JCO INTERVIEWS
Dr. Birte Melsen on Adult Orthodontics
DR. BURSTONE Dr. Melsen, we are delighted to have you here for this interview. We know that you have done a great deal of work in the treatment of adult cases. Are there special problems that we must consider in treating an adult?
DR. MELSEN Yes. Appliances that one can use successfully in young children will not always work in the adult.
DR. BURSTONE Could you be more specific about some of the problems?
DR. MELSEN My interest in adult orthodontics really came from the fact that I was working with bone biology. It was interesting to try to use the mechanical stimulus from orthodontic appliances and watch the bone reaction in the adult patient. It is clear that you don't have the same possibilities in the adult that you do in the young individual, since you don't have any vertical development of the alveolar process. Vertical control is, therefore, a very important issue. Also, you have to adapt the force system and the magnitude of force to the adult situation.
DR. BURSTONE Perhaps we should define "adults".
DR. MELSEN When I talk about adults, I am talking about non-growing individuals, including elderly adults with degenerating dentitions.
DR. BURSTONE Are there special considerations for the elderly adult?
DR. MELSEN Among the elderly adults, the marginal bone level must be taken into consideration. Therefore, you have to lower the magnitude of force and monitor the moment-to-force ratio for certain tooth movements.
DR. BURSTONE In what way would you change the amount of force?
DR. MELSEN I think orthodontists use force levels that are rather high in relation to what we actually need.
DR. BURSTONE For all types of cases?
DR. MELSEN Yes. In the adult you don't have the same pool of cells available when you start your treatment as you have in the young individual. Therefore, the initial force should be lower. Also, the amount of bone that must resorb in relation to a particular tooth movement is generally less in the adult.
DR. BURSTONE Are you suggesting starting with lower forces and increasing them later on?
DR. MELSEN Yes, but you must think more about the stress distribution--force per unit of bone--instead of just thinking about force per tooth.
DR. BURSTONE Is there some practical way you could make an estimate of what forces are needed?
DR. MELSEN On adult patients, we always take periapical radiographs and estimate the center of resistance of the tooth, which is usually around one-third or 40% from the marginal bone level in the apical direction. In cases with a considerable amount of marginal bone loss, that might change the center of resistance and require a different moment-to-force ratio.
DR. BURSTONE By how much do you generally reduce the magnitude of force?
DR. MELSEN In the adult patient, we cut the force down to about 50% of what has normally been recommended in young individuals, and the force level is generally dictated by the vertical force, because we have set our standards for the intrusive force component. If you know the direction of your force, then the other forces can be calculated.
DR. BURSTONE You have already said that there are different moment-to-force ratios in working with adult patients based on the amount of alveolar process present. Would you develop that idea?
DR. MELSEN In the young individual, you can move teeth through bone. In the older individual, you would usually like to move the tooth with its bone. Sometimes you move it into an area where the alveolar process is not so well developed and where no natural bone development is going on. Therefore, you have to move with direct resorption, which is followed by a corresponding apposition. When you do that, you move teeth with bone and you must avoid forces leading to hyalinization. Hyalinization occurs in areas of high stress in the periodontal ligament, for example if you perform uncontrolled tipping even with light forces. Sometimes you have to move teeth through the sinus, and you want to move the tooth with its cortical bone. This requires stress distribution leading to direct resorption and a corresponding apposition, so that the bone follows the tooth.
DR. BURSTONE This also relates to why it is important to control the magnitude of force.
DR. MELSEN Certainly.
DR. BURSTONE What are some special considerations for bodily tooth movement on adults?
DR. MELSEN First of all, you have to change the moment-to-force ratio, especially in older adults with bone loss and a dentition in a degenerating state in which you cannot allow any iatrogenic damage. You have to plan for as small a tooth movement as possible, and to avoid round-tripping. You cannot start with an uncontrolled system and then do root movement following that. You have to try to reach your treatment goal in the shortest possible way, with a minimum of tooth movement.
DR. BURSTONE Many situations require translation of teeth. Since most adults have alveolar bone loss, would you say that for the same forces you are going to need more moment?
