Comparison of Three Options for Neuromuscular Deprogramming Treatment
The TMJ is a highly complex joint that can suffer alterations in intracapsular soft and hard tissues, as well as in the muscles that work with it, resulting in abnormalities that inevitably lead to TMD. The prevalence of TMD is between 5% and 12%, but there is a higher prevalence in young people, which is unusual for chronic-pain conditions. TMD primarily affects women, with twice as many cases as in men; in addition, women who use supplemental estrogens or oral contraceptives are more likely to seek treatment for TMD.1-5
TMD can affect the joint, muscles, or both, but the aim of treatment is always to prevent further degeneration and restore joint stability. In cases involving muscular TMD, an occlusal splint known as a neuromuscular deprogramming appliance (NDA) can be used to ensure that the condyles reach an anatomically and orthopedically stable position, while providing a functional occlusion. This treatment is effective, but it tends to take a long time, depending on the severity of the damage.6,7
The use of botulinum toxin type A (BTX-A) can reduce TMD treatment time by diminishing muscle activity. BTX-A blocks the synapses of the neurotransmitter acetylcholine, thus inhibiting nerve impulses and preventing the injected muscle from contracting.8,9 Bakke was the first to use BTX-A to treat TMD, demonstrating how anterior disc displacement improved after application of the toxin.10 In cases of myofascial pain associated with masseteric hypertrophy, injection of BTX-A into both masseters has produced an immediate state of relaxation and reduced biting forces.11,12
Another option is laser radiation, which has been used in the management of inflammatory processes and lesions affecting soft, muscular, and osteoarticular tissues of the musculoskeletal system. The radiation is absorbed by the tissue and produces a biochemical interaction that increases adenosine triphosphate reserves, which in turn enhance oxygen consumption and the normalization of tissue damaged by inflammation, trauma, or osteoarticular injury.13 Laser therapy has been successfully used in dentistry for bone regeneration and treatment of hypersensitivity and tissue damage, as well as for improvement of muscle function and reduction of symptoms in TMD patients.14,15
The aim of this clinical trial was to compare the effectiveness and efficiency of three neuromuscular deprogramming treatments, using NDA only, NDA plus diode laser radiation, and NDA plus BTX-A.
Materials and Methods
The study sample included patients with muscular TMD who were treated at the Temporomandibular Disorder Clinic of the Master of Orthodontics program, Universidad de la Salle Bajío, between September 2014 and April 2017. The project was evaluated and authorized by the Research and Ethics Committee of the University Research Office. Patients with rheumatoid arthritis, those who were allergic to BTX-A, and pregnant women were excluded. Twenty male and 19 female patients, ranging in age from 12 to 64 (average age 29.0 ± 12.5) met the selection criteria and agreed to participate in the study. After being told of the study’s purpose, procedures, risks, and benefits, they signed informed-consent forms. Equal numbers of patients (13 each) were randomly assigned to three treatment groups:
Group A—NDA only
Group B—NDA and diode laser therapy
Group C—NDA and botulinum toxin
Before fitting of the NDA, an initial reading was taken with a condylar position indicator (CPI) based on two wax registrations: one with the jaw in centric relation (guiding the patient’s anatomical arc of closure) and another with no mandibular manipulation. The NDA was used in the same way in all three groups: the appliance was worn 24 hours per day, and all patients were required to return for weekly checkups. At each checkup, the occlusion was adjusted in an attempt to achieve centric relation and thus to obtain punctiform, bilateral, symmetrical contact points of equal intensity. The appliance was adjusted to ensure smooth, prompt, and progressive functional guides (Fig. 1).

Fig. 1 Upper neuromuscular deprogramming appliance (NDA). A. Maximum intercuspal position. B. Mandibular protrusion with anterior guidance. C. Right mandibular lateral movement with canine guidance. D. Left mandibular lateral movement with canine guidance.
Once the patient’s jaw could easily be manipulated into centric relation and the occlusal points on the NDA were stable (Figs. 2,3), with no indentations or scratches, weekly appointments were scheduled to take new CPI readings with the patient’s normal bite. Neuromuscular deprogramming was deemed complete when three consecutive CPI readings showed no change.
