CASE REPORT
Treatment of a Brodie Bite in an Adolescent Patient
Brodie bite, also known as Brodie syndrome, scissor bite, or buccal crossbite, is a rare malocclusion that occurs in 1-1.5% of the population.1 First described by Allan G. Brodie in 1952, it is caused by a transverse occlusal discrepancy, which can be accompanied by varying degrees of facial asymmetry.2-4 Its etiology can involve genetic factors or a functional or muscular imbalance.
Clinically, a scissor bite presents as contact between the buccal surfaces of the lower posterior teeth and the palatal surfaces of the upper posterior teeth,5 with no occlusal contact between the proper cusps and fissures. It can appear in either a skeletal form, characterized by excessive maxillary width or a mandibular transverse deficiency, or a dentoalveolar form, marked by buccally inclined upper posterior teeth, lingually inclined lower posterior teeth, or both.3,5 A mixed etiology involving both skeletal and dentoalveolar components5,6 can be recognized by an excessive maxillary intermolar distance, associated with a slight transverse maxillomandibular dentoalveolar compensation.2 A scissor bite can also be classified as unilateral, with a flat, asymmetrical palatal vault, or bilateral, with a flat but symmetrical palatal vault2; of the two, the bilateral variant is easier to treat.7 Associated malocclusions include a mandibular rotation or lateral shift, facial asymmetry with an inclined occlusal plane, or an anterior or posterior deep bite. In addition, patients can develop such adverse habits as chewing only on the side contralateral to the scissor bite.
Management of a Brodie bite can be challenging.8 An early diagnosis will significantly improve the prognosis9: in a patient with remaining growth, normal bone development can resume as soon as the transverse buccal crossbite is corrected,10 whereas a delay in treatment could result in a more severe malocclusion in the permanent dentition.11 Clinical analysis, study models, photographs, two-dimensional radiographs, and three-dimensional craniofacial x-rays can be used to differentiate between the skeletal and dentoalveolar forms of scissor bite2; an evaluation of the shapes of the palatal vault and midpalatal raphe can help determine whether the Brodie bite is unilateral or bilateral. Analysis of 3D images will facilitate the identification of dentoalveolar compensations, which can involve both the transverse and vertical planes.10 The diagnosis should also consider the orientation of the alveolar process at the canine, premolar, and molar levels; the curves of Spee and Wilson; and the degree of occlusal canting.
If the scissor bite is dentoalveolar in origin, without a severe skeletal asymmetry, potential treatment options include maxillary constriction plates, intermaxillary cross-elastics, the “dragon helix” appliance, and functional appliances.3 Temporary anchorage devices (TADs) can be used to limit the undesirable side effects of dental anchorage.12 This article discusses the appropriate treatment mechanics for different types of Brodie bites and presents a case treated with skeletal anchorage.
Diagnosis and Treatment Plan
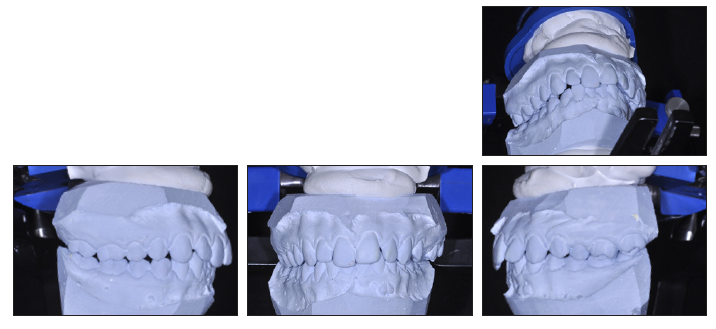
A 15-year-old female presented for a routine orthodontic examination (Fig. 1A). Clinical examination showed a brachyfacial growth pattern and a mildly retrusive chin. From the front, the face was slightly asymmetrical, with the lower midline slightly deviated to the right of the facial midline. The transverse width of the maxilla was excessive, and the maxillary occlusal plane was canted, with the left side lower than the right. The curve of Spee was exaggerated.
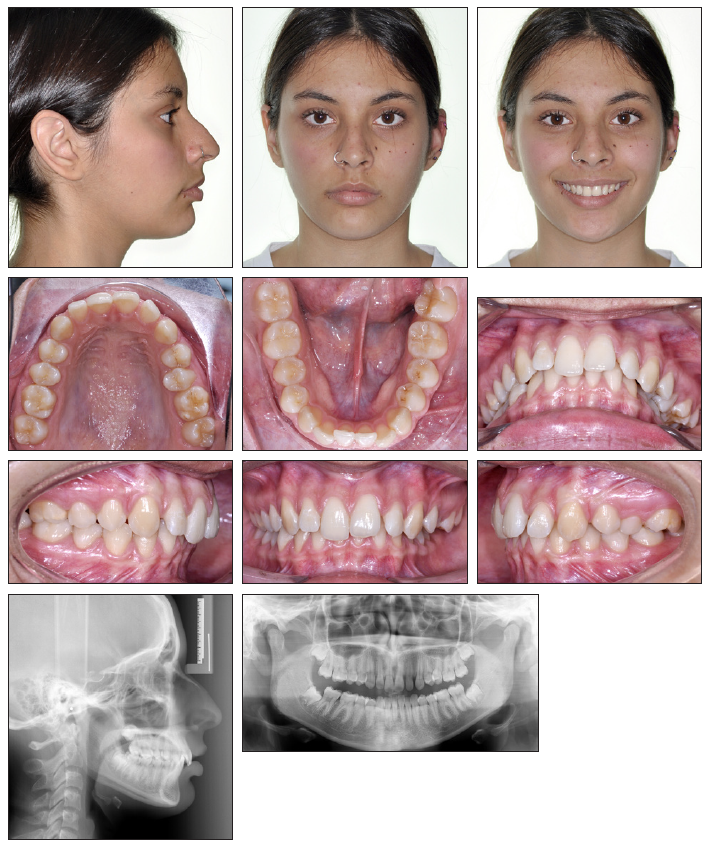
Fig. 1 15-year-old female patient with Brodie bite at left first premolar and left first and second molars before treatment (continued in next image).