DR. MELSEN Lower forces are needed, and relatively more moment. It is important to have full control over the tooth movement. You cannot move teeth along a wire in a frictional system. You will have to be in a non-frictional system, and this leads us to the approach we have taken for this movement.
DR. BURSTONE What are the periodontal considerations?
DR. MELSEN The periodontist can assure you that you have a healthy condition before you start intrusion. The routine in our clinic is that if motivation and scaling do not bring the pockets down to a level of 3-4mm, then the patient has to go through periodontal surgery with open curettage and a flap operation during which the pocket is reduced. Very quickly following surgery--maybe after two to three days--we will start the intrusion, and the patient is then seen on a routine basis by the periodontist throughout the treatment period, which means every six weeks to two months. Depending on the situation, the periodontist will then do scaling or even curettage, trying to remove some of the pocket epithelium if a pocket should develop during the treatment.
DR. BURSTONE If you do not do curettage, is it still possible to have an increased attachment?
DR. MELSEN I think you get an increased attachment following the surgery and the initial orthodontic treatment, but curettage has something to do with the continuous movement of the attachment in a coronal direction.
DR. BURSTONE There has been a lot of debate about whether intrusion will actually produce an improved attachment. What has been your clinical experience, and what has your research shown?
DR. MELSEN Our first clinical trials were carried out more than 10 years ago, and we found that these patients got shorter clinical crowns. The periodontist couldn't measure any pockets, so our conclusion was that probably they had what was called a long epithelial attachment. On this basis, we set up a monkey study, where we produced pockets and started to intrude teeth following surgery. We had marked the roots at the level of the attachment at the time of surgery and, much to our surprise, we found that we had gained attachment three months following intrusion and a continuous hygiene regime. There was a variable but very consistent gain in the attachment--from .5 to almost 3 millimeters.
DR. BURSTONE How do you mechanically produce the intrusion?
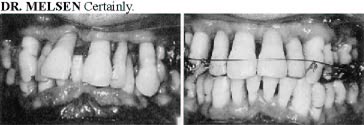
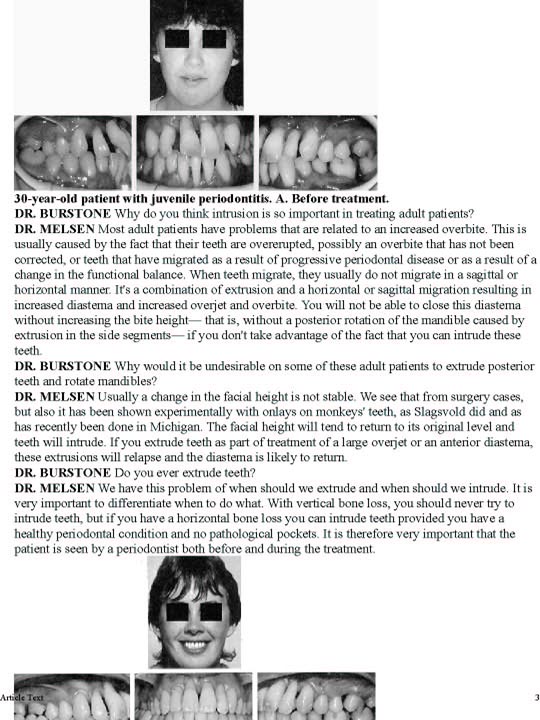
DR. MELSEN We have tried several types of appliances, and we have found that if you want to intrude teeth you should use very light continuous forces (Fig. 1). Even with the newer low stiffness, superelastic wires, the forces are not low enough and the load deflection rate istoo high in a continuous arch due to the small interbracket distances.
DR. BURSTONE Therefore, the other teeth would erupt?
DR. MELSEN Definitely. We use a base arch and consequently a long interbracket distance, and we can apply a low force which has a very low load-deflection rate. The appliance is thereby also very forgiving. It is not so important whether you activate it one millimeter more or less.
DR. BURSTONE On adult patients with periodontal problems, is the point of force application important?
