CASE REPORT
Orthodontic Treatment of a Patient after Removal of a Dentigerous Cyst and Supernumeraries
The etiology of malocclusions includes a number of endogenous or exogenous factors,1 intrinsic or extrinsic factors,2 and genetic or environmental factors.3 Among the potential environmental causes are cysts or tumors,4,5 of which radicular cysts are the most common (42.9%), followed by dentigerous (also known as follicular) cysts (39%).6
Dentigerous cysts have a prevalence between .91% and 7.3%7,8 and are found more frequently in male than in female patients.9 They are most often associated with the third molars, upper canines, and lower premolars.10 In about 5.5% of cases,11 mostly involving the anterior region of the maxilla,12,13 dentigerous cysts are associated with supernumerary teeth.
Supernumeraries have an overall prevalence of 2.6% and are more common in the maxillary arch than in the mandibular arch.14 Their etiology is unknown, although both environmental and genetic factors are believed to be involved.10,15 In about 43% of cases, the presence of supernumerary teeth will delay or prevent eruption of the associated permanent incisors.14 Crowding and ectopic eruption are other potential consequences,16 with such complications typically caused by the supernumerary teeth themselves rather than any associated cysts.17
Although the standard treatment protocol involves surgical removal of the supernumeraries and cysts, further surgical intervention is required in a reported 30-54% of these cases to assist in the eruption of affected permanent teeth.10,17,18 After surgical exposure of a permanent tooth, the two treatment options are to bond an orthodontic accessory for forced eruption19 or to monitor the tooth as it spontaneously erupts.19,20
This case report describes an extended multidisciplinary approach to the orthodontic treatment of a patient with a horizontally impacted lateral incisor caused by previously removed supernumeraries and a dentigerous cyst.
Diagnosis and Treatment Plan