The permanent dentition had fully erupted, with the third molars in the intraosseous stage of development. Bilateral Class II molar and canine relationships were present. A 4mm overjet and 7mm overbite were measured in maximum intercuspation (Fig. 1B). Because the upper central incisors were overerupted relative to the occlusal plane, the tooth exposure at rest was excessive (6mm). The upper lateral incisors were undersize, and the lower arch had 6mm of crowding, creating a 4mm Bolton discrepancy. The upper segment was overextruded and buccally inclined, while the lower central incisors and left premolars and molars were lingually inclined. The overall result was a Brodie bite on the left side at the first premolar and the first and second molars (Fig. 2A).
During the functional examination, the patient reported neck and back pain. The lateral cephalogram showed an abnormal cervical spine curvature, with the odontoid process significantly displaced to the right relative to the atlas vertebra in the coronal plane. Although no active TMD symptoms were reported, cone-beam computed tomography (CBCT) revealed excessive movement of the condyles above the temporal eminences during maximum mouth opening, as well as a slight discrepancy between maximum intercuspation and the musculoskeletally stable position (Fig. 2B).

Fig. 2 A. Brodie bite before treatment (continued in next image).
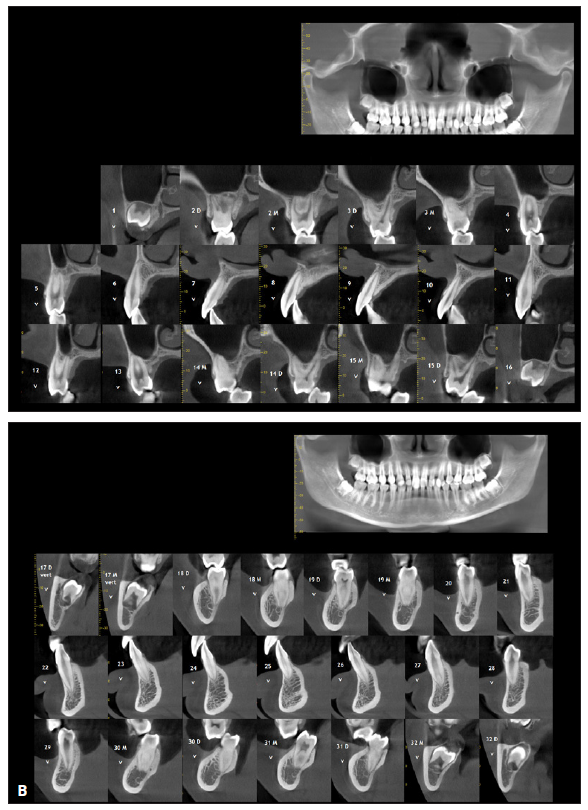
Fig. 2 (cont.) B. Cone-beam computed tomography (CBCT) used to visualize positions and bone support of teeth involved in Brodie bite.
Cephalometric analysis (Table 1) indicated a skeletal Class II malocclusion (ANB = 5°, Wits appraisal = +6mm).
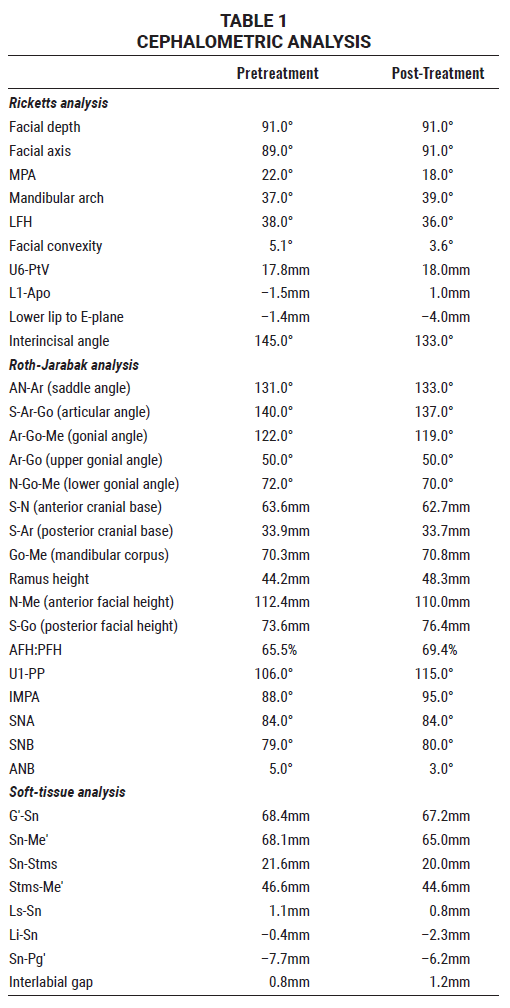
The brachyfacial growth pattern was confirmed by an anterior-to-posterior facial-height ratio of 70%,13,14 deficient gonial and articular angles, and an excessive mandibular angle. A reduced facial-depth angle supported the diagnosis of a Class II malocclusion, while an increased saddle angle suggested a lack of mandibular development in the sagittal dimension. Soft-tissue analysis found an adequate anteroposterior relationship of the upper and lower lips, along with a retrusive soft-tissue pogonion. In the transverse dimension, the Penn CBCT Analysis demonstrated a 4.54mm maxillary excess (Fig. 3),15 while element III of Andrews’s analysis indicated a 4.5mm excess (Fig. 4).16
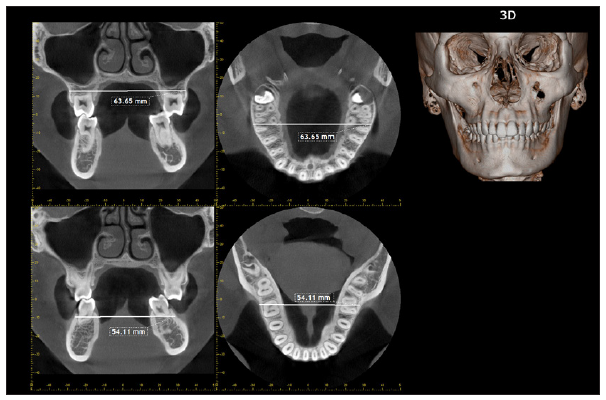
Fig. 3 Penn CBCT Analysis15: 54.11mm mandibular width and 63.65mm maxillary width (rather than expected 59.11mm), indicating 4.54mm maxillary excess.
