(Continued from the April 2005 issue of JCO.)
DR. KEIM Your presentation at the AAO annual session last year in Orlando focused on the development of alveolar bone and periodontal tissues by means of tooth movement to prepare implant sites. Can you give our readers an overview of this principle?
DR. ZACHRISSON The creation of new alveolar bone and gingiva in the vertical plane by means of selective orthodontic extrusion of single teeth utilizes the normal tissue reactions to tooth movement (Figs. 14, 15, 16, and 17). When the periodontal fiber bundles elongate, new bone will be deposited in areas of the alveolar crest along the stretched fiber bundles. The bone deposition is a result of the tension exerted by the stretched fibers. The ability to affect the environment is maintained along the entire attachment apparatus of the root, as long as the residual apical attachment is healthy.21
Similar articles from the archive:
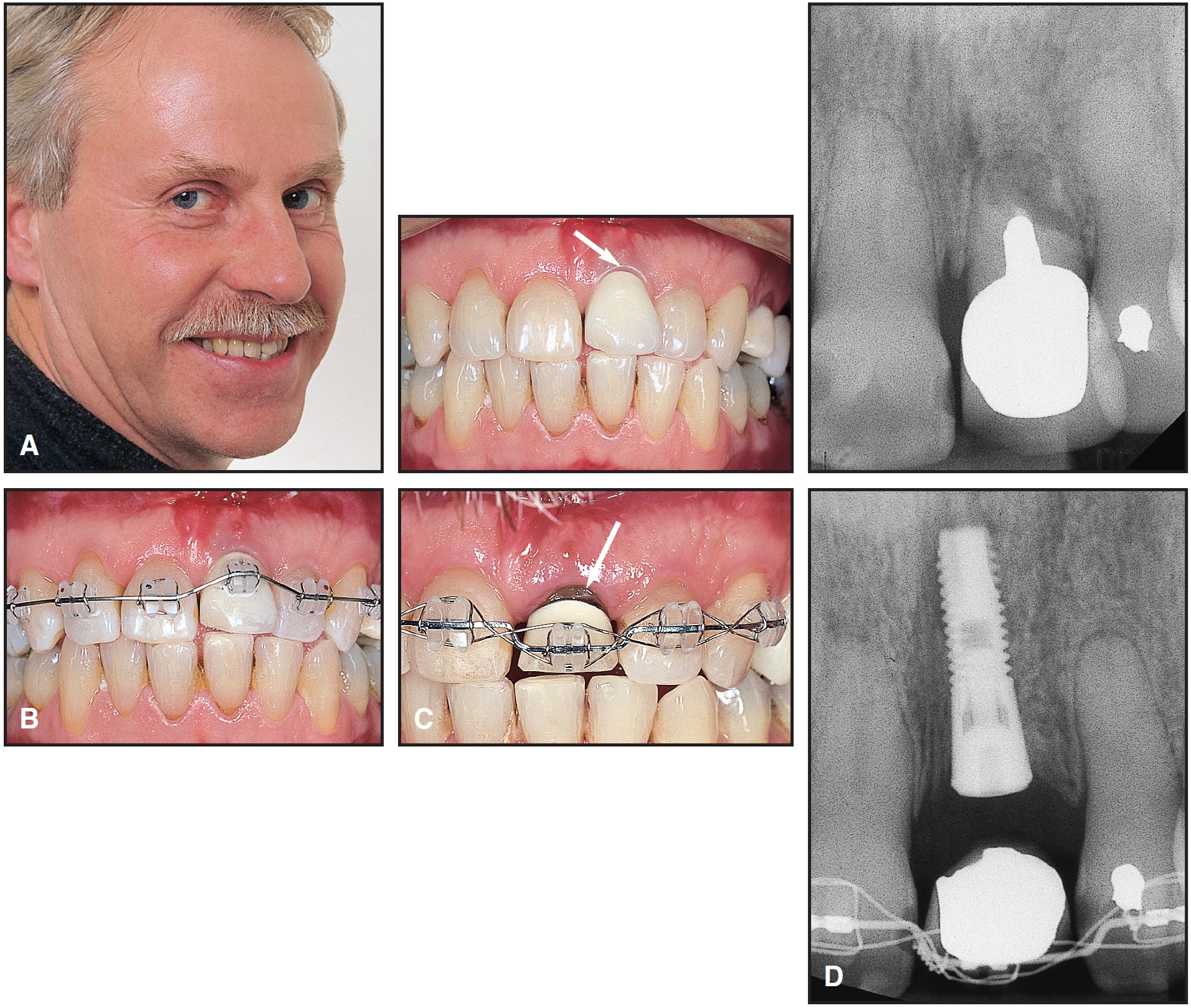
Fig. 14 A. Adult male patient whose maxillary left central incisor had poor prognosis and more apical gingival margin (arrow) than on adjacent central incisor. B. Implant site development by extrusion of left central incisor, with bracket bonded apically, and initial leveling with superelastic wire. C. Interrupted continuous forces used to extrude incisor; incisal edge progressively ground out of occlusion with opposing arch. Increased root exposure (arrow) confirms that gingival tissue does not completely follow extruded tooth. D. Both labial soft tissue and alveolar bone followed extruded incisor enough to allow placement of implant-supported crown. (Reprinted by permission.41)
