CASE REPORT
Management of a Large Dentigerous Cyst in the Mixed Dentition
Dentigerous cysts, also termed follicular cysts, are the most common type of odontogenic cysts associated with impacted, embedded, or unerupted teeth.1,2
Two types of dentigerous cysts are reported in the literature: the developmental type, resulting in fluid accumulation from a mature tooth, and the inflammatory type, developing in an immature permanent tooth as a result of a spread of inflammation from an overlying nonvital deciduous tooth.3
Usually, a dentigerous cyst is solitary, slow-growing, and asymptomatic, discovered in the course of routine radiographic examination to identify a missing tooth.4 Radiographically, the cyst presents as a well-defined unilocular radiolucency surrounding the crown of an unerupted tooth.3,4 Since cysts can attain considerable size with minimal or no symptoms, early detection and treatment are important to reduce morbidity.4 Dentigerous cysts can be treated either by complete surgical enucleation, with or without peripheral ostectomy, or marsupialization.5
Surgical enucleation is considered an aggressive treatment modality because it generally requires the complete removal of the tooth buds.2 Marsupialization is a more conservative treatment for a large cyst in which a pouch-like surgical cavity on the wall of the cyst is incised and, consequently, the contents of the cyst are emptied and the continuity between the cyst and oral cavity is maintained. After marsupialization, the impacted teeth may erupt spontaneously if their root formation is incomplete and sufficient space exists.2
This case report describes the management of a large, severe inflammatory dentigerous cyst caused by long-term inflammation and infection of a maxillary deciduous central incisor. The nonextraction treatment involved an interdisciplinary approach: conservative surgical decompression of the cyst and orthodontic recovery of the impacted teeth.6
Diagnosis and Treatment Plan
A 9-year-old male presented to the Department of Orthodontics of the University of Rome “Tor Vergata” for evaluation. The chief complaint was an eruption disturbance resulting in an unesthetic appearance. The parent referred to a trauma to the maxillary deciduous incisors that had occurred when the child was 4, inducing necrosis of the left central incisor. On extraoral examination, the patient had a balanced facial pattern with a convex profile and an asymmetrical smile (Fig. 1).
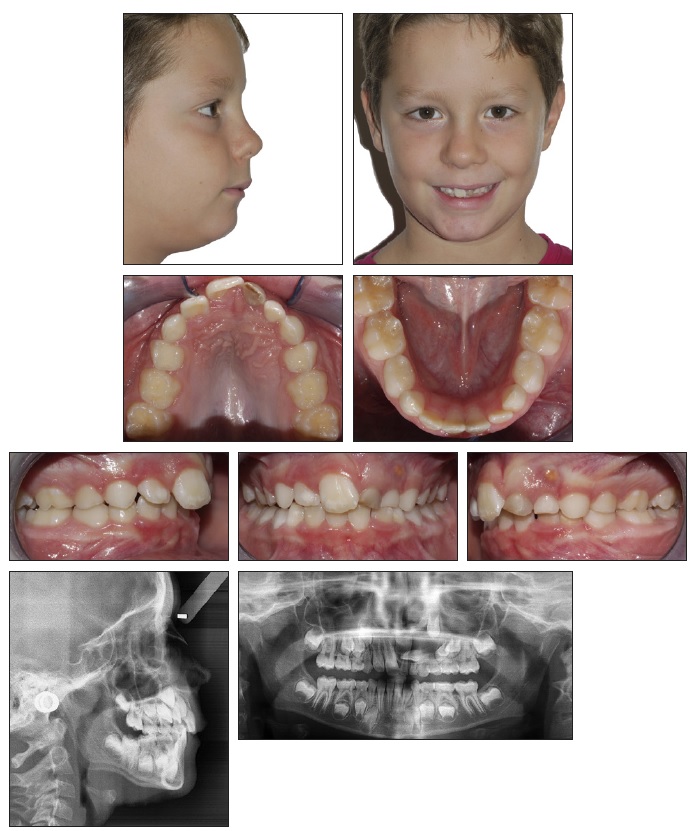
Fig. 1 9-year-old male patient with altered sequence of eruption and buccal swelling from upper left deciduous central incisor to lateral incisor before treatment.