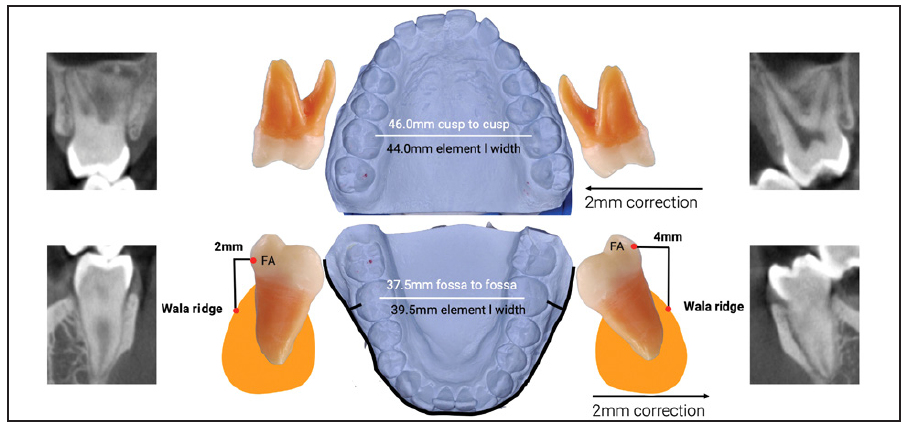
Fig. 4 Element III of Andrews’s analysis16: 46mm maxillary width measured at palatal cusps of first molars, adjusted to 44mm due to inclination of left molar, and 37.5mm mandibular width measured at central fossae of first molars, adjusted to 39.5mm due to inclination of left molar, indicating 4.5mm maxillary excess.
The treatment goals were to address the Class II malocclusion and Brodie bite, level the curve of Spee, and correct the Bolton discrepancy. Fixed appliances would be used, along with TADs and a bite plate. All third molars would be extracted during treatment to make room for the planned tooth movements.
Individual tooth movements were based on a CBCT assessment of the inclination and bone support for each tooth involved in the Brodie bite
(Fig. 2B). In the maxilla, the upper molars would be distalized and slightly intruded, and the torque of the upper incisors would be corrected during their intrusion. The lower curve of Spee would be leveled through lower-incisor intrusion and slight proclination. Autorotation of the mandible would project the chin forward, helping to correct the Class II malocclusion. At the end of treatment, the Bolton discrepancy would be addressed with restorations.
Treatment Progress
Complete Clinical Orthodontics*-prescription brackets were bonded, and leveling and alignment were initiated with .014" heat-activated nickel titanium wires in both arches (Fig. 5).

Fig. 5 Complete Clinical Orthodontics*-prescription self-ligated brackets bonded and .014" heat-activated nickel titanium archwires inserted; bite plate and temporary anchorage devices (TADs) used for early Brodie bite treatment.
At the same time, 2mm × 9mm TADs** were placed between the upper and lower left first and second molars to support correction of the Brodie bite (Fig. 6A).
Elastomeric chains were attached from the lower TAD to lingual buttons bonded to the lower left molars, and from the upper TAD to buccal tubes on the upper left molars. A palatal anterior bite plate was placed to prevent occlusal trauma. After two months, it became apparent that the TADs had been placed too close to the teeth; to enable further tooth movement, both TADs were replaced three months later (Fig. 6B).
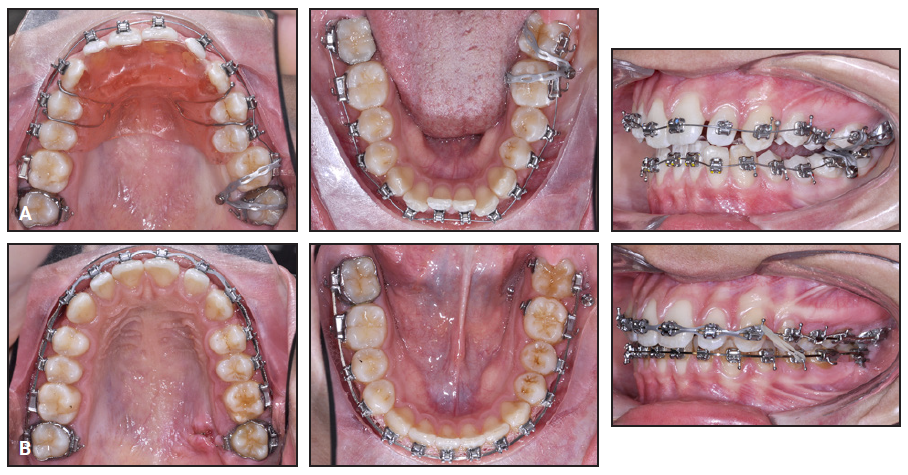
Fig. 6 A. TADs placed too close to teeth, limiting tooth movement. B. After five months, TADs replaced.