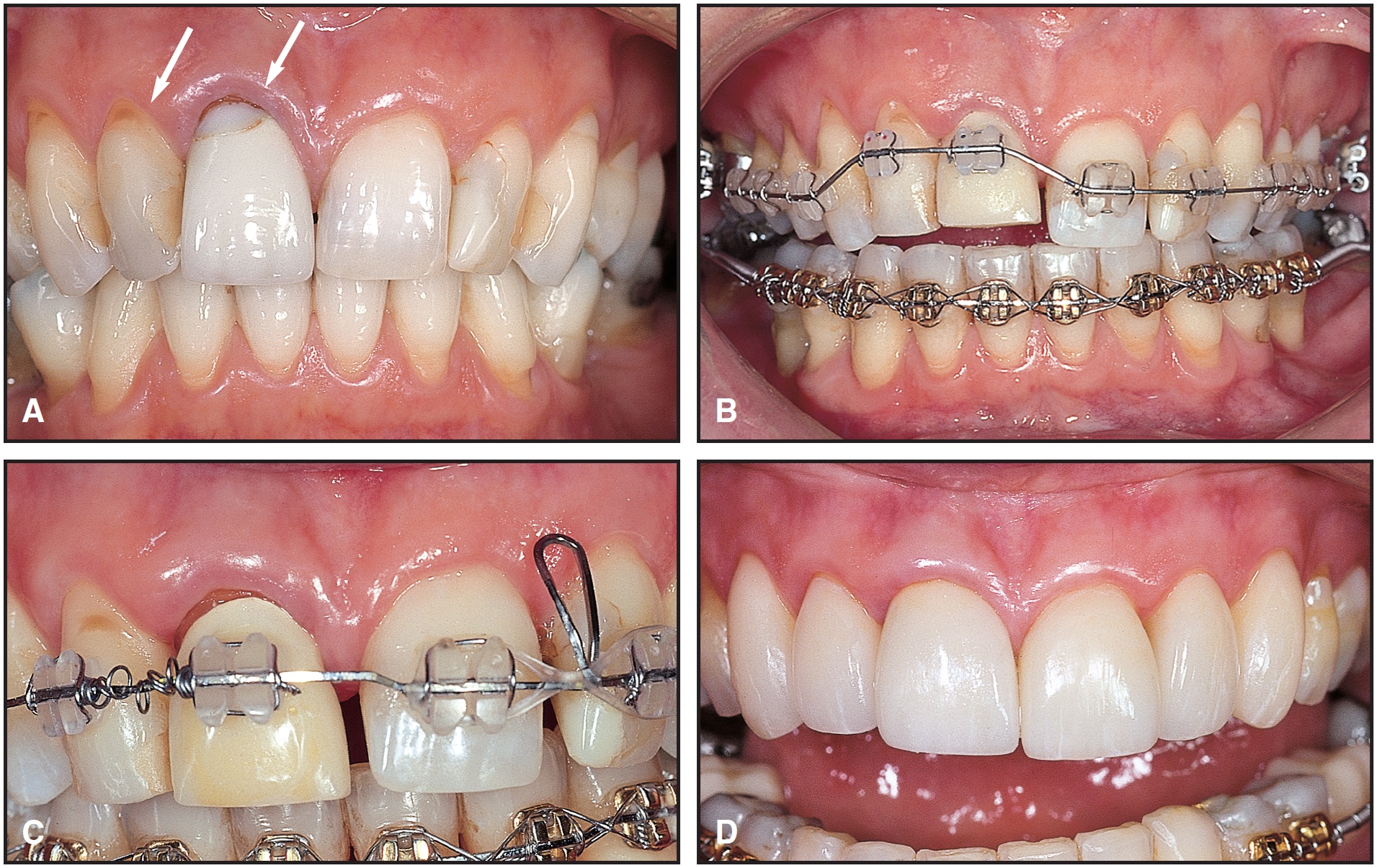
Fig. 15 A. 55-year-old female patient with labial gingival recession before treatment (arrows). B. Brackets bonded apically, and continuous force from superelastic wire used for extrusion of maxillary right lateral and central incisors. Incisal edges were ground with diamond bur to avoid occlusal interferences. C. Improvement in gingival levels after three months of treatment. D. After placement of six porcelain laminate veneers (courtesy of Dr. Roy Samuelsson, Oslo, Norway), note improved symmetry of anterior gingival levels. (Reprinted by permission.41)

Fig. 16 A. Adult female patient with severe local periodontal tissue breakdown (see Figure 17). Bone support for mandibular right first premolar was much better than that for canine and second premolar (arrows). B. Slow orthodontic extrusion of canine and second premolar used to improve vertical bone height prior to placement of implant-supported restorations. After removal of pulps, incisal edges of extruded teeth were ground to avoid jiggling with maxillary teeth. C. After 10 months of leveling, extruded teeth were extracted with forceps. Note even gingival and bone levels. D. Marked improvement in periodontal tissues around implant crowns one year after treatment. (Reprinted by permission.41)
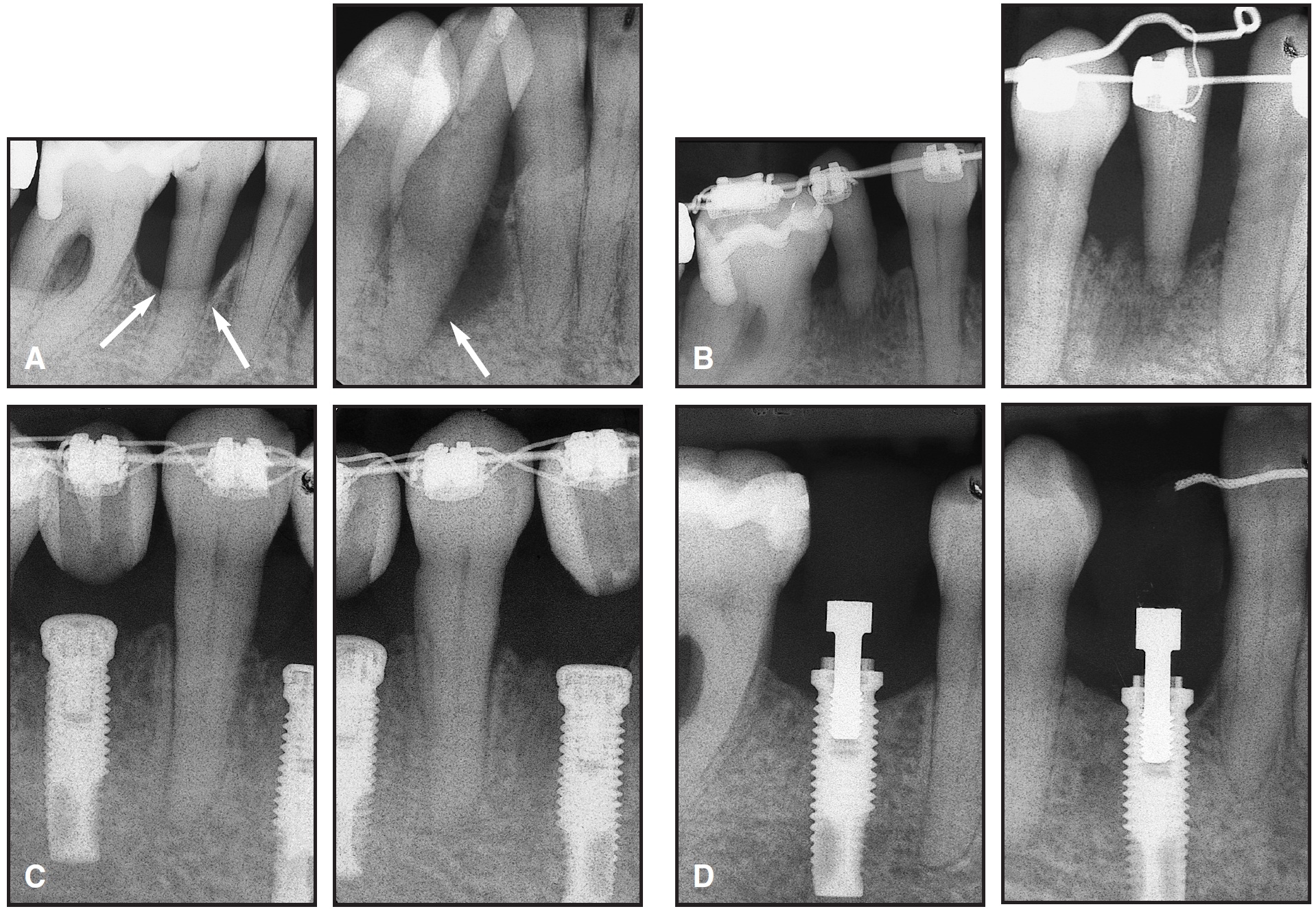
Fig. 17 A. Same patient as in Figure 16, showing bone levels before treatment (arrows). B. Remarkable amount of bone build-up after 10 months of leveling (darker areas indicate immature bone). C. After placement of implants. D. Normal appearance one year after treatment, with bone levels up to first threads of Brånemark implants.
