Clinical Effectiveness and Efficiency of Customized vs. Conventional Preadjusted Bracket Systems
The ideal bracket system would allow orthodontists to provide high-quality treatment in less time, with fewer appointments and reduced chair-time. Attempts to devise such a system began with Andrews's Straight-Wire Appliance, which improved the efficiency of treatment by incorporating 1st-, 2nd-, and 3rd-order compensations into the brackets.1 Clinicians have found, however, that finishing with a straight wire is rarely possible; detailing bends are usually required due to variations in tooth-surface morphology,2-8 inaccuracies of direct bonding,2,5,9,10 and mechanical deficiencies of edgewise orthodontic appliances.2,5,11
In the Insignia custom bracket system, the clinician creates a virtual design of the final occlusion and alignment using computer-assisted technology, with reverse-engineered brackets and archwires used to obtain the intended result. Bracket slots are customized to accommodate a straight wire that moves each tooth to the ideal final position as identified by the virtual setup. Virtual bracket positions are transferred to the patient by means of indirect-bonding transfer jigs.
This pilot study compares the Insignia system to a modified Roth-prescription conventional bracket system, Titanium Orthos*, in terms of clinical effectiveness and efficiency.
Materials and Methods
Similar articles from the archive:
This retrospective study included cases treated by two orthodontists who had provided feedback to the Insignia manufacturer during development of the appliance. In Practice A, pre- and post-treatment records for subjects treated between September 2006 and June 2010 were examined using inclusion and exclusion criteria; in Practice B, consecutive cases treated between February 2008 and December 2009 were evaluated. The records of patients from Practice A who had malocclusions similar to those of the Insignia patients, but were treated with Titanium Orthos brackets during the same period, were used as a comparative group.
Inclusion criteria for both the Insignia and conventional-appliance groups were as follows:
- Complete maxillary and mandibular fixed appliances were used.
- Treatment included only intraoral, intra-arch, and/or interarch mechanics.
- All permanent teeth were erupted and present in the arch (except for third molars).
- Complete chart entries, pre- and post-treatment casts, and post-treatment panoramic radiographs were available.
Subjects were excluded if:
- Functional appliances, growth modification, extractions, temporary skeletal anchorage, or orthognathic surgery was involved in treatment.
- Post-orthodontic restorative treatment was required.
- Pre- or post-treatment records were incomplete.
Treatment records were reviewed and data recorded by a calibrated examiner (Dr. Weber), who was blinded to the bracket system used to treat the case until all scoring was complete. The pretreatment diagnostic casts were analyzed using the Peer Assessment Rating (PAR) system12; post-treatment casts and panoramic radiographs were evaluated by both the PAR index and the ABO grading system.13 The efficiency of each bracket system was recorded in terms of:
- Number of debonded brackets.
- Number of repositioned brackets.
- Number of finishing wire bends.
- Number of scheduled appointments.
- Number of unscheduled emergency appointments.
- Total treatment time (number of months from initial bonding to debonding).
Intra-Examiner Reliability
To ensure consistent evaluation, 20 non-study calibration cases were scored for PAR and ABO criteria and then rescored at least one week later. Reliability and systematic bias were assessed using intraclass correlation (ICC) and a paired t-test, respectively.
The ICC demonstrated excellent consistency between the standard PAR scores from the University of North Carolina and the examiner's Week 1 scores (ICC = .96). Additionally, the examiner displayed excellent consistency between Week 1 and Week 2 PAR scores (ICC = .99) and ABO scores (ICC = .96). No statistically significant differences were found between the standard PAR scores and the examiner's Week 1 PAR scores or between the Week 1 and Week 2 PAR scores or ABO scores.
Statistical Analysis
Analyses were performed using SAS version 9.1**, with the level of significance set at p < .05. Unpaired t-tests were used to assess whether the two Insignia bracket samples were similar with respect to age at start of treatment, initial PAR, total treatment time, final PAR, and ABO score. Because there were no statistically significant differences, the two groups were combined for further analysis. In addition, there was no significant difference between the Insignia and conventional appliance groups in their initial malocclusions, as determined by age at start of treatment and initial PAR scores. Total treatment time and the effectiveness measures (final PAR and ABO scores) of the two test groups were compared using analysis of covariance (ANCOVA), with the treatment group as the explanatory variable and patient age, pretreatment PAR, age by treatment group, and pretreatment PAR by treatment group interactions as covariates. The interaction covariates for total treatment time and final PAR were not statistically significant and were therefore removed from the model. The age by treatment group interaction term was statistically significant and was retained in the final model for ABO score. The overall final models that included all main effects and significant interactions were statistically significant (final PAR: p = 0.04; ABO score: p = 0.001; treatment time: p < 0.001).
