SureSmile Technology in a Patient-Centered Orthodontic Practice
A patient-centered practice is one that delivers high-quality care with a minimal amount of patient discomfort, compliance demands, and chairtime, and completes treatment on time in as short a period as possible. Any variations in care delivery can significantly limit the ability of the orthodontist to meet these conditions.
SureSmile* technology was designed to substantially reduce errors in treatment resulting from appliance management. It provides image-capturing, three-dimensional visualization tools for diagnosis, monitoring, and patient communication, along with precision appliances that can help the orthodontist deliver truly customized care in a patient-centered practice.
This article provides an update on recent developments in SureSmile technology and an overview of clinical studies under way at the OraMetrix Clinical Research Center.1
Clinical Procedure
The dentition is prepared for scanning by applying a thin white film, similar to articulating spot spray (Fig. 1). The dental arches are then scanned using the OraScanner*, a handheld device that captures real-time, in vivo images of the dentition (Fig. 2).
Similar articles from the archive:
- JCO INTERVIEWS Dr. Rohit C.L. Sachdeva on A Total Orthodontic Care Solution Enabled by Breakthrough Technology April 2000
- Computer-Aided Fabrication of Bonded Lingual Retainers October 1996
- A Comparison of Standard Edgewise, Preadjusted Edgewise, and Tip-Edge in Class II Extraction Treatment March 2001
Fig. 1 Thin film applied to teeth to make them visible to OraScanner.
The OraScanner uses structured white light to take images in rapid succession, and is reference-independent, meaning that the image-capturing process is not affected by movement of the patient or the scanner. The scanner and computer can be stored in a mobile SureSmile cart that rolls from chair to chair (Fig. 3).
During the initial appointment, a quick scan of the dentition can be taken to visually demonstrate the patient's needs. An interactive CD-ROM helps orthodontists and treatment coordinators describe how the process works and educate patients on their role in successful treatment. A full OraScan is taken during the records appointment, integrated with conventional photographs and x-rays, and entered into an electronic patient record.
OraScan Image Processing Software combines the captured images into an accurate, three-dimensional representation of the dentition, which can be viewed at the SureSmile workstation from a wide variety of perspectives (Fig. 4).
Fig. 2 OraScanner captures live images of dentition.
Fig. 3 OraScanner and computer housed in chairside SureSmile cart.
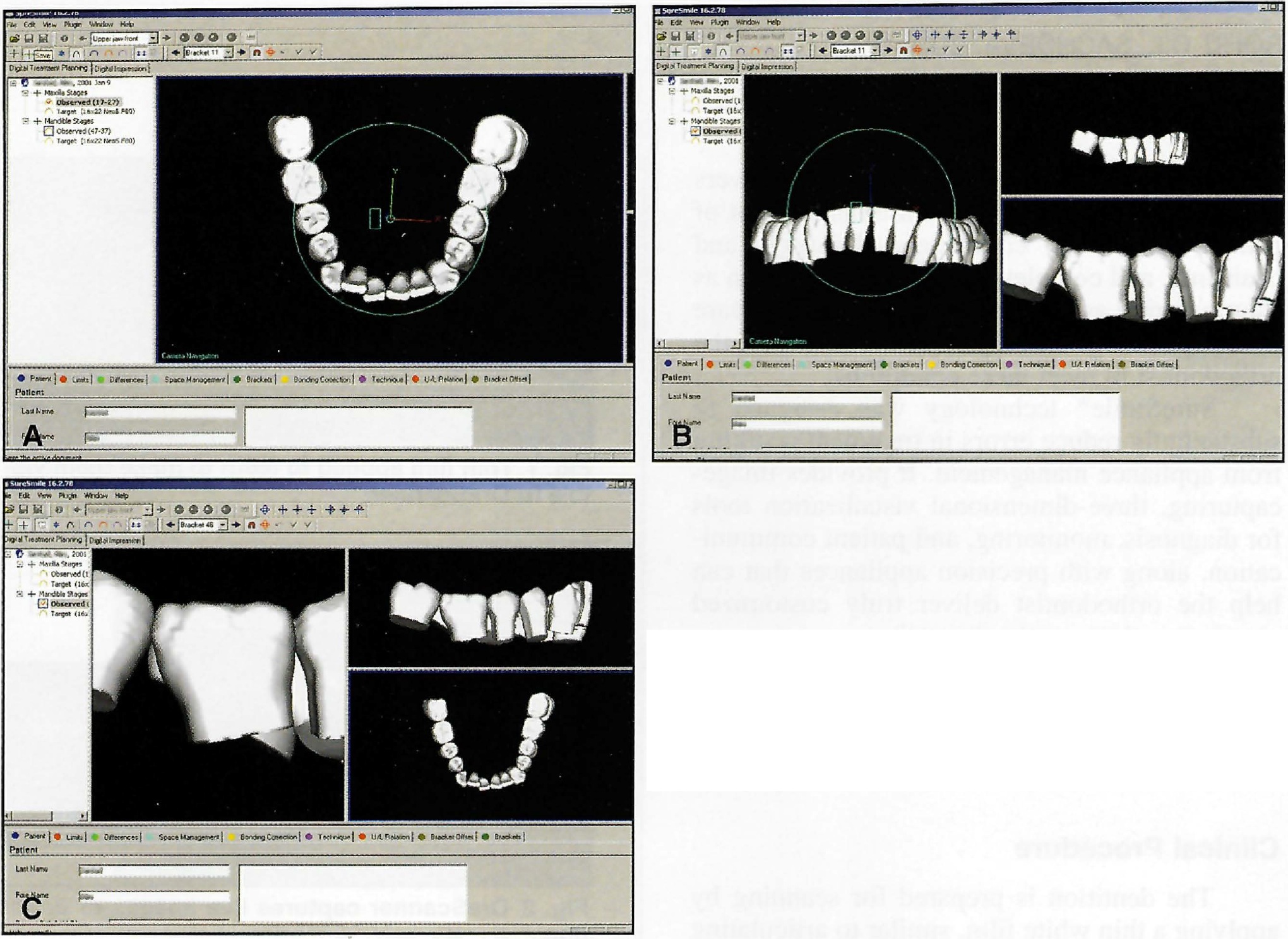
Fig. 4 A. Mandibular OraScan. B. Frontal and lateral views, with curve of Spee clearly discernible. C. Teeth may be viewed individually while maintaining overall perspective of dentition.