This offers a unique possibility to use teeth with a poor or hopeless long-term prognosis for regenerative purposes (Figs. 14, 16, and 17). Salama and Salama suggested the term "orthodontic extraction", since the purpose is to extrude the tooth, with all the augmentative benefits inherent to the process.22 They used four to six weeks for the eruptive phase, followed by six weeks of stabilization before the tooth was removed and the implant was placed. It should be noted that the orthodontic extrusion does not create a new attachment, but merely relocates the existing attachment in a coronal direction. The relationship between the CEJ and the bone crest is maintained--in other words, the bone follows the tooth. The marginal periodontium migrates with the extruding tooth, while the location of the mucogingival junction remains stable.23,24 The labial gingival margin follows the extruded tooth about 80% of the distance (Figs. 14 and 15). Thus, the clinical crown length of an extruded tooth may increase by some 20%,24 and the width of the attached gingiva will also increase.
In the horizontal plane, tooth movement may be an exciting alternative to bone grafting or other surgical augmentation procedures (Figs. 18 and 19). The principle is that a tooth (generally a premolar) is moved orthodontically into an edentulous space, and the implant is placed in the position previously occupied by the tooth that has been moved. The bone deposited on the tension side behind the orthodontically moved tooth recreates a surprisingly wide bony ridge that will be optimal for placement of the implant (Figs. 18B,C and 19B-D).

Fig. 18 A. 41-year-old female patient with agenesis of both mandibular central incisors, multiple spaces, thin periodontal tissues, and prominent root topography. Alveolar ridge was too thin labiolingually to allow implant placement in anterior region (arrow). B. Orthodontic movement used for implant site development mesial to mandibular left first molar. C. Wide area of bone on tension side provided ample space for titanium implant. Panoramic radiographs taken before (D) and after (E) treatment show placement of implant in area previously occupied by left second premolar. (Reprinted by permission.41)
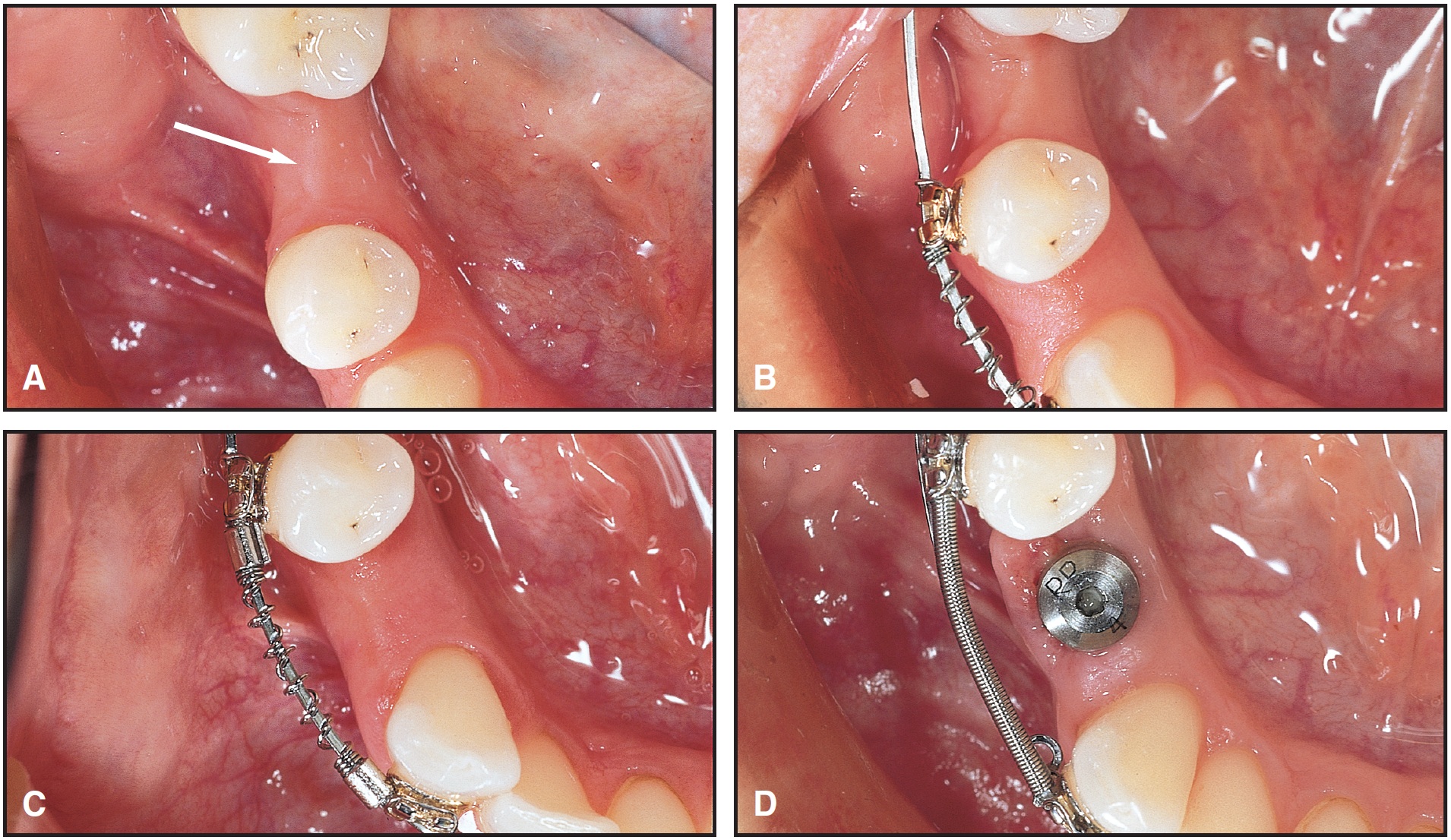
Fig. 19 A. Adult female patient requiring implant in narrow area of alveolar bone, mesial to first molar (arrow). B. Horizontal implant site development by distal movement of mandibular right first premolar with continuous force from superelastic coil spring. C. Wide area of bone developing on tension side. D. Ample buccolingual space provided for implant.
DR. KEIM How fast can teeth be erupted to prepare a site vertically?
DR. ZACHRISSON Slow orthodontic extrusion of teeth (and roots) appears to have a unique potential for significant vertical alveolar and labiolingual ridge augmentation without surgery. However, we do not know at present how slowly it is necessary to extrude the teeth for the bone to follow optimally and to obtain the most successful orthodontic ridge augmentation. To my knowledge, there exist no scientific studies of what kind of force systems (continuous vs. interrupted forces, segmented vs. continuous archwires, etc.) and what force levels and treatment times should be recommended to obtain the most efficient, complete, and predictable regeneration of bone. As I mentioned, Salama and Salama used only four to six weeks for the extrusive phase,22 whereas a more recent study by Zuccati and Bocchieri of nine teeth in seven patients used three to four months for the extrusion, and the implants were inserted two to four months later, when the soft-tissue healing was complete.21 Based on empirical considerations, we prefer to use interrupted continuous forces that allow rest periods between the activations, and our treatment times may be as long as 10 months or more (Figs. 14, 15, 16, and 17).
DR. KEIM How fast can teeth be moved horizontally to develop a hypoplastic implant site? Is there any danger to the teeth or alveolar bone from moving the teeth too rapidly?
DR. ZACHRISSON By slow, bodily movement of teeth into edentulous areas of reduced bone height, the periosteum on the labial and lingual surfaces of the alveolus will normally form bone.25 On the tension side of the teeth, the full height of the bone will be maintained (Figs. 18 and 19). If the teeth are moved too rapidly, there is a risk for development of a dehiscence.25,26 Since the principle involved in horizontal implant site development as a rule is to move a selected premolar one tooth width mesially or distally, and the rate of tooth movement is optimally around 1mm per month when a continuous force is used, the treatment periods for horizontal implant site development may approach one year.