Results
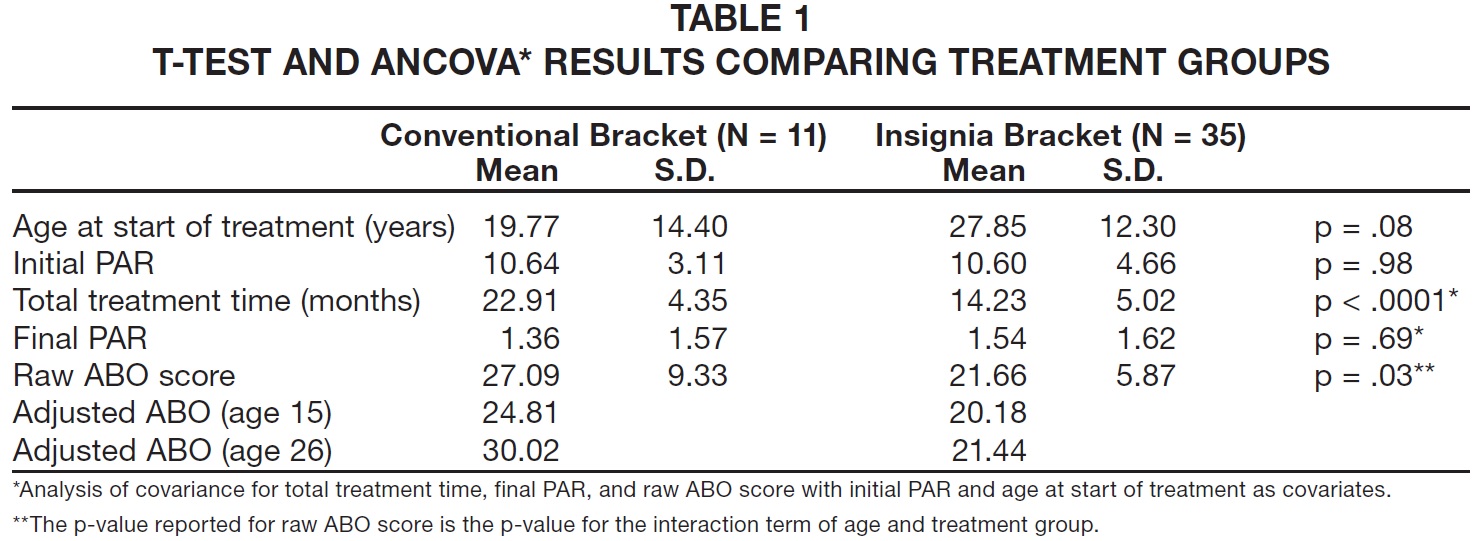
The conventional-bracket group included 11 cases, six male (55%) and five female (45%), with an age range of 12.2-52.7 years (Table 1). The combined Insignia group consisted of 35 subjects, 17 male (49%) and 18 female (51%), with an age range of 12-51.8 years.
Effectiveness Measures
Final PAR scores, after adjusting for age at start of treatment and initial PAR, were not significantly different between the two groups, which showed a similar reduction in PAR scores after treatment (Table 1). Unadjusted mean scores for each section of the ABO Cast and Radiographic Evaluation form are shown in Table 2. Because the interaction between the age at start of treatment and the treatment group was statistically significant, the ABO score for each group was estimated and compared at age 15 and the overall mean age of 26. At both ages, the Insignia group had a lower average ABO score, indicating a finished result closer to the ideal ABO criteria (Table 1).
Efficiency Measures
The adjusted treatment time was significantly shorter for the Insignia patients, with about seven fewer appointments on average (Fig. 1). Numbers of unscheduled emergency appointments, debonded brackets, repositioned brackets, and wire bends were similar between the two treatment groups.