A coronal cross-section, like a CAT scan, is available for evaluation of 3rd-order relationships (Fig. 5).
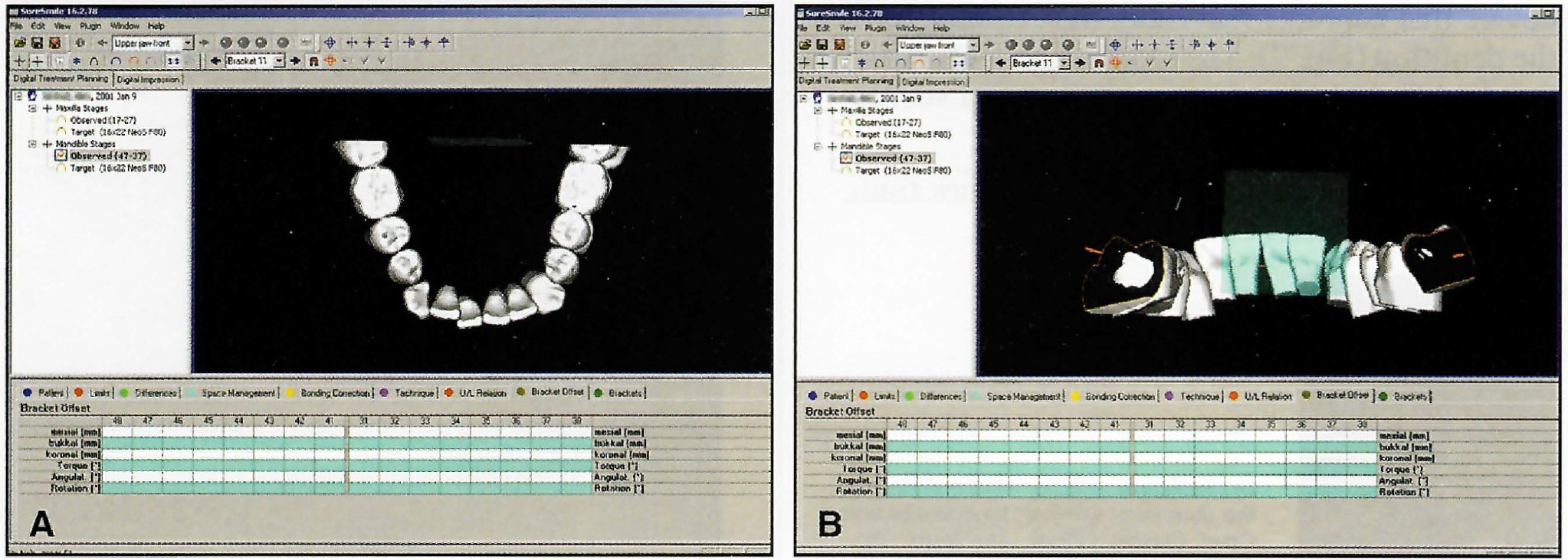
Fig. 5 A. Coronal cross-section of second molars used to evaluate 3rd-order relationships. B. Lingual view of cross-section demonstrates 3rd-order differentials.
The clinician plans treatment based on parameters such as midline, occlusal plane level, and arch dimensions (Fig. 6). Multiple plans can be simulated for comparison. The final treatment plan is then represented in the form of a three-dimensional digital diagnostic setup--the target occlusion (Fig. 7).
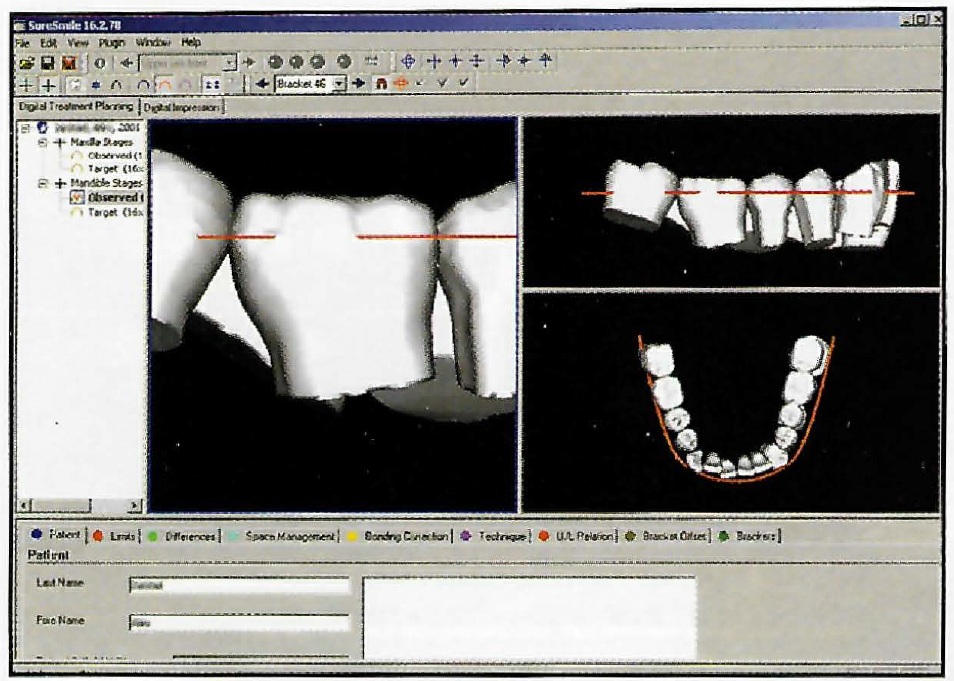
Fig. 6 Target functional occlusal plane level (defined through marginal ridges), arch dimensions, and midline selected by clinician.
