Indications and Mechanics for First-Molar Extractions
Orthodontic problems involving space discrepancies and the soft-tissue profile are often addressed using such methods as premolar extractions, orthognathic surgery, or arch expansion. Extractions can provide the space needed to correct problems related to overbite, overjet, and intercuspation1; the premolars are commonly chosen for extraction to help relieve crowding or protrusion in either arch.
Clinicians are often hesitant to remove the first molars given their importance in occlusion. Because of the high prevalence of caries in the first molars, however, extraction should be considered whenever their integrity is compromised.2 Other indications for first-molar extractions include extensive caries, hypoplastic lesions, apical pathoses, substantial restorations, root fractures or perforations, and ankylosis,3 as well as significant posterior crowding, a high mandibular-plane angle, anterior open bite,1 a protrusive profile, a Class II or III dental relationship, buccal crossbite, or open bite. A lack of patient cooperation with wearing headgear, severely blocked-out upper canines, extreme overjet, and a Class II malocclusion with little remaining prospect for growth have also been mentioned as indications.4
There are several challenges to consider when extracting first molars. It is crucial to ensure the presence of the second and third molars for substitution, so that a good occlusion can be achieved once the space is closed.1 Another frequent concern for practitioners is the additional time needed for such substantial space closure—six to eight months longer, on average, than premolar extraction-space closure.1 Space closure is more successful when performed on larger rectangular wires, but the mechanics must be designed to prevent the second molars from tipping lingually and mesially during space closure.
Practitioners should consider other potential disadvantages, such as changes in chewing habits and problems associated with the periodontium and TMJ. Studies have shown that patient age is important in terms of extraction timing: it is best to wait until at least age 8, because early extraction can lead to dentofacial asymmetry, premature contacts, and uncontrolled tipping.5 Another challenge during space closure involves gingival clefts remaining at the extraction sites. Removal of any such gingival clefts after treatment will improve gingival health and help prevent relapse.1
Anatomical Considerations
When substituting the upper second molar for the first, the anatomical differences must be considered so that proper occlusion can be achieved.6 The upper first molar is the most complex tooth in its morphology, yet is the least variable. Its large crown is normally composed of four cusps, but a fifth, the cusp of Carabelli, may be present off the mesiolingual cusp. The crown may be in the shape of a rectangle, a square, or a rhomboid. The upper second permanent molar is usually smaller and more variable in its anatomy, especially in the number of cusps. The occlusal table can have a tetracuspid, tricuspid, or compression morphology. From the buccal view, the first molar’s two buccal cusps are nearly identical in size, but the second molar’s distobuccal cusp is smaller. From the lingual, the first molar’s distolingual cusp is smaller than its mesiolingual cusp; the second molar’s distolingual cusp is much smaller or nearly absent. From the occlusal, the first molar is wider in the lingual direction, whereas the second molar is narrower.7
The lower first and second molars also differ in their anatomy. A “5 cusp” or “Y” groove pattern is most common in first molars, but the “4 cusp” or “+” groove pattern is more prevalent in second molars. From the buccal view, the first molar has three cusps and two grooves, while the second molar has two cusps and one groove. From the lingual, the first-molar crown tapers more in the lingual direction, which could affect torque considerations for occlusal purposes when substituting the second molar. From the proximal, the first molar is wider faciolingually.7
Given these anatomical considerations, it is essential to monitor the patient closely for three months after active treatment is completed.8 Because the second molar’s smaller size will create a Bolton discrepancy, it may start to drift distally to achieve better intercuspation. If this space fails to close naturally, composite restorations can be placed.1 The amount of restorative material needed will vary, depending on the patient’s Angle classification and sex, but the restoration can be planned to account for the difference in molar width, allowing proper settling to occur.
Contraindications for first-molar extractions include the presence of a severe arch-length discrepancy, since it would be imprudent to remove a tooth that accounts for much of the occlusal function in a patient with an already shortened archform.9 In cases where anchorage is a concern, molar extractions can result in a critical loss of posterior anchorage because of their large root-surface areas.10 In patients with missing lower first molars, the upper first premolars have been suggested as an alternative for extraction.1
Molar distalization is an option in some cases, with the advantages that patient compliance is not as much of an issue, and less flaring of the incisor segments will occur.12
Ethnic differences in skeletal and dental patterns and the soft-tissue profile should also be considered when designing the treatment plan. For example, one study showed that Japanese patients may need both premolars and molars extracted to relieve severe protrusion.3 On the other hand, in Caucasian patients, extraction of both premolars and molars might flatten the profile.