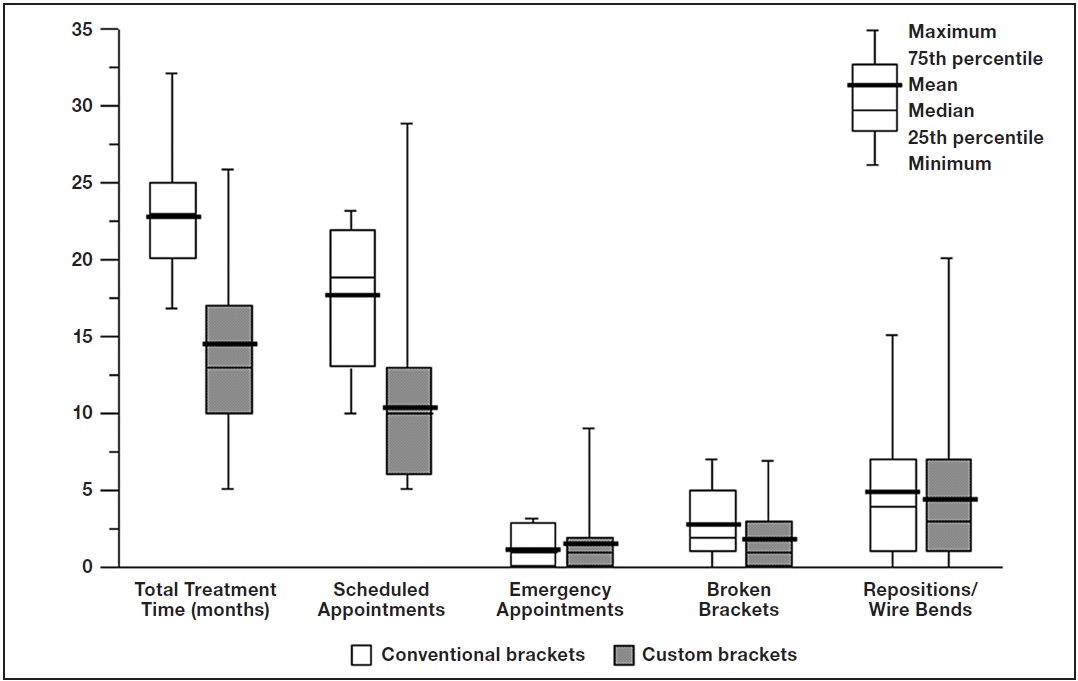
Fig. 1 Efficiency variables comparing treatment groups.
Discussion
The findings of this study must be viewed with caution because of the small size of the conventional-appliance group selected to match the small group of Insignia patients from Practice A, as well as the variability and relatively low initial PAR scores for both groups (Table 1). Two different practices were used in an attempt to increase the sample size of the Insignia group, but since the cases were treated over nearly a four-year period, successive versions of the Insignia system were used; more recent releases may be superior in performance to their predecessors. Finally, it should be noted that the results of this study may not apply to patients with more severe malocclusions.
With these limitations in mind, the final PAR scores suggest that the Insignia system is capable of achieving clinical results similar to those of a conventional edgewise appliance. The ABO scores, which emphasize the details of tooth positioning, were superior in the Insignia group in almost every area, especially alignment/rotations, overjet (arch coordination), and root angulations (Table 2).