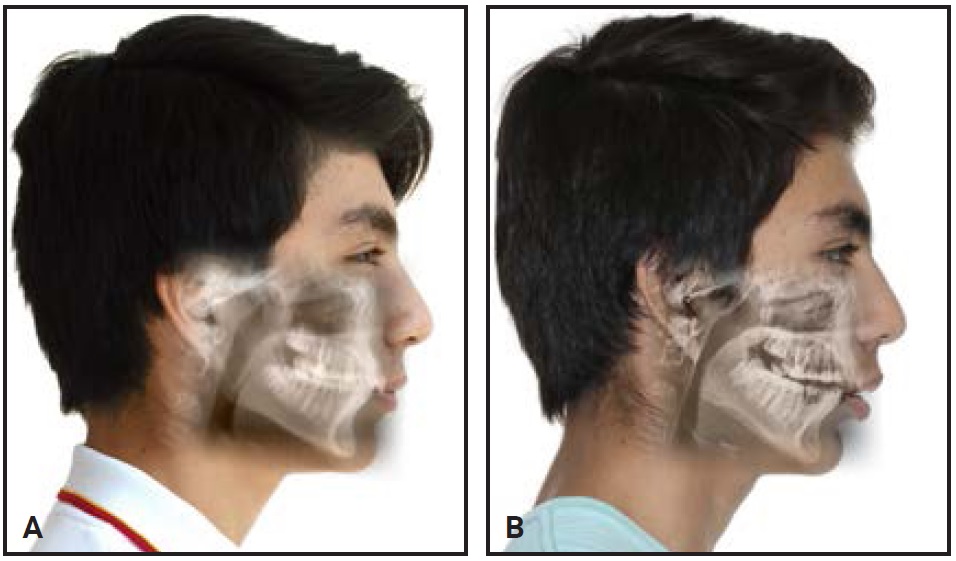
Fig. 2 A. Patient before articular treatment. B. Effects of NDA, including clockwise mandibular rotation from condylar seating into centric relation, producing increase in vertical dimension with lower lip and chin retrusion. Note increase in overjet and reduction of overbite.
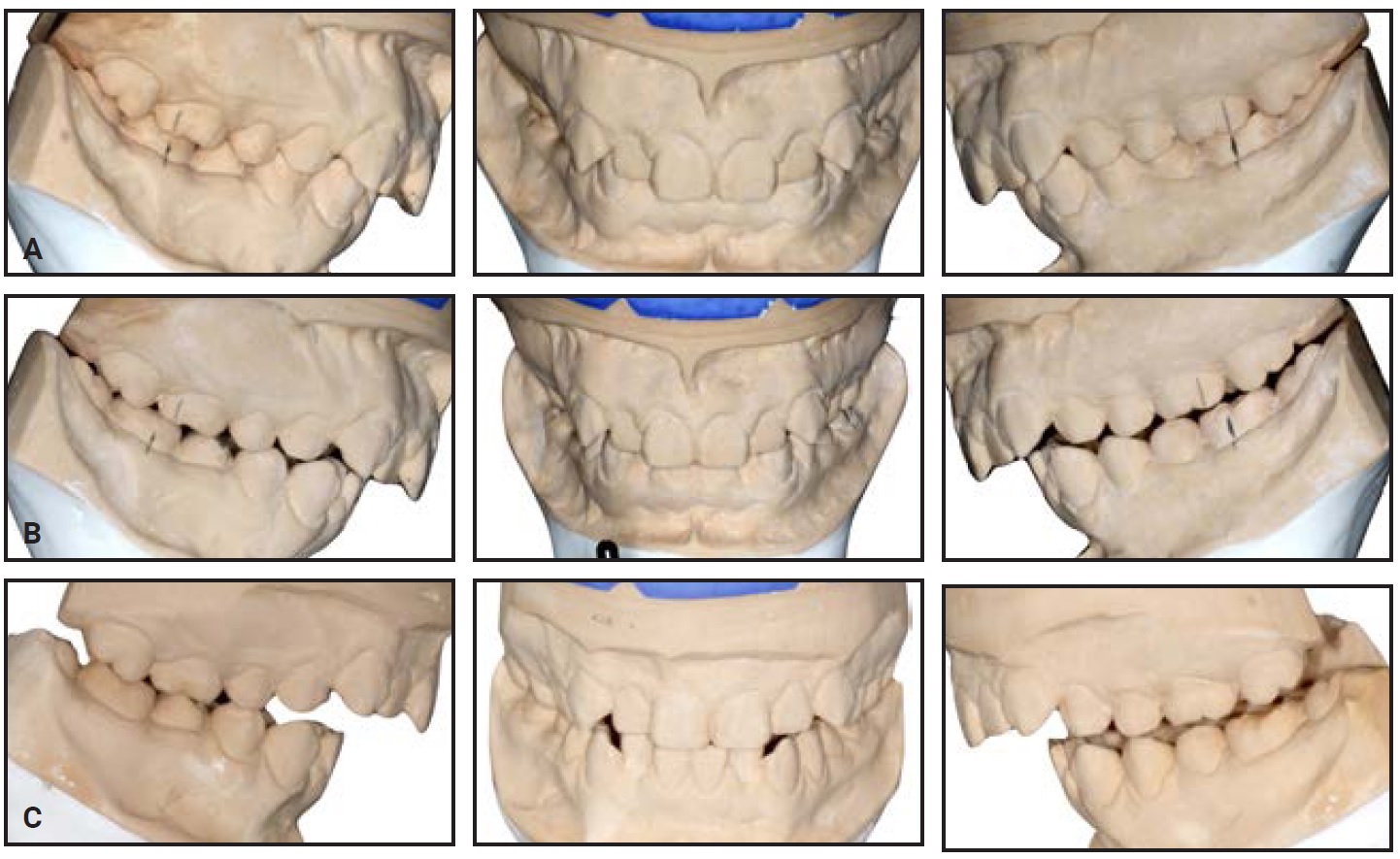
Fig. 3 Patient’s articulated models. Note that occlusion changes as mandibular condyles are seated into centric relation. A. Maximum intercuspal position. B. First mounting attempt does not reflect patient’s true centric relation due to muscle stiffness. C. Use of NDA results in muscular relaxation, showing patient’s actual malocclusion in centric relation.
In group B, in addition to the NDA treatment, each patient received diode laser therapy for trismus with a Quantum IR-810** (120V, 60Hz, 24W, IEEC825-1, Type IIIb, 100-200mW, 810nm, 7.9°), which was applied in scan mode to each masseter and temporal muscle for 100 seconds at an intensity level of 10J/cm2 (Fig. 4). The laser was then applied in pulse mode in each TMJ region for 100 seconds at an intensity of 10J/cm2.
In group C, each patient was injected with 80U of BTX-A in each masseter muscle and 20U in each temporal muscle on the day the NDA was fitted (Fig. 5). This was done after identifying which areas to inject and asking the patient to contract and hold the muscle during the intramuscular injection. The patient was then instructed not to touch the injection site nor to lie down for two hours.