Mechanical Considerations
Mechanics for space closure should be meticulously planned to make the most efficient use of treatment time and to achieve ideal positioning of the teeth. If the first molars have been extracted and there is a concern that the second molars will erupt and drift mesially into the extraction sites, a lingual arch or Nance appliance can be used until the second molars have fully erupted, thus preserving the space needed for relief of crowding and protrusion. If a second molar tips into the extraction space,9 it will need to be uprighted before power chains or closing-loop mechanics can be utilized to close the space. Even after the roots are uprighted and made parallel, space reopening and open contacts can still become a problem following treatment. Space closure without optimal root parallelism can sometimes result from maxillary sinus pneumatization, but that is not a contraindication to this approach. Space closure is sometimes even preferred to implants in such cases, because implant placement requires the patient to undergo a sinus lift.9 Absent pneumatization, space closure is usually faster and easier mechanically in the maxillary arch than in the mandibular arch.
Another approach for managing first-molar extraction space is to use an en masse plate fitted with an Interlandi headgear to improve the premolar and canine relationships.13 This can be done before placing a full fixed appliance, since distal drifting of the canine and mesial drifting of the second molar have been observed even without appliance engagement on those teeth. The optimal plate design includes double Adams clasps on the first and second premolars, occlusal rests in a “butterfly” configuration on the occlusal surfaces of the adjacent premolars, a stainless steel expansion screw, acrylic palatal coverage, an anterior bite plane, a Kloehn facebow, and headgear tubes.13
Either friction or frictionless mechanics can be utilized to close spaces orthodontically, but an understanding of biomechanics is required to use either method. Frictionless mechanics generate forces by means of loop bends; the moments and anchorage control can be varied to suit the scenario. Closing an extraction space requires both a force to move the teeth and a root-paralleling moment to prevent crown tipping into the space.14 The benefit of closing loops is that they provide a continuous movement that is predictable and adaptable in terms of the moment-to-force ratio. The resulting efficiency may be more of an advantage than the simplicity of sliding mechanics, depending on the clinician’s preferences.15
In closing-loop mechanics, the spring properties are determined by the wire material and size, the distance between attachments, and the loop design. Loops are generally failsafe, so that undesirable consequences will not occur if a patient misses an appointment.14 Closing-loop designs include the teardrop loop, helical loop, T-loop, closed vertical loop with helix, open vertical loop with helix, reverse vertical loop with helix, bull loop, closed vertical loop, open vertical loop, and reverse vertical loop. The most commonly used is the stainless steel teardrop loop, which is easy to fabricate and delivers strong forces with only 1mm of activation. The drawback of this heavy, intermittent force delivery is that treatment may be extended. T-loops offer a more constant way to deliver forces over a large deactivation span. In general, the position of a closing loop determines its mechanism of action, and the mechanics must be controlled to avoid crown tipping into an extraction space.15
In contrast, friction mechanics work by sliding brackets along an archwire to close extraction spaces by means of force from coil springs or elastics. Elastomeric chains are simpler to place, but their force decays over time. On the other hand, austenitic nickel titanium superelastic coil springs produce an ideal, predictable force that does not change much during space closure.14 While friction mechanics are inherently simpler than closing loops, the downside is that friction is counterproductive to sliding mechanics. If differential movement of the posterior and anterior units is needed, headgear or miniscrew anchorage may have to be considered to avoid reciprocal space closure.15 When sliding mechanics are used, 3mm of play between bracket and wire is ideal to prevent friction, but 2mm is adequate. Bracket width is another important factor: if the bracket is wider than half the width of the tooth, the dental alignment can be adversely affected by the reduced interbracket distance.
In either mechanical system, the correct wire size and shape must be selected to combat lingual tipping of the incisor crowns during space closure. A full-size rectangular archwire will prevent excessive play between the bracket and wire, but it may need to be twisted or used with special springs in some cases. The addition of 3rd-order bends for high-torque activation will create unpredictable moment-to-force ratios and generally requires multiple adjustments in the wires during space closure. A torquing arch can aid in achieving ideal incisor torque.15
Orthodontic mesialization of the second molars is a viable option that can maintain the incisor positions and soft-tissue profile while dental crowding or other concerns are addressed. If skeletal anchorage is not used in the anterior region, however, the reciprocal retrusion of the maxilla and mandible will cause a posterior displacement of the upper and lower lips, resulting in a change in profile.2
Although there are some contraindications to first-molar extractions, there are many cases in which they can provide better results than might otherwise be achieved. Patient selection and mechanics must be carefully considered to ensure successful treatment, as demonstrated by the following clinical cases.
