CASE REPORT
Anterior Repositioning Appliance for Relief of TMD in Conjunction with Definitive Orthodontic Treatment
Temporomandibular dysfunction is a common issue, affecting as much as 33% of the population.1 Although the etiology of TMD is complex, one major cause is trauma, which can result in muscle pain, TMJ pain, and intracapsular changes. Trauma can predispose a patient to the development of disc displacements; stretching of the ligaments supporting the TMJ; or formation of irregularities within the condyle, fossa, or disc, leading to catching movements.2
An anterior repositioning appliance is often used for the treatment of disc displacement with reduction. The patient can wear the device only at night to begin; as symptoms resolve, the patient can gradually reduce appliance wear. If symptoms persist, the patient may need to wear the appliance for a longer period, since the adaptive process of the TMJ complex may take two to three months. Another reason for persistent symptoms is a lack of stability within the joint. In such a case, the bite will need to be constructed around a stable occlusion achieved through definitive orthodontics or prosthodontics.3
This case report describes the application of an anterior repositioning appliance in conjunction with definitive orthodontic treatment using Class III elastics.
Diagnosis and Treatment Planning
A 31-year-old female presented with the chief complaints of TMD symptoms and a changing bite (Fig. 1A). Her dental history included treatment for trauma-induced TMD at age 8 (with an intraoral neuromuscular device) and again at age 15. The patient stated that her right condyle was a source of pain due to a physical blow to the right side of her face in 1992. She had begun having migraines with photopia and nausea shortly after the incident. The migraines varied in intensity and frequency, with a peak occurrence of three times per day and an intensity as high as 10 out of 10 on the pain scale. The migraines eventually became milder (1 out of 10), and the patient identified caffeine as a trigger. Her physician had prescribed beta blockers, which were unsuccessful, and Topamax,* which produced negative side effects.
Clinical examination found a slightly convex profile with a fuller right side of the face and asymmetrical commissures (lower on the right). The lower facial third was long, and a dental cant was evident; the chin was positioned slightly to the left of the midsagittal plane. The patient had a Class I occlusion with 2-3mm of crowding in the maxillary arch, 4-5mm of crowding in the mandibular arch, and a canted occlusal plane. The overbite and overjet were normal. A Bolton discrepancy was attributable to excessive tooth size in the mandibular arch. The TMJ complex showed a maximum opening of 45mm with a 10mm range of protrusive, left lateral, and right lateral movements. The right and left external pterygoid muscles were tender on palpation; the left condyle clicked on lateral movements, while the right clicked on opening (Fig. 1B).