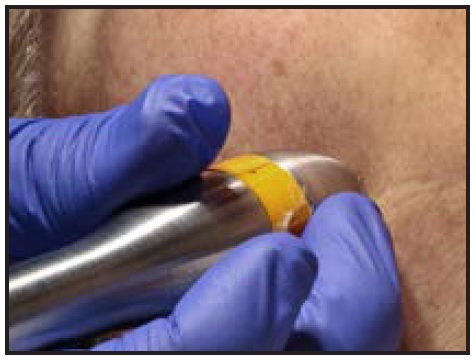
Fig. 4 Therapeutic laser application in trismus mode at right masseter in patient from group B.
At the beginning and end of treatment, the level of muscle pain was measured using a Visual Analog Scale (0 = no pain, 10 = maximum pain). Deprogramming time for each patient was measured in weeks between the fitting of the NDA and the date on which the patient was told it was no longer required.
To quantify the amount of condylar seating achieved by neuromuscular deprogramming, we compared the initial and post-treatment CPI readings. Statistical analysis was performed with SPSS v.21.*** The three groups were compared using a one-way analysis of variance; the Bonferroni test was used for post-hoc analysis. Statistical significance was evaluated using the chi-square test, with the significance level set at p < .05.

Fig. 5 Planning and application of botulinum toxin type A in right masseter muscle of patient from group C.
Results
There were no significant differences among the three treatment groups according to sex or age, although the average age was highest in the BTX-A group (Table 1). The percentages of patients with baseline pain and the initial CPI readings on the X and Z axes were not significantly different among the three groups.