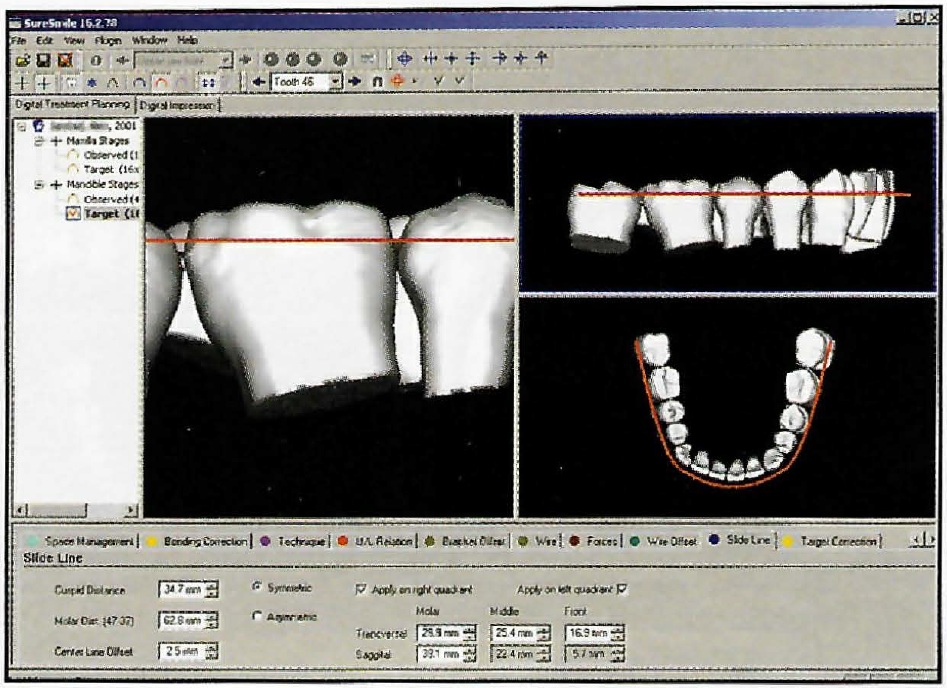
Fig. 7 Three-dimensional digital setup of target occlusion.
When the orthodontist is satisfied with the target positions, the automatic digital bonding feature is activated (Fig. 8A). Initial bracket positions are determined by doctor-defined default settings, chosen from a digital library that contains most common bracket types and prescriptions.
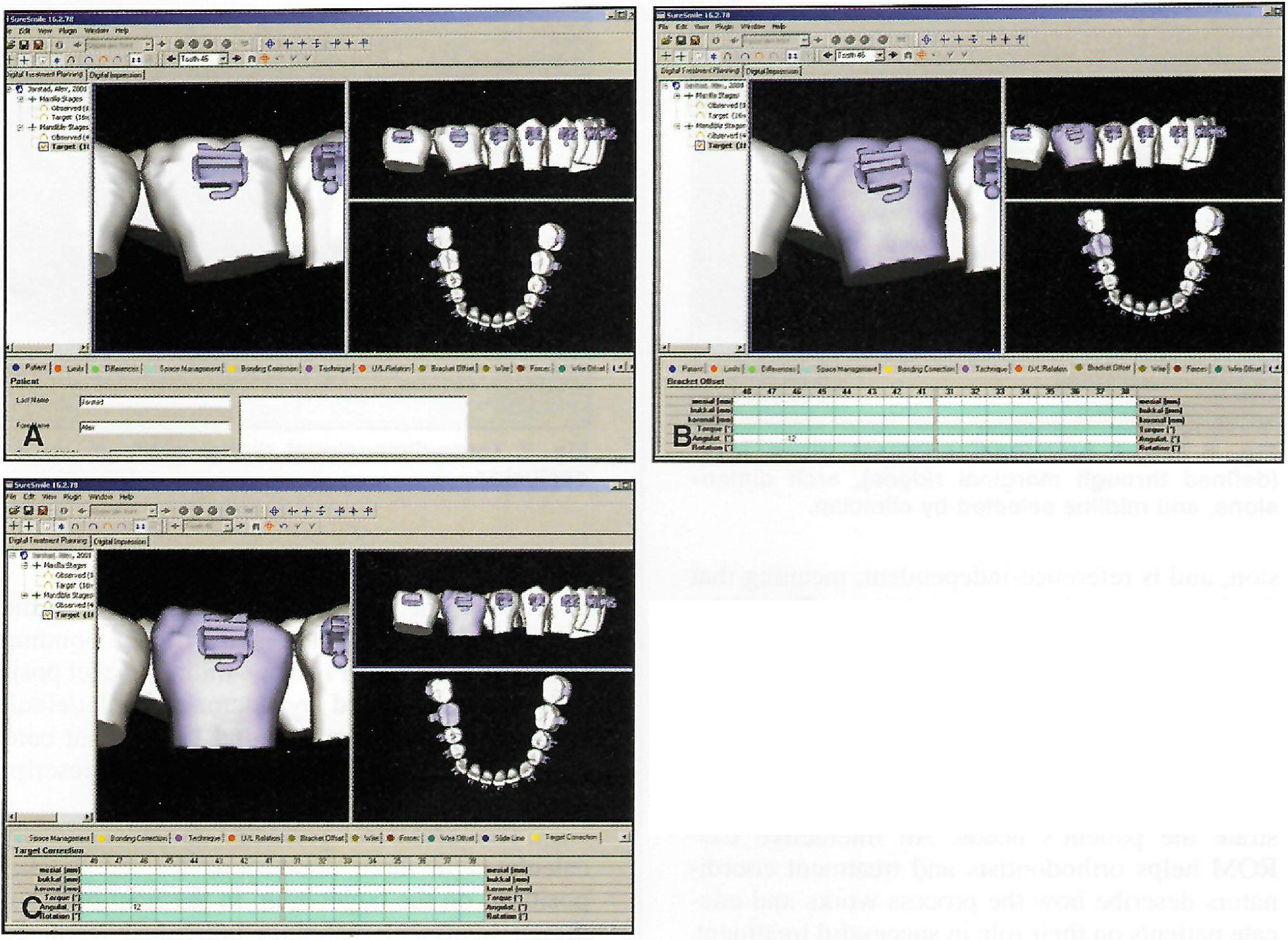
Fig. 8 A. Target arch with bracket positions defined by default settings. Note misplaced mandibular first molar bracket. B. Bracket position on mandibular first molar digitally corrected in 2nd order. C. Simulation of first molar correction in response to bracket repositioning.