The archwire sequence continued with upper and lower .020" × .020" heat-activated nickel titanium wires, followed by .019" × .025" stainless steel. The lower arch was overexpanded on the left, and the upper arch was constricted to assist in the transverse correction.
After the Brodie bite was corrected, the bite plate was discontinued. At this point, the Class II correction began with the insertion of bilateral 2mm × 12mm infrazygomatic TADs and nighttime wear of intermaxillary elastics (1⁄8", 4oz).*** The TADs were activated with a double-force system, using size E7 E-Chains† from the upper canines and premolars to the TADs (Fig. 7) and size E4 E-Chains to distalize the upper arch. Because the elastics delivered a force below the maxilla’s center of resistance, they produced maxillary posterior intrusion, stimulating mandibular autorotation and a consequent increase in chin projection.
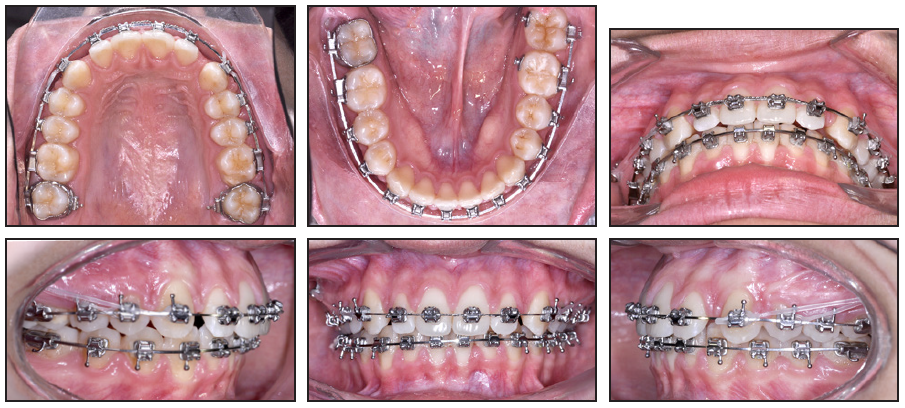
Fig. 7 After one year of treatment, bilateral infrazygomatic TADs inserted for Class II correction; E-Chains† attached from TADs to upper canines and first premolars.
All four third molars were extracted at this time. An .020" stainless steel archwire with a reverse curve was inserted in the lower arch for further leveling of the curve of Spee. The upper incisors were intruded and retruded with an upper .019" × .025" TMA‡ archwire, with loops to close the spaces (Fig. 8). Because the incisor intrusion was excessive, however, the incisors had to be releveled with the subsequent archwire. Interproximal reduction was performed on the distal sides of the lower canines to facilitate space closure distal to the upper canines.
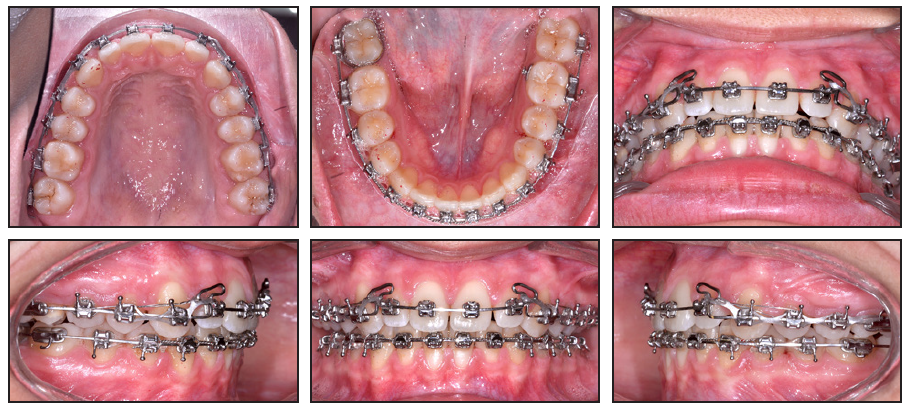
Fig. 8 After two years and eight months of treatment, showing upper .019" × .025" TMA‡ wire with single loops used to close spaces and interproximal reduction performed on distal sides of lower canines to assist in closing spaces distal to upper canines; note undesirable incisor intrusion.
For detailing and settling, .021" × .025" upper and lower braided archwires were used with short elastics (1⁄8", 4oz) in different positions (Fig. 9). Occlusal adjustments were made several times over the course of treatment to improve the bite.
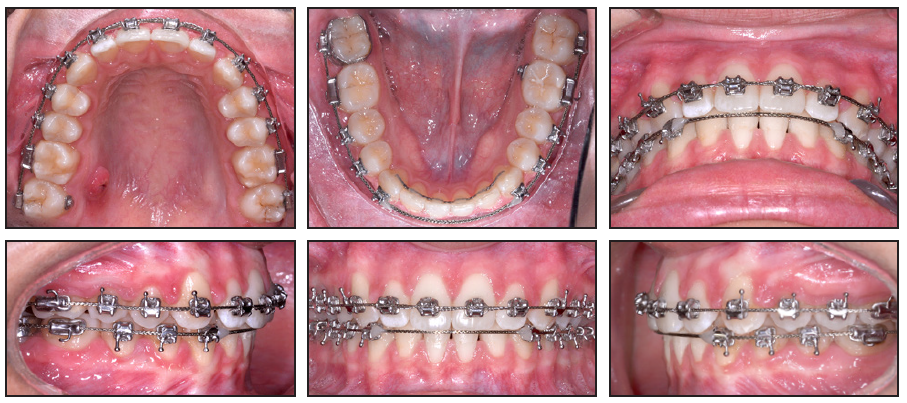
Fig. 9 Braided .021" × .025" wires inserted in both arches for detailing and settling.