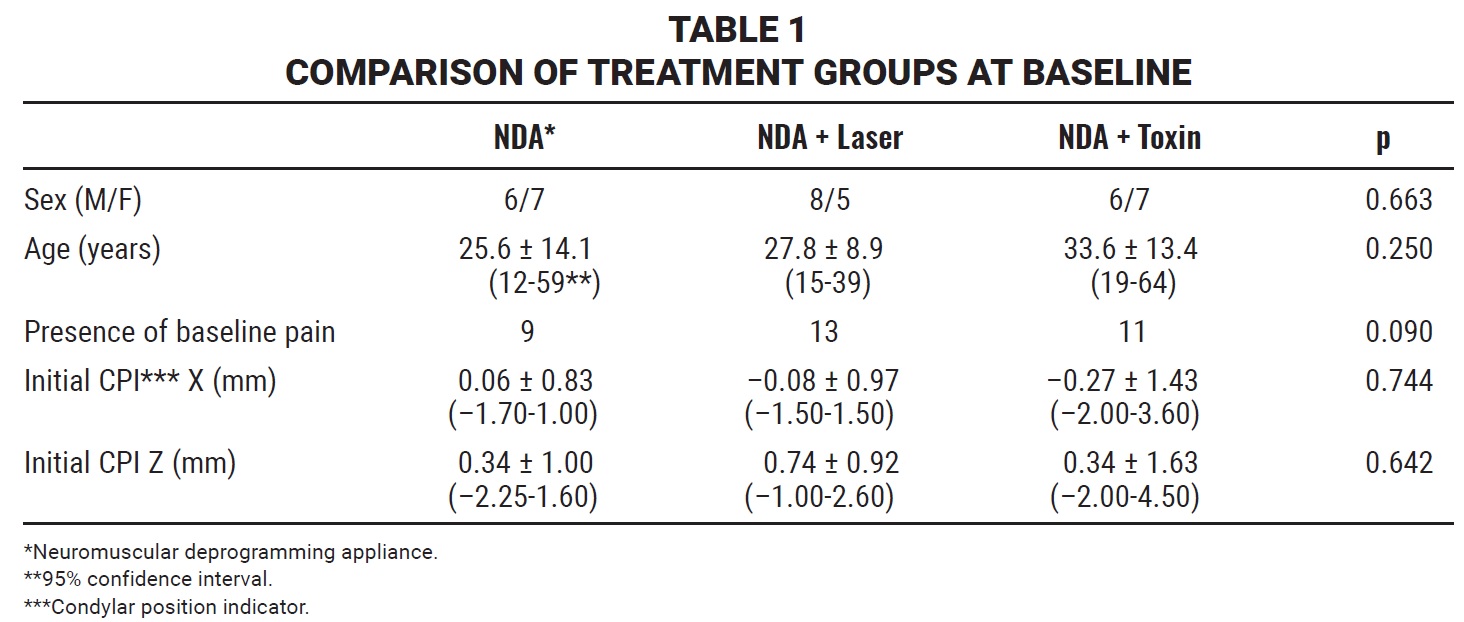
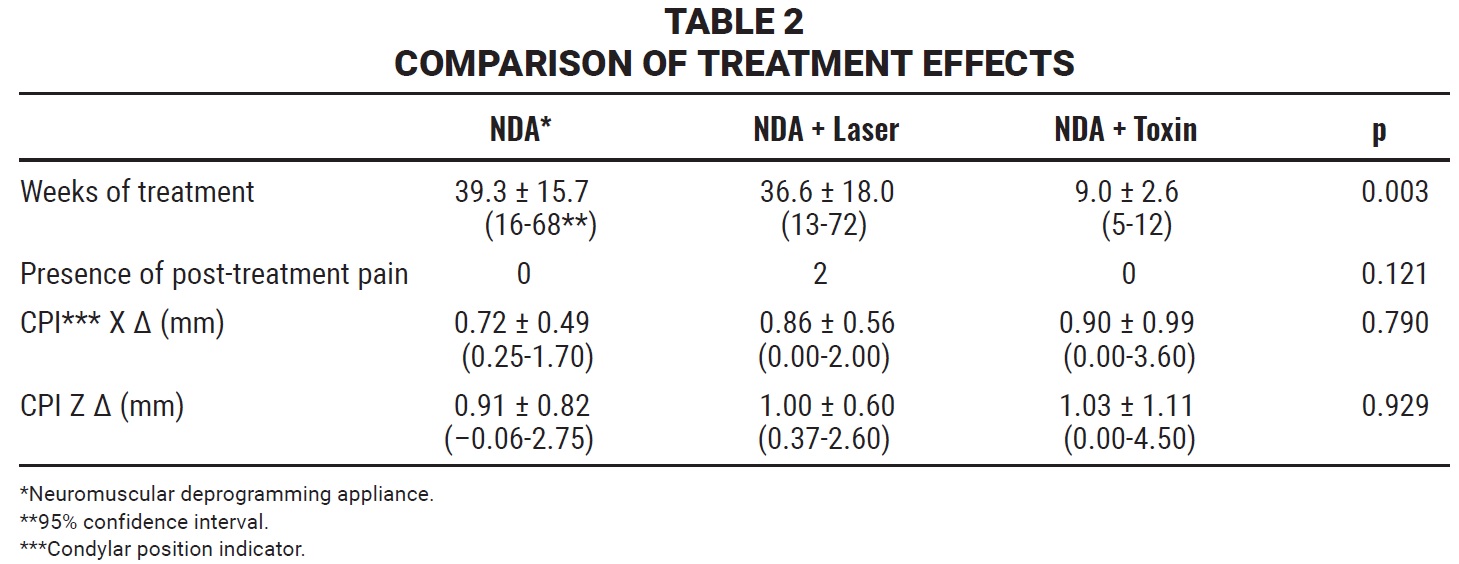
Treatment time was significantly less in the NDA plus BTX-A group, with no significant difference between the NDA only and NDA plus laser groups (Table 2). The percentages of patients reporting pain were significantly reduced in all three groups (p < .001); at the end of treatment, only two patients in the NDA plus laser group reported mild pain. Although all three treatments achieved significant condylar seating in centric relation compared to the baseline, there was no significant difference among the three groups in terms of sagittal or vertical changes (Δ) in CPI readings.