The archwire geometry is automatically calculated in three dimensions for the bracket positions on the target arch. In the final phase of digital treatment planning, individual teeth are viewed close up using the zoom function, and the position of each tooth is further refined by changing bracket position, archwire geometry, or a combination of the two (Figs. 8, 9, and 10).
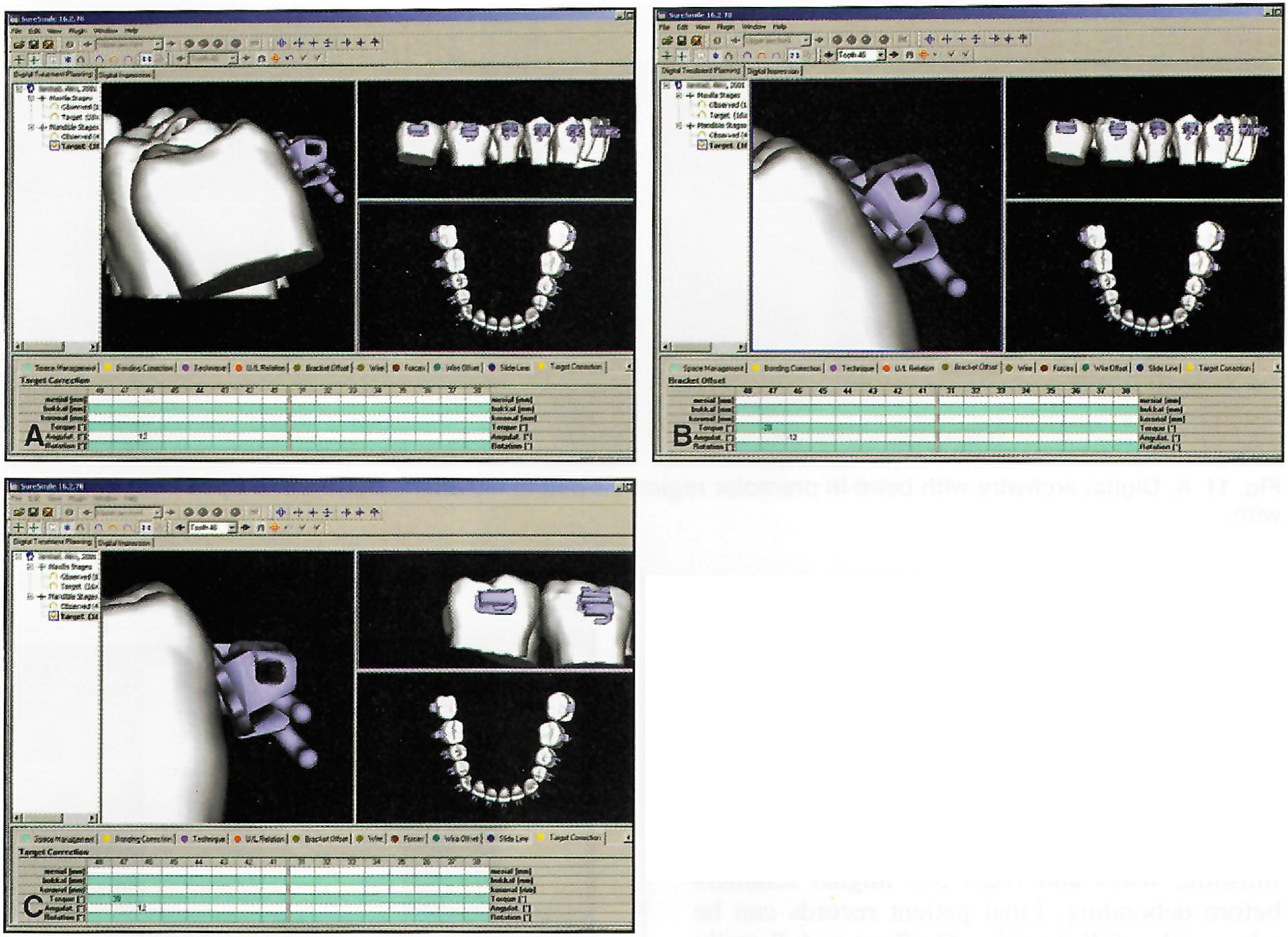
Fig. 9 A. Excessive lingual crown torque on mandibular right second molar. B. Corrected molar tube position provides buccal crown torque on second molar. Gap between bracket base and tooth represents adhesive thickness. C. Simulation of 3rd-order correction on second molar. Gap between bracket base and tooth demonstrates incongruity between base and tooth surface.