Intraoral clinical examination showed an early mixed dentition stage with an altered sequence of eruption, the absence of the maxillary permanent left central and lateral incisors, and necrosis of the maxillary deciduous left central incisor. A painless buccal swelling extended from the mesial of the maxillary deciduous left central incisor to the distal of the deciduous left lateral incisor, with a buccal fistula due to the nonvital deciduous tooth. Occlusal analysis found a Class II molar and canine relationship on the right side and a Class I molar and canine relationship on the left side. The upper arch was narrow, and there was minor dental crowding in the lower arch, with normal overjet and overbite.
The panoramic radiograph revealed the presence of a well-defined unilocular radiolucent area, characterized by a sclerotic border in relation to the roots of the maxillary left deciduous incisors and canines, surrounding the crowns of the maxillary permanent left central and lateral incisors.
The central incisor was displaced near the nasal floor. It had a shorter root than the contralateral tooth, and its root growth seemed blocked between the cyst, the bud of the lateral incisor, and the palatal plane. The lateral incisor was displaced in the horizontal plane, almost parallel to the occlusal plane. The permanent left canine bud presented a severe displacement in the vertical plane, with an increased distance from the occlusal plane compared with the contralateral canine. A distal displacement of the first maxillary premolar bud was also evident.
Cephalometric analysis (Table 1) indicated a skeletal Class II malocclusion (ANB = 7°) in a hyperdivergent pattern (FMA = 30°). The lower incisor showed a lingual inclination in the mandibular plane (IMPA = 84°). Cone-beam computed tomography (CBCT) confirmed the presence of the cyst involving the maxillary left permanent incisors and canine, extending on the buccal and lingual sides (Fig. 2).