Case 1
A 22-year-old female presented with an open bite, a protrusive profile, upper and lower crowding, and an impacted upper left canine (Fig. 1). She had no history of extractions, and her first molars were heavily restored and compromised. Clinical findings included a retained upper left deciduous canine, a stainless steel crown on the upper left first molar, and hypocalcification of the upper right first molar. The patient had Class I canine and molar relationships on the left side and Class III canine and molar relationships on the right, with 5-6mm of crowding in the upper arch and 3-4mm of crowding in the lower arch. The overjet was 2-3mm, and the overbite was 0mm to –1mm.
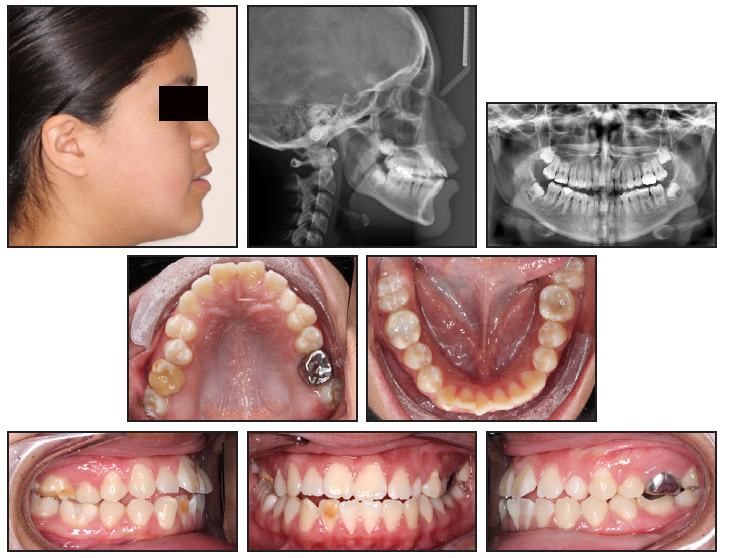
Fig. 1 Case 1. 22-year-old female patient with open bite, impacted upper left canine, protrusive profile, crowding in both arches, and compromised upper first molars before treatment.
Treatment began with extraction of all four first molars and the retained deciduous canine. Space closure with sliding mechanics was initiated on .019" × .025" nickel titanium archwires and continued on .019" × .025" stainless steel wires. A transpalatal arch was inserted with a chain attached to erupt the impacted canine (Fig. 2). A continuous power chain was applied in the lower arch for space closure; in the upper arch, power chains were placed initially from the first premolars to the second molars to create space for the impacted canine, then extended across the entire arch. Open and closed power chains were interchanged, depending on the space distribution.
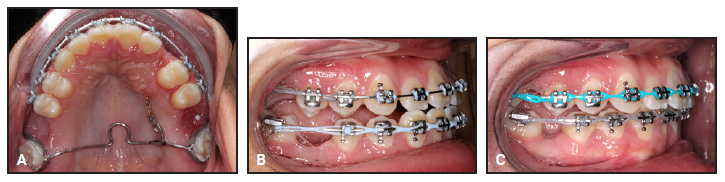
Fig. 2 Case 1. Treatment mechanics following extraction of upper and lower first molars. A. Transpalatal arch with chain attached to impacted canine. B. Power chains attached from upper first premolars to second molars, and from lower second molar to second molar, for space closure. C. Further space closure with continuous power chains in both arches.
Total treatment time was 30 months for both arches (Fig. 3). The soft-tissue profile was improved, but the posterior intercuspation on the right side was less than ideal. The left side was finished in a half-step Class II canine and Class I molar position, while the right side was finished with a Class I canine and half-step Class III molar relationship.

Fig. 3 Case 1. Patient after 30 months of treatment.
Case 2
A 15-year-old female presented with an end-on Class II canine and molar relationship on the left side and a Class II molar relationship on the right, with an impacted upper right canine that made canine classification impossible (Fig. 4).