DR. MELSEN Definitely. We try to intrude the teeth as much as possible with translation (Figs. 2, 3. That was another result that came out of the animal experiments. In previous studies on intrusion, orthodontists had tried to intrude by tipping part of the tooth into bone. If you do that, you produce a compression of the periodontal ligament and you get resorption. We tried to make a true translation in an apical direction.
DR. BURSTONE By translation, you mean along the long axis of the tooth?
DR. MELSEN Along the long axis, so that you are stretching the periodontal ligament. When you stretch the fibers of the periodontal ligament, you have formation along the bone surface instead of resorption. On the animal experiments, we have also seen a large increase in the mitotic activity of bone formation cells.
DR. BURSTONE How do you handle the anchorage of the posterior teeth while you are doing intrusion?
DR. MELSEN Since the vertical forces are very low--about 5-10 grams per tooth--the vertical problem is not very big because occusal forces can always overcome forces at that level. The big problem is the moment delivered by the base arch. One way of controlling the moment is to use the occlusal forces. We do that in different ways. Either we can build up occlusion in composite if the occlusion is not very tight to start with, or we add a splint that is adjusted for occlusal contact to all teeth. Then the patient will be able to tell you if you get the primary contact in the premolar region due to the big moment delivered by the base arch. You can also use articulating paper to determine that.
DR. BURSTONE So you ask the patient with or without a splint to tell you if they feel any changes in occlusion?
DR. MELSEN Yes, and they can tell you that long before you can ever see that you are about to lose anchorage.
DR. BURSTONE Are some of your adult patients extraction cases?
DR. MELSEN Yes, but again we have a difference between orthodontically young individuals and elderly adults. Extraction is often dictated by the status of the dentition with regard to the periodontium and decay. If you need to extract, you would choose the tooth with the worst prognosis.
DR. BURSTONE And how do you control anchorage in extraction cases? Do you use much headgear?
DR. MELSEN We never use headgear. The reason for not using headgear is that the interference of headgear with the force systems that we are using is so large that we find it unacceptable. We are trying to monitor our forces very closely, and if you have forces in the range of 10-30 grams then interaction from the headgear will change the force system considerably. If you have a headgear where the line of action is above the center of resistance of the reactive unit, you may intrude teeth more; and if it is below the center of resistance, you may extrude incisors. So we do not feel that we can allow that.
DR. BURSTONE If you have an arch where you must hold the anchorage, how do you do that?
DR. MELSEN We use the maximum number of teeth as anchorage and, on top of that, the force applied to the reactive unit will be monitored as closely as possible to that of the deliverance of the translation. Translation does not create primary contact as much as the moment does.
DR. BURSTONE Do you try to increase the tipback of molars?
DR. MELSEN Not really, because if you do that you produce a large moment and run into a problem of developing eruption in the premolar region. We try and keep the moment-to-force ratio close to that of the translation, between 7 and 10.
DR. BURSTONE You want to make sure that if posterior teeth move at all, they will translate?
DR. MELSEN If they would move they would translate, and we routinely use transpalatal arches. Usually in the adult we use two transpalatal arches crossing each other and welded in the middle, which makes a posterior unit that is very large and very rigid. If the patient has bridges, these bridges are also included in the anchorage.
DR. BURSTONE Some orthodontists have suggested using headgear directly to the incisors for intrusion. Is this a viable option?
DR. MELSEN I think not, because you cannot use a headgear with forces as light as we have found necessary. Dellinger showed several years ago that you don't get intrusion if you use forces at the level of 50 or 100 grams per tooth. We tried to use J-hook headgear on younger patients, but I didn't like the periapical findings. There was some root resorption that was much more pronounced than what we see with a base arch.
DR. BURSTONE Could you elaborate on your idea of a posterior anchorage unit?
DR. MELSEN There are different ways. If you limit yourself to conventional orthodontics, you are limited by the size of the bracket. With an .018" slot you are especially badly off, because the largest-dimension wire you can use is an .018" x .025". An 022" slot is a bit better, but we don't find that satisfactory in adult patients, so we would use fracture splints from TP on which we can weld a tube directly. Or you can use the very heavy .036" wire embedded in a splint, and then combine two mini-splints--one in each molar region--with a double transpalatal arch. You actually produce one big posterior tooth, which is in maximum occlusion.