Discussion
An NDA is recommended in patients who present with muscular pain, occlusal dysfunction, facial asymmetries, anterior open bites, dolichofacial patterns, or skeletal Class II or III malocclusions, and whose jaws are difficult to manipulate into centric relation, with a difference of more than 2mm in the CPI reading between centric occlusion and centric relation. The aim of NDA treatment is to obtain an anatomically and orthopedically stable mandibular position in all three planes of space before designing an orthodontic treatment plan.16,17
The time needed for neuromuscular deprogramming reportedly varies from three to six months on average.18 The present study indicates, however, that neuromuscular deprogramming using only an NDA can take nearly 10 months with weekly checkups at an educational institution. Clinical experience has shown that when more frequent checkups are performed, the disorder is corrected more quickly, although specific monitoring procedures would need to be evaluated to confirm this statement in a more methodological way.
In 1989, the American Food and Drug Administration approved the use of BTX-A in TMD treatment because of its muscle-relaxing effect. This paved the way for its use in cases of bruxism, where the toxin is applied to the masseter and temporal muscles to reduce motor activity and associated muscular hypertrophy.19-21 Similarly, the toxin has been used to treat masseter pain in patients with TMD associated with tension headaches.22 In cases of clicking due to direct interaction between the pterygoid muscle and the articular disc, BTX-A has even been injected into the external pterygoid, where it produced a statistically significant elimination of joint noises and was shown by magnetic resonance imaging to promote repositioning of the articular disc.23-26 Since these studies used only toxin applications without occlusal splints, a direct comparison cannot be made with our results. Our study did show that the average treatment time when NDA and BTX-A were combined was only nine weeks—a significantly shorter period than the average 39 weeks required when using only the occlusal splint or the average 36 weeks for the splint plus diode laser therapy.
The reduction in deprogramming time was attributable to the relaxation of the masseter and temporal muscles. When nervous synapse was prevented, mandibular manipulation could be performed with no muscle resistance, making this a more attractive treatment option for the patient, more efficient for the practitioner, and more inexpensive for both. One adverse outcome was the need for a second application of BTX-A in two patients after four weeks with no positive evolution in terms of mandibular manipulation and muscle resistance, indicating insufficient relaxation of the masseter and temporal muscles. According to the literature, some patients may require a booster injection of BTX-A to achieve muscle relaxation, but this is enough to achieve synapses without the need for a third shot.27
Nearly all authors agree that there is a significant increase in the maximum range of jaw movement after the use of diode laser therapy for management of TMD. Opinion is divided on its analgesic efficacy, however, even though the average intensity used in all studies was 4J/cm2.28-35 In studies reporting a reduction in symptoms, the average frequency of laser application was two to three times per week, whereas in studies where no analgesic effect was found, the laser was applied weekly—as in our study. Our results showed a 100% rate of pain remission in both the NDA group and the NDA plus BTX-A group, corroborating previous reports.22,36-40 In the NDA plus laser group, the pain remission rate was 85%. This suggests the need for controlled studies of the diode laser’s analgesic effectiveness, varying the intensity, frequency, form, rhythm, and duration of the applications.