Fig. 1 31-year-old female patient with previous TMD treatment, Class I occlusion, Class II skeletal relationship, canted occlusal plane, lower Bolton discrepancy, and 45mm maximum TMJ opening before treatment (continued in next image).
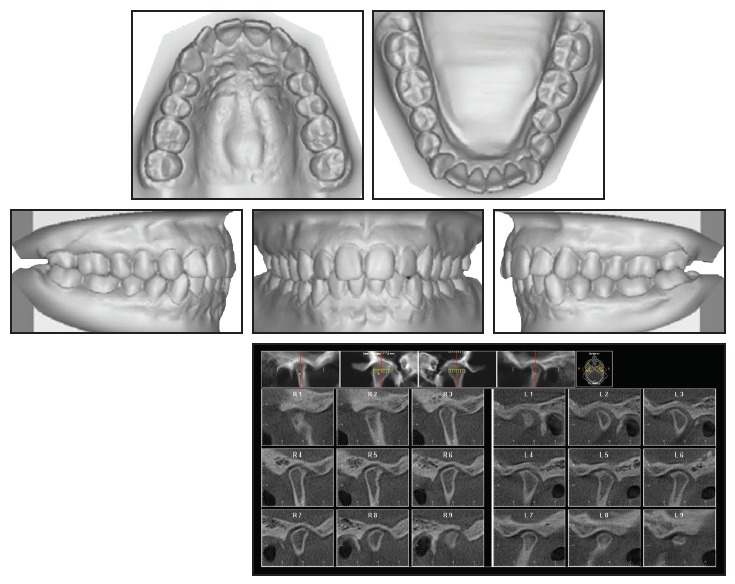
Fig. 1 (cont.) 31-year-old female patient with previous TMD treatment, Class I occlusion, Class II skeletal relationship, canted occlusal plane, lower Bolton discrepancy, and 45mm maximum TMJ opening before treatment.
Cephalometric analysis indicated a Class II skeletal relationship, due to a slightly retrognathic mandible, and a steep mandibular plane. The panoramic radiograph showed parallel roots, previously extracted third molars, and a short ramus on the left side. The right TMJ evidenced remodeling with a posterosuperior loss of volume, thin joint space, posteriorly positioned condyle, and flattened eminence. The left TMJ exhibited inactive degenerative joint disease with a posterosuperior loss of volume, thin joint space, posteriorly positioned and small condyle, flattened eminence, and anterior osteophyte.
The patient was no longer taking the migraine medications, but her headaches had again increased in intensity and were occurring daily upon waking. Nortrel** taken as a contraceptive was her only current prescription. The medical history showed allergies to penicillin and copper; subjective surgical history included a reduction of turbinates, removal of bone spurs on the ethmoidal plate, and correction of a deviated septum.
The treatment objectives were to resolve the TMD (clicking and instability) and the posteriorly displaced condyles, relieve the pain and muscle soreness, eliminate the dental crowding, and maintain a Class I occlusion while correcting the Bolton discrepancy.
Three treatment options were suggested: an anterior repositioning appliance followed by orthodontic treatment, comprehensive orthodontic treatment with heavy interproximal reduction (IPR), and comprehensive orthodontic treatment after extraction of a lower incisor. The patient accepted the first option.
Treatment Progress
To construct the anterior repositioning appliance, impressions and facebow records were taken, and a bite registration was made in centric relation with wax and blue mousse. The casts were mounted on an articulator, and an occlusal stent was fabricated on the mandibular cast.
The patient returned for delivery of the orthotic (Fig. 2). Acrylic was added to the occlusal surface and allowed to set in centric relation, using the bilateral manual manipulation technique.4 The stent was adjusted to slightly reduce the vertical dimension of occlusion (Fig. 3).
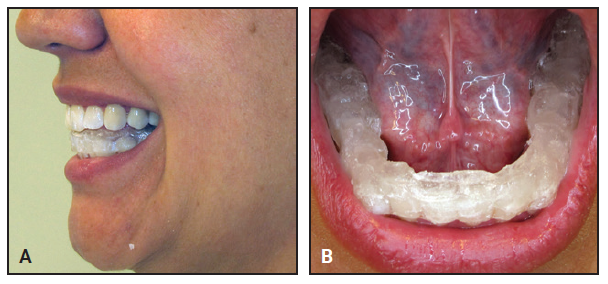
Fig. 2 A. Anterior repositioning appliance on delivery. B. Acrylic added to occlusal surface and allowed to set in centric relation.

Fig. 3 A. Stent adjusted to slightly reduce vertical dimension of occlusion. B. Posterior stops used to verify vertical dimension.
On each subsequent visit, the mandible was moved anteriorly until the condyle reduced. If this occurred earlier than on the previous visit, a new bite was taken, and the appliance was equilibrated again. In this manner, the condyle-disc relationship was “walked back” into the fossa, guiding the teeth into maximum intercuspation while stabilizing the joint.
Over the first eight weeks of wearing the appliance 24 hours per day, the patient experienced a reduction in pain and headaches (both frequency and severity), and she reported no clicking or popping (Fig. 4). Our recommendation to wear the orthotic another eight weeks for stability was declined due to time constraints.

Fig. 4 Adjusted appliance worn for eight weeks.
Orthodontic treatment was then initiated by bonding the maxillary arch. The archwire sequence progressed to .018" stainless steel over three months, and the lower first molars were allowed to erupt vertically into the occlusion (Fig. 5). Four weeks later, the orthotic was cut off distal to the second premolars, and elastics were prescribed from the upper to lower first molars while the patient wore the orthotic continuously.