DR. BURSTONE So you think it is very important that the anchorage unit be very rigid.
DR. MELSEN That is the only way you can control what is happening to your active unit.
DR. BURSTONE You are then really not trying to do any tooth movement in the posterior segment, particularly on an intrusion case?
DR. MELSEN If you make a change in occlusion--say, change a distal occlusion to a mesial occlusion--loss of vertical control is possible. In young individuals, this is overcome by growth.
DR. BURSTONE If you have a patient who requires some movement of the posterior teeth, would you do that later as a separate step?
DR. MELSEN In the posterior region, the elderly patient usually has need for movement of teeth in order to set up reconstruction or to close earlier extraction spaces. That doesn't mean changing the occlusion. That means moving one or two individual teeth. When you want to change the occlusion, I think you are into orthognathic surgery.
DR. BURSTONE Many orthodontists will say that it is more difficult to treat adult patients. Would you say that's true?
DR. MELSEN Yes and no. Orthodontic treatment of the adult is not so forgiving. When you look at treatment of young patients, sometimes you wonder why the treatment result was so good when you look at the force systems being used. In the adult, you get the result from what you applied, and if you get a bad result it was because your force system was wrong.
DR. BURSTONE What problems do we have in treating an adult patient that we would not have in a growing patient?
DR. MELSEN The force level has to be kept low. The moment-to-force ratio has to be adapted to the marginal bone level. Vertical control has to be maintained, and that has to do with the anchorage that has also been mentioned. But apart from that, the tooth movement runs according to the mechanical stimulus you give the tooth.
DR. BURSTONE Do you think adults can handle major tooth movement, or do they need special consideration or compromise?
DR. MELSEN They can have major orthodontic treatment. You can read in the literature that orthodontic treatment of adults is limited to smaller tooth movements, but it is not true. We have seen tooth movements of 15-18 millimeters without any loss of bone or any iatrogenic damage. But it's important that in the adult the tooth movement is not through bone but with bone, which means that it must not be done by uncontrolled tipping with a very high stress distribution, but as much as possible by translation where you move a tooth along with direct resorption and corresponding apposition.
DR. BURSTONE Therefore, your force system must be more precise for the adult.
DR. MELSEN Yes, and along with the tooth movement you build up the alveolar process if it has been lost. In many cases, if the molars have been lost, we move second bicuspids distally and actually build up the alveolar process and create a situation where a patient can have bridgework instead of a denture.
DR. BURSTONE How would you correct a Class II occlusion in an adult?
DR. MELSEN I would look at the skeletal pattern and, if I don't think I could get an acceptable result by dentoalveolar remodeling, then I would go into surgery. If I saw I could get an acceptable profile by moving the maxillary teeth back, then I would probably do a two-premolar extraction. I would not try to correct a distal molar relationship unless I had severe crowding in the lower jaw,and then do a differential space closure. This would be something you could do in a younger adult, but I wouldn't go into this kind of treatment in an older adult.
DR. BURSTONE In treatment planning for the adult, what procedures do you use? Are the records different?
DR. MELSEN Parts of the records are the same as for the young patient. You also have to have very good periapical radiographs and some information from the periodontist on the periodontal status and resistance of the patient. You have to be fully aware of where you want your mandibular position. In 30% of our cases, the patient will come in with severe temporomandibular joint disturbances. In these cases you must establish the position of the mandible before you go any further. That's done by means of a splint, sometimes by us and sometimes by a gnathologist.
It is important that we know the reference position to which we have to treat our patients, and that we establish that position before we start any tooth movement. In the patients with symptoms, we have them on a splint until we have found the position where they don't have any symptoms. In this position, we will then make a deep indentation in the splint so that the patient can recognize this position, and the splint will be cemented. These splints are usually very thin and even perforated in certain areas. In patients who do not have any symptoms, if we have missing teeth or a deteriorating dentition, the splint may be part of the anchorage.
DR. BURSTONE With patients who have TMJ problems, do you make your splints on an articulator?