However, the problem of how fast the teeth can be moved without compromising the integrity of the moved teeth and without losing any bone largely depends on the degree of vertical and horizontal atrophy of the edentulous segment. Clinical studies have shown that reconstruction of an atrophied alveolar ridge after previous extractions may occur during tooth movement.27-29 Periosteal bone apposition takes place in the pressure direction in front of the tooth and in a labiolingual direction. However, when the alveolar ridge is quite narrow, as with long-standing extraction spaces (approaching a knife-edge appearance), with buccal and lingual layers of dense cortical bone and little trabecular bone in between, we have experienced iatrogenic damage. Thus, extensive lateral root resorptions may occur in the alveolar ridge areas when teeth are moved with continuous force from superelastic coil springs (Fig. 20). We don't know yet if we can avoid such resorptions by using discontinuous forces, preorthodontic alveolar ridge augmentation by means of guided tissue regeneration, 30 surgical alveolar ridge augmentation,29 corticotomy, or cortical perforation.31 Further studies are needed to elucidate this problem.
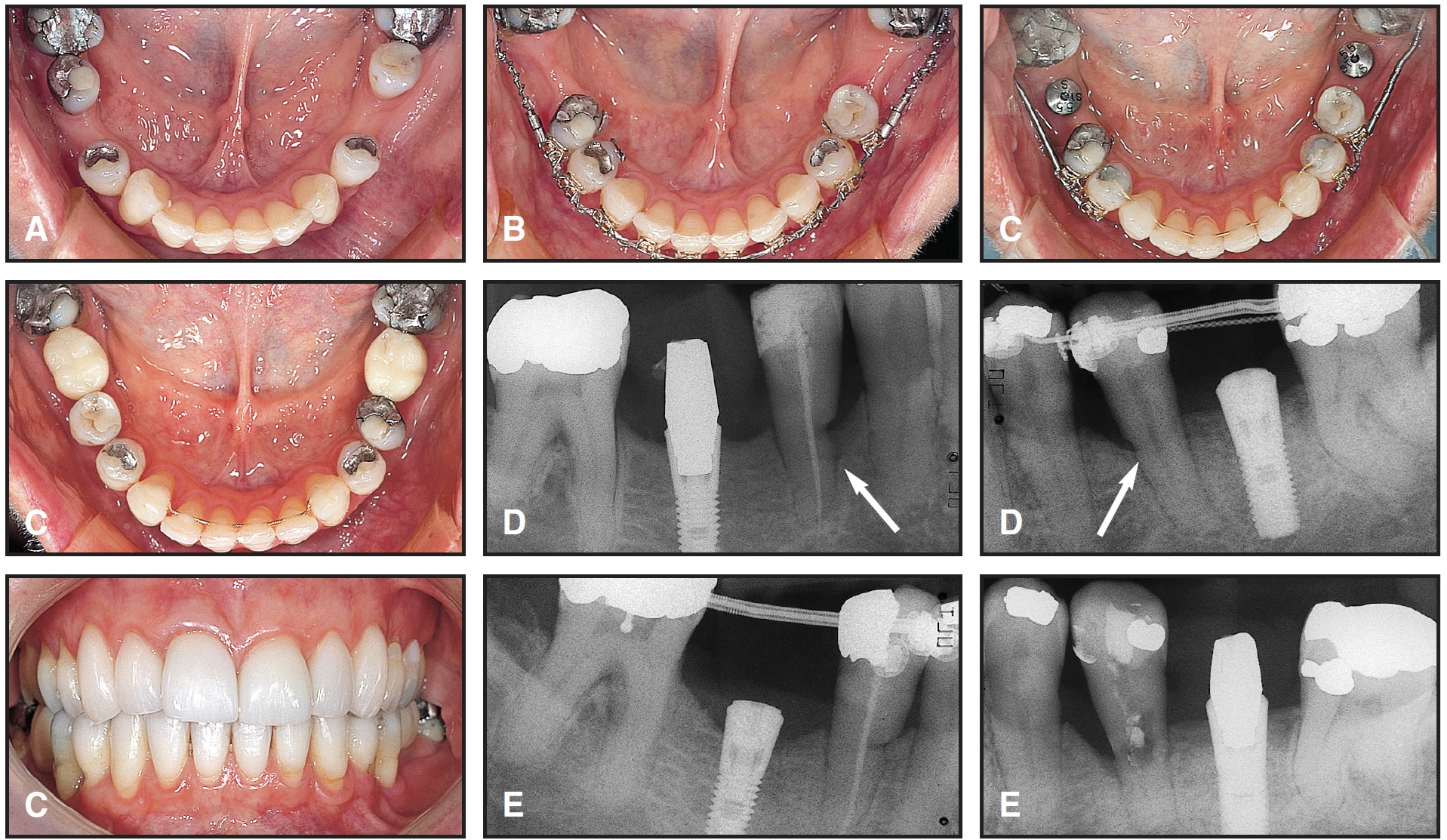
Fig. 20 A. Adult female patient (same as in Figure 15) with buccolingually thin alveolar process, contraindicating implant placement without surgical ridge augmentation, especially on right side. Nonsurgical treatment was planned. B. Second premolars derotated and moved mesially into contact with first premolars, which were also derotated. C. Increased buccolingual width of alveolar bone on tension side, allowing placement of two implants. D. Radiographic evaluation confirms successful osseointegration of implants in newly regenerated alveolar bone, but shows pronounced lateral root resorption on pressure sides of both premolars (arrows). E. One year later, left first premolar had to be extracted, and long-term prognosis for right first premolar was poor due to resorption in marginal portion of root.
DR. KEIM In what instances would you use orthodontic tooth movement to develop bone in both planes of space?
DR. ZACHRISSON Whenever it is needed. Figures 15 and 20 and Figures 21 and 22 show two such cases. In the first case, early extractions of both mandibular first molars in a female 55-year-old patient had left an alveolar process that was thin buccolingually, so that implant placement was contraindicated on both sides without some form of ridge augmentation (Fig. 20A). At the same time, this patient had marked labial gingival recessions on the maxillary right lateral and central incisors (Fig. 15A). As an alternative to surgical correction of both problems, a biological, nonsurgical approach was chosen.
The complicated case in Figures 21 and 22 required orthodontic extrusion of the right lateral and left central incisors to develop alveolar bone for three implants, as well as mesial movement of the right central incisor toward the midline. The extrusion of the incisors required 11 months of treatment, and the implants were inserted at 15 months (Fig. 22D).