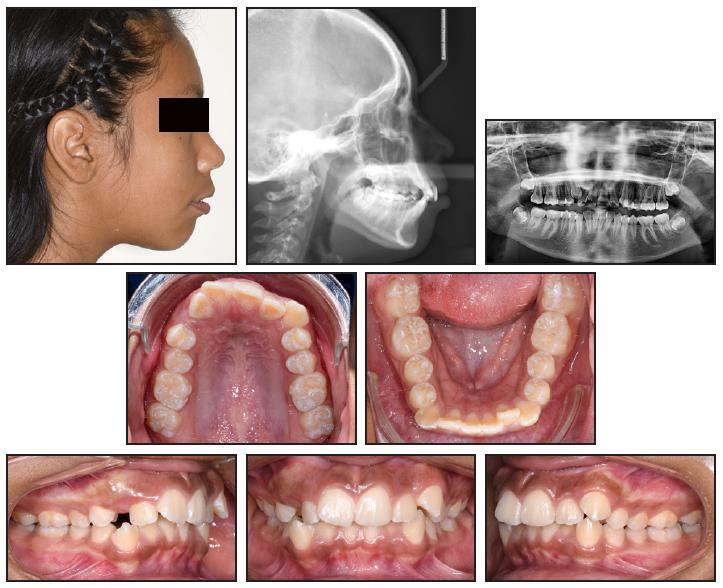
Fig. 4 Case 2. 15-year-old female patient with end-on Class II canine and molar relationship on left, Class II molar relationship on right, upper and lower crowding, and impacted upper right canine before treatment.
After extraction of the upper first premolars and lower second premolars, a Nance appliance was placed to keep the posterior teeth from moving forward into the extraction sites (Fig. 5). Temporary anchorage devices (TADs) were inserted to anchor the anterior retraction.
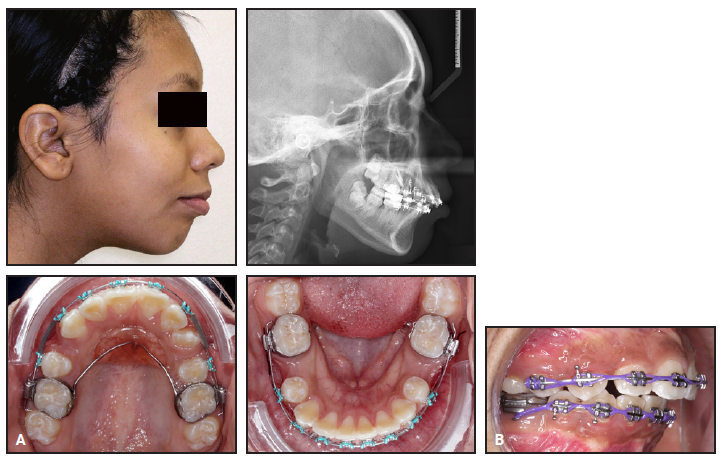
Fig. 5 Case 2. A. After extraction of upper first premolars and lower second premolars, Nance appliance placed on upper first molars to anchor anterior retraction. B. Upper and lower power chains used for space closure.
Following 14 months of this initial treatment, the patient still presented a Class II profile and bimaxillary protrusion, with another 4-5mm of retraction required. The overjet remained at 6-7mm, and the overbite at 3-4mm. There was still 12mm of crowding in the maxillary arch, and 6-8mm in the mandibular arch. The decision was then made to extract the upper first molars, facilitating a reduction of the remaining bimaxillary protrusion, overjet, and crowding (Fig. 6).
Sliding mechanics were used to close the extraction spaces on an .017" × .025" stainless steel archwire, followed by .019" × .025" nickel titanium, .019" × .025" TMA,* and .019" × .025" stainless steel. Power chains were placed both under and over the archwire during the last few visits.
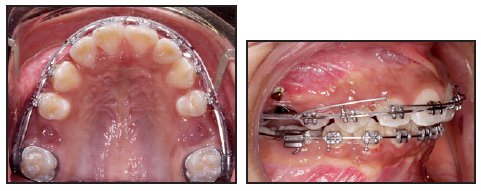
Fig. 6 Case 2. After 14 months of treatment, upper first molars extracted to help improve bimaxillary protrusive appearance, with power chains used for space closure. Auxiliary archwire facilitated simultaneous intrusion of upper incisors during retraction.
Some space closure was seen after 10 months, but distal crown tipping of the upper second molars had created additional spaces. Another four months of treatment was needed for root alignment and final space closure (Fig. 7). Although the case was still in progress at the time of this writing, the soft-tissue profile showed an improvement over the patient’s initial presentation.