DR. MELSEN They are frequently produced on an articulator, but even after a precise mounting we have to do some adaptation in the mouth.
DR. BURSTONE What is your concept of centric occlusion on adult patients? Do you want that to be identical with centric relation? or a muscular position?
DR. MELSEN I think terminology is a big problem in relation to TMJ. In Denmark we talk about the structural position, which is the position where the patient has no symptoms, where there is harmony between the musculature and the joint and the occlusion. This is the position we try to achieve in these patients.
DR. BURSTONE So, if the patient is comfortable with the splint, that's the position you would use.
DR. MELSEN Yes. One of the reasons for cementing the splint is that we want the splint to be very thin, because the patients are uncomfortable with splints that are thick.
DR. BURSTONE If you have a patient without any symptoms, is the splint sometimes your anchorage unit?
DR. MELSEN The splint will then be the anchorage unit, because you may be moving teeth in the upper jaw and maybe you have some missing teeth in the upper jaw, maybe some missing teeth in the lower jaw, and some teeth out of occlusion. By using a splint, you bring all teeth available into the unit that is used in the occlusion. The splint can help you do that.
DR. BURSTONE Are there some limits to adult treatment?
DR. MELSEN Biologically there is no limit to how far you can move a tooth, but the limit comes in the number of teeth that are available for anchorage and the force system that is generated. If you want to move two teeth toward each other, you can do it; but if you want to move both teeth in the same direction, it is of course not possible.
DR. BURSTONE In America, there is much interest in esthetic orthodontics. Is this important for you?
DR. MELSEN My patients come because they want to maintain their teeth and because they want to get the most esthetically satisfactory result that can be obtained with the teeth available. But during treatment some of these patients ask why we are using awkward appliances that cannot be made invisible. Then you have to choose whether you want to limit yourself to what you can do with lingual orthodontics or with a continuous arch on plastic or ceramic brackets.
DR. BURSTONE You think your treatment goal and your mechanics to do it are most important and esthetics is secondary?
DR. MELSEN The force system comes first. Then you can consider whether you can provide the patient with this force system in away that is also esthetically satisfactory.
DR. BURSTONE I have seen many of your cases that were very difficult to treat, but are there many adults who just come in for esthetic considerations?
DR. MELSEN I don't see so many of those, because they get treated by my colleagues in private practice. The larger mutilations come to the dental school and from my periodontist.
DR. BURSTONE Before you actually make your appliances, do you plan out the force system on each patient?
DR. MELSEN Oh, yes. The treatment planning itself is a very important part of total treatment, and it has to be accepted by the patient. There might be several alternatives, and the patient can choose the one he or she wants. It is also dependent on how much reconstruction work will have to be done after treatment, and how the retention phase is going to be handled. Very often retention is lifelong. Then we start planning the treatment, and we do what we call free-body diagrams of the forces needed and the desired tooth movements. Then we select the best biomechanics for the patient.
DR. BURSTONE I assume you do the planning not only to reach your goals, but to minimize side effects during treatment.
DR. MELSEN In the adult you want to minimize side effects. You also want to do that in the young, but in the young side effects are often taken care of by growth. That's not the case in the adult. You must be more careful in the adult. Also, by minimizing side effects you reduce the treatment time. Our treatment times have been reduced in younger patients based on our experiences with adults. Most of our treatments are finished within 12-15 months.
DR. BURSTONE Is it necessary to compromise treatment in some adult patients?
DR. MELSEN Very often. Most treatment goals are compromises. You do not always have 28 perfect teeth available, and you also have skeletal patterns that you have to accept if you do not want to go into surgery.
DR. BURSTONE In the adult patient, how do you handle retention?
DR. MELSEN If you have marginal bone loss, even if you reach perfect intercuspation and good incisal relationships, you cannot anticipate this to be stable by itself. You will have to do some permanent retention, such as splinting from canine to canine. This can be done either by a twisted wire or by any type of bonded appliance. On top of that I recommend that my patients use what we call a "tooth pajama". It is really nothing but a fully balanced splint. They can use it to control tooth position. They don't have to use it every night. They can use it when they are in stress situations. We want to avoid parafunctions, which often occur at night. You don't usually overload your teeth during the day, but you may do so at night.