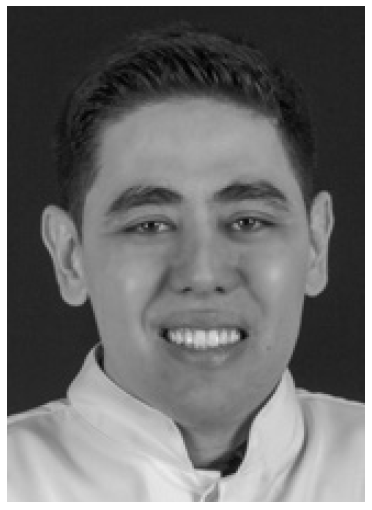
A 12-year-old male presented for orthodontic treatment. The parents reported that the patient had undergone surgery at age 6 to remove supernumerary teeth and a dentigerous cyst. Clinical examination found a mesofacial growth pattern with harmonious facial thirds and a passive lip seal (Fig. 1). The profile was slightly convex, with a slightly acute nasolabial angle. A mild projection was observed in the labial region, with the upper lip slightly more prominent than the lower lip. The patient exhibited a Class II, division 2 malocclusion and a unilateral right posterior crossbite. The upper left lateral incisor was not clinically visible, and the adjacent canine had migrated mesially into the lateral-incisor space.
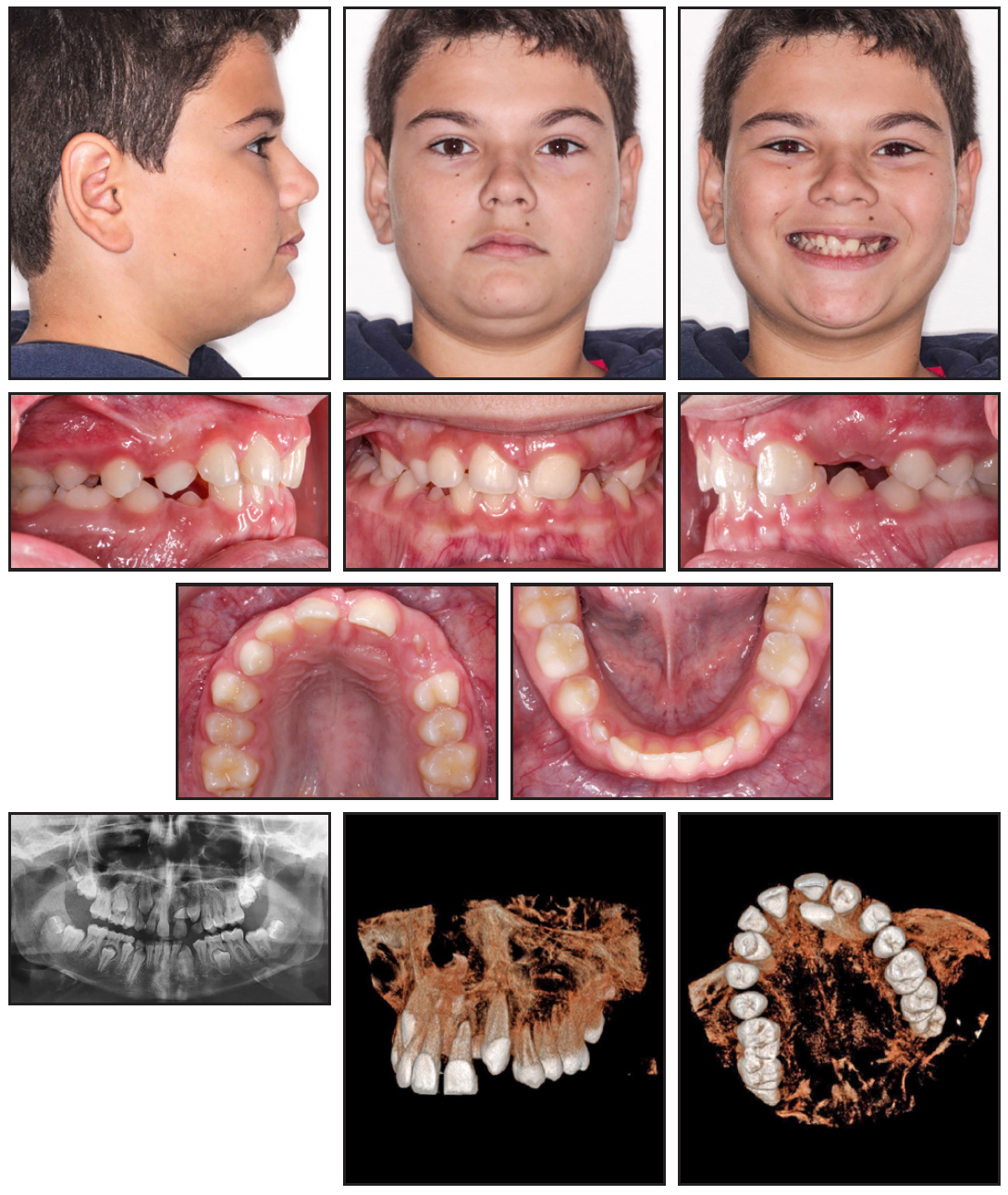
Fig. 1 12-year-old male patient with Class II, division 2 malocclusion, unilateral right posterior crossbite, and horizontally impacted upper left lateral incisor caused by previously removed dentigerous cyst and supernumeraries.
The panoramic radiograph showed that all teeth were present and that the upper left lateral incisor was horizontally impacted. Cone-beam computed tomography (CBCT) confirmed the horizontal position of the upper left lateral incisor and the proximity of its crown to the middle thirds of the upper left central incisor and canine.
The parents provided CBCT scans that were taken before the earlier surgery. In these records, two supernumeraries were visible in the upper-incisor region, one of which was associated with a dentigerous cyst (Fig. 2). The lesions were apparently responsible for the delay and deviation in the eruption of the upper right central and lateral incisors and the impaction of the upper left lateral incisor.
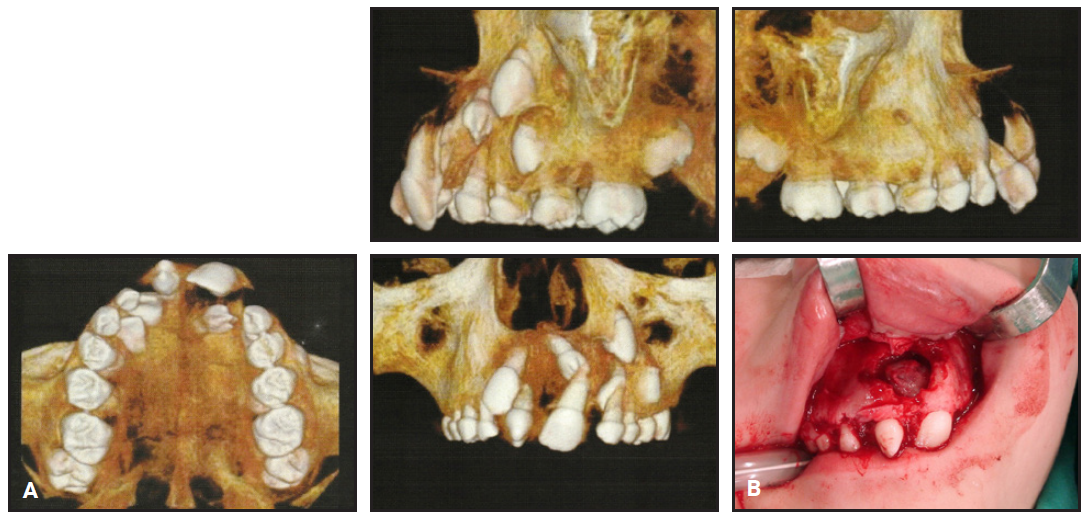
Fig. 2 Previous surgery performed at age 6. A. Presurgical cone-beam computed tomography scans. B. Surgery to remove dentigerous cyst and supernumeraries. (Image courtesy of Dr. Fernando Giovanella.)