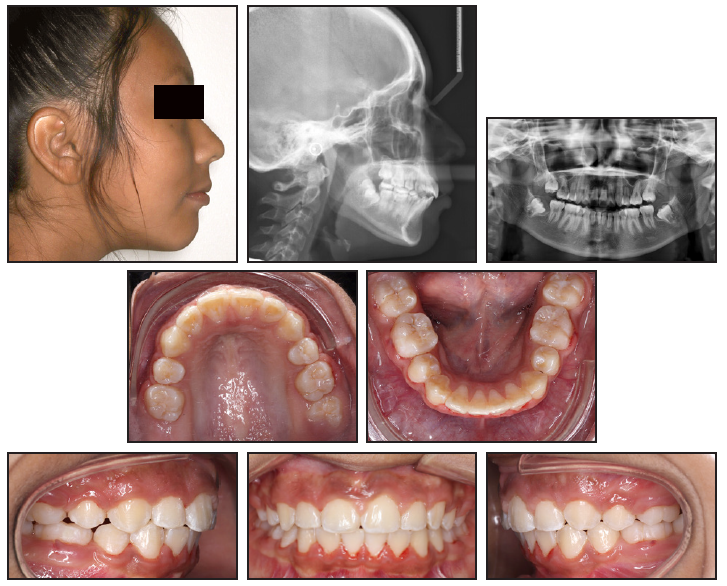
Fig. 7 Case 2. Patient after 28 months of treatment.
Case 3
A 25-year-old female presented with severe incisor flaring, Class II buccal segments, and a Class II skeletal profile after previous extraction of the upper and lower first premolars (Fig. 8). Her canines and molars were in Class II relationships, and she exhibited 0-1mm of upper and lower crowding, 8-9mm of overjet, and an anterior open bite of –1mm to –2mm. The upper first molars were selected for extraction to help correct the remaining problems.

Fig. 8 Case 3. 25-year-old female with anterior open bite, proclined and protrusive upper incisors and lower premolars, Class II buccal segments, Class II skeletal profile, and previously extracted upper and lower first premolars before treatment.
After the extractions, a Nance appliance was placed on the upper second molars for anchorage (Fig. 9). Power chains from the canines to the second molars were used to segmentally retract the anterior dentition.
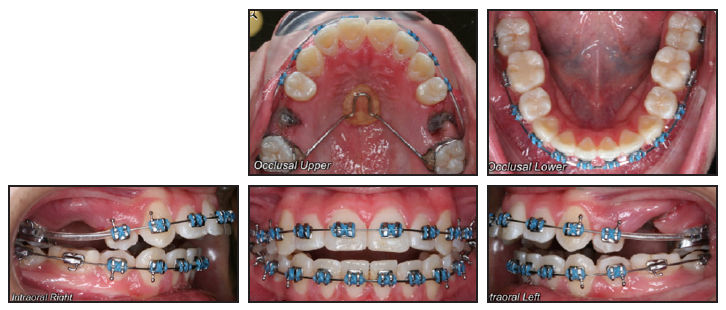
Fig. 9 Case 3. After extraction of upper first molars, Nance appliance placed on upper second molars to anchor anterior retraction.
After 15 months of treatment, the Nance appliance was removed, and power chains were extended across the entire maxillary arch to continue retraction of the anterior segment (Fig. 10).

Fig. 10 Case 3. A. Upper incisor segment initially tied together, with power chains extending from upper canines to second molars. B. After 15 months of treatment, continued space closure with power chains from upper first molar to first molar.
This was followed by four months of retraction using an .018" × .025" stainless steel closing-loop archwire (Fig. 11).
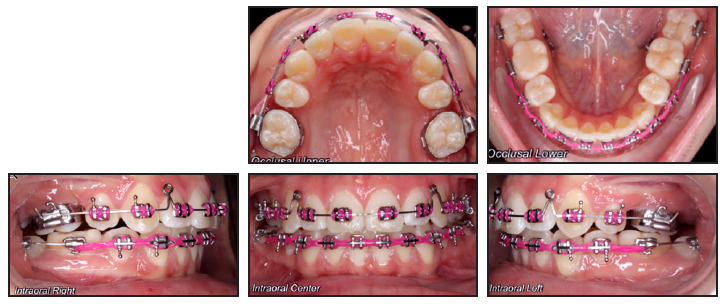
Fig. 11 Case 3. After 18 months of treatment, retraction of upper anterior segment with closing-loop mechanics.