DR. BURSTONE I know that you have been quite interested in early treatment using functional appliances and headgear. Are there some situations that you feel should be handled early?
DR. MELSEN I was a student of Harvold's and I became interested in functional appliances as a student. Later, when I was visiting in San Francisco, I observed treatment of hemifacial microsomia. We tried to apply Harvold's principles in the treatment of these cases, and we had somesurprises. In many cases if you start early enough--and these cases are started at the age of 3 or 4--you can even avoid surgery in the treatment of hemifacial microsomia.
DR. BURSTONE Will these patients have surgery later?
DR. MELSEN Some of them will, but some of them can avoid it. It depends on the mobility on the affected side. We have used the same principles in the treatment of children suffering from rheumatoid arthritis affecting the temporomandibular joint. In these cases you can actually produce apposition in the condylar area--not only on the condyle, but also of the cranial base.
DR. BURSTONE It has been suggested for patients with mandibular asymmetries who require surgery that some type of functional appliance would be useful before the surgery.
DR. MELSEN It is used before surgery for several reasons. It is used to avoid secondary asymmetry of the maxilla through the growth period before the surgery. But it is also used to stimulate or change the neuromuscular pattern in the direction of the surgical procedure.
DR. BURSTONE Do you use many functional appliances in Denmark for mixed dentition treatment?
DR. MELSEN We started to use a lot of functional appliances, and then we had a headgear period. I think we are now going back more and more to functional appliances, but also to the combination of functional appliances and extraoral anchorage.
DR. BURSTONE What are some of the advantages to using a functional appliance over headgear?
DR. MELSEN With a headgear, you only apply your forces to the maxilla, and very few of the cases are maxillary prognathic. They are more mandibular retrognathism. I find you get a more harmonious face with a functional appliance.
DR. BURSTONE Do you think you can alter mandibular growth with a functional appliance?
DR. MELSEN I think you get a temporary alteration with an improvement in occlusion, and the skeletal pattern will probably return to what it was.
DR. BURSTONE So you are not sure that you are going to get long-term skeletal changes, but just some changes that help you while you are correcting the malocclusion?
DR. MELSEN I am pretty sure that we don't get long-term skeletal changes, but that we get short-term skeletal changes and then you will return to the original pattern. If you look at a crossbite that hasn't been treated and look at that patient at the age of 18 years, one half of the mandible is longer than the other. So you could probably produce long-term results if the appliance were used for a major period of development, but that is not the case with orthodontic treatment.
DR. BURSTONE You mentioned the use of headgear with functional appliances. Is that to control the vertical dimension?
DR. MELSEN Yes. We use a high-pull headgear with a bite plate in the side segment. We have been inspired by Teuscher's work, and it is in his direction that we are working.
DR. BURSTONE I know that you have been a close associate of Bjork. Are there new developments coming out of implant research, and what are the implications for orthodontic treatment?
DR. MELSEN Bjork is retired now, but he has been an inspiration to all of us. My first research in growth and development on a histological basis was influenced by Professor Bjork. In Copenhagen, they are now more interested in head posture and the effect of respiration. However, they are still working on some of his implant material.
DR. BURSTONE We hear a great deal about growth prediction. How good are we these days in predicting growth on our patients?
DR. MELSEN I don't think you can predict growth. I think you can come pretty close on a group of patients, but not on the individual by just using the average. That was very clearly shown by Baumrind in a paper in AJO last year.
DR. BURSTONE Do you try to do a growth prediction on a new patient?
DR. MELSEN We are very pessimistic. We always predict the worst possible growth and plan our treatment accordingly. That way we get nice surprises when the patient grows better than we anticipated.
DR. BURSTONE Americans are very interested in orthodontic programs in Europe. You've had an opportunity to visit many programs in the United States. Do you think there are differences compared to programs such as you have in your school?
DR. MELSEN I think our program and the programs in Scandinavia are very close to programs in the United States. Programs in other parts of Europe are still developing, especially since the specialty has only been in existence a few years in these countries. Our program is now accepting students from other Common Market countries. We have 12 students, six of whom are from other European countries.