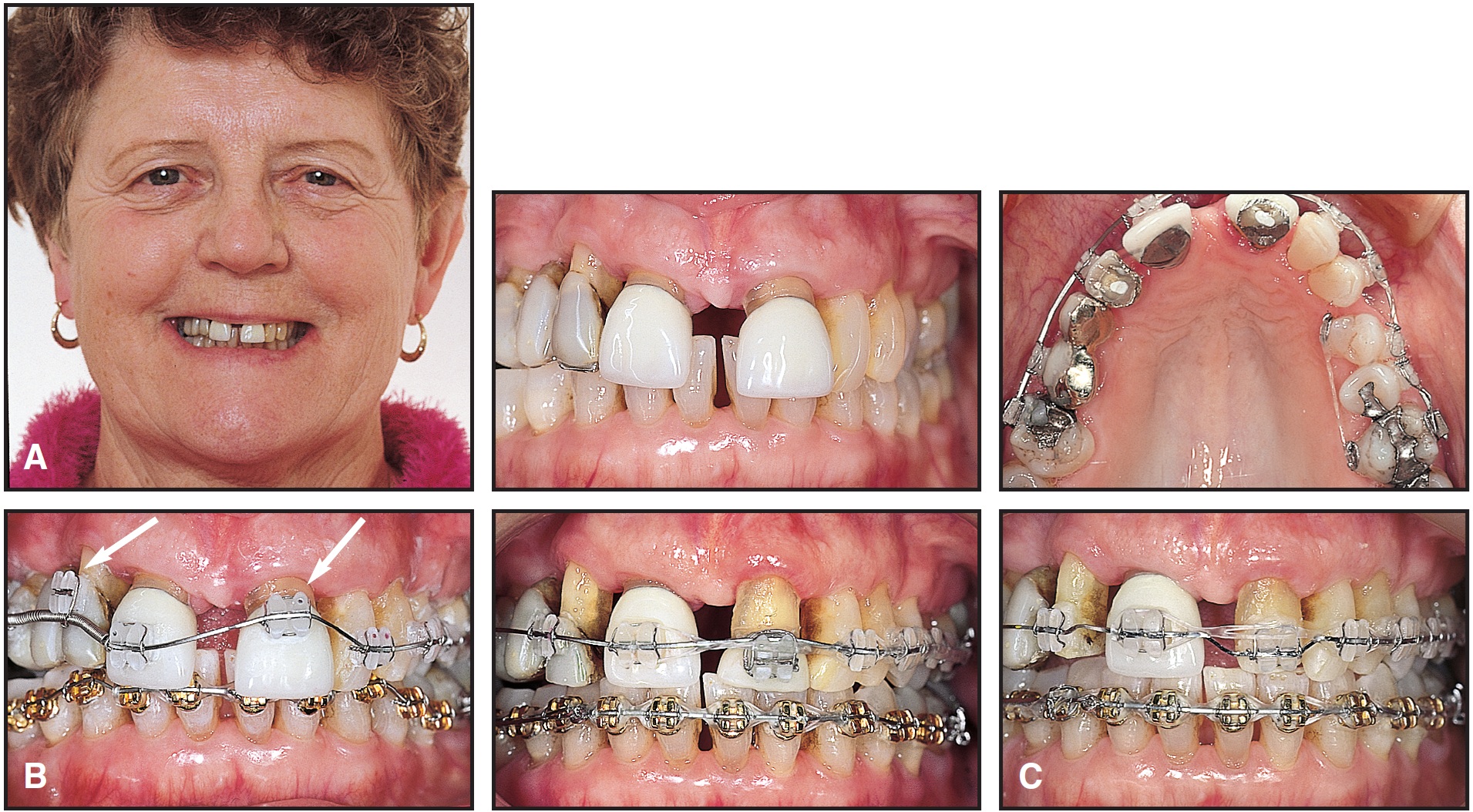
Fig. 21 A. Horizontal and vertical implant site development in 66-year-old female patient with severe periodontal tissue breakdown (see Figure 22). B. Brackets bonded apically on porcelain crowns of maxillary right lateral and left central incisors for orthodontic extrusion (arrows); right central incisor was moved mesially to correct midline deviation. C. Extruded crowns were ground incisally to avoid jiggling with mandibular teeth, and later rebonded onto roots.
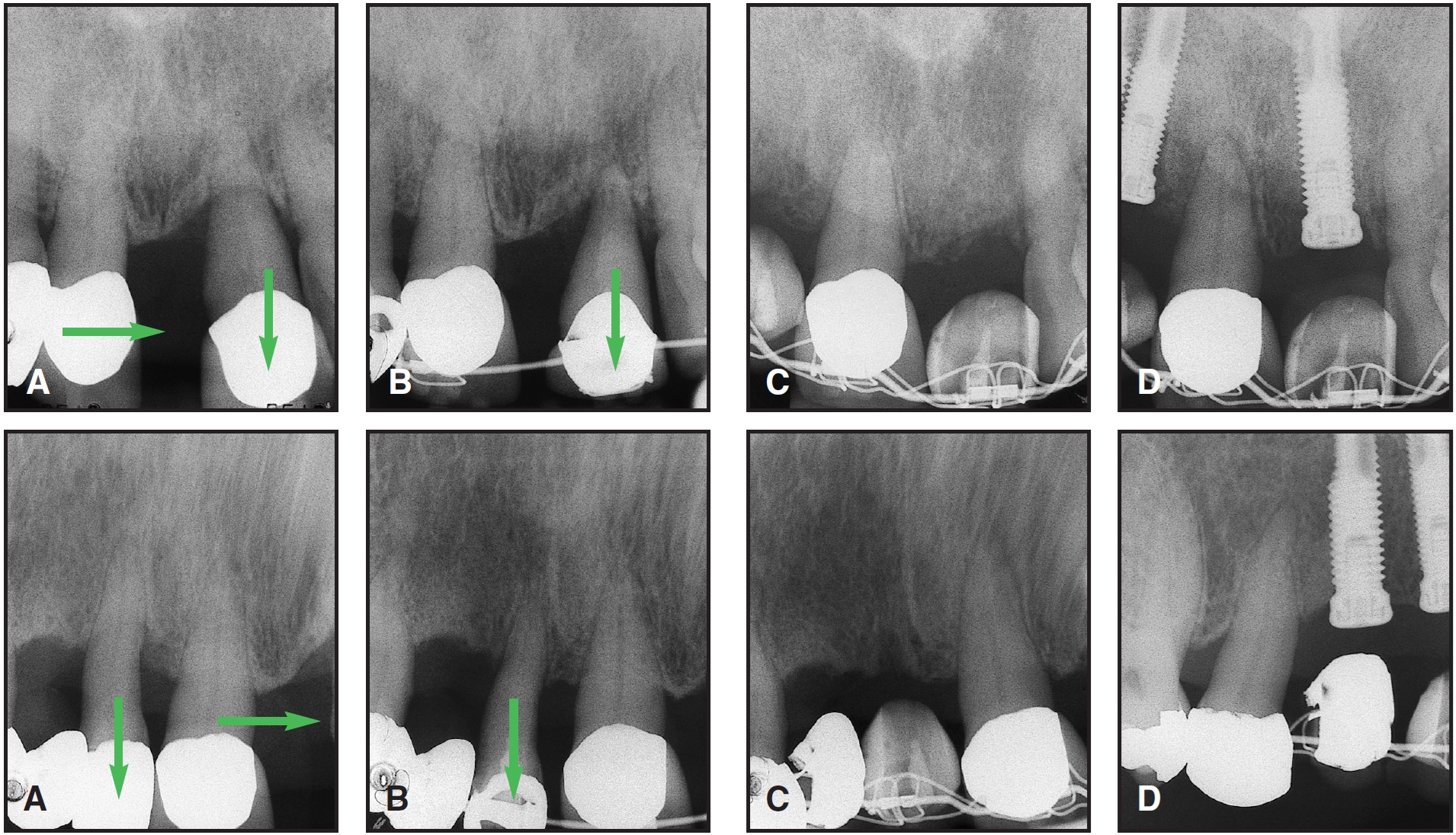
Fig. 22 Same patient as in Figure 21. Upper row: Right and left central incisors; lower row: right lateral and central incisors. A. Alveolar bone levels before treatment. B. After five months of extrusion. C. After 11 months of extrusion. D. Improved alveolar bone height for implants after 15 months of treatment.