After 25 months of treatment, the patient showed an improved soft-tissue profile, Class I canine and molar relationships, closure of the open bite, and a reduction in overjet (Fig. 12).
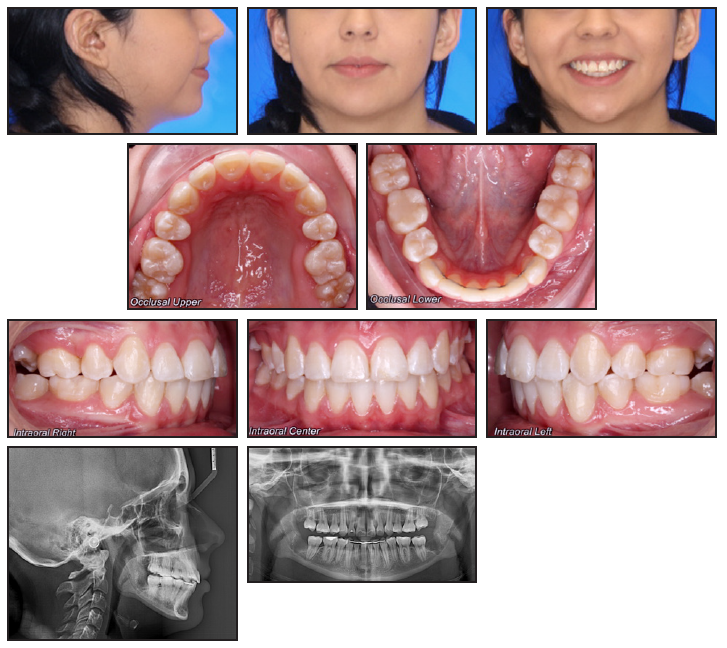
Fig. 12 Case 3. Patient after 25 months of treatment.
Discussion
The orthodontic mechanics were much the same in these three cases. Sliding mechanics with power chains were utilized for space closure; the power chains were attached over or under the archwires as needed for additional force. Both two-step and en masse retraction of the anterior segments were used, depending on the required amount of retraction and overjet reduction.
Initial examination of Case 1 found an open bite, impacted upper left canine, protrusive profile, and compromised upper first molars, indicating extraction of the first molars rather than the more conventional premolars. In a similar example, a patient presented with a Class II occlusion and blocked-out canines, an arch-length discrepancy of 9mm, and compromised first molars.9 After first-molar extractions, a Nance appliance was placed to help distalize the premolars into the extraction sites and to create space for the blocked-out canines, and a fixed appliance was used to achieve a Class I occlusion.
Case 2 began with upper and lower crowding, as well as an impacted upper right canine. After extraction of the upper first premolars and lower second premolars, the remaining Class II profile and bimaxillary protrusion were indications for additional first-molar extractions. In a similar case, a 17-year-old female presented with a convex profile and crowded, protrusive teeth.10 The premolars were healthy, but the first molars were endodontically treated and still needed crowns. Because of their compromised integrity, the first molars were chosen for extraction. Space closure was completed on .019" × .025" stainless steel archwires, with V-bend mechanics and toe-in bends to avoid mesiolingual rotation of the second molars. In another example, a 13-year-old female presented with a convex profile, protruded and crowded teeth, incompetent lips, a 6mm interlabial gap, and mentalis strain on closure.10 The same scenario, with healthy premolars and dubious molar integrity, indicated extraction of the first molars. Space closure was performed in the same manner, although mesiobuccal rotation of the second molars was desirable in this case to create good interdigitation with the embrasures of the lower first and second molars.
In our Case 3, the first molars were extracted due to the patient’s persistent anterior open bite, severe incisor flaring, Class II buccal segments, Class II skeletal profile, excessive overjet, and open bite after previous extraction of the upper and lower first premolars. In a similar example, a patient presented with enamel hypoplasia of the molars, posterior crowding, a full Class II molar relationship, and severe overjet.9 The clinician extracted the first molars at age 9-10, when the second molars exhibited calcification of the interradicular bifurcations. Proper timing of extractions will help simplify the mechanics in the later stages of treatment, as demonstrated by the three cases presented in this article.