Since the patient was still in the second transitional phase of the mixed dentition, a two-stage treatment was proposed. The objective for the first stage was to open space for eruption of the impacted upper left lateral incisor, using a fixed appliance. After surgical exposure of the incisor crown, either an orthodontic accessory would be bonded to the tooth for forced eruption, or the tooth would be allowed to erupt spontaneously. After an explanation of the advantages and disadvantages of each alternative, the patient and parents opted for natural eruption. The second stage of treatment would begin once the permanent dentition had fully emerged. Objectives for this stage were to correct the Class II malocclusion and crossbite, as well as to improve the appearance of the smile.
Treatment Progress
The upper permanent teeth were bonded with MBT*-prescription .022" × .028" brackets for the first stage of treatment. Leveling and alignment were performed with a series of nickel titanium (.014", .016", .018", and .020") and stainless steel (.017" × .025") archwires. After six months of treatment, an open nickel titanium spring was attached to the stainless steel wire to open space for the upper left lateral incisor (Fig. 3). The active treatment time for this stage was eight months.
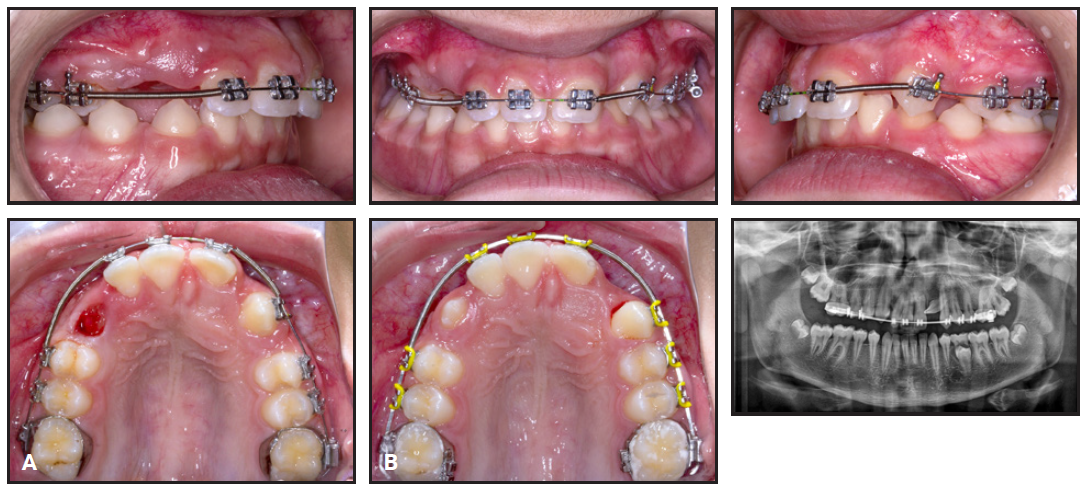
Fig. 3 A. After six months of treatment. B. After 10 months of treatment.
After eleven months, the brackets were removed, and the patient was referred for surgery to expose the crown of the upper left lateral incisor. A button was bonded in case traction would be required. Gingivectomies of the anterior teeth and an upper labial frenectomy were performed at the same time. Monthly appointments were scheduled to monitor the spontaneous eruption of the tooth (Fig. 4).
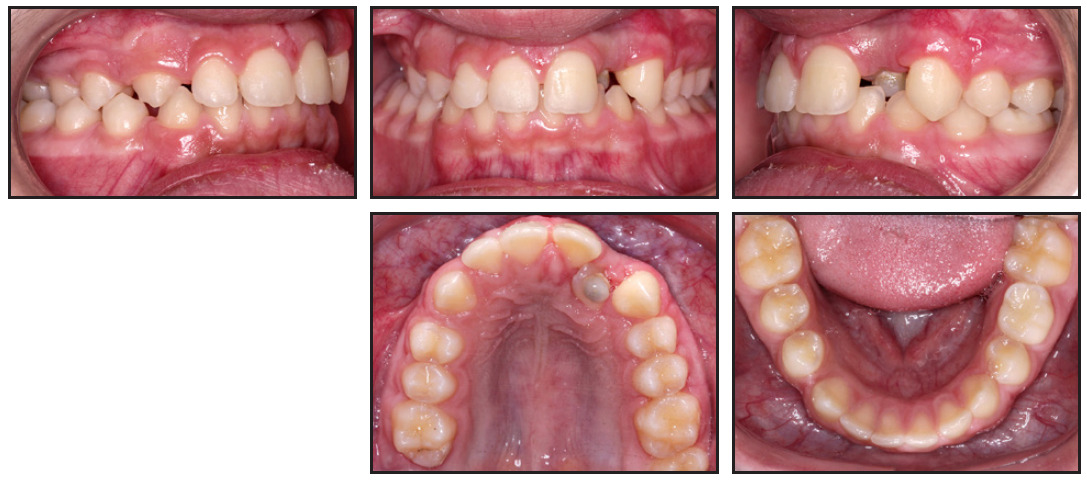
Fig. 4 After one year of treatment, showing results of surgical exposure of upper left lateral incisor.