As with the BTX-A treatment, the effectiveness of using diode laser therapy in conjunction with occlusal splints has yet to be explored. Öz compared laser treatment and NDA in two separate groups and concluded that the analgesic effects were practically the same.41 Condylar position and stability in the laser group would need to be assessed, however, as would the analgesic effect in the short and medium terms.
All three treatment options evaluated in our study allowed the condyles to be seated in centric relation, as confirmed by three consecutive CPI readings showing no change.42-44 An unmistakable sign that neuromuscular pacification has been achieved is the ease with which the jaw can be manipulated into centric relation. Nevertheless, since this parameter is subjective and varies from one practitioner to another, we recommend more definitive studies.
After neuromuscular deprogramming therapy, patients will remain stable only as long as they continue to wear their occlusal splints. This requires continued use of an NDA until centric occlusal stability is achieved, whether through orthodontic treatment, prosthetic rehabilitation, surgery, or a combination of these methods. If a patient chooses not to pursue any of these options, the appliance should be used at night indefinitely to prevent joint relapse. Expectations regarding the stability of neuromuscular deprogramming remain uncertain for patients who opt not to undergo second phases of treatment.
FOOTNOTES
- *Dysport, trademark of Galderma, Fort Worth, TX; www.galderma.com.
- **Laser Systems México, Santiago de Querétaro, Mexico; www.lasersystems.com.mx.
- ***IBM, Armonk, New York; www.ibm.com.
REFERENCES
- 1. Johansson, A.; Unell, L.; Carlsson, G.E.; Söderfeldt, B.; and Halling, A.: Gender difference in symptoms related to temporomandibular disorders in a population of 50-year-old subjects, J. Orofac. Pain 17:29-35, 2003.
- 2. Macfarlane, T.V.; Blinkhorn, A.S.; Davies, R.M.; Kincey, J.; and Worthington, H.V.: Oro-facial pain in the community: Prevalence and associated impact, Comm. Dent. Oral Epidemiol. 30:52-60, 2002.
- 3. Pow, E.H.; Leung, K.C.; and McMillan, A.S.: Prevalence of symptoms associated with temporomandibular disorders in Hong Kong Chinese, J. Orofac. Pain 15:228-234, 2001.
- 4. Llodra-Calvo, J.C.; Bravo Pérez, M.; Almerich Silla, J.M.; Canorea Díaz, E.; Casals Peidró, E.; Cortés Martinicorena, F.J.: Expósito Delgado, A.J.; Gómez Santos, G.; Hidalgo Olivares, G.; Lamas Oliveira, M.; Martínez Beneyto, Y.; Monge Tàpies, M.; Montiel Company, J.M.; Navarro Moreno, M.; Otero Casal, M.P.; Sainz Ruiz, C.; and Trullols Casas, M.C.: Oral health survey in Spain (in Spanish), RCOE, 7:19-63, 2002.
- 5. Goulet, J.P.; Lavigne, G.J.; and Lund, J.P.: Jaw pain prevalence among French-speaking Canadians in Quebec and related symptoms of temporomandibular disorders, J. Dent. Res. 74:1738-1744, 1995.
- 6. Karl, P.J. and Foley, T.F. The use of a deprogramming appliance to obtain centric relation records, Angle Orthod. 69:117-124, 1999.
- 7. Okeson, J.P.: Management of Temporomandibular Disorders and Occlusion, 5th ed., Mosby Elsevier, St. Louis, 2003.
- 8. Nayyar, P.; Kumar, P.; Vashisht Nayyar, P.; and Singh, A.: BOTOX: Broadening the horizon of dentistry, J. Clin. Diag. Res. 8:ZE25-ZE29, 2014.
- 9. Bogucki, A.Z. and Kownacka, M.: Clinical aspects of the use of botulinum toxin type A in the treatment of dysfunction of the masticatory system, Adv. Clin. Exp. Med. 25:569-573, 2016.
- 10. Bakke, M.; Møller, E.; Werdelin, L.M.; Dalager, T.; Kitai, N.; and Kreiborg, S.: Treatment of severe temporomandibular joint clicking with botulinum toxin in the lateral pterygoid muscle in two cases of anterior disc displacement, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 100:693-700, 2005.
- 11. Abdulgabar, S.; Beheiri, G.; and Abdel Khalik, D.: Botox injection in the lateral pterygoid muscle versus arthrocentesis: An approach to management of internal derangement of the temporomandibular joint, master’s thesis, Cairo University, Giza, Egypt, 2009.