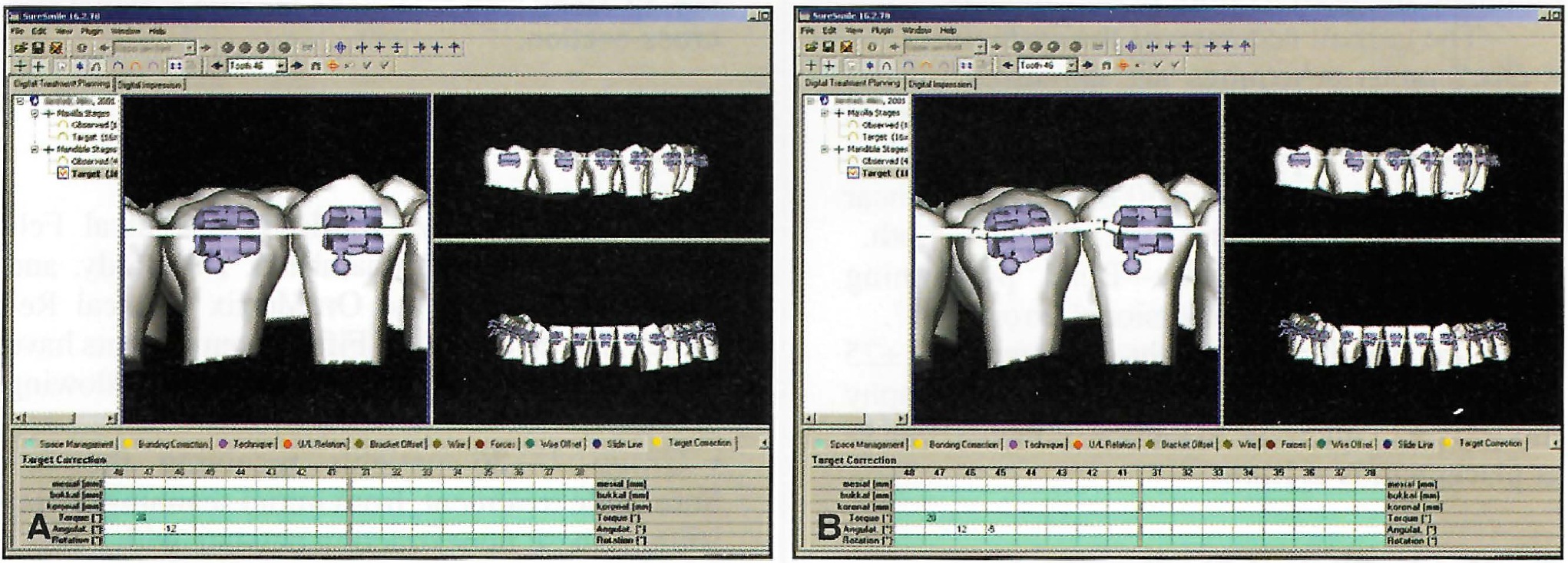
Fig. 10 A. Mandibular second premolar requiring 2nd-order correction. B. Second premolar position corrected with bend in digital archwire.
The archwire geometry may also be viewed in isolation in three-dimensional space, and compound geometries such as curve of Spee, expansion, and asymmetric archforms can be designed into the archwire (Fig. 11).
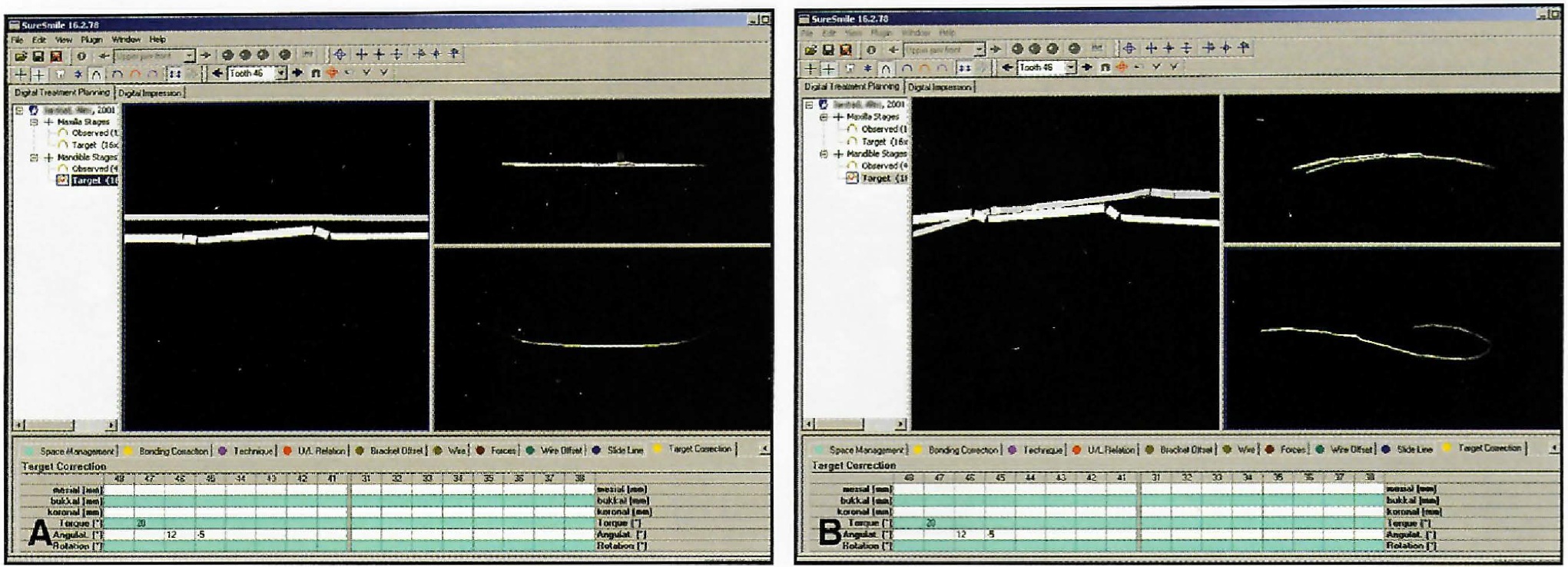
Fig. 11 A. Digital archwire with bend in premolar region viewed in isolation. B. Curve of Spee built into archwire.
After the geometry of the digital archwire has been finished, the orthodontist selects the appropriate cross-section, material, and force output from the computer menu (Fig. 12).
The result is an electronic prescription of the archwire design and customized bracket positions on the image of the original malocclusion (Fig. 13).