Fig. 5 Maxillary arch bonded, with wire sequence progressing to .018" stainless steel over three months. Lower first molars allowed to erupt vertically into occlusion; note first molars in constructed bite without orthotic in place.
After two more months, the orthotic was cut off distal to the canines, and the lower first and second premolars were bonded to enable their vertical eruption (Fig. 6).

Fig. 6 Orthotic cut off distal to canines; lower first and second premolars bonded to enable vertical eruption.
Another three weeks later, a full archwire was inserted, with comfort tubing in the anterior region, and Class III vertical elastics were worn while the patient maintained orthotic wear from canine to canine (Fig. 7).
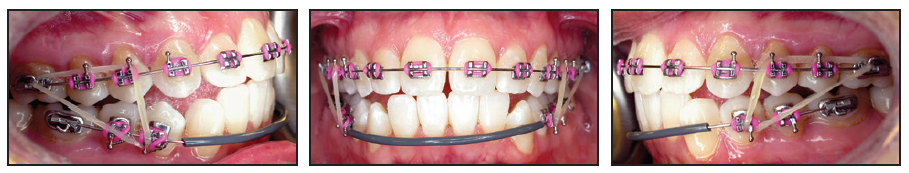
Fig. 7 Full archwire with anterior comfort tubing and Class III vertical elastics.
Eight weeks later, Class III sliding jigs were added, extending to the lower second molars, to provide direct distalization for Class III correction (Fig. 8). Elastics were worn from the upper first molars to anterior hooks on the sliding jigs.

Fig. 8 Class III sliding jigs extended to lower second molars to provide direct distalization for Class III correction; elastics attached from upper first molars to anterior hooks on sliding jigs.
After another nine weeks of treatment, the remaining teeth were bonded (Fig. 9). Vertical elastics were worn from the upper canines to the lower canines and first premolars. Finishing and detailing were carried out prior to debonding, and IPR was performed from lower canine to canine to resolve the Bolton discrepancy.

Fig. 9 Remaining teeth bonded nine weeks later.
Treatment Results
Total treatment time was 21 months (Fig. 10A). A normal overbite and overjet were established, while the Class I occlusion was maintained. The midlines were coincident, and a straighter profile was achieved. The patient showed slightly increased incisal angulations, proper root angulations, and normalized condylar positions with no further condylar remodeling. Cephalometric superimpositions indicated flaring of the upper and lower incisors and some mandibular protrusion (Fig. 10B).