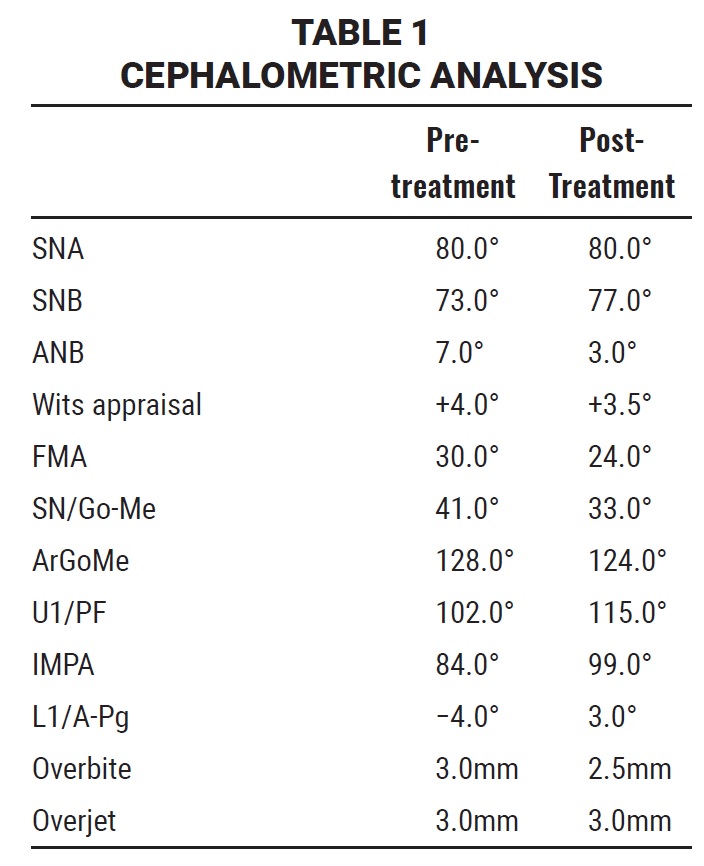
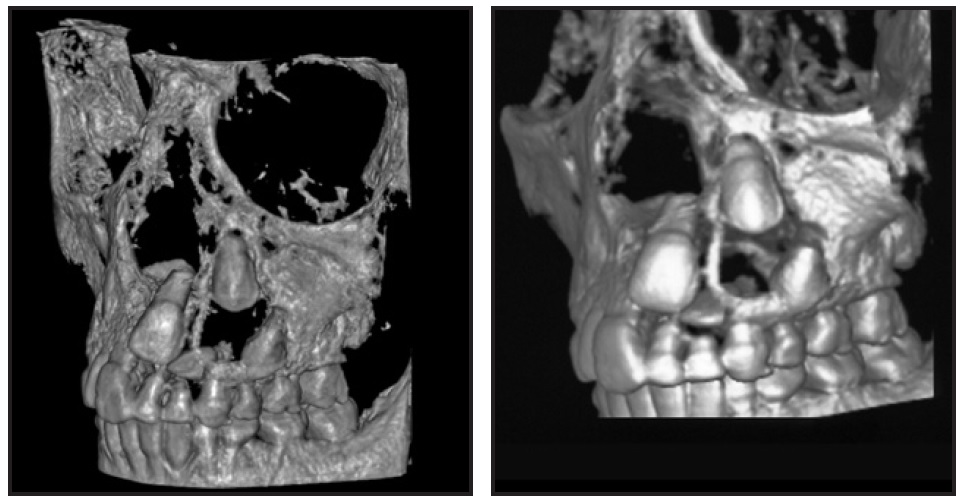
Fig. 2 Cone-beam computed tomography (CBCT) confirms presence of cyst involving upper left permanent incisors and canine.
The following treatment objectives were established: treat the cyst, using a less aggressive technique to create new bone in the defect; remove any inflammation to prevent recurrence of cyst formation; conserve the teeth affected by the dentigerous cyst and maintain their pulp vitality; recover space in the maxillary arch for spontaneous eruption of the permanent left central and lateral incisors; create a stable functional occlusion; and establish adequate attached gingiva and symmetrical gingival margins for the anterior teeth.
Treatment alternatives included extraction of the maxillary deciduous incisors, complete enucleation of the cyst, extraction of the maxillary permanent left lateral incisor, and restoration with a bridge or an implant after the cessation of growth7; extraction of the maxillary deciduous incisors, marsupialization of the cyst, and orthodontic traction of the impacted teeth into their proper positions7; and extraction of the maxillary deciduous incisors, marsupialization of the cyst, and interceptive orthopedic and orthodontic treatment involving rapid maxillary expansion, cervical headgear, and fixed appliances to recover space for the impacted teeth and allow their spontaneous eruption and alignment in the dental arch. After discussing the alternatives, the orthodontist and surgeon chose the last treatment option.
Treatment Progress
The multi-disciplinary approach involved surgical-orthodontic treatment. First, the patient was treated by marsupialization under local anesthesia (Fig. 3).
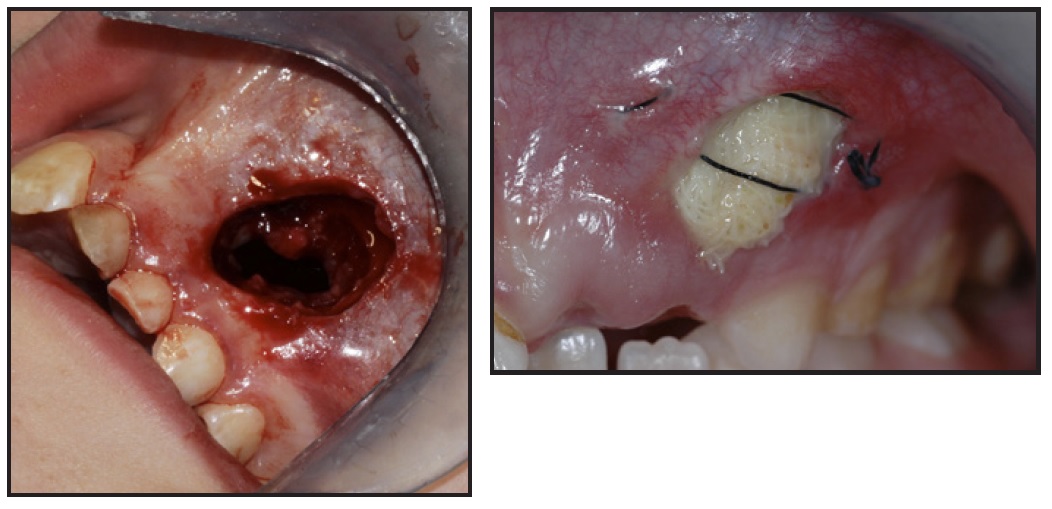
Fig. 3 Marsupialization of cyst.