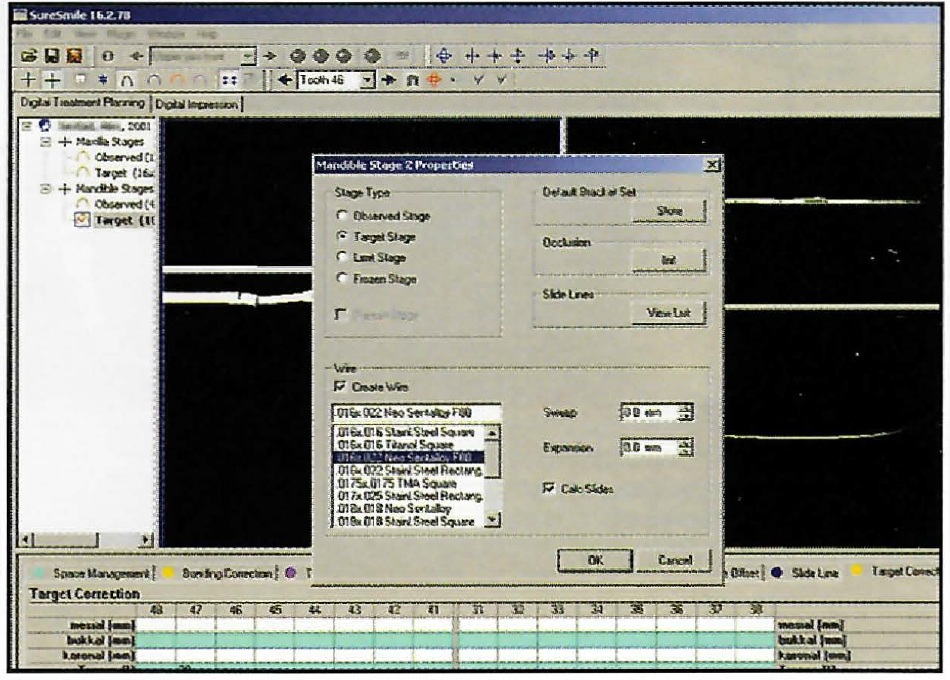
Fig. 12 Menu with selections for wire material and cross-section.
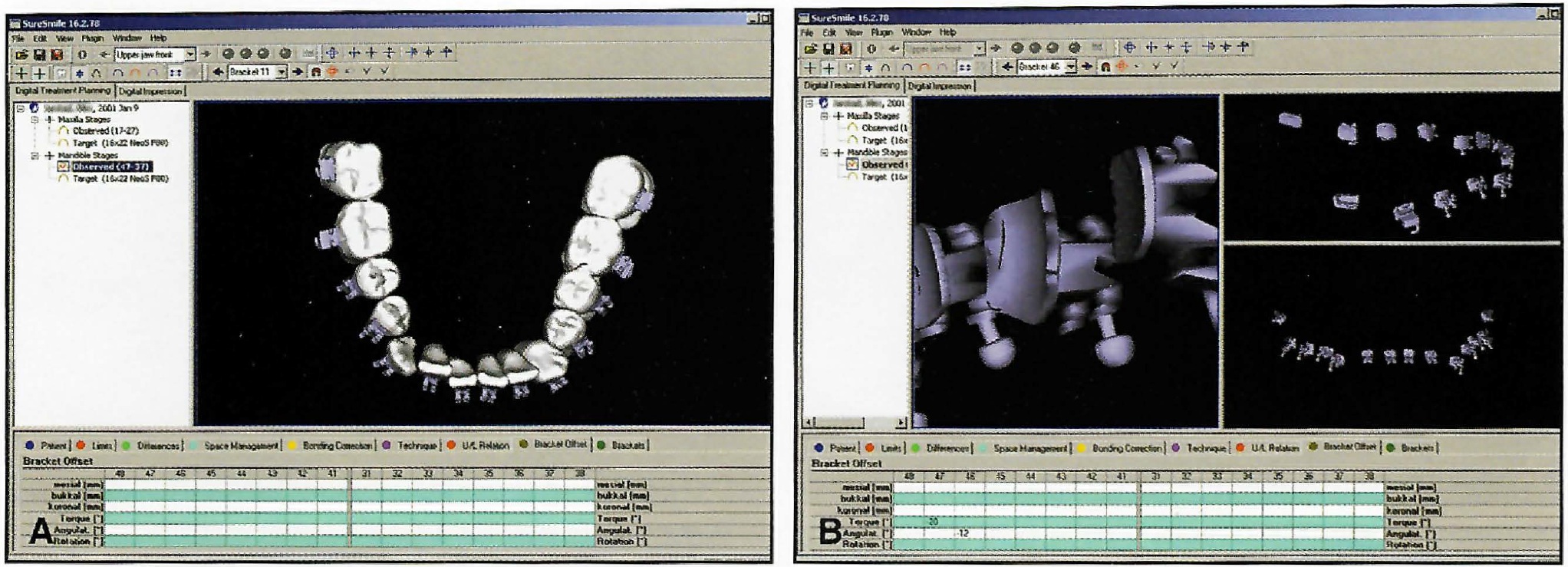
Fig. 13 A. Bracket positions transferred to pretreatment scan. B. Digital bracket template viewed in isolation.
This treatment plan is sent over a secure computer network to the SureSmile Precision Appliance Center for fabrication of archwires and precision bracket trays. A passive archwire can also be designed for presurgical orthodontics or stabilization of periodontally compromised teeth (Fig. 14).
Within 10 days after the order is placed, the orthodontist receives the prescription wires and blank precision trays for indirect bonding. These trays are currently fabricated with a Biostar** vacuum former over solid models generated by stereolithography from the OraScan images. Ora-Metrix eventually plans to fabricate precision trays directly from the OraScan and eliminate the intervening steps.
Brackets are placed in the precision trays in the orthodontist's office and are then ready to bond using any conventional indirect bonding technique (Fig. 15). If Reliance Maxi-Cure Sealants A and B*** are used, the second tray can be placed in the mouth about three minutes into the cure cycle. The trays are easily removed, with little risk of dislodging the brackets. Complete bonding of both arches is accurate and fast using this method, although direct bonding can be used if preferred by the clinician.