After another five months, when the permanent dentition was complete, the profile had become less convex, while the mesofacial vertical pattern was preserved (Fig. 5). A half-step Class II, division 2 subdivision malocclusion with a mandibular midline deviation to the left was observed, along with a unilateral crossbite on the right. The panoramic radiograph showed significant improvement in the position of the upper left lateral incisor, which was now vertically oriented. During the second stage of treatment, the upper left lateral incisor would be guided into the arch, and intermaxillary elastics would be used to correct the Class II malocclusion and posterior crossbite.
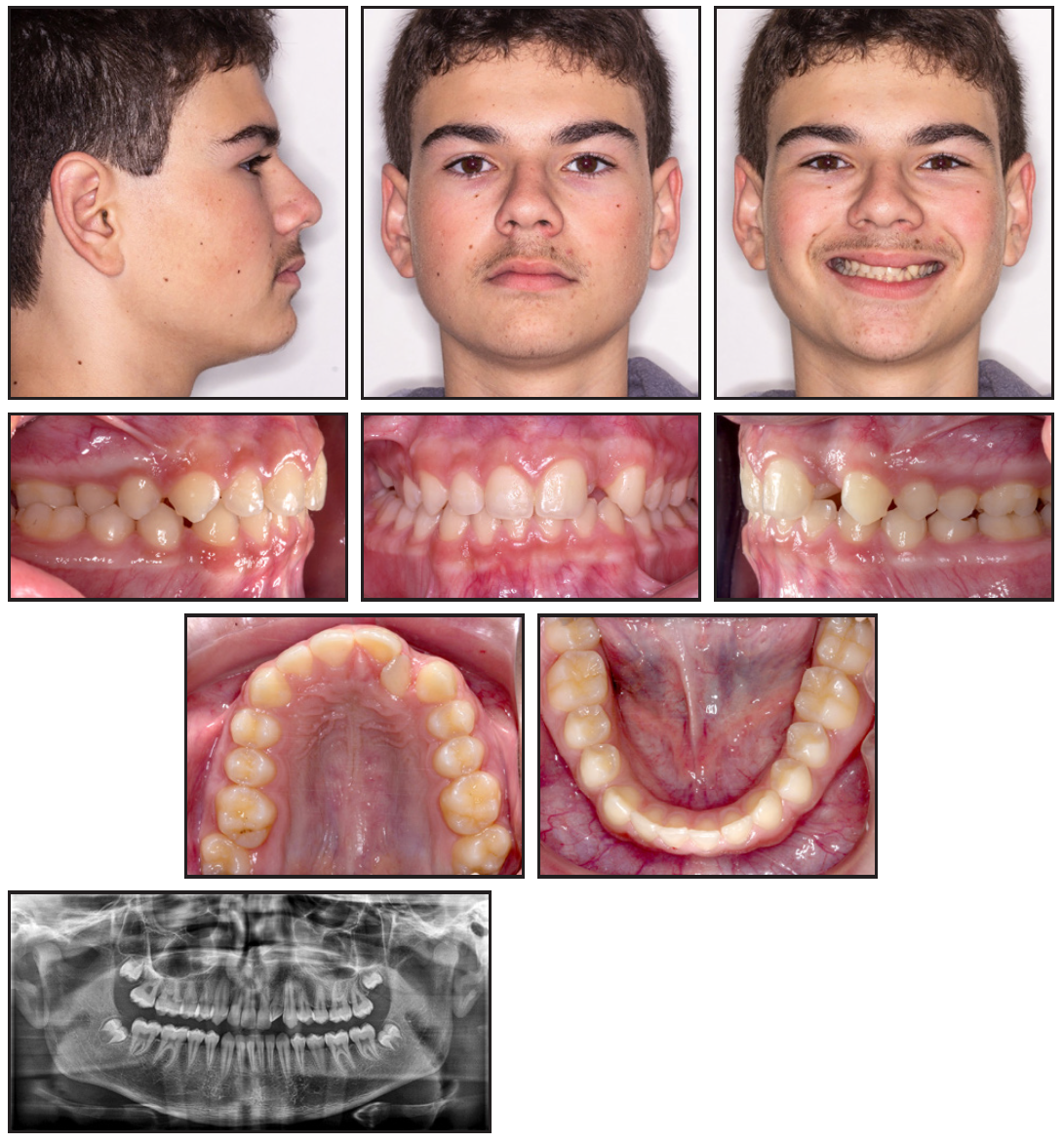
Fig. 5 Before second stage, 16 months after beginning of treatment.