An accessory cavity was created within the cyst’s bony wall, which led to the opening of the cavity, and the cystic lining was sutured to the oral mucosa. This formed a pouch connecting the oral and cystic cavities. A thick, brown-colored fluid was drained during the procedure.3
Care was taken to avoid disturbing the developing tooth buds and to preserve the maxillary bone. The excised tissue was sent out for a biopsy to confirm the histopathologic diagnosis of an inflammatory dentigerous cyst. An anti-inflammatory gauze iodoform pack was inserted into the cyst cavity to keep it open. Finally, the deciduous left central and lateral incisors were extracted. The gauze pack was replaced every two weeks, taking care to avoid damaging the buds of the impacted teeth.
A five-month follow-up examination revealed the clinical presence of the upper left permanent central incisor, which was erupting spontaneously in an ectopic position (Fig. 4). A panoramic radiograph was performed six months after removal of the cyst to assess the progress of healing and eruption of the impacted teeth. This showed an improvement in the intraosseus position of the upper left central incisor and canine, while that of the upper left lateral incisor seemed to be worsening (Fig. 5).

Fig. 4 Spontaneous eruption of upper left permanent central incisor after surgical removal of cyst.

Fig. 5 Six months after cyst removal, showing improved positions of upper left central incisor and canine and worsening position of upper left lateral incisor.
Palatal expansion would allow correction of the interarch relationship so as to improve the dental alignment and the intraosseous positions of the lateral incisor and canine. A modified rapid maxillary expander*8 was designed with an .028" chrome cobalt Crozat wire soldered to the metal arms and adjusted mesial to the maxillary permanent right central incisor to recover space for the missing teeth (Fig. 6). The screw was activated twice daily until overcorrection was reached. After active expansion, the palatal expander was kept in place as a passive retainer for six months.
An interim CBCT was requested to monitor bone healing and the intraosseous position of the impacted teeth. The lateral incisor was still placed horizontally, with the canine crown lying atop it (Fig. 7A). After rapid maxillary expansion, spontaneous eruption of the lateral incisor into the oral cavity behind the crown of the central incisor was observed (Fig. 7B).
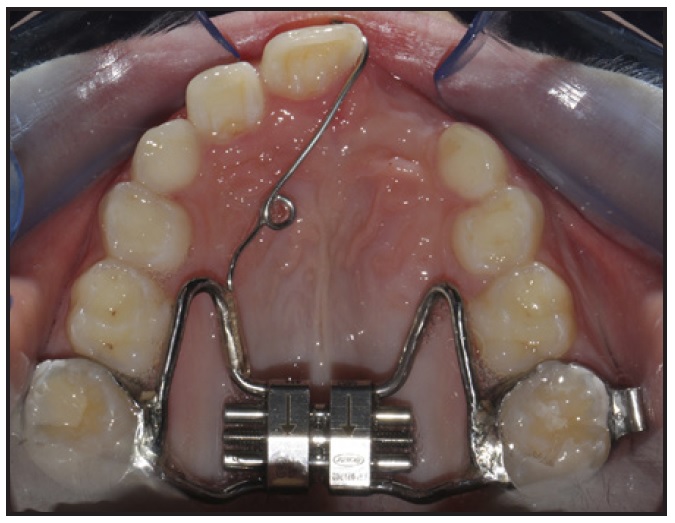
Fig. 6 Modified palatal expander* with Crozat arm extending forward mesial to permanent right central incisor.