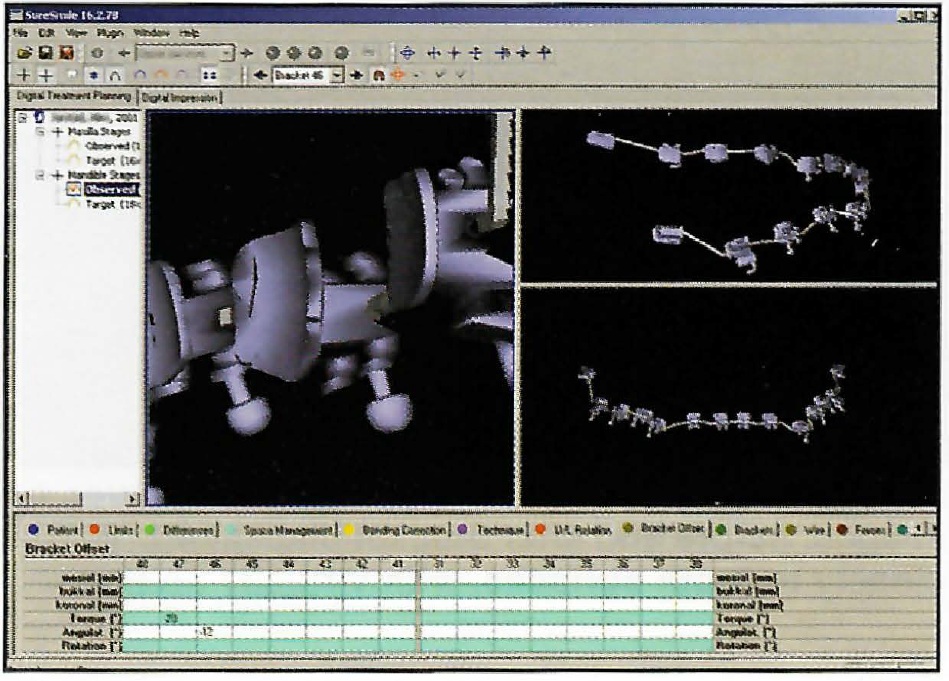
Fig. 14 Passive archwire designed for bracket positions.
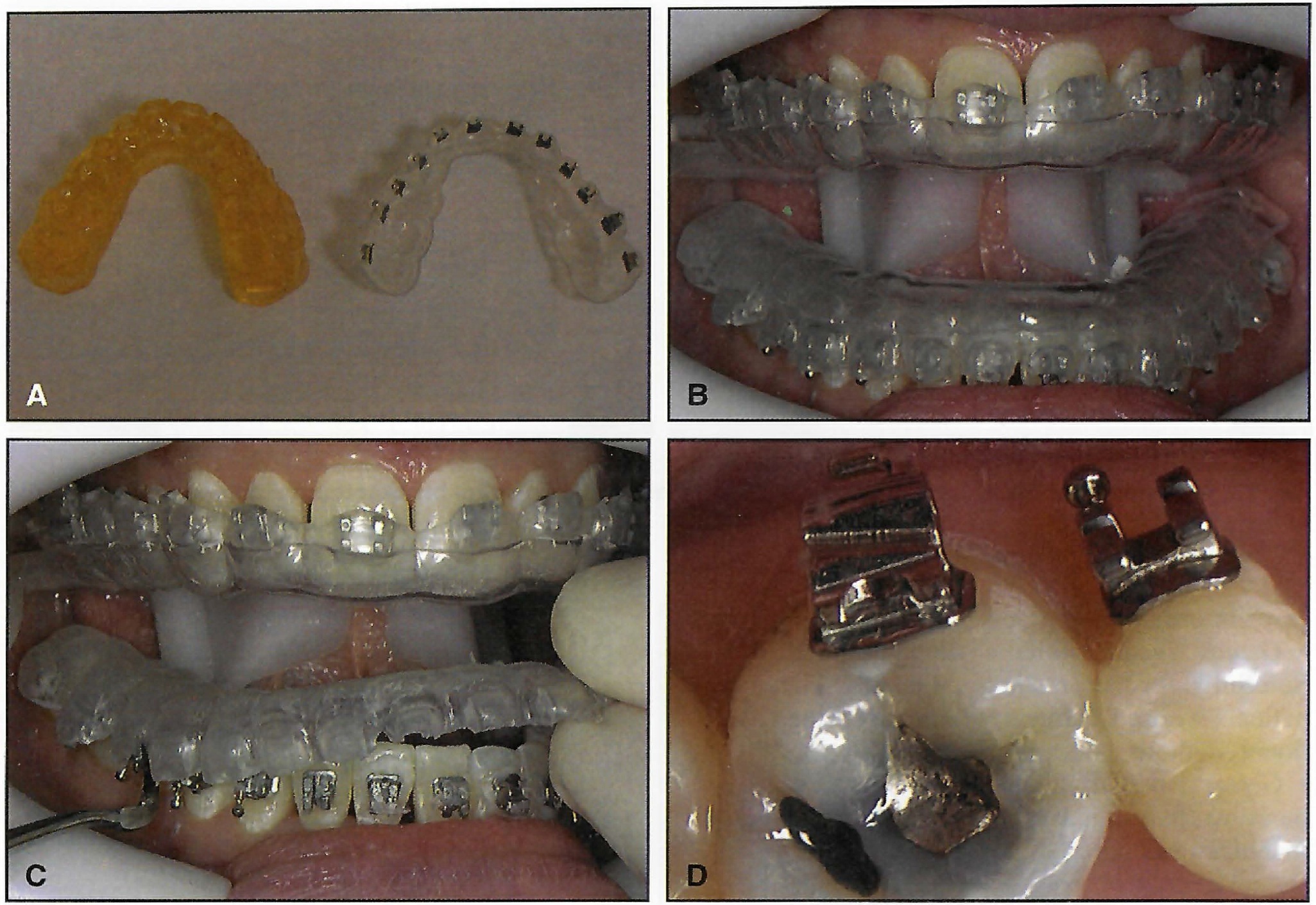
Fig. 15 A. Precision bonding tray made over solid model generated by stereolithography from OraScan images, before and after bracket placement. B. Bonding trays in mouth. C. Tray removal. D. Brackets conform closely to tooth surfaces, with virtually no flash.
At subsequent visits, the orthodontist can use the OraScanner to quantify progress and communicate this progress to the patient. SureSmile can be used to manage errors at any stage during the care cycle. If rebonding is necessary, the clinician can use the initial indirect bonding tray, order a new tray, or fabricate a tray from the solid model (with printed brackets) provided by the Appliance Center. The orthodontist can also replace a bracket by direct bonding and verify its position with the digital bracket template.
New OraScans can be used for designing finishing wires and fixed 3-3 lingual retainers before debonding. Final patient records can be taken with a full-dentition OraScan and digitally archived for future reference. Digital records eliminate the need to store plaster models.