- 12. Kim, K.S.; Byun, Y.S.; Kim, Y.J.; and Kim, S.T.: Muscle weakness after repeated injection of botulinum toxin type A evaluated according to bite force measurement of human masseter muscle, Dermatol. Surg. 35:1902-1906, 2009.
- 13. Canales Sánchez, M.: The medium power laser and its applications in medicine (in Spanish), Plast. Neurol. Rest. 6:43-45, 2007.
- 14. Ayyildiz, S.; Emir, F.; and Sahin, C.: Evaluation of low-level laser therapy in TMD patients, Case Rep. Dent. 424213, 2015.
- 15. Melis, M.; Di Giosia, M.: and Zawawi, K.H.: Low level laser therapy for the treatment of temporomandibular disorders: A systematic review of the literature, Cranio 30:304-312, 2012.
- 16. Martin, D.; Rozencweig, S.; Maté, A.; and Valenzuela, J.: The importance of condyle position in the diagnosis, treatment and prevention of TMD (in French), Orthod. Fr. 86:125-149, 2015.
- 17. Guillén-Rivas, J.; Anguiano-Flores, L.; Salinas-Escoboza, C.; and Guizar-Mendoza, J.M.: Management of myofascial pain and orthodontic treatment completed in centric relationship in a patient with a history of mandibular fracture: Report of a case (in Spanish), Rev. Esp. Ortod. 48:179-186, 2018.
- 18. Ré, J.P.; Perez, C.; Darmouni, L.; Carlier, J.F.; and Orthlieb, J.D.: The occlusal splint therapy, Int. J. Stomat. Occ. Med. 2:82-86, 2009.
- 19. Jadhao, V.A.; Lokhande, N.; Habbu, S.G.; Sewane, S.; Dongare, S.; and Goyal, N.: Efficacy of botulinum toxin in treating myofascial pain and occlusal force characteristics of masticatory muscles in bruxism, Ind. J. Dent. Res. 28:493-497, 2017.
- 20. Al-Ahmad, H.T. and Al-Qudah, M.A.: The treatment of masseter hypertrophy with botulinum toxin type A, Saudi Med. J. 27:397-400.
- 21. Kim, H.J.; Yum, K.W.; Lee, S.S.; Heo, M.S.; and Seo, K.: Effects of botulinum toxin type A on bilateral masseteric hypertrophy evaluated with computed tomographic measurement, Dermatol. Surg. 29:484-489, 2003.
- 22. Pihut, M.; Ferendiuk, E.; Szewczyk, M.; Kasprzyk, K.; and Wieckiewicz, M.: The efficiency of botulinum toxin type A for the treatment of masseter muscle pain in patients with temporomandibular joint dysfunction and tension-type headache, J. Head Pain 17:29, 2016.
- 23. Fu, K-Y.; Chen, H-M.; Sun, Z-P.; Zhang, Z-K.; and Ma, X-C.: Long-term efficacy of botulinum toxin type A for the treatment of habitual dislocation of the temporomandibular joint, Br. J. Oral Maxillofac. Surg. 48:281-284, 2010.
- 24. Ziegler, C.M.; Haag, C.; and Mühling, J.: Treatment of recurrent temporomandibular joint dislocation with intramuscular botulinum toxin injection, Clin. Oral Investig. 7:52-55, 2003.
- 25. Esmael, W.; Mostafa, H.; and Mekhemer, S.: Clinical assessment of the efficacy of botulinum toxin type A in the treatment of chronic recurrent temporomandibular joint dislocation, master’s thesis, Cairo University, Giza, Egypt, 2010.
- 26. Emara, A.S.; Faramawey, M.I.; Hassaan, M.A.; and Hakam, M.M.: Botulinum toxin injection for management of temporomandibular joint clicking, Int. J. Oral Maxillofac. Surg. 42:759- 764, 2013.
- 27. Alvarez-Pinzon, N.; Sigua-Rodriguez, E.A.; Goulart, D.R.; Olate, S.; Farah, G.J.; and Iwaki-Filho, L.: Botulinum toxin for the treatment of temporomandibular disorders (in Spanish), Int. J. Odontostomatol. 12:103-109, 2018.
- 28. Rodrigues da Silva, M.A.M.; Botelho, A.L.; Vogt Turim, C.; and Bettoni Rodrigues da Silva, A.M.: Low level laser therapy as an adjunctive technique in the management of temporomandibular disorders, Cranio 30:264-271, 2012.