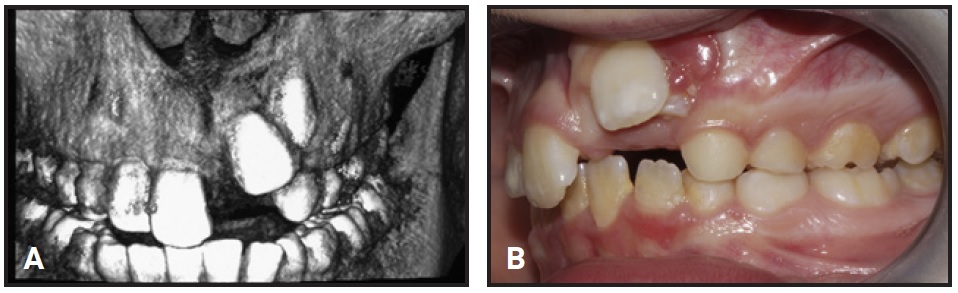
Fig. 7 A. After six months of active expansion, CBCT shows adequate bone healing, but upper left lateral incisor still positioned horizontally with canine impinging on it. B. Spontaneous eruption of lateral incisor.
The next step was to move the central incisor into its proper position in the arch, away from the lateral incisor. The maxillary right first molar, permanent central and lateral incisors, and deciduous canine were bonded and connected with an .016" × .022" stainless steel archwire as an anchor unit. A bracket was then bonded to the crown of the left central incisor, and an elastomeric chain (60-90g) was tied to the right central incisor to move the tooth mesially. The patient was checked every three weeks.
The patient was also asked to wear a conventional cervical headgear (adapted to the tubes of the maxillary first-molar bands) 14 hours per day. As recommended by Lima Filho and colleagues,9 the outer bows were bent 20° upward to prevent molar distal tipping, and a force of about 450g was applied.
Three months later, the crown of the left permanent canine erupted spontaneously over the lateral incisor. A button was then bonded to the canine crown, and an elastomeric chain (60-90g) was tied to the left second deciduous molar to move the tooth away from the root of the lateral incisor. After three months, a segmented arch was used to move the canine into a more distal and vestibular position (Fig. 8).
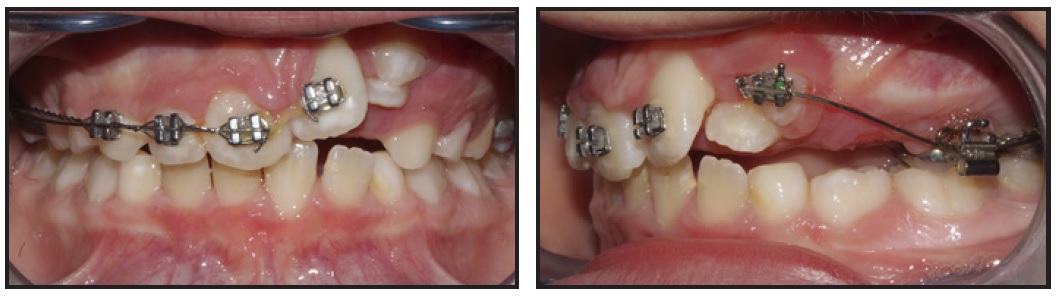
Fig. 8 After three months of headgear wear, spontaneous eruption of upper left canine; segmented arch used to move canine distolabially.