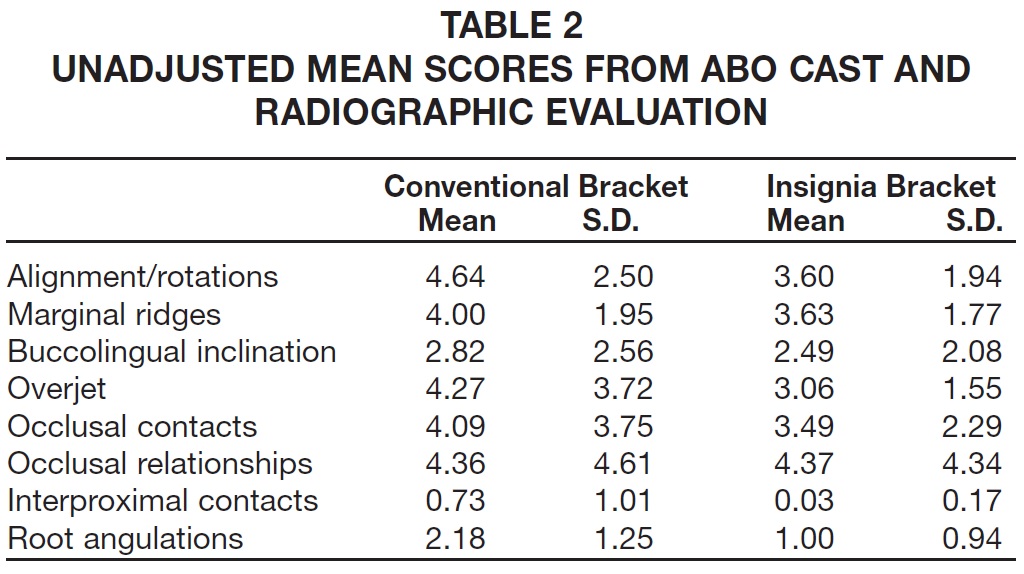
The improved alignment is likely due to the customized slot orientation and the ability to visualize the final occlusal setup at the beginning of treatment. To achieve optimal results, however, the transfer jigs must position the computer-designed slots accurately for indirect bonding. Archwires are contoured to the designed archform and sequentially coordinated from aligning wires to finishing wires, thus maintaining arch coordination throughout treatment and optimizing occlusal relationships in the transverse plane. The setup software generates virtual roots using normative data from dentalanatomy texts and estimates root angulations based on the morphology of the associated crowns. The combination of virtual root setups and marginal ridge visualization most likely accounted for the improvement in root parallelism.14
There are several possible explanations for the reduction in treatment time and number of appointments for the Insignia group compared to the conventional-appliance group. The quality of results was not compromised; some ABO measures actually showed better outcomes (Table 2). The relative difficulty of the conventional and Insignia cases may have been a factor, although the conventional cases were chosen to match the custom cases and the initial and final PAR scores for the two groups were quite similar (Table 1). Another possibility is that PAR score may not be precise enough to identify all the nuances of treatment difficulty. The skill level of the different operators could also be an issue, but the outcomes suggest that all cases were finished to a similar level.
With the Insignia system, since all tooth positions are designed virtually, it is possible that the teeth move in a more direct path to the final occlusion. Although the average numbers of wire bends, emergency appointments, and bracket repositions were similar in both groups, it is plausible that any alignment errors were less severe in the Insignia group and thus took less time to correct toward the end of treatment. The cumulative benefit of these differences may have been enough to reduce treatment time regardless of the number of wire bends, emergencies, bracket repositions, and broken brackets. The individualized archform may also add some advantages that were not assessed by the ABO scores.
Only one patient in the conventional-appliance group and five patients in the Insignia group did not require bracket repositions or wire bends, which suggests that the custom system was not a true "straightwire appliance" (Fig. 1). Possible reasons include variable biological responses to orthodontic forces, less-than-ideal virtual setups, inaccuracies in fabrication or seating of the transfer jigs, and mechanical deficiencies in the tolerance between bracket slots and archwires. In addition, it is possible that bends were needed to compensate for side effects from tooth movement: the slots are designed from a static model of the final occlusion, but tooth movement is actually a dynamic process.
Many authors have argued that a true straightwire appliance is impossible to achieve because of inaccurate bracket placement,2,5,9,10 variations in tooth morphology,2-8 skeletal discrepancies,2,15 the tissue-rebound effect,2,16-18 and deficiencies in appliance mechanics.2,5,11 Miethke and Melsen concluded that "it is unreasonable to anticipate that any straight wire appliance without individual adjustments can be anticipated to lead to an optimal tooth alignment" and proposed that "if the straight wire approach should be followed, the bracket would have to be custom made".3
The customized Insignia appliance may overcome variations in tooth-surface morphology through its manufacturing and bonding process. In the virtual setup, a standard bracket pad is placed on the tooth with at least three points of contact. The transfer jig then allows the clinician to transfer the virtual bracket position to the mouth and hold the customized bracket in place, so that the composite resin can create a "modified custom bracket pad". Logically, the more time spent perfecting and detailing the virtual setup, the less time will be required for wire bends or bracket repositioning to detail and finish the case. Even if virtual treatment planning provides an effective visualization of the final leveling and alignment of the individual arches, however, it can't necessarily predict the interocclusal fit of the arches, which depends on such factors as the leveling biomechanics, the mandibular plane angle, and the severity of the original malocclusion.