Fig. 10 A. Patient after 21 months of treatment (continued in next image).
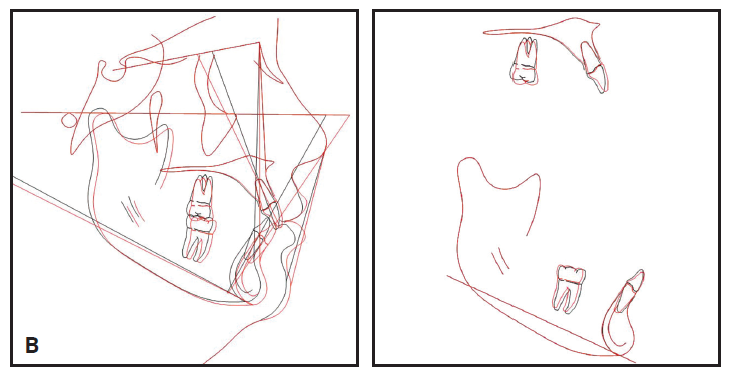
Fig. 10 (cont.) B. Superimposition of pre- and post-treatment cephalometric tracings.
A lower 3-3 retainer was bonded. Upper and lower Essix*** retainers were prescribed to be worn 24 hours per day (except while eating) for three months, after which the patient could switch to nightly wear. She reported no post-treatment TMD symptoms.
Discussion
Simmons posed this question in a 2006 American Academy of Craniofacial Pain white paper: Is there a value to having the joint properly positioned?5 He concluded that a proper condyle-to-fossa relationship, with the disc in a normal position, affords protection from a myriad of potential problems. A stable TMJ relationship safeguards against degenerative joint disease from osteoarthritis, encourages normal mandibular growth, limits myofascial pain, and reduces pain in the TMJ complex.
An anterior repositioning appliance allows healing of the retrodiscal tissues, redistributes forces within the complex, and promotes condylar remodeling.6 Practitioners have used such appliances for treatment of anterior displacement with or without reduction, tension headaches,7 and a variety of intracapsular issues.8 Grummons recommended beginning TMD treatment with an anterior repositioning appliance because it can help resolve joint clicking, locking, stiffness, and inflammation.9 Since pain within the TMJ complex cannot be differentiated among intracapsular disorders, the anterior repositioning appliance is a logical place to start.10
Conti and colleagues demonstrated adequate pain control from night-only wear of an anterior repositioning appliance, observing no changes in occlusion after one year of use.11 Even if the disc were still displaced to a degree, the remodeling would be adequate for some patients. On the other hand, Chen and colleagues found a 60% relapse after discontinuation of an anterior repositioning appliance.12 Lundh and colleagues concluded from a study of 63 patients that anterior repositioning appliances provided better pain reduction than flat-plane stents during disc recapture.13 Nevertheless, they observed a relapse when appliance wear was discontinued after six months, emphasizing the need for definitive treatment on a case-by-case basis. Gelb and Gelb also showed anterior repositioning appliances to be superior to flat-plane stents in reducing TMJ pain and noises.7
As in the present case, a Class II skeletal relationship often predisposes the patient to posterior displacement of the condyles.14 In addition, De Boever and Keersmaekers found that an etiology of trauma was associated with a greater magnitude of TMJ pain and headaches.15 In their study, patients with and without trauma showed similarly successful results after one year of treatment.
In our patient, we suspected bilateral disc displacement with reduction because most patients with TMD symptoms demonstrate reducing discs.16 Magnetic resonance imaging (MRI) can be used before treatment to establish a differential diagnosis. An MRI may also be taken after use of an anterior repositioning appliance to confirm disc recapture. Patients with reducing discs show a 91% recapture rate when the condyle is moved into the proper Gelb 4/7 position (Fig. 11) with an anterior repositioning appliance, as evaluated by MRI.4
Our patient was placed in a musculoskeletally stable position with a bilateral manual manipulation technique, which is described by Okeson as a method of moving the condyles into their most superoanterior positions when the mouth closes.17 Clinically, this manipulation eliminated the TMJ clicking and popping in our case. A bite registration was then made in centric relation (Fig. 2), since the coincidence of centric occlusion with centric relation is of paramount importance as the teeth guide the condylar axes.18