Fixed orthodontic treatment was begun four months later to align the lateral incisor in the occlusal plane.1 A bracket was placed on the lateral incisor crown, and leveling and alignment of the six anterior teeth were carried out over the next nine months on a sequence of .016" × .022" nickel titanium and .016" × .022" stainless steel archwires. After 21 months of Phase I treatment, the patient was placed on observation recall for two years, until the permanent dentition. A second phase of treatment with fixed appliances was used to finish the occlusion in 22 months.
Treatment Results
The impacted maxillary left central and lateral incisors and the impacted maxillary canine were brought into proper positions (Fig. 9). The final appearance of the teeth was esthetically pleasing, with normal gingival margins. The teeth responded well to vitality testing and showed no abnormalities in their crown shapes.
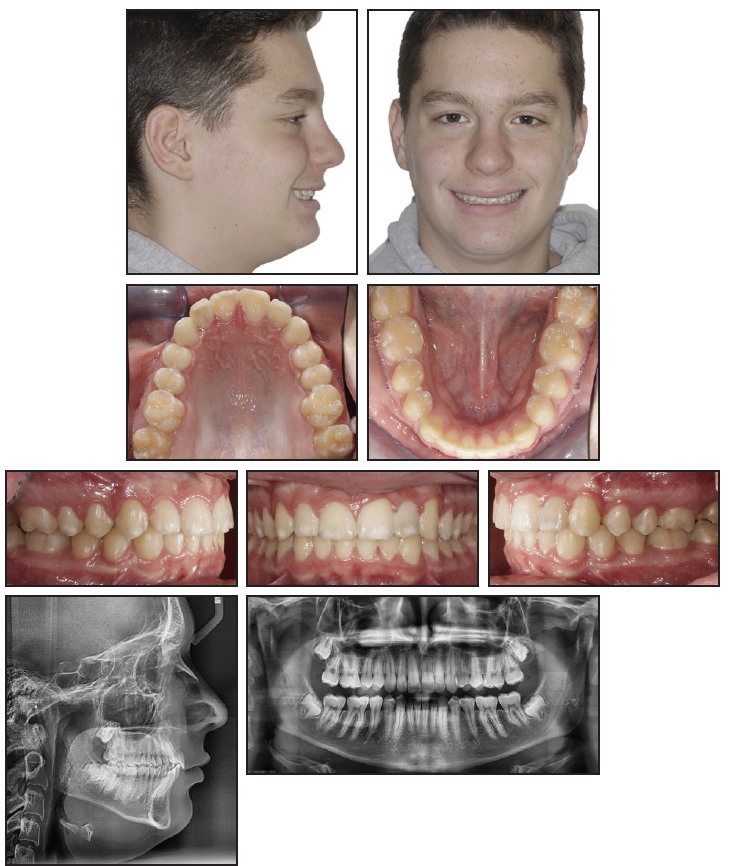
Fig. 9 Patient after 21 months of Phase I treatment, two years of observation, and 22 months of Phase II treatment.
The final appearance of the teeth was esthetically pleasing, with normal gingival margins. The teeth responded well to vitality testing and showed no abnormalities in their crown shapes.
From a periodontal point of view, a band of labial keratinized gingiva measuring 4mm was present, and pocket depths ranged from 1mm to 2mm. Hard and soft tissues were preserved. Healing and bone regeneration were excellent: new bone apposition was observed after marsupialization, with no recurrence of cyst formation. Final panoramic and lateral cephalometric radiographs indicated proper root alignment and no bone disease, but the left central incisor root did not complete its development.