After 35 months of active treatment, the TADs were removed and the patient was debonded. A lower 3-3 stainless steel Ortho-Flextech†† chain was bonded, and upper and lower wraparound Hawley retainers with customized acrylic extensions on the buccal surfaces of the teeth were delivered to be worn full-time for six weeks and at night thereafter.
Six months after appliance removal, an acrylic occlusal splint was prescribed, to be worn at night, and restorative work was performed to correct the Bolton discrepancy, with buildups added on the distal sides of the upper lateral incisors and the mesial side of the upper left canine (Fig. 10A).
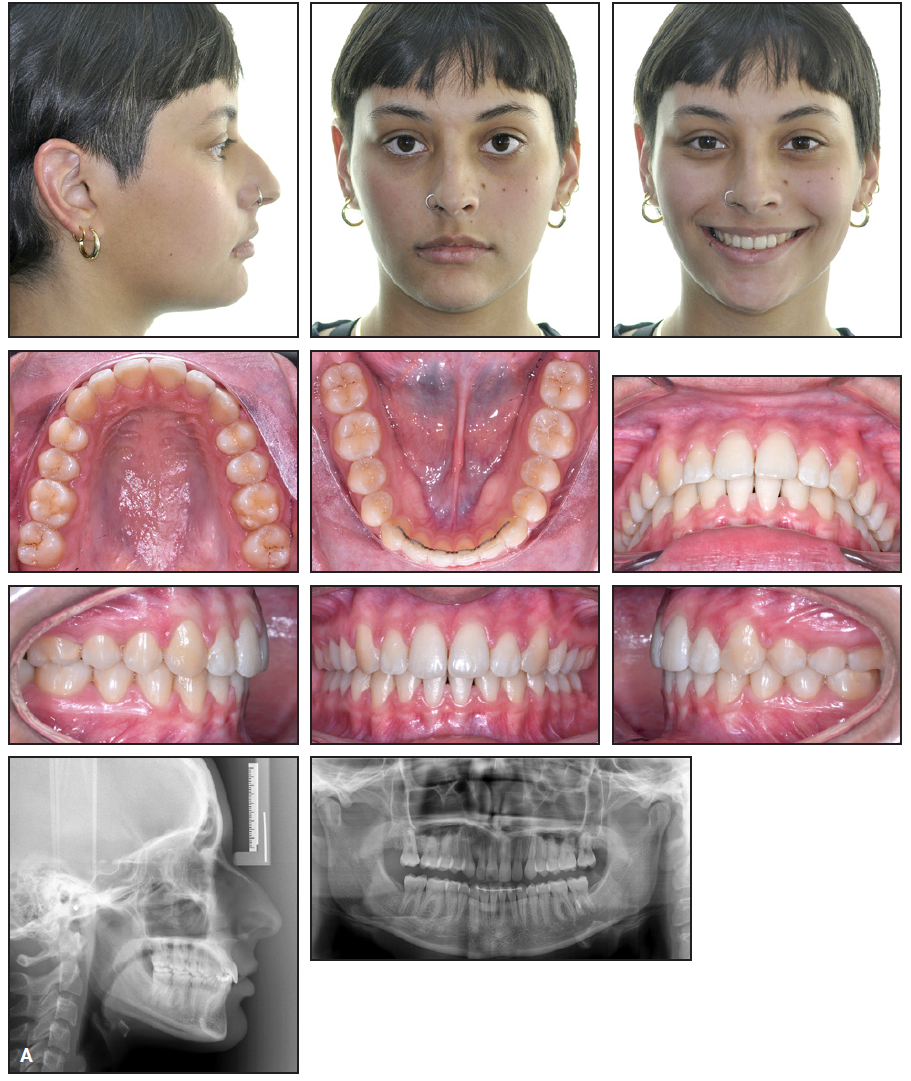
Fig. 10 A. Six months after debonding, restorative work completed (continued in next image).
Treatment Results
Cephalometric analysis confirmed closure of the facial-axis angle and vertical growth of the maxilla, along with intrusion of the upper molars
(Table 1). The upper incisors were intruded and favorably inclined. The curve of Spee was leveled, with intrusion and slight protrusion of the lower incisors and extrusion of the lower first molars (Fig. 10B).
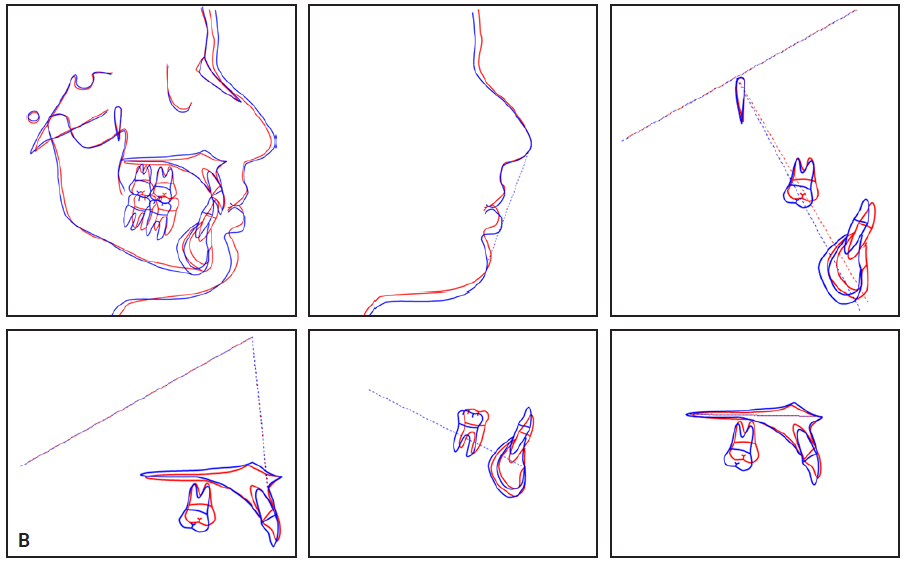
Fig. 10 (cont.) B. Superimpositions of pretreatment (blue) and post-treatment (red) cephalometric tracings (continued in next image).
