can be varied for the individual case.
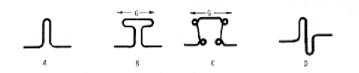
I should also point out that there is a reason for the design of various loops used in the retraction springs. Within recent years there has been more interest in the placement of added wire or configurations between brackets. The shape of the loop is determined by the force system you want and it is not true that the more wire you put between two brackets the better. It's where you place the wire that is important. More wire should be placed in what is technically a part of the critical section. In poorly designed loops, a lot of wire may be placed, but in the wrong spot. If it is placed in the wrong spot, it may not have much of an effect on the load-deflection rate. Even more important is what added wire does to the force system. We have already talked about the difference it makes if an L loop is faced forward or backward during leveling. Where you place the wire is also very important in designing a retraction loop or spring.
DR. GOTTLIEB Could you focus in on where you place it? What's the right place? What's the wrong place?
DR. BURSTONE In designing a loop for space closure, not only do we want a force tending to move the crowns together, but we would like the roots to be controlled as well. That means that on the cuspid we need a torque or a moment, which tends to move the root back and the crown forward. If we want to move the tooth bodily, or translate it, we would like to develop as much moment as would be required to control the tooth. On a typical cuspid, that might mean a moment that is about twelve times as large as the magnitude of the force. If we use a vertical loop, when it is activated, not only do you develop a force, but you also develop a moment in the proper direction to control the root, because the arms will go up at an angle as you activate the loop. But, unfortunately, with a simple vertical loop you only get a moment to force ratio of less than 2:1 and we said we needed 12:1.
The moment to force ratio can be increased by making the loop longer and wider gingivally. When you increase the wire gingivally, not only do you lower the load-deflection rate and get less force, but you also get more moment to control the root for any given amount of force. But, you run out of room for such a loop. Eight millimeters, occasionally 10, is about as long as you can get without soft tissue impingement. Typically, it should be around 6 to 8 millimeters. If we designed a retraction spring with additional wire placed occlusally in order to improve comfort, the wire would be placed in the wrong place. The more occlusally you put wire, the more you tend to throw the root forward. Since there are limitations on how far we can go gingivally with a simple vertical loop, additional wire placed gingivally is most helpful in raising the moment to force ratio (Fig. 3).
DR. GOTTLIEB What do you mean by moment to force ratio?
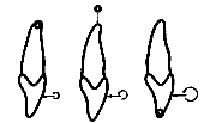
DR. BURSTONE It can be demonstrated that where a tooth will move is determined by the moment to force ratio. The force refers to any single force that is applied at the bracket to the crown of the tooth. However, if we just apply single forces, we are very limited in the type of tooth movement we can produce. We could only produce centers of rotation close to the center of the root. If we would like to produce different centers of rotation to tip a tooth at its apex or move it bodily, we do this by adding a pure moment or a couple to the single force.
DR. GOTTLIEB What is a pure moment or a couple?
DR. BURSTONE A pure moment or a couple is two forces that are equal and opposite, not in the same line of action. Since the forces are equal, it has no effect on moving teeth in a linear direction. If you grab the steering wheel of a car and pull down on one side and up on the other, that is a couple. A couple will tend to spin a tooth around its center of resistance, since its two forces are separated by a distance. It produces a twisting action and, combined with an additional force, we can produce various centers of rotation of teeth.
DR. GOTTLIEB Could you please describe how that occurs?
DR. BURSTONE If we put a loop in a round archwire and activate it to produce a lingual force, we could tip upper incisors lingually with a center of rotation near the center of the root. If we add some lingual root torque anteriorly by using a rectangular wire, we could put the center of rotation at the apex. This would control the tipping and the root would not displace forward. We have produced a given moment to force ratio (lingual force to torque). If we increase the amount of torque and keep the force the same, instead of tipping the tooth would translate. If we increase the torque more, we can hold the incisal edge where it is and move the root lingually. Varying the torque or moment to force ratio can produce different centers of rotation (Fig. 4). It is difficult to calibrate the moment to force ratio in a simple wire, and that is why many retraction appliances can be so unpredictable. The load-deflection rates are so high that even if you have the right moment to force ratio to begin with, it could change as the tooth begins to move. The tooth could wiggle back and forth during space closure.
DR. GOTTLIEB What about using force gauges to measure forces in the mouth?
DR. BURSTONE Orthodontic force gauges only measure forces. A force gauge can measure the force of an intrusive arch or an elastic pull, since only a force reading is required to describe the force system. They can't measure the torques or the moments. Most appliances produce forces and moments. Therefore, a force gauge does not give you the information that a clinician needs. Force gauges are also limited in their application, because of their inaccuracy.
DR. GOTTLIEB Do the precalibrated springs tell you anything more than force?
DR. BURSTONE In a precalibrated spring, the millimeters of activation is measured and, by using a table or a computer, the orthodontist can know his force system. One reason for prefabrication is that, as you change the geometry of a loop, you can radically change the magnitude of the force and the moment to force ratio. Prefabricated springs are more predictable.
DR. GOTTLIEB Do you know the moment to force ratio in a precalibrated spring?
DR. BURSTONE Yes. For a given activation, not only do you know the force of a retraction spring, you know the moment on the anterior segment on a cuspid, the moment on the posterior segment, and you also know the vertical forces that are present. With this body of data, if you produce a given activation, you then know the forces and the moments that you will get in the mouth. Hence, the tooth movement is more predictable.