DR. KEIM How long after bone development by tooth movement can implants be placed?
DR. ZACHRISSON Significant resorption and narrowing of the alveolar ridge after the orthodontic treatment could jeopardize placement of the implant. Fortunately, an edentulous ridge created by orthodontic extrusion or separation of teeth appears to be less prone to resorption over time compared to what occurs following conventional tooth extractions. For example, research has shown that after extractions, the ridge will narrow by approximately 30% over just the first three months.32 If bone grafting is performed after the extraction, the shrinkage may be reduced to 10% at six months. However, the amount of bone loss when the bone is regenerated by horizontal tooth movement is much less. This problem is illustrated by the events following distal movement of a maxillary canine to provide space for a lateral incisor implant. Using tomograms through the edentulous ridge at four-year recall appointments, and sectioning dental casts across the ridge, Spear and colleagues revealed that the amount of bone loss in a sample of 20 such patients was less than 1% over four years.33 This demonstrates that considerably less resorptive changes are likely to occur over time after orthodontic tooth movement compared to what occurs following tooth extractions.
DR. KEIM What techniques other than tooth movement are available to implantologists for bone and gingival development?
DR. ZACHRISSON Augmentation of the resorbed alveolar crest can be achieved with different surgical techniques, including onlay bone grafts, membrane techniques, bone distraction, and bone splitting.33,34 Maxillary sinus floor elevation and bone grafting may increase the height of bone in the maxillary posterior areas. Bone grafting and guided bone regeneration (GBR) can increase the width and, to some extent, the height of the alveolar bone. Lateral widening without vertical augmentation is possible with a crestal-split technique. All these methods for osseous reconstruction are technique-sensitive.
The gold standard at present is autogenous bone grafts taken from the maxillary tuberosity, the ramus, the symphysis, or the mandibular retromolar area. The most commonly recommended technique to build up soft-tissue thickness and height is to use connective tissue grafts from the palate, frequently in combination with coronally repositioned flap procedures.
It's interesting to note that a recent review of the current literature concerning augmentation of a narrow alveolar crest after dental and alveolar trauma, prior to implant placement, covered a multitude of methods to increase bone quantity and quality, including augmentation with bone grafts; augmentation with allogenic grafts; GBR; osteoinduction, osteopromotion, and osteoconduction; osteocondensation; distraction of low and narrow alveolar crests; and widening of alveolar crests with chisels.34 Orthodontic tooth movement was hardly mentioned as an alternative in this review, and was just briefly commented upon as an application of the principles of distraction. It is apparent that the use of orthodontic tooth movement for implant site development is little known among our colleagues in other areas of dentistry.
DR. KEIM Is there a difference in the prognosis for implants placed in sites developed by tooth movement vs. sites that did not need any development or sites that were developed by one of the other techniques?
DR. ZACHRISSON So far, publications in this area comprise case reports of only one or a few cases. We don't have any evidence-based scientific or clinical data to reliably answer your question. Reports of Spear and colleagues33 and Thilander and colleagues26 have shown successful long-term follow-ups when a premolar was moved orthodontically into an edentulous space, with an implant then placed in the position previously occupied by the premolar and provided with an implant-supported crown.
Zuccati and Bocchieri reported that after the extrusion of nine teeth with poor prognosis in seven patients, enhancement of the implant site and successful osseointegration were achieved in every case that had a healthy apical residual attachment.21 They also showed that orthodontic movement can be used to enhance the thickness of the bony ridge by combining the extrusion with labial root torque. However, no bone growth was detected around one tooth where repeated abscesses occurred during treatment. Our experiences are in agreement with these findings.
DR. KEIM Is the quality of bone different between implant sites developed by tooth movement and sites developed by other techniques?
DR. ZACHRISSON Although we now know that it is possible to regenerate bone by extrusion of teeth with healthy residual periodontia, provided the periodontal infection is controlled, and by horizontal bodily movement of premolars and canines, there are still many questions remaining to be answered with regard to an optimal implant osseointegration. In particular, we need more information on the quality and density of the regenerated bone. In implantology, there exists a close correlation between bone density and success of osseointegration. The poorest prognosis is seen in low-density trabecular bone. It is not unlikely that both prolonged orthodontic treatment time and prolonged healing time would enhance the maturation of orthodontically regenerated alveolar bone. Until more information is gained, the surgeon should treat orthodontically regenerated bone the same as bone obtained by guided bone regeneration or particulated autografts.
In comparison, it may be mentioned that in distraction osteogenesis, a fixation period of one year or more may be required before the structure of the newly formed bony tissue is comparable to that of the preexisting bone. However, even if the volume of the new and old bone is the same, it is conceivable that the mineral content, radiodensity, and tensile strength could be lower in the new bone.
Another possibility for faster and more complete osseointegration of single implants in orthodontically regenerated bone is to use more recent, bioactive implants rather than the traditional machined Brånemark implants. Research is needed in this area.
DR. KEIM What is the potential for tooth movement into the maxillary sinus to improve implant sites in this area?
DR. ZACHRISSON Teeth can be moved "with the bone" or "through the bone". To elicit a "with the bone" type of tooth movement, a direct resorption of bone in the direction of movement must take place, with a balance between resorption and apposition. If hyalinization occurs, indirect resorption results, and the tooth will move through the bone without any apposition. Especially in adult patients, the force level should be kept low to avoid formation of hyalinization areas and promote proliferation of periodontal cells; the clinician should apply the light force with a high moment-to-force ratio.28,35
Some recent case reports indicate that with properly controlled movement, a premolar can be moved through the maxillary sinus area while maintaining pulp vitality and bone support, and exhibit normal width of the periodontal ligament both on the pressure and tension sides.35,36 Implant placement in the previous alveolus is then possible. The relatively complicated sinus-lift surgical augmentation procedure that would otherwise be necessary can thus be avoided. However, the real spatial relationship between the root of the displaced premolar, the subperiosteal layer, and the sinus recesses is not known, since it would require a histologic evaluation.
Figure 23 shows a case with apparently successful premolar movement into the sinus, in which I used a non-osseointegrated miniscrew (Spider Screw**) as the source for posterior anchorage. In other instances, however, my attempts to move a premolar into the maxillary sinus region have failed, with the tooth apparently hitting against the sinus wall for a long time, while developing lateral root resorptions.