The Class II correction was achieved primarily through an increase in chin projection resulting from posterior intrusion and mandibular growth and autorotation; no distal movement of the upper molars was observed. The patient reported that she was no longer experiencing neck and back pain (Fig. 10C).
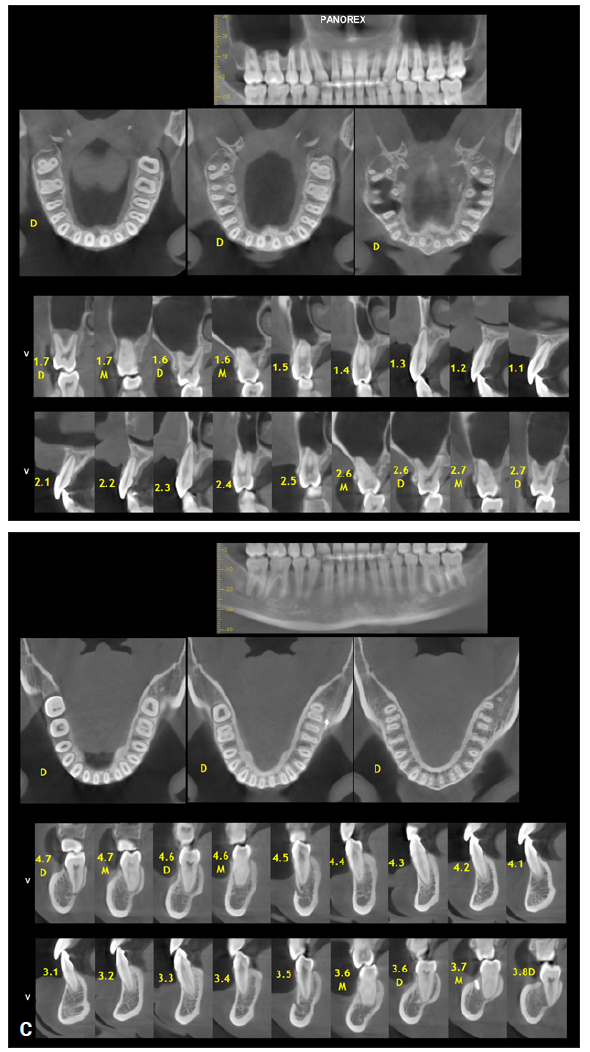
Fig. 10 (cont.) C. CBCT images of involved teeth after correction of Brodie bite.
At the six-month post-retention appointment, the results remained stable,17 and the patient demonstrated compliance with the prescribed retention protocol (Fig. 11).

Fig. 11 Patient three years after treatment, demonstrating stable results (shown with cosmetic dental jewels).
Discussion
Since a Brodie bite does not affect a patient’s appearance from the front, it often remains undiagnosed until late in its development,18 potentially resulting in complications such as Class II malocclusion, mandibular-development disorders, TMD, asymmetrical growth, or lateral deviations with functional shifts.6,19
Brodie bites are classified according to the arches affected and the dentoskeletal compensations that can generate alveolar and skeletal asymmetries, which in turn can produce canted occlusal planes. In adults, these compensations tend to occur in the vertical dimension, worsening the bite and causing lesions and ulcerations in the mucosa. The dental extrusion can sometimes be severe, leading to serious periodontal problems.2
Accurate identification and characterization of the segments involved in the Brodie bite are essential in treatment planning. Vergara’s Brodie Bite Checklist20 (Table 2) lists the clinical characteristics that should be evaluated in the diagnosis. Three different Brodie bite scenarios can occur in the upper arch, each with its own recommended treatment. Scenario 1 (Fig. 12A), exhibiting extrusion and buccal inclination of the upper segment, as in the current case, should be treated with upper intrusion and palatal movement, supported by a palatal TAD in a high midline position (Fig. 12B). In scenario 2 (Fig. 12C), where straight upper extrusion is observed, treatment should involve straight, bodily upper intrusion, anchored by palatal and buccal infrazygomatic TADs (Fig. 12D). In scenario 3 (Fig. 12E), the upper segment is both extruded and lingually inclined, and a two-stage treatment is advised: first, a buccal infrazygomatic TAD is used to bring the tooth into a vertical position (Fig. 12F); second, a palatal TAD is added for intrusive mechanics (Fig. 12G).
Because the lower arch is always lingually inclined in a Brodie bite case, lower-TAD placement need consider only whether the involved teeth are extruded. If extrusion is not observed (Fig. 13A), the TAD should be inserted so that its head is level with the archwire or the occlusal plane (Fig. 13B). If the lower segment is extruded (Fig. 13C), as in the current case, the head of the TAD should be located below the center of resistance (Fig. 13D). A low buccal-shelf position can be used to correct the lingual inclination and extrusion simultaneously. A longer miniscrew is recommended to keep the head closer to the archwire level or the facial-axis point of the anatomical crown, which will generate a smaller intrusive vector. A more buccal position relative to the molar root’s center of rotation and a more elevated TAD head will generate a more buccal and less intrusive force than with an interradicular screw, thus facilitating molar uprighting.21
When planning buccal-shelf screws in the mandible, the clinician must consider the vertical position and lingual inclination of the upper molars, since the screw head can interfere with these teeth during mouth closure. If interference is likely, an interradicular lower TAD can be used initially, or the inclination of the upper teeth can be corrected before screw insertion. If all premolars and canines are involved in the Brodie bite, the buccal shelf may be too posterior for the required tooth movements, and an interradicular TAD or multiple lower TADs should be used instead.