Molars have been extracted in various situations when patients have refused surgery to correct their Class III malocclusions.3 In yet another case example, a patient presented with a Class III dentition, but orthognathic surgery was not considered because the skeletal discrepancy was minor and the patient was satisfied with the facial appearance.1 This case was further complicated by the patient’s refusal to have a TAD inserted for distalization of the mandibular dentition. No changes were needed in the upper lip posture, and the lower third molars were in good positions. The lower first molars, rather than premolars, were selected for extraction because of their capacity to provide more retraction space. Elastic chains were used for space closure, and lingual buttons were placed to avoid rotations. Class III and II elastics were utilized to achieve Class I molar and canine relationships. Gingival clefts were surgically removed after the space closure to prevent relapse.
In summary, there are many clinical scenarios in which first-molar extractions can be beneficial. Either sliding or closing-loop mechanics can be used, depending on the orthodontist’s preferences. In the cases shown here, the initial orthodontic concerns were largely improved after treatment involving first-molar extractions. Although the final occlusions were not entirely Class I in every case, the results were acceptable in terms of the cost-benefit ratio.
ACKNOWLEDGMENT: Case 1 was treated by Drs. Kaveh Najibfard and Bloyce Britton. Case 2 was treated by Drs. Komal Patel and Vishnu Raj. Case 3 was treated by Dr. Ravikumar Anthony.
FOOTNOTES
- *Trademark of Ormco Corporation, Brea, CA; www.ormco.com.
REFERENCES
- 1. Ruellas, A.C.; Baratieri, C.; Roma, M.B.; Izquierdo Ade, M.; Boaventura, L.; Rodrigues, C.S.; and Telles, V.: Angle Class III malocclusion treated with mandibular first molar extractions, Am. J. Orthod. 142:384-392, 2012.
- 2. Jacobs, C.; Jacobs-Müller, C.; Luley, C.; Erbe, C.; and Wehrbein, H.: Orthodontic space closure after first molar extraction without skeletal anchorage, J. Orofac. Orthop. 72:51-60, 2011.
- 3. Asai, M.; Tomochika, A.; and Asai, Y.: Molar extraction: A perspective on a clinical study, Orthod. Waves 66:41-51, 2007.
- 4. Grave, K.C. and Gallagher, D.P.: Upper first molar extractions, J. Clin. Orthod. 18:738-740, 1984.
- 5. Hatami, A. and Dreyer, C.: The extraction of first, second or third permanent molar teeth and its effect on the dentofacial complex, Austral. Dent. J. 64:302-311, 2019.
- 6. Genaro, L.; Ferreira, G.; Conte, M.; Gonçalves, M.; and Capote, T.: Morphological differences between the first and second permanent upper molars, J. Morphol. Sci. 36:303-308, 2019.
- 7. Scheid, R.: Woelfel’s Dental Anatomy: Its Relevance to Dentistry, Jones & Bartlett Learning, Burlington, MA, 2007.
- 8. Malkoç, S.; Başçiftçi, F.A.; Nur, M.; and Çatalbaş, B.: Maxillary and mandibular mesiodistal tooth sizes among different malocclusions in a sample of the Turkish population, Eur. J. Orthod. 33:592-596, 2011.
- 9. Sabri, R.: Multidisciplinary management of permanent first molar extractions, Am. J. Orthod. 159:682-692.
- 10. Dhole, P.M. and Maheshwari, D.O.: Orthodontic space closure using simple mechanics in compromised first molar extraction spaces: Case series, J. Ind. Orthod. 52:51-59, 2018.
- 11. Baik, U.B.; Mandair, S.; and Park, J.H.: Extraction alternatives in cases with missing lower first molars, J. Clin. Orthod. 53:181-182, 2019.
- 12. Mohamed, R.N.; Basha, S.; and Al-Thomali, Y.: Maxillary molar distalization with miniscrew-supported appliances in Class II malocclusion: A systematic review, Angle Orthod. 88:494-502, 2018.
- 13. Orton, H.S. and Carter, N.E.: Initial management of first molar extraction cases, J. Clin. Orthod. 22:230-234, 1988.
- 14. Proffit, W.R.; Fields, H.; Larson, B.; and Sarver, D.M.: Comprehensive treatment in adolescence: Space closure and Class II/Class III correction, in Contemporary Orthodontics, 6th ed., Mosby Elsevier, Philadelphia, 2018.
- 15. Ribeiro, G.L. and Jacob, H.B.: Understanding the basis of space closure in orthodontics for a more efficient orthodontic treatment, Dent. Press J. Orthod. 21:115-125, 2016.





COMMENTS
.