All teeth except the upper left lateral incisor were bonded with MBT-prescription .022" × .028" brackets, and progressively larger nickel titanium archwires (.014", .016", .018", and .020") were used for leveling and alignment (Fig. 6A). In the lower arch, reverse curves were added to .020" and then .017" × .025" stainless steel archwires to correct the curve of Spee.
After seven months, an .019" × .025" stainless steel wire was placed in the upper arch. A nickel titanium spring was added to open space for traction of the upper left lateral incisor, and orthodontic accessories were bonded to create a binary force that would correct its rotation (Fig. 6B).
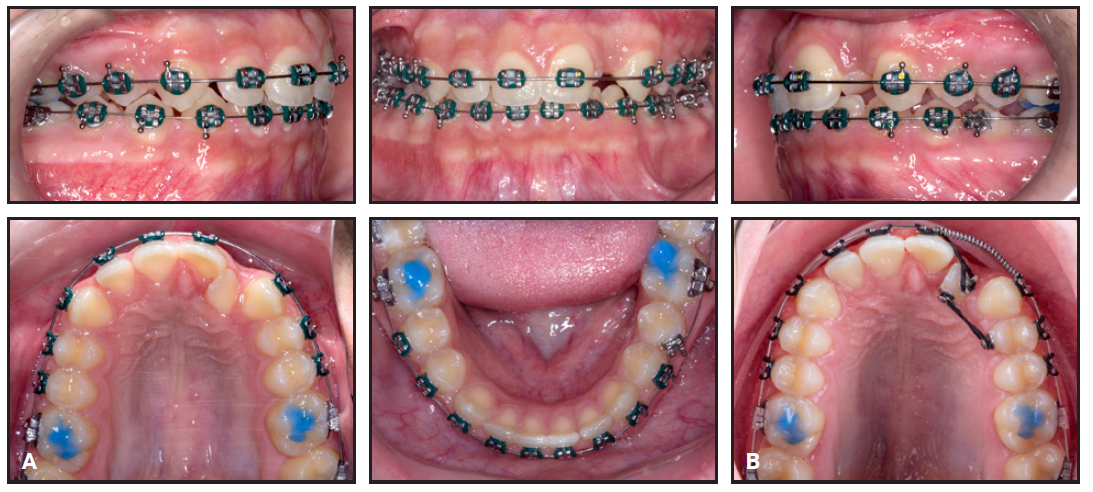
Fig. 6 A. Two months into second stage of treatment. B. Seven months into second stage.
Three months later, the upper left lateral incisor was bonded with a bracket that was inverted 180° to promote buccal root torque during buccal traction,21,22 and the same sequence of nickel titanium archwires was repeated. In the lower arch, correction of the curve of Spee was complete after another two months, and the archwire was changed to .019" × .025" stainless steel; three months later, the final .019" × .025" stainless steel wire was inserted in the upper arch (Fig. 7).
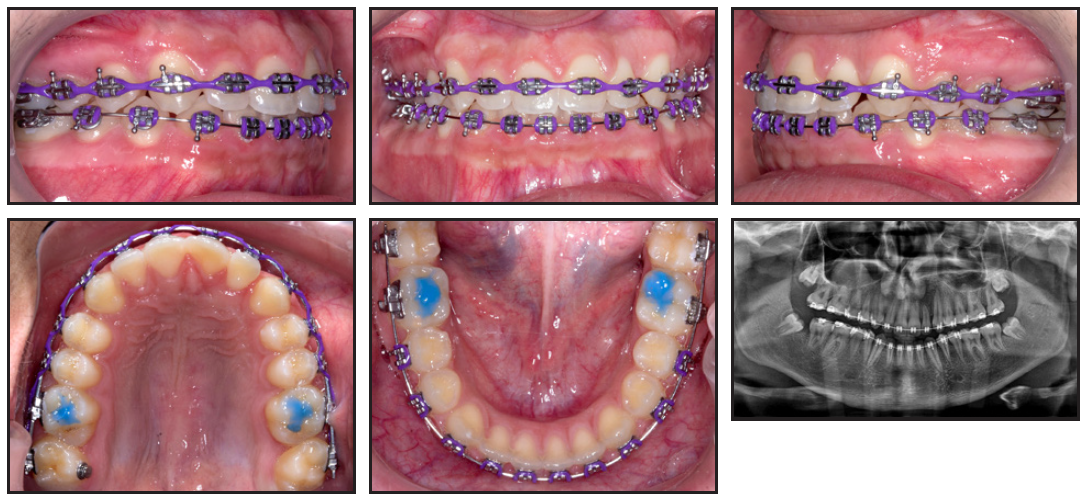
Fig. 7 18 months into second stage of treatment.