During bite disarticulation and crossbite correction, a bite-opening device must be used to prevent occlusal trauma. Appropriate appliances include an acetate plate with a bite block on the unaffected side, a modified Hawley appliance, or an anterior bite plate, as used in the current case (Fig. 5). When intrusion is desirable, upper palatal and lower lingual bonded bite turbos can be placed on the compromised teeth. Before prescribing a bite-opening device, it is essential to clearly differentiate the teeth involved in the scissor bite from those that are already well articulated. To avoid generating new complications such as occlusal-plane canting or additional open-bite regions, only the segments with adequate occlusion should be used for anchorage. Isolated bite turbos on the unaffected side should be utilized with care, since they can increase the risk of unwanted intrusion.
Other appliances used for Brodie bite correction include palatal distalizers,22 lip bumpers,23 or headgears.23 Surgical correction is another option24 The appropriate surgical procedure will depend on the patient’s developmental stage: mandibular distraction osteogenesis can be performed in growing patients, while the options for adults include Le Fort I osteotomy, sagittal splint ramus osteotomy, and posterior subapical mandibular surgery to relocate the affected segments.3 The choice of procedure should also consider the morphology of the arches and the number of teeth involved in the Brodie bite, as well as their degree of inclination and overeruption.3
As this case report demonstrates, an early diagnosis and careful evaluation will enable the ideal treatment mechanics to be selected for successful correction of a Brodie bite.
FOOTNOTES
- *Registered trademark of Dentsply Sirona, York, PA; www.dentsplysirona.com.
- **BioMaterials Korea, Inc., Seoul, South Korea; biomk2013.koreasme.com.
- ***Dentaurum, Ispringen, Germany; www.dentaurum.de.
- †Registered trademark of TP Orthodontics, Inc., LaPorte, IN; www.tportho.com.
- ‡Registered trademark of Ormco Corporation, Brea, CA; www.ormco.com.
- ††Reliance Orthodontics, Inc., Itasca, IL; www.relianceorthodontics.com.
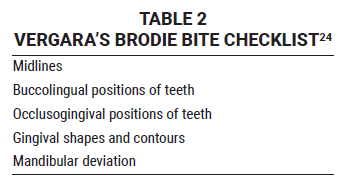
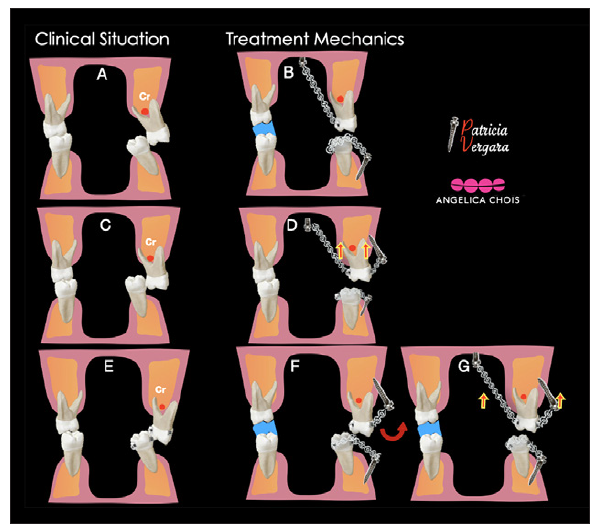
Fig. 12 Possible Brodie bite scenarios in upper arch. A. Scenario 1: Extruded and buccally inclined upper segment. B. Mechanics: Palatal TAD in high midline position for upper intrusion and palatal movement. C. Scenario 2: Straight upper extrusion. D. Mechanics: Palatal and buccal infrazygomatic TADs for straight, bodily upper intrusion. E. Scenario 3: Extruded and lingually inclined upper segment. F. Stage 1 mechanics: Buccal infrazygomatic TAD used to upright tooth. G. Stage 2 mechanics: Palatal TAD added for intrusive mechanics.
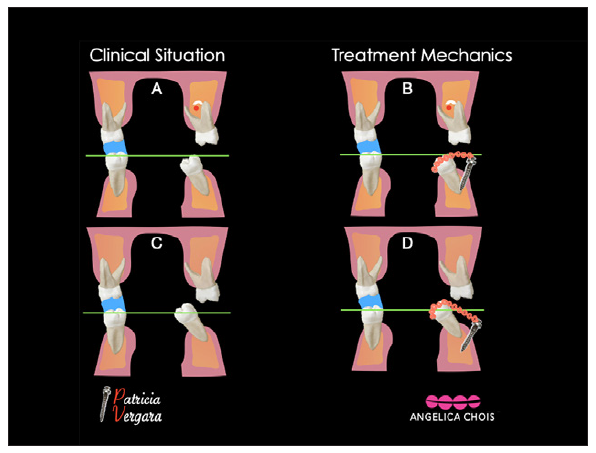
Fig. 13 Possible Brodie bite scenarios in lower arch. A. Scenario 1: Lower segment lingually inclined but not extruded. B. Mechanics: Head of TAD located at wire or occlusal level. C. Scenario 2: Lower segment lingually inclined and extruded. D. Mechanics: Head of TAD located below center of resistance.