Every orthodontist in some way relates his activations to the type of force system that he is getting. If he uses a loop for space closure and after three weeks the posterior segments tip into the extraction site, technically we would say that there is not enough moment on the posterior segments. While he may not use the same terminology, he would do something to correct the problem, such as increase the amount of tipback in the posterior segment. But rather than do this by the seat of our pants in a hit or miss manner, I think it is far better to put in predictable forces, so that you can be assured that you are going to get the response that you expect.
DR. GOTTLIEB You mentioned that you like to use undersized wires in the bracket slots. Doesn't this create too much play for the wire to be effective?
DR. BURSTONE It is true that if there is too much play, orientation is lost, but I think there is an advantage in having some play between the wire and the bracket. If you are aligning and rotating teeth, the brackets have to slide along the wire to assume their correct position. Many posterior segments have pretty good buccolingual axial inclinations at the beginning of treatment, and we would be well advised in the average case not to change them. If you do change them, you are likely to run into crossbite problems or place roots through the buccal and lingual bony plates. There are a lot of advantages to using undersized wires, provided they are rigid enough to hold an arch form. Lighter wires, with or without loops, can be overbent during the stage of initial alignment, eliminating undesirable play.
DR. GOTTLIEB Do you discontinue undersized wires in the later stages?
DR. BURSTONE No, I prefer to use undersized wires in the finishing procedures. Rarely will I use anything larger than an .018" X .025" in an .022" slot, at least in the anterior segment. The only time you may want to fill up the bracket slot is for third order activation or torque, or to connect teeth rigidly. I don't think that most steel edgewise wires are that efficient anyway, if you want third order corrections. I prefer specialized, constant-force root springs.
DR. GOTTLIEB Would the TMA wire be especially good for torque?
DR. BURSTONE TMA wire can be efficient in producing torque, because of its low load-deflection rate and its high maximum elastic deflection. For example an .018" X .025" TMAwire twisted about 30° in the upper incisor region would deliver about 1500 gm-mm using twin brackets in the average patient. An .018" X .025" steel wire requires only 17° of activation for the same effect and it is less efficient, since the torque dissipates more rapidly and it is more difficult to determine the proper activation, because a few degrees of error in fabrication radically changes the torque. So, more is involved than just filling up the bracket slots and hoping that the wire will give you the inclinations that you want. That is why I prefer to vary the material of the wire for stiffness to control play.
DR. GOTTLIEB How does that relate to a straight wire arch in pretorqued and preangulated brackets?
DR. BURSTONE The reason that "straight wire attachments" work is that most orthodontists use undersized wires, and there is enough play so that you are not really producing third order changes. Let's assume there was no play between the wire and the bracket, and you have some type of vertical loop for cuspid retraction. You wouldn't have a high enough moment to force ratio to control your root apices when you retract. If you wanted to control them, you would have to place a "gable" bend in the wire. So, another way to do it is to angle the brackets in a second order direction. I imagine that some orthodontists are putting more angulation in their brackets, because they are having trouble controlling their axial inclinations during retraction. However, it is expecting too much for these angulations to give the proper moments or torques. I prefer to use average angulations for a typical strapup, because I would be building the force system into my ires.
DR. GOTTLIEB Do you have an opinion on gnathostatic finishing?
DR. BURSTONE Orthodontics has rediscovered what dentistry has been talking about for a long time--principles of occlusion. There is a lot of argument about what is ideal functional occlusion. I think the most important concept is the coincidence of centric relation and centric occlusion. The concept of cuspid rise is debatable. No rise is acceptable, provided there are no balancing contacts. However, cuspid rise is a convenient way to minimize balancing contacts. In treating open bites and deep overbites, it is hard to know what function we should build into them. I am reluctant to treat a deep overbite to too much cuspid rise or to have disengagement anteriorly immediately after treatment, because I have worked too hard to correct the deep overbite. I want over-treatment in the vertical dimension, particularly if the mandible has been rotated open during treatment.
DR. GOTTLIEB What about the relationship of functional occlusion and TMJ dysfunction?
DR. BURSTONE There is a lot of interest in TMJ in relation to occlusion, but I am not sure that anyone has shown positively that variations in function are really what produces TMJ problems. Most evidence is anecdotal. In treating orthodontic cases, we ought to treat to good functional occlusion, placing centric relation and centric occlusion close together with no balancing interferences. But, it is hard to say whether this will be preventive of TMJ problems.
DR. GOTTLIEB How precise can you be in regulating occlusion?
DR. BURSTONE I think that centric relation can be established clinically, without a gothic arch tracing or a hinge axis registration in most patients. If we place the teeth within ½mm, we are doing pretty well. Teeth migrate after treatment. To get a more accurate registration, to ¼mm, usually is not warranted. I think that casts should be trimmed in centric relation, not centric occlusion, for diagnostic purposes. I scribe a V-shaped groove on the backs of my models, which positively orients the casts in centric. The groove also orients the occlusogram used for treatment planning and wire design. l don't usually mount casts on an articulator, although that might be useful for certain patients. The occlusogram that I use is equivalent to an articulator mounting.
At the end of treatment, we will want to see if CR and CO coincide, but--once again--I think that can be determined clinically. Occasionally, muscle spasm makes this difficult. A headgear can be used on a Class II patient, if a small discrepancy develops between CR and CO during retention. It is true that lateral and protrusive movements can be evaluated more carefully on an articulator, but the percentage return on mounting cases on an articulator can be minimal in the average patient. It is a healthy sign that orthodontists are taking a greater interest in functional occlusion. More objective research is needed in this area.
DR. GOTTLIEB Charles, I want to thank you on behalf of our readers for this interesting discussion on the important subject of orthodontic force control.