For the remainder of treatment, Class II elastics (3⁄16", 4.5oz) were worn on the left side; vertical elastics (3⁄16", 4.5oz) were worn between the upper
and lower right second premolars, first molars, and second molars to address the crossbite. Once the sagittal and transverse relationships were corrected, a finishing stage was begun using rebonded brackets and intercuspation elastics (3⁄16", 2.5oz). The total treatment time for the second stage was 24 months.
Treatment Results
The treatment duration for both stages was 40 months, including the eight months of waiting for eruption of the permanent teeth. The nasolabial angle and the relationship between the upper and lower lips were slightly improved, enhancing facial harmony (Fig. 8). The midline deviation was corrected, and bilateral Class I molar and canine relationships were achieved. The patient’s periodontal health was considered good, even in the soft and hard tissues adjacent to the upper left lateral incisor. Adequate root parallelism was achieved, although the impacted tooth lost some root integrity. Mild root resorption of the upper right central incisor was noted, consistent with remodeling in response to tooth movement.23
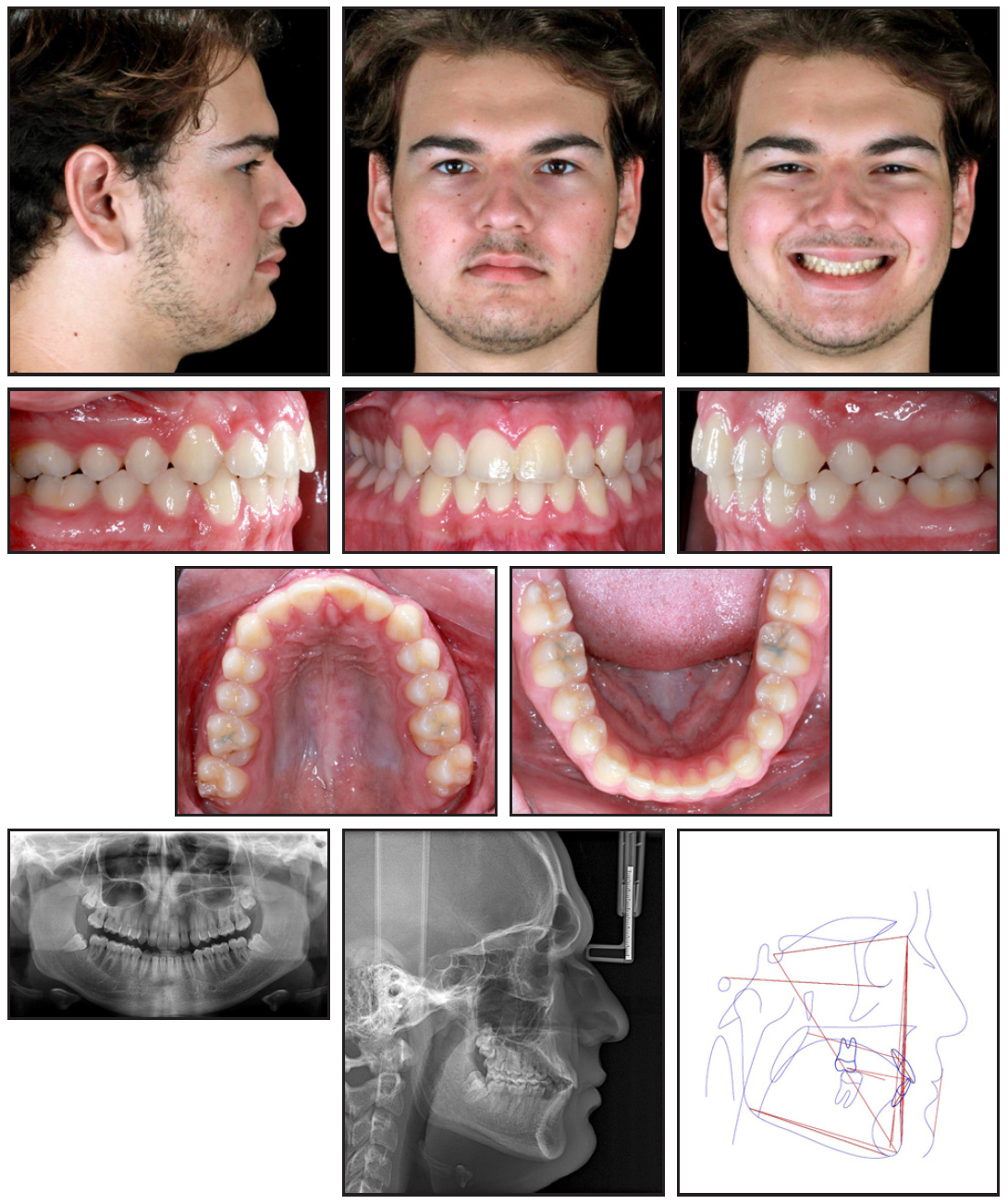
Fig. 8 Patient after 40 months of treatment, showing well-aligned teeth and improved facial harmony.