Further research, including randomized clinical trials with larger sample sizes, should be conducted to analyze the effectiveness and efficiency of the Insignia custom bracket system. Studies analyzing the accuracy of the bonding jigs in transferring virtual bracket positions to the mouth would also be beneficial.
ACKNOWLEDGMENT: This study was partially supported by a research grant from the Southern Association of Orthodontists.
FOOTNOTES
- *Trademark of Ormco Corporation, Orange CA; www.ormco.com.
- **Registered trademark of SAS Institute, Inc., Cary, NC; www.sas.com.
REFERENCES
- 1. Andrews, L.F.: The Straight-Wire Appliance, J. Clin. Orthod. 10:174-195, 1976.
- 2. Creekmore, T.D. and Kunik, R.L.: Straight wire: The next generation, Am. J. Orthod. 104:8-20, 1993.
- 3. Miethke, R.R. and Melsen, B.: Effect of variation in tooth morphology and bracket position on first and third order correction with preadjusted appliances, Am. J. Orthod. 116:329-335, 1999.
- 4. Dellinger, E.L.: A scientific assessment of the straight-wire appliance, Am. J. Orthod. 73:290-299, 1978.
- 5. Schwaninger, B.: Evaluation of the straight arch wire concept, Am. J. Orthod. 74:188-196, 1978.
- 6. Miethke, R.R.: Third order tooth movements with straight wire appliances. Influence of vestibular tooth crown morphology in the vertical plane, J. Orofac. Orthop. 58:186-197, 1997.
- 7. Germane, N.; Bentley, B.E. Jr.; and Isaacson, R.J.: Three biologic variables modifying faciolingual tooth angulation by straight-wire appliances, Am. J. Orthod. 96:312-319, 1989.
- 8. Bryant, R.M.; Sadowsky, P.L.; and Hazelrig, J.B.: Variability in three morphologic features of the permanent maxillary central incisor, Am. J. Orthod. 86:25-32, 1984.
- 9. Balut, N.; Klapper, L.; Sandrik, J.; and Bowman, D.: Variations in bracket placement in the preadjusted orthodontic appliance, Am. J. Orthod. 102:62-67, 1992.
- 10. Taylor, N.G.: Letter to the Editor: Further comment on bracket positioning; reply by L. Klapper, Am. J. Orthod. 102(5):23A-24A, 1992.
- 11. Archambault, A.; Lacoursiere, R.; Badawi, H.; Major P.W.; Carey, J.; and Flores-Mir, C.: Torque expression in stainless steel orthodontic brackets: A systematic review, Angle Orthod. 80:201-210, 2010.
- 12. Richmond, S.; Shaw, W.C.; O'Brien, K.D.; Buchanan, I.B.; Jones, R.; Stephens, C.D.; Roberts, C.T.; and Andrews, M.: The development of the PAR Index (Peer Assessment Rating): Reliability and validity, Eur. J. Orthod. 14:125-139, 1992.
- 13. The American Board of Orthodontics Grading System for Dental Casts and Panoramic Radiographs, American Board of Orthodontics, June 2008.
- 14. Hartsfield, J.K. and Crane, C.L.: Association of marginal ridge discrepancies and root angulation errors, 2011 IADR General Session, San Diego; abstract published in J. Dent. Res. 90 (Spec. Iss. A):994, 2011.
- 15. Ross, V.A.; Isaacson, R.J.; Germane, N.; and Rubenstein, L.K.: Influence of vertical growth pattern on faciolingual inclinations and treatment mechanics, Am. J. Orthod. 98:422-429, 1990.
- 16. Zachrisson, B.U.: JCO Interviews Dr. Bjorn Zachrisson on excellence in finishing, Part 2, J. Clin. Orthod. 20:536-556, 1986.
- 17. Roth, R.H.: Treatment mechanics for the straight wire appliance, in Orthodontics: Current Principles and Techniques, ed. T.M. Graber and B.F. Swain, C.V. Mosby, St. Louis, 1985, pp. 665-716.
- 18. Swain, B.F.: Straight wire design strategies: Five-year evaluation of the Roth modification of the Andrews straight wire appliance, in Orthodontics: State of the Art, Essence of the Science, ed. L.W. Graber, C.V. Mosby, St. Louis, 1986, pp. 279-298.