- 29. Mazzeto, M.; Hirono Hotta, T.; and Campi de Andrade Pizzo, R.: Measurements of jaw movements and TMJ pain intensity in patients treated with GaA1As laser, Braz. Dent. J. 21:356-360, 2010.
- 30. Sayed, N.; Murugavel, C.; and Gnanam, A.: Management of temporomandibular disorders with low level laser therapy, J. Maxillofac. Oral Surg. 13:444-450, 2014.
- 31. Kulekcioglu, S.; Sivrioglu, K.; Ozcan, O.; and Parlak, M.: Effectiveness of low-level laser therapy in temporomandibular disorder, Scand. J. Rheumatol. 32:114-118, 2003.
- 32. Wang, X.; Yang, Z.; Zhang, W.; Yi, X.; Liang, C.; and Li, X.: Efficacy evaluation of low-level laser therapy on temporomandibular disorder (in Chinese), Hua Xi Kou Qiang Yi Xue Za Zhi 29:393-395, 2011.
- 33. Chen, J.; Huang, Z.; Ge, M.; and Gao, M.: Efficacy of low-level laser therapy in the treatment of TMDs: A meta-analysis of 14 randomised controlled trials, J. Oral Rehab. 42:291-299, 2015.
- 34. Shobha, R.; Narayanan, V.S.; Jagadish Pai, B.S.; Haishankar, H.P.; and Jijin, M.J.: Low-level laser therapy: A novel therapeutic approach to temporomandibular disorder: A randomized, double-blinded, placebo-controlled trial, Ind. J. Dent. Res. 28:380-387, 2017.
- 35. Da Cunha, L.A.; Macedo Firoozmand, L.; Pereira da Silva, A.; Esteves Afonso Camargo, S.; and Oliveira, W.: Efficacy of low-level laser therapy in the treatment of temporomandibular disorder, Int. Dent. J. 58:213-217, 2008.
- 36. Connelly, S.T.; Myung, J.; Gupta, R.; Tartaglia, G.M.; Gizdulich, A.; Yang, J.; and Silva, R.: Clinical outcomes of Botox injections for chronic temporomandibular disorders: Do we understand how Botox works on muscle, pain, and the brain? Int. J. Oral Maxillofac. Surg. 46:322-327, 2017.
- 37. Sunil Dutt, C.; Ramnani, P.; Thakur, D.; and Pandit, M.: Botulinum toxin in the treatment of muscle specific oro-facial pain: A literature review, J. Maxillofac. Oral Surg. 14:171-175, 2015.
- 38. Torres Huerta, J.C.; Hernández Santos, J.R.; Ortiz Ramírez, E.M.; and Tenopala Villegas, S.: Botulinum toxin type A for pain management in patients with chronic myofascial pain syndrome (in Spanish), J. Span. Soc. Pain 17:22-27, 2010.
- 39. González Magaña, F.; Miranda, L.M.; Malagón Hidalgo, H.; and González Amesquita, V.: Use of botulinum toxin for the treatment of hypertrophy of the masseter muscle (in Spanish), Ibero-Latin Am. Plast. Surg. 38:3, 2012.
- 40. Martínez-Pérez, D.: Botulinum toxin and its use in oral and maxillofacial pathology (in Spanish), Rev. Esp. Cir. Oral Maxilofac. 26:149-154, 2004.
- 41. Öz, S.; Gökçen-Röhlig, B.; Saruhanoglu, A.; and Bülent Tuncer, E.: Management of myofascial pain: Low-level laser therapy versus occlusal splints, J. Craniofac. Surg. 21:1722-1728, 2010.
- 42. Ciaravella, D.; Parziale, V.; Mastrovincenzo, M.; Palazzo, A.; Sabatucci, A.; Suriano, M.M.; Bossù, M.: Cazzolla, A.P.; Lo Muzio, L.; and Chimenti, C.: Condylar position indicator and T-scan system II in clinical evaluation of temporomandibular intracapsular disease, J. Craniomaxillofac. Surg 40:449-455, 2012.
- 43. Ponces, M.J.; Tavares, J.P.; Dias Lopes, J.; and Pinhão Ferreira, A.: Comparison of condylar displacement between three biotypological facial groups by using mounted models and a mandibular position indicator, Kor. J. Orthod. 44:312-319, 2014.
- 44. Rinchuse, D.J.: A three-dimensional comparison of condylar change between centric relation and centric occlusion using the mandibular position indicator, Am. J. Orthod. 107:319-328, 1995.





COMMENTS
.