After eight weeks of pain-free splint wear, we initiated orthodontic treatment. In a TMD patient, there is always a concern when posterior forces are exerted on the mandibular structure. Hu and colleagues, evaluating the effects of Class III interarch elastics, demonstrated that the condyloid rotated counterclockwise, with an overall displacement posteriorly and superiorly.19 Because shorter Class II and III elastics were found to be gentler, our vertical Class III elastics were configured to provide a short-elastic effect. Forces were controlled by progressively equilibrating the splint and removing material to reestablish the bite. The mandibular complex was maintained in centric relation, ensuring dentoalveolar movement rather than movement of the entire TMJ complex.
FOOTNOTES
- *Registered trademark of Janssen Pharmaceuticals, Inc., Meridian, CO; www.topamax.com.
- **Teva Pharmaceuticals USA, Inc., Parsippany, NJ; www.tevausa.com.
- ***Registered trademark of Dentsply Sirona Orthodontics Inc., Sarasota, FL; www.essix.com.
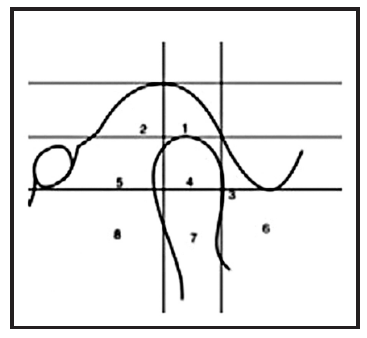
Fig. 11 Gelb diagram of proper 4/7 condyle/fossa relationship.
REFERENCES
- 1. Wright, E.F. and North, S.L.: Management and treatment of temporomandibular disorders: A clinical perspective, J. Man. Manip. Ther. 17:247-254, 2009.
- 2. Wright, E.F.: Manual of Temporomandibular Disorders, 3rd ed., Wiley-Blackwell, Hoboken, NJ, 2014.
- 3. Okeson, J.P.: Management of Temporomandibular Disorders and Occlusion, 3rd ed., Mosby Elsevier, St. Louis, 2008.
- 4. Simmons, H.C. III.: Orthodontic finishing after TMJ disk manipulation and recapture, Int. J. Orthod. Milwaukee 13:7-12, 2002.
- 5. Simmons, H.C. III: Guidelines for anterior repositioning appliance therapy for the management of craniofacial pain and TMD, Funct. Orthod. 23:22-31, 2006.
- 6. Liu, M.Q.; Chen, H.M.; Yap, A.U.; and Fu, K.: Condylar remodeling accompanying splint therapy: A cone-beam computerized tomography study of patients with temporomandibular joint disk displacement, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 114:259-265, 2012.
- 7. Gelb, M.L. and Gelb, H.: Gelb appliance: Mandibular orthopedic repositioning therapy, in Intraoral Orthotics, ed. S.W. Bledsoe Jr., Williams & Wilkins, Baltimore, 1991.
- 8. Simmons, H.C. III and Gibbs, S.J.: Recapture of temporomandibular joint disks using anterior repositioning appliances: An MRI study, Cranio 13:227-237, 1995.
- 9. Grummons, D.: Orthodontics for the TMJ-TMD Patient, Wright & Co., Scottsdale, AZ, 1994.
- 10. Chantaracherd, P.; John, M.T.; Hodges, J.S.; and Schiffman, E.L.: Temporomandibular joint disorders’ impact on pain, function, and disability, J. Dent. Res. 94:79-86, 2015.
- 11. Conti, P.C.; Miranda, J.E.; Conti, A.C.; Pegoraro, L.F.; and Araújo Cdos, R.: Partial time use of anterior repositioning splints in the management of TMJ pain and dysfunction: A one-year controlled study, J. Appl. Oral Sci. 13:345-350, 2005.
- 12. Chen, H.M.; Liu, M.Q.; Yap, A.U.; and Fu, K.Y.: Physiological effects of anterior repositioning splint on temporomandibular joint disc displacement: A quantitative analysis, J. Oral Rehab. 44:664-672, 2017.
- 13. Lundh, H.; Westesson, P.L.; Jisander, S.; and Eriksson, L: Disk-repositioning onlays in the treatment of temporomandibular joint disk displacement: Comparison with a flat occlusal splint and with no treatment, Oral Surg. Oral Med. Oral Pathol. 66:155-162, 1988.
- 14. Fichera, G.; Ronsivalle, V.; Santonocito, S.; Aboulazm, K.S.; Isola, G.; Leonardi, R.; and Palazzo, G.: Class II skeletal malocclusion and prevalence of temporomandibular disorders: An epidemiological pilot study on growing subjects, J. Funct. Morphol. Kinesiol. 6:63, 2021.
- 15. De Boever, J.A. and Keersmaekers, K.: Trauma in patients with temporomandibular disorders: Frequency and treatment outcome, J. Oral Rehab. 23:91-96, 1996.
- 16. Simmons, H.C. III and Gibbs, S.J.: Initial TMJ recapture with anterior repositioning appliances and relation to dental history, Cranio 15:281-295, 1997.
- 17. Okeson, J.P.: Evolution of occlusion and temporomandibular disorder in orthodontics: Past, present, and future, Am. J. Orthod. 147:216-223, 2015.
- 18. Crawford, S.D.: Condylar axis position, as determined by the occlusion and measured by the CPI instrument, and signs and symptoms of temporomandibular dysfunction, Angle Orthod. 69:103-116, 1999.
- 19. Hu, M.; Xiang, Y.N.; Li, H.; Guo, K.F.; and Wang, F.: The stress distribution of the temporomandibular joint under four types of inter-arch elastics: A three dimensional finite element model analysis, W. China J. Stomatol. 28:145-148, 2010.





COMMENTS
.