Discussion
Impaction of maxillary permanent incisors occurs in .2-1% of the population.10 In children, impacted maxillary incisors can compromise facial esthetics because of their prominent location and their importance to facial esthetics.11 Early referral is common, considering the concern of parents and general dentists regarding delayed eruption of these teeth.12,13
The literature indicates several causes of failed or delayed eruption of maxillary incisors. Eruption failure may occur if pathological obstructions develop in the eruptive path of the incisor; it can also be caused by tooth malformation or dilacerations.14,15 The most common pathological obstructions are supernumerary teeth, odontomas, and cysts.14
In the present case, a large, severely inflammatory dentigerous cyst caused the impaction of the central and lateral maxillary incisors. This type of dentigerous cyst is found only in the mixed dentition, developing when inflammation at the root apex of a nonvital primary tooth spreads to involve the follicles of immature unerupted successors—in our case, the upper left permanent incisors and canine.3
Careful planning, including thorough clinical and radiographic diagnosis, is required when treating an impacted incisor.16 CBCT images can clearly identify the intraosseus location, root resorption, inclination, and morphology of impacted teeth, as well as their distance from adjacent structures.17,18 The treatment strategy in the present case involved elimination of the obstacle through marsupialization, followed by early interceptive orthopedic-orthodontic treatment to allow spontaneous eruption of the delayed incisors and canine and improve their intraosseous positions.
Marsupialization is considered the best method to conserve a tooth affected by an inflammatory dentigerous cyst and permit its eruption, especially in a growing patient.2 This treatment is a gradually diminishing process, using the tendency of peripheral bone to grow centripetally into the cavity center after the relief of internal hydrostatic pressure.3 An accessory cavity is created within the cyst’s bony wall, and the cystic lining is sutured to the oral mucosa, forming a pocket and allowing new bone to fill the defect. The benefits of this approach include preservation of tooth buds, reduced risk of damage to adjacent anatomical structures, maintenance of pulp vitality, and elimination of an obvious jawbone defect that would affect the patient’s quality of life.5
Maxillary expansion has been proposed as an alternative interceptive treatment for impacted incisors and as a means of facilitating eruption of the teeth after the removal of obstacles.19,20 In our case, expansion of the maxillary anterior segment allowed us to recover space in the arch and improve the intraosseous vertical and angular positions of the impacted teeth. Moreover, with the increased upper arch length obtained through the use of headgear, the impacted teeth erupted spontaneously without any surgical intervention for orthodontic traction.21
The orthodontic mechanics used to distalize the permanent canine allowed proper alignment of the lateral incisor. Once the canine was no longer impinging on it, the root position of the lateral incisor was corrected by vestibular root torque.
Through careful orthodontic biomechanics, the impacted teeth were moved into their correct positions in the dental arch, and the final result was successful.
Conclusion
This case report shows how an interceptive multidisciplinary approach can achieve results that would not be possible if either surgical or orthodontic treatment were applied independently. Establishment of anterior guidance, leveling of gingival margins, and restoration of new bone in the defect were possible only through the combined efforts of both specialists. Satisfactory functional and esthetic results were obtained, gingival attachment was maintained, and the integrity of maxillary bone was restored.22
FOOTNOTES
- *Leone S.p.A., Sesto Fiorentino, Firenze, Italy; www.leone.it.
REFERENCES
- 1. Kalaskar, R. and Kalaskar, A.: Multidisciplinary management of impacted central incisors due to supernumerary teeth and an associated dentigerous cyst, Contemp. Clin. Dent. 2:53-58, 2011.
- 2. Qian, W.T.; Ma, Z.G.; Xie, Q.Y.; Cai, X.Y.; Zhang, Y.; and Yang, C.: Marsupialization facilitates eruption of dentigerous cyst-associated mandibular premolars in preadolescent patients, J. Oral Maxillofac. Surg. 71:1825-1832, 2013.
- 3. Kumar, R.; Singh, R.K.; Pandey, R.K.; Mohammad, S.; and Ram, H.: Inflammatory dentigerous cyst in a ten-year-old child, Natl. J. Maxillofac. Surg. 3:80-83, 2012.
- 4. Mishra, R.; Tripathi, A.M.; and Rathore, M.: Dentigerous cyst associated with horizontally impacted mandibular second premolar, Int. J. Clin. Pediat. Dent. 7:54-57, 2014.
- 5. Allon, D.M.; Allon, I.; Anavi, Y.; Kaplan, I.; and Chaushu, G.: Decompression as a treatment of odontogenic cystic lesions in children, J. Oral Maxillofac. Surg. 73:649-654, 2014.