Discussion
Uncommon conditions that require invasive treatment can create significant psychosocial challenges in young patients, including dissatisfaction with their facial appearance and medical trauma from multiple surgeries. School bullying is a particularly common stressor for adolescents between the ages of 12 and 14, with consequent effects on self-image.24 Diastemas, missing or discolored teeth, and prominent anterior teeth are the three most common dental conditions associated with bullying of children.24 As a result, esthetic concerns that adults might consider secondary can severely diminish a child’s quality of life.25
In the present case, the previously removed cyst and supernumerary teeth had delayed the eruption of the upper left lateral incisor, producing a large diastema that affected the patient’s self-image. To address this concern and lessen the emotional impact of treatment, we chose the conservative open exposure approach often used for impacted canines, in which space is created for the impacted tooth, which is then exposed and allowed to erupt naturally.16,26
To meet the patient’s individual needs, we customized the torque of the bracket on the upper left lateral incisor, as several authors have suggested.27,28 After the rotation of the upper left lateral incisor was corrected, the tooth’s root was palatally displaced. Therefore, we inverted the bracket 180° to change the torque from +10° to –10°. The adjustment produced 10° of lingual crown torque and, consequently, buccal root torque, counteracting the undesirable moment by applying a force below the center of resistance. Further torque adjustments can be made if needed, but in this case, the inverted bracket produced the desired result.
FOOTNOTES
- *Registered trademark of Solventum, St. Paul, MN; www.solventum.com.
REFERENCES
- 1. Korkhaus, G.: Biomechanische Gebiss- und Kieferorthopädie (Orthodontie), in Gebiss-, Kiefer- und Gesichtsorthopädie [in German], ed. C. Bruhn, H. Hofrath, and G. Korkhaus, Springer Berlin, Heidelberg, Germany, 1939, pp. 140-742.
- 2. Graber, T.M.: Orthodontics: Principles and Practice, 3rd ed., W.B. Saunders Co., Philadelphia, 1972.
- 3. Salzmann, J.A.: Orthodontics in Daily Practice, Lippincott, Philadelphia, 1974.
- 4. Garib, D.G.; da Silva Filho, O.G.; and Janson, G.: Etiology of malocclusions: Clinical perspective, Part I: Genetic factors [in Portuguese], Dent. Press J. Orthod. 9:77-97, 2010.
- 5. Garib, D.G.; da Silva Filho, O.G.; and Janson, G.: Etiology of malocclusions: Clinical perspective, Part II: Environmental factors [in Portuguese], Dent. Press J. Orthod. 9:61-73, 2010.
- 6. Garg, R.K.; O’Connor, M.K.; Sterling, D.A.; Jacob, L.; Hammoudeh, J.A.; and Andrews, B.T.: Pediatric odontogenic and maxillofacial bone pathology: A global analysis, J. Craniofac. Surg. 33:870-874, 2022.
- 7. Açikgöz, A.; Uzun-Bulut, E.; Özden, B.; and Gündüz, K.: Prevalence and distribution of odontogenic and nonodontogenic cysts in a Turkish population, Med. Oral. Patol. Oral Cir. Bucal. 17:e108-e115, 2012.
- 8. Johnson, N.R.; Gannon, O.M.; Savage, N.W.; and Batstone, M.D.: Frequency of odontogenic cysts and tumors: A systematic review, J. Investig. Clin. Dent. 5:9-14, 2014.
- 9. Anthonappa, R.P.; Ekambaram, M.; Neboda, C.N.G.; King, N.M.; and Rabie, A.B.M.: Genetic basis of dentigerous cysts associated with supernumerary teeth: A narrative review, J. Investig. Clin. Dent. 9, 2018.
- 10. Shah, K.M.; Karagir, A.; Adaki, S.; and Pattanshetti, C.: Dentigerous cyst associated with an impacted anterior maxillary supernumerary tooth, BMJ Case Rep. 31, 2013.
- 11. Padha, K.; Harsha, M.P.; and Dilesh, P.K.: A dentigerous cyst arising from an ectopic supernumerary tooth lodged in the posterolateral wall of the maxillary sinus: A rare case report and treatment modality, Ind. J. Otolaryngol. Head Neck Surg. 74:4628-4631, 2022.