The current accuracy of the system:
- OraScanner--Acquires six unblurred images per second with as many as 3,500 three-dimensional measuring points per image. The accuracy of each point is better than 50 microns; the linear error of scan is no greater than .1mm per tooth.
- Wire-bending accuracy--Bend positioning error is ±.1mm; angular/torsional error is ±1°.
- Digital bracket placement--Accurate to ±25 microns. The accuracy of the stereolithography model is ±25 microns. Accuracy of in vivo bracket placement is ±.1mm.
OraMetrix Clinical Studies
Clinical research studies are currently being conducted by OraMetrix's Clinical Fellows--Drs. James Archambeau, Pat Brady, and Monte Collins--at the OraMetrix Clinical Research Center in Dallas. Fifty-seven patients have been recruited and divided into the following groups:
- Group 1--26 patients receiving the full SureSmile treatment, from initial scanning to finishing. These nonextraction patients with Class I malocclusions and minor-to-moderate crowding represent the most commonly treated types of cases in orthodontic practice.
- Group 2--11 patients being treated with SureSmile for the finishing phase only. These are patients whose treatment was begun using traditional methods.
- Group 3--20 patients being treated only to measure the clinical effectiveness of precision-manufactured wires.
The control group comprises a retrospective sample of treated patients selected from the practices of the Clinical Fellows. Recruitment continues to enlarge the study samples. Ora-Metrix plans to expand its research program into the academic setting later this year.
Various clinical parameters have been selected to evaluate the clinical effectiveness and efficiency of the SureSmile process, including ease of use and clinical utility of treatment planning with the SureSmile software, clinical reliability of the precision bonding process, control of tooth movement, length of treatment, number of archwire changes and adjustments, appliance failures, and patient discomfort. Most important, the American Board of Orthodontics guidelines for case evaluation have been adopted to weigh the quality of treatment.2 An external review board, made up of experienced specialists from both academia and private practice, will be recruited to evaluate the treatment results.
Preliminary clinical findings are listed below.
Group 1
OraMetrix's current clinical protocol uses an indirect-bonded .018" Mini Diamond† bracket system with .016" X .022" nickel titanium archwires for alignment and .017" X .025" TMA† wires for leveling and finishing. Depending on the care plan, the treatment time has been projected to be 10-14 months. Of course, factors such as biological response, severity of the malocclusion, patient compliance, oral hygiene, iatrogenic effects, broken appliances, and missed appointments can lengthen treatment. Our initial observations include:
- It appears that the custom archform designed with SureSmile provides excellent control of arch width, and that initial alignment occurs unimpeded.
- For most patients under care, there appears to be no more discomfort associated with these wires than with wires of smaller cross-section.
- Extended appointment intervals (in our current protocol, two months) do not seem to adversely affect the quality of care.
- We anticipate that the OraMetrix Clinical Fellows will complete the care of these patients using the two recommended archwires within the projected treatment time.
OraMetrix does not necessarily endorse this care protocol or products. For the purposes of our studies, we have tried to minimize conflicting variables; once SureSmile is in wider use, clinical benchmarks will evolve as a result of experiences shared by practitioners.
Group 2
Patients in this group are still under treatment, with the expectation that a single precision finishing wire, requiring no adjustments, may reach the desired results in about half the time required for the control group.
Group 3
Care has been completed on eight patients, with these results:
- Finishing was completed in four months, as compared to seven months in the matched control group.
- The quality of the treatment is currently being evaluated.
Discussion
The results presented here must be considered with caution because they represent only clinical impressions. As the sample size increases, the inclusion criteria for patients are broadened, and more completed case histories are added, the data will allow better statistical evaluation of the SureSmile care process. As the SureSmile technology continues to mature and be tested, more clinical and research findings will be made available to orthodontists.
In early observation of Clinical Fellows using the SureSmile software, we find they are able to learn the system relatively quickly--in most cases, in a matter of hours--even though some have little or no familiarity with the computer. The visual interface contributes to this ease of learning by being intuitive and having a clinical feel.
The OraScan and its associated visualization and measurement tools provide an unprecedented aid to the clinician in evaluating the spatial position of each tooth in the dental arch, easily surpassing conventional study models. The look and feel of a virtual study model appear to be an improvement over the traditional model. SureSmile also offers a reliable, reproducible, and efficient approach to indirect bonding that is easily learned and adapted into clinical practice.
The ability to plan care from a common baseline and to simulate and visualize various scenarios in three-dimensional space has allowed the clinicians to be more creative in seeking treatment solutions. It seems that the capability of precisely placing brackets three dimensionally and of designing accurate, force-system-driven archwires has made them acutely aware of previous clinical limitations in controlling these factors. This realization has allowed them to build maximum effectiveness and efficiencies into their appliance designs and to streamline their therapeutic protocols.
Conclusion
SureSmile can substantially reduce many common errors in fixed appliance treatment, and it can enhance the quality of care afforded to the patient by compressing the treatment cycle and reducing the number of appointments. SureSmile gives the clinician powerful tools to deliver consistent, high-quality care to all patients, regardless of practice volume. In short, this technology is designed for the patient-centered practice.
ACKNOWLEDGMENTS: The author would like to acknowledge Ed Kelton for his editorial assistance and the preparation of this manuscript. The comments of Dr. James Archambeau, Dr. Pat Brady, Dr. Monte Collins, Dr. Gregg Cohen, Calvin Head, Scott Iserman, Lea Nesbit, Rüdger Rubbert, Gary Sadow, and Thomas Weise are gratefully appreciated.
FOOTNOTES
- *Trademark of OraMetrix, Inc., 12740 Hillcrest, Suite 100, Dallas, TX 75230.
- **Great Lakes Orthodontics, 190 Fire Tower Drive, Tonawanda, NY 14150.
- ***Reliance Orthodontic Products, P.O. Box 678, Itasca, IL 60143.
- †Registered trademark of Ormco/“A” Company, 1717 W. Collins Ave., Orange, CA 92867.
REFERENCES
- 1. JCO Interviews Dr. Rohit C.L. Sachdeva on a Total Orthodontic Care Solution enabled by breakthrough technology, J. Clin. Orthod. 34:223-232, 2000.
- 2. Found at www.americanboardortho.com.