REFERENCES
- 1. Nojima, K.; Takaku, S.; Murase, C.; Nishii, Y.; and Sueishi, K.: A case report of bilateral Brodie bite in early mixed dentition using bonded constriction quad-helix appliance, Bull. Tokyo Dent. Coll. 52:39-46, 2011.
- 2. Deffrennes, G. and Deffrennes, D.: Management of Brodie bite: Note on surgical treatment, Int. Orthod. 15:640-676, 2017.
- 3. Kim, K.A.; Yu, J.J.; Chen, Y.; Kim, S.J.; Kim, S.H.; and Nelson, G.: Surgery versus nonsurgery option for scissors bite treatment, J. Craniofac. Surg. 26:726-729, 2015.
- 4. Brodie, A.G.: Consideration of musculature in diagnosis, treatment, and retention, Am. J. Orthod. 38:823-835, 1952.
- 5. Sebbag, M. and Cavaré, A.: Treatment of Brodie syndrome, J. Dentofac. Anom. Orthod. 20:109-134, 2017.
- 6. Ramsay, D.S.; Wallen, T.R.; and Bloomquist, D.S.: Case report MM: Surgical-orthodontic correction of bilateral buccal crossbite (Brodie syndrome), Angle Orthod. 60:305-311, 1990.
- 7. Keski-Nisula, K.; Lehto, R.; Lusa, V.; Keski-Nisula, L.; and Varrela, J.: Occurrence of malocclusion and need of orthodontic treatment in early mixed dentition, Am. J. Orthod. 124:631-638, 2003.
- 8. Lee, S.A.; Chang, C.C.H.; and Roberts, W.E.: Severe unilateral scissors-bite with a constricted mandibular arch: Bite turbos and extra-alveolar bone screws in the infrazygomatic crests and mandibular buccal shelf, Am. J. Orthod. 154:554-569, 2018.
- 9. Simsuchin, C.; Chen, Y.; Huang, S.; Mallineni, S.K.; Zhao, Z.; Hagg, U.; and McGrath, C.: Unilateral scissor bite managed with prefabricated functional appliances in primary dentition: A new interceptive orthodontic protocol, Children (Basel) 8:957, 2021.
- 10. Song, G.; Chen, H.; and Xu, T.: Nonsurgical treatment of Brodie bite assisted by 3-dimensional planning and assessment, Am. J. Orthod. 154:421-432, 2018.
- 11. Chandorikar, H.; Nagrik, A.; Bhad, W.A.; Chavan, S.J.; and Doshi, U.H.: Early correction of unilateral scissor bite using transforce appliance and modified twin block appliance, J. Orthod. Sci. 6:76-80, 2017.
- 12. Jung, M.H.: Treatment of severe scissor bite in a middle-aged adult patient with orthodontic mini-implants, Am. J. Orthod. patient with orthodontic mini-implants, Am. J. Orthod.
- 13. Jarabak, J.R. and Fizzell, J.A.: Technique and Treatment with Light-Wire Edgewise Appliances, vol. 2, Mosby, St. Louis, 1972.
- 14. Björk, A.: Prediction of mandibular growth rotation, Am. J. Orthod. 55:585-599, 1969.
- 15. Tamburrino, R.K.; Boucher, N.S.; Vanarsdall, R.L.; and Secchi, A.G.: The transverse dimension: Diagnosis and relevance to functional occlusion, RWISO J. 2:11-20, 2010.
- 16. Andrews, L.F.: The six elements of orofacial harmony, Andrews J. Orthod. Orofac. Harmony 1:13-22, 2000.
- 17. Baik, U.B.; Kim, Y.; Sugawara, J.; Hong, C.; and Park, J.H.: Correcting severe scissor bite in an adult, Am. J. Orthod. 156:113-124, 2019.
- 18. Li, H.; Wang, Q.; and Wu, T.: Nonsurgical treatment of unilateral scissor bite in a growing patient, J. Clin. Orthod. 48:249-255, 2014.
- 19. Jussila, P.; Krooks, L.; Näpänkangas, R.; Päkkilä, J.; Lähdesmäki, R.; Pirttiniemi, P.; and Raustia, A.: The role of occlusion in temporomandibular disorders (TMD) in the Northern Finland Birth Cohort (NFBC) 1966, Cranio 37:231-237, 2019.
- 20. Weinstein, C.; Hirschhaut, M.; Vergara, P.; de la Hoz Chois, A.; and Flores-Mir, C.: A three-dimensional perspective on Brodie Bite's diagnosis, planning, treatment alternatives, and complications, Semin. Orthod. 30:538-556, 2024.
- 21. Chen, B.; Chang, C.H.; and Roberts, E.: Simple solution for Brodie bite with skeletal Class II asymmetry, J. Dig. Orthod. 62:4-23, 2021.
- 22. Thurzo, A.; Urbanová, W.; Novák, B.; Waczulíková, I.; and Varga, I.: Utilization of a 3D printed orthodontic distalizer for tooth-borne hybrid treatment in Class II unilateral malocclusions, Mater. (Basel) 15:1740, 2022.
- 23. Araujo, E. and Tanaka, O.M.: The Brodie bite: Addressing a confounding orthodontic problem, AJO-DO Clin. Compan. 1:232-244, 2021.
- 24. Shimazaki, K.; Otsubo, K.; Yonemitsu, I.; Kimizuka, S.; Omura, S.; and Ono, T.: Severe unilateral scissor bite and bimaxillary protrusion treated by horseshoe Le Fort I osteotomy combined with mid-alveolar osteotomy, Angle Orthod. 84:374-379, 2014.





COMMENTS
.