DR. BURSTONE How long is this program?
DR. MELSEN The program is three years long and leads to a master's degree.
DR. BURSTONE Are there any other differences compared to programs in America?
DR. MELSEN You don't get a specialty certificate until you have passed a Board examination, which you can take at the earliest two years following your education, including a minimum of 10 completed cases.
DR. BURSTONE Do you see major changes in the way Europeans treat orthodontic cases in the last 15 years?
DR. MELSEN Yes, there was a big change from a lot of removable appliances to fixed appliances, and fixed appliances were thought to be the solution to all problems. The tendency now is more varied. Most people work with both types of appliances. Straight wire was also thought to be the solution for many problems, but there is an increasing interest in more differentiated biomechanics. People are not just satisfied in seeing teeth move. They want to know where they move.
DR. BURSTONE Sometimes over here we get the idea that patients in Europe, particularly Northern Europe, are easier to treat--not so many vertical problems, more flat mandibular planes, more horizontal growth. Is there any truth to that?
DR. MELSEN They certainly have more brachycephalic children in Italy and fewer long faces, but they may have a higher frequency of Class III malocclusions. In Scandinavia, we have much like what you have over here--a fair amount of long faces.
DR. BURSTONE Do you think it is more important to have a working relationship with other specialties in dentistry today?
DR. MELSEN I think what is happening in dentistry is a tendency we also see in medicine. Wehave to improve our interdisciplinary work in order to provide the patient with a better service. Things are getting so specialized that no one person can handle a patient's problems. Especially in relation to adult orthodontics, we can certainly not be without periodontists and gnathologists and the people who do reconstruction following treatment. Our colleagues are important in order to carry out our work and also to maintain the results of our treatment.
DR. BURSTONE Does basic research help us understand the responses of bone in adult orthodontics?
DR. MELSEN I am involved in a major project on osteoporosis, and my husband is a pathologist with a special interest in bone. We have been working together in many areas, including bone reaction to different forces. Right now we are in the middle of a large project in which we are trying to analyze forces on bone and bone reaction to mechanical stimulus, with regard to orthodontic treatment and to the development of osteoporosis.
DR. BURSTONE If we have a patient with osteoporosis, does that influence how we do the orthodontics?
DR. MELSEN If you anticipate a reduction in bone volume, you would start off with very low forces. If you have an actual osteoporosis, you would also advise the patient to seek treatment for it. In adult patients, we have to be aware that there are more patients with metabolic bone diseases and that these have to be treated. It is interesting that sometimes we may even detect these diseases for the first time by an abnormal reaction to the stimulus we apply to the teeth. We also have to have good interprofessional relations with the endocrinologist.
DR. BURSTONE Is there anything we should look for as an orthodontist? Are the x-rays helpful or must we do medical tests?
DR. MELSEN You can look at the x-rays, and you have to look at whether your tooth movement is occurring in a different way than you anticipated according to your forces. If you suddenly see that a tooth becomes very loose or that a tooth doesn't move at all, it may be a sign of difference in the bone turnover.
DR. BURSTONE Why wouldn't the teeth move?
DR. MELSEN Patients who are on cortisone treatment have a very low cell pool available, and their bone is covered with a very thin layer of osteoids so that bone resorption is not very likely to occur. They have sterile bone surfaces without any activity going on.
DR. BURSTONE You would think that as we train new graduate students today bone biology would be very important, especially in view of the growth of adult orthodontics.
DR. MELSEN Definitely. I think it also applies to the treatment of children. We see children on a regular basis. With some medical background we might be able to detect diseases even before they give the patients real symptoms.
DR. BURSTONE Is there any evidence to suggest that calcium supplements should be prescribed for adult patients?
DR. MELSEN I think that should be determined by the endocrinologist. It has been a big question whether women in menopause should have estrogen treatment. If we treat patients who are close to menopause and they aren't getting any hormone supplement, we must be aware that there is an increased bone turnover, which may increase the risk for root resorption and undesirable side effects.
DR. BURSTONE Thank you very much, Professor Melsen.