- 6. Santos, B.Z.; Beltrame, A.P.; Bolan, M.; Grando, L.J.; and Cordeiro, M.M.: Dentigerous cyst of inflammatory origin, J. Dent. Child. (Chic.) 81:112-116, 2014.
- 7. Pinho, T.; Neves, M.; and Alves, C.: Impacted maxillary central incisor: Surgical exposure and orthodontic treatment, Am. J. Orthod. 140:256-265, 2011.
- 8. Cozza, P.; Giancotti, A.; and Petrosino, A.: Rapid palatal expansion in mixed dentition using a modified expander: A cephalometric investigation, J. Orthod. 28:129-134, 2001.
- 9. Lima Filho, R.M.A.; Lima, A.L.; and de Oliveira Ruellas, A.C.: Mandibular changes in skeletal Class II patients treated with Kloehn cervical headgear, Am. J. Orthod. 124:83-90, 2003.
- 10. Kurol, J.: Early treatment of tooth eruption disturbances, Am. J. Orthod. 121:588-591, 2002.
- 11. Smailiene, D.; Sidlauskas, A.; and Bucinskiene, J.: Impaction of the central maxillary incisor associated with supernumerary teeth: Initial position and spontaneous eruption timing, Stomatologija 8:103-107, 2006.
- 12. Kolokitha, O.E. and Papadopoulou, A.K.: Impaction and apical root angulation of the maxillary central incisors due to supernumerary teeth: Combined surgical and orthodontic treatment, Am. J. Orthod. 134:153-160, 2008.
- 13. Becker, A.; Brin, I.; Ben-Bassat, Y.; Zilberman, Y.; and Chaushu, S.: Closed-eruption surgical technique for impacted maxillary incisors: A postorthodontic periodontal evaluation, Am. J. Orthod. 122:9-14, 2002.
- 14. Huber, K.L.; Suri, L.; and Taneja, P.: Eruption disturbances of the maxillary incisors: A literature review, J. Clin. Pediat. Dent. 32:221-230, 2008.
- 15. Chokron, A.; Reveret, S.; Salmon, B.; and Vermelin, L.: Strategies for treating an impacted maxillary central incisor, Int. Orthod. 8:152-176, 2010.
- 16. Duncan, W.K.; Ashrafi, M.H.; Meister, F. Jr.; and Pruhs, R.J.: Management of the nonerupted maxillary anterior tooth, J. Am. Dent. Assoc. 106:640-644, 1983.
- 17. Sawamura, T.; Minowa, K.; and Nakamura, M.: Impacted teeth in the maxilla: Usefulness of 3D dental-CT for preoperative evaluation, Eur. J. Radiol. 47:221-226, 2003.
- 18. Chen, Y.; Duan, P.; Meng, Y.; and Chen, Y.: Three-dimensional spiral computed tomographic imaging: A new approach to the diagnosis and treatment planning of impacted teeth, Am. J. Orthod. 130:112-116, 2006.
- 19. Pavoni, C.; Paoloni, V.; Ghislanzoni, L.T.H.; Laganà, G.; and Cozza, P.: Geometric morphometric analysis of the palatal morphology in children with impacted incisors: A three-dimensional evaluation, Angle Orthod. 87:404-408, 2017.
- 20. Pavoni, C.; Mucedero, M.; Paoloni, V.; and Cozza, P.: Interceptive management for multiple eruption disturbances: A follow-up evaluation, Eur. J. Paediat. Dent. 15:191-194, 2014.
- 21. Leonardi, M.; Armi, P.; Franchi, L.; and Baccetti, T: Two interceptive approaches to palatally displaced canines: A prospective longitudinal study, Angle Orthod. 74:581-586, 2004.
- 22. Kokich, V.G. and Spear, F.M.: Interdisciplinary management of anterior guidance: A case report, Adv. Esth. Interdisc. Dent. 3:2-6, 2007.







COMMENTS
.