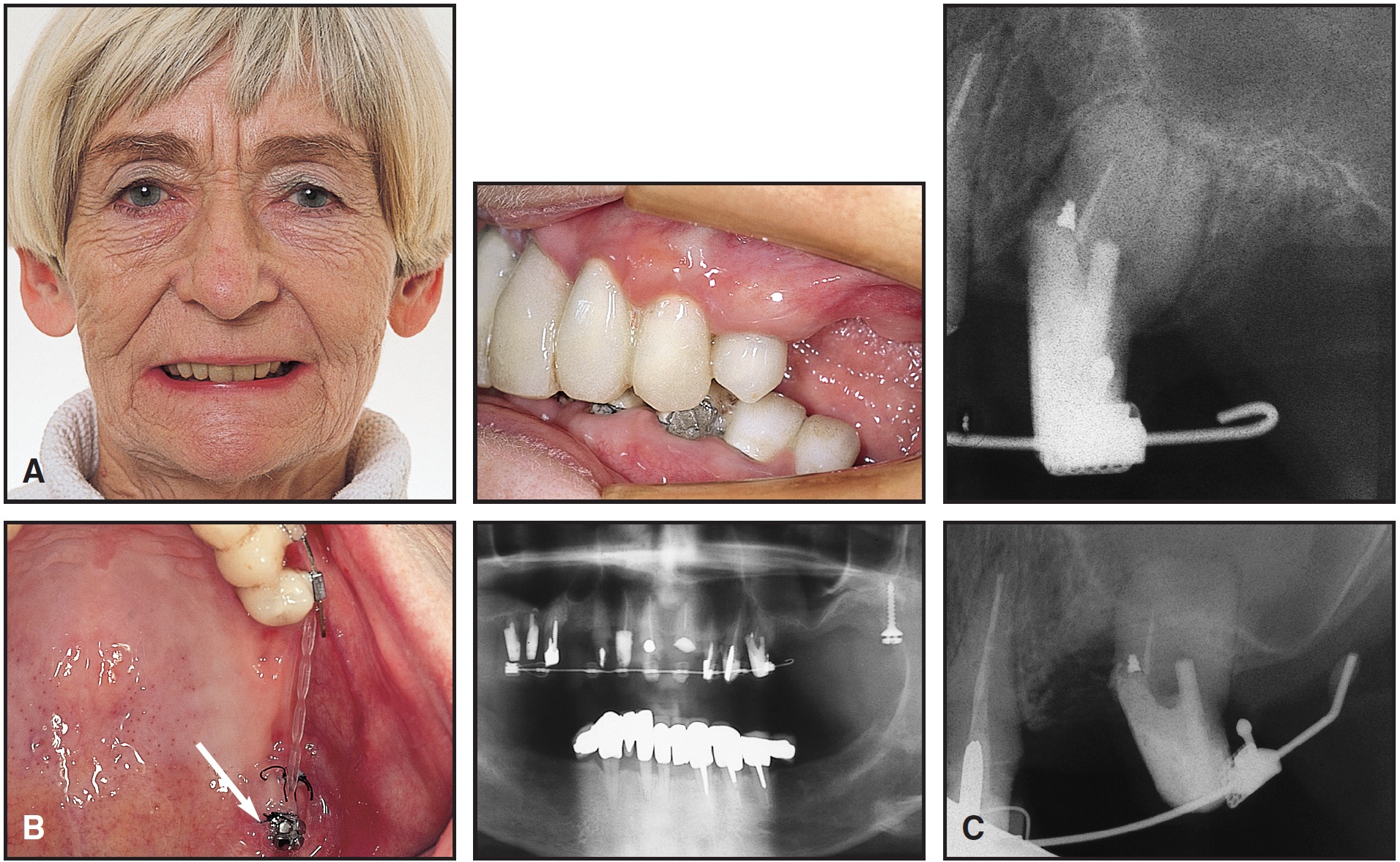
Fig. 23 A. Low extension of sinus on left side made implant placement impossible without sinus-lift surgery in 66-year-old female patient whose crowns were all artificial. B. Non-osseointegrated Spider Screw inserted in tuberosity (arrow) and immediately loaded with light force for distal movement of left second premolar through maxillary sinus. C. After 12 months, space and alveolar bone were created for implant by 8mm distal movement of second premolar. Both premolar and bone were apparently moved into sinus, with immature bone (darker areas) forming on tension side.
DR. KEIM Are there any other techniques particularly applicable to older patients that might be of interest to our readers?
DR. ZACHRISSON Of the techniques that I use routinely, the custom-made transpalatal arch (TPA), having one large anterior loop and two smaller posterior loops (Fig. 24), should be useful for other orthodontists in many adult and older patients.37,38 The main differences between my design and the traditional Goshgarian-type TPA are in the amount and shape of the wire in the palatal loop. Increasing the length of the wire increases its springiness and range, reduces the load-deflection rate, and makes the forces more constant and precise.38 Thus, lower and more constant moments of derotation are produced, and the engagement into the lingual attachments is easier, with less activation loss. It takes less time to derotate molars with our design than with traditional Goshgarian arches.38
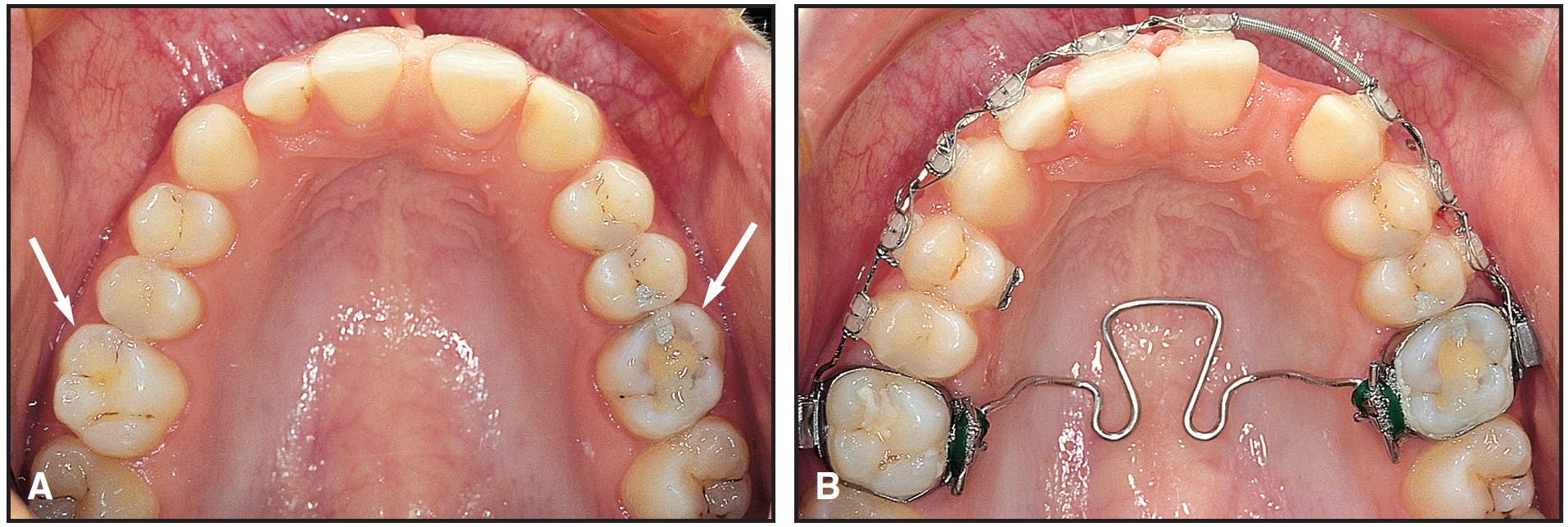
Fig. 24 A. Patient with mesially rotated upper first molars in Class II malocclusion (arrows). B. Zachrisson transpalatal arch offers clinical advantages over conventional Goshgarian design, allowing simple and accurate molar derotation.
The improved design has several clinically relevant advantages. It appears to be an optimal appliance for supporting posterior anchorage, improving vertical control, maintaining arch widths and archforms during treatment, quickly and completely derotating mesiolingually rotated maxillary first and second molars, adding buccal root torque to the molars, expanding the maxillary arch, and correcting mesiodistal asymmetries. When soldered extension spurs are added, the TPA can act as an ideal tool for tooth movements that are difficult, if not impossible, to achieve with conventional labial archwires, including torque control, palatal intrusion, and lingual movement of maxillary second molars.38
DR. KEIM What has been your experience with micro- or miniscrews?