- 12. Datli, A.; Pilanci, O.; Cortuk, O.; Saglam, O.; and Kuvat, S.V.: Ectopic tooth superiorly located in the maxillary sinus, J. Craniofac. Surg. 25:1927-1928, 2014.
- 13. Chagas Júnior, O.L.; Moura, L.B.; Sonego, C.L.; de Farias, E.O.; Giongo, C.C.; and Fonseca, A.A.: Unusual case of sinusitis related to ectopic teeth in the maxillary sinus roof/orbital floor: A report, Craniomaxillofac. Trauma Reconstr. 9:260-263, 2016.
- 14. Di Biase, D.D.: Midline supernumeraries and eruption of the maxillary central incisor, Dent. Pract. Dent. Rec. 20:35-40, 1969.
- 15. Hou, L.; Acharya, K.; Ghimire, B.; Kasula, D.; Haque, I.B.; Lamichhane, N.S.; Li, L.; and Hu, X.Y.: Clinical and imaging analysis of 22 cases of supernumerary teeth in the mandibular region, J. Stomatol. Oral Maxillofac. Surg. 2:101525, 2023.
- 16. Seehra, J.; Yaqoob, O.; Patel, S.; O’Neill, J.; Bryant, C.; and Noar, J.: National clinical guidelines for the management of unerupted maxillary incisors in children, Br. Dent. J. 224:779-785, 2018.
- 17. Seehra, J.; Mortaja, K.; Wazwaz, F.; Papageorgiou, S.N.; Newton, J.T.; and Cobourne, M.T.: Interventions to facilitate the successful eruption of impacted maxillary incisor teeth due to the presence of a supernumerary: A systematic review and meta-analysis, Am. J. Orthod. 163:594-608, 2023.
- 18. Fujii, R.; Kawakami, M.; Hyomoto, M.; Ishida, J.; and Kirita, T.: Panoramic findings for predicting eruption of mandibular premolars associated with dentigerous cyst after marsupialization, J. Oral Maxillofac. Surg. 66:272-276, 2008.
- 19. Nahajowski, M.; Hnitecka, S.; Antoszewska-Smith, J.; Rumin, K.; Dubowik, M.; and Sarul, M.: Factors influencing an eruption of teeth associated with a dentigerous cyst: A systematic review and meta-analysis, BMC Oral Health 21:180, 2021.
- 20. Kokich, V.G.: Surgical and orthodontic management of impacted maxillary canines, Am. J. Orthod. 126:278-283, 2004.
- 21. McLaughlin, R.; Bennet, J.; and Trevisi, H.: A clinical review of the MBT orthodontic treatment program, Orthod. Perspectives 4:3-12, 1997.
- 22. Capelozza Filho, L,. Silva Filho, O.G.; Ozawa, T.O.; and Cavassan, A.O.: Individualization of brackets in the straightwire technique: Review of concepts and suggested indications for use [in Portuguese], Dent. Press J. Orthod. 4:87-106, 1999.
- 23. Consolaro, A. and Consolaro, M.F.M.O.: Controversies in orthodontics and atlas of tooth movement biology, Maringá Dent. Press, 2008.
- 24. Al-Bitar, Z.B.; Sonbol, H.N.; Al-Omari, I.K.; Badran, S.A.; Naini, F.B.; Al-Omiri, M.K.; and Hamdan, A.M.: Self-harm, dentofacial features, and bullying, Am. J. Orthod. 162:80-92, 2022.
- 25. Fantini, L.C.; Carneiro, D.P.A.; Venezian, G.C.; de Menezes, C.C.; Vedovello, S.A.S.; and Vedovello Filho, M.: What factors are associated with health-related quality of life in mixed dentition children? Pesqui. Bras. Odontopediat. Clin. Integr. 22:210157, 2022.
- 26. Björksved, M.; Arnrup, K.; Lindsten, R.; Magnusson, A.; Sundell, A.L.; Gustafsson, A.; and Bazargani, F.: Closed vs open surgical exposure of palatally displaced canines: Surgery time, postoperative complications, and patients’ perceptions: A multicentre, randomized, controlled trial, Eur. J. Orthod. 40:626-635, 2018.
- 27. Johnson, E.: Selecting custom torque prescriptions for the straight-wire appliance, Am. J .Orthod. 143:161-167, 2013.
- 28. Pour, R.D.; Papageorgiou, S.N.; Safi, S.; Eble, O.S.; Jäger, A.; and Gölz, L.: Clinical implementation of axial angulation of incisors in the course of routine fixed appliance treatment: A retrospective cohort study, Clin. Oral Investig. 27:659-669, 2023.







COMMENTS
.