DR. ZACHRISSON I believe that the recently developed miniscrews, or so-called temporary anchorage devices (TADs), in coming years will become a more significant aid than at present to support posterior and/or anterior anchorage in both the maxilla and the mandible for many older patients, who may have incomplete or diseased dentitions. My experience with different TADs designed for pull forces via superelastic coil springs or elastomers and, particularly, those with bracket-like heads that allow ligation of orthodontic wires (Spider Screw, Aarhus Anchorage System,*** TOMAS†, etc.) is positive, and the indications for using such devices are basically limited only by one's imagination. By the same token, the new, temporarily osseointegrated midpalatal or paramedian palatal implants may be increasingly used in the future to support or replace toothborne anchorage.39
DR. KEIM What do you see as the main areas of research in orthodontics for the older patient that will be addressed in the next decade?
DR. ZACHRISSON There are several interesting areas where future research can provide helpful clinical advice to further improve our orthodontic treatment results.
It would be interesting to know more about applications, indications, esthetics, and possible harmful side effects to the teeth and periodontium following extensive stripping in older adults with various malocclusions, and to compare these results with those following incisor or premolar extractions, to better know where the limits are for each of these procedures.
Another area of clinical significance requiring more extensive research is on orthodontic implant site development and methods for improved osseointegration following vertical and horizontal tooth movements. As I discussed earlier, there are several important questions that need to be answered in the coming years. Furthermore, we have already begun some clinical and histologic studies of what happens when teeth may unintentionally come into intimate contact with temporarily inserted miniscrews during orthodontic treatment. The incidence of possible complications and clinically significant damage from such screw-tooth contacts represents an interesting research area that could result in useful clinical advice.
It would also be of interest to learn more about the esthetic and functional outcome following different interdisciplinary approaches to complicated clinical problems in older patients, as it would be with all adult orthodontic patients. For example, it would be prudent to further evaluate the long-term esthetic, occlusal, and periodontal outcome of implant-supported crowns in the esthetic zone,40 and to compare the results following orthodontic space closure, and with different designs of two-unit composite or porcelain cantilever bridges.
DR. KEIM Dr. Zachrisson, on behalf of our readers, I'd like to thank you for sharing your knowledge about this increasingly important area of orthodontics.
FOOTNOTES
- **Registered trademark of HDC, Via dell'Industria, 19, 36030 Sarcedo, Italy; www.hdc-italy.com.
- ***Medicon eG, Gänsäcker 15, D-78532 Tuttlingen, Germany; www.medicon.de.
- †Dentaurum, Turnstrasse 31, D-75228 Ispringen, Germany; www.dentaurum.com.
REFERENCES
- 21. Zuccati, G. and Bocchieri, A.: Implant site development by orthodontic extrusion of teeth with poor prognosis, J. Clin. Orthod. 37:307-311, 2003.
- 22. Salama, H. and Salama, M.: The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects, Int. J. Period. Restor. Dent. 13:312-333, 1993.
- 23. Berglundh, T.; Marinello, C.P.; Lindhe, J.; Thilander, B.; and Liljenberg, B.: Periodontal tissue reactions to orthodontic extrusion, J. Clin. Periodontol. 18:330-336, 1991.
- 24. Kajiyama, K.; Murakami, T.; and Yokota, S.: Gingival reactions after experimentally induced extrusion of the upper incisors in monkeys, Am. J. Orthod. 104:36-47, 1993.
- 25. Lindskog-Stokland, B.; Wennström, J.L.; Nyman, S.; Thilander, B.: Orthodontic tooth movement into edentulous areas with reduced bone height: An experimental study in the dog, Eur. J. Orthod. 15:89-96, 1993.
- 26. Thilander, B.; Odman, J.; and Lekholm, U.: Orthodontic aspects of the use of oral implants in adolescents: A 10-year follow-up study, Eur. J. Orthod. 23:715-731, 2001.
- 27. Hom, B.M. and Turley, P.K.: The effects of space closure of the mandibular first molar area in adults, Am. J. Orthod. 85:457-469, 1984.
- 28. Fontenelle, A.: Lingual orthodontics in adults, in Current Controversies in Orthodontics, ed. B. Melsen, Quintessence, Chicago, 1991, pp. 219-268.
- 29. Diedrich, P.R.; Fuhrmann, R.A.W.; Wehrbein, H.; and Erpenstein, H.: Distal movement of premolars to provide posterior abutments for missing molars, Am. J. Orthod. 109:355-360, 1996.
- 30. Basdra, E.K.; Mayer, T.; and Komposch, G.: Guided tissue regeneration precedes tooth movement and crossbite correction, Angle Orthod. 65:307-310, 1995.
- 31. Wilcko, W.M.; Ferguson, D.J.; Bouquot, J.E.; and Wilcko, M.T.: Rapid orthodontic decrowding with alveolar augmentation: Case report, World J. Orthod. 4:197-205, 2003.
- 32. Carlsson, G.: Changes in contour of the maxillary alveolar process under immediate dentures, Acta Odont. Scand. 25:1-31, 1967.
- 33. Spear, F.M.; Mathews, D.M.; and Kokich, V.G.: Interdisciplinary management of single-tooth implants, Semin. Orthod. 3:45-72, 1997.
- 34. Oikarinen, K.S.; Sandor, G.K.B.; Kainulainen, V.T.; and Salonen-Kemppi, M.: Augmentation of the narrow traumatized anterior alveolar ridge to facilitate dental implant placement, Dent. Traumatol. 19:19-29, 2003.
- 35. Melsen, B.: Limitations in adult orthodontics, in Current Controversies in Orthodontics, ed. B. Melsen, Quintessence, Chicago, 1991, pp. 147-180.
- 36. Re, S.; Cardaropoli, D.; Corrente, G.; and Abundo, R.: Bodily tooth movement through the maxillary sinus with implant anchorage for single tooth replacement, Clin. Orthod. Res. 4:177-181, 2001.
- 37. Gündüz, E.; Zachrisson, B.U.; Hönigl, K.D.; Crismani, A.G.; and Bantleon, H.P.: An improved transpalatal bar design: Part I. Comparison of moments and forces delivered by two bar designs for symmetrical molar derotation, Angle Orthod. 73:239-243, 2003.
- 38. Zachrisson, B.U.: Clinical use of custom-made transpalatal arches—Why and how, World J. Orthod. 5:260-267, 2004.
- 39. Bantleon, H.P.; Bernhart, T.; Crismani, A.G.; and Zachrisson, B.U.: Stable orthodontic anchorage with palatal osseointegrated implants, World J. Orthod. 3:109-116, 2002.
- 40. Bernard, J.P.; Schatz, J.P.; Christou, P.; Belser, U.; and Kiliaridis, S.: Long-term vertical changes of the anterior maxillary teeth adjacent to single implants in young and mature adults: A retrospective study, J. Clin. Periodontol. 31:1024-1028, 2004.
- 41. Zachrisson, B.U.: Orthodontic tooth movement to relocate gingival margins and regenerate alveolar bone for single-tooth implants, in Growth and Treatment: A Meeting of the Minds, Vol. 41, Craniofacial Growth Series, ed. J.A. McNamara, Jr., University of Michigan Press, Ann Arbor, MI, 2004, pp. 73-88.



