CASE REPORT
Unexpected Tooth Movement Under Bonded Retainers
Stability of orthodontic treatment results requires long-term retention, possibly throughout the patient’s lifetime, to prevent relapse and manage ongoing side effects of the dentition’s aging processes.1 In addition to prescribing removable retention appliances for nighttime wear, orthodontists commonly bond lingual retainer wires,2,3 which can be effective independent of patient cooperation.
In recent years, there have been an increasing number of reported cases with unexpected tooth movements despite the presence of fixed retainers.4-10 Undesirable tooth movements have included torque differences between two adjacent incisors (“X” effect), opposite torque of canines (twist effect), and increased buccal or lingual inclination of single canines.7-9,11,12 When such movements show no similarities to the pretreatment malocclusion, they are considered to be a newly developed post-treatment malocclusion rather than re-lapse.9,11,12
Little is known about the etiology of these tooth movements, since they have been identified primarily in case reports.4-6,8,11-14 Their prevalence ranges from 1.1% to 43.3% for mandibular retainers7,9,11,12 and 20.9% for maxillary retainers.15 The reported movements have almost always involved flexible spiral or dead-soft wire retainers with six bonding points from canine to canine,4-15 although one patient exhibited bilateral intercanine expansion beneath a stiff retainer wire bonded only to the two canines.8
This case report describes a patient who experienced severe buccal inclination of the lower left canine in the presence of two different bonded retainers (a stiff wire followed by a flexible spiral wire). A retrospective analysis including three-dimensional superimposition of dental casts reveals a canine movement tendency under stiff wire retention that was not noted clinically.
Diagnosis and Treatment Planning
A 24-year-old female presented with the chief complaint of a progressive buccal inclination of the lower left canine (Fig. 1).

Fig. 1 24-year-old female patient with progressive buccal inclination of lower left canine nine years after end of active orthodontic treatment and supervised retention period.
She had previously been treated in our department for a Class II, division 1 malocclusion, beginning at age 9 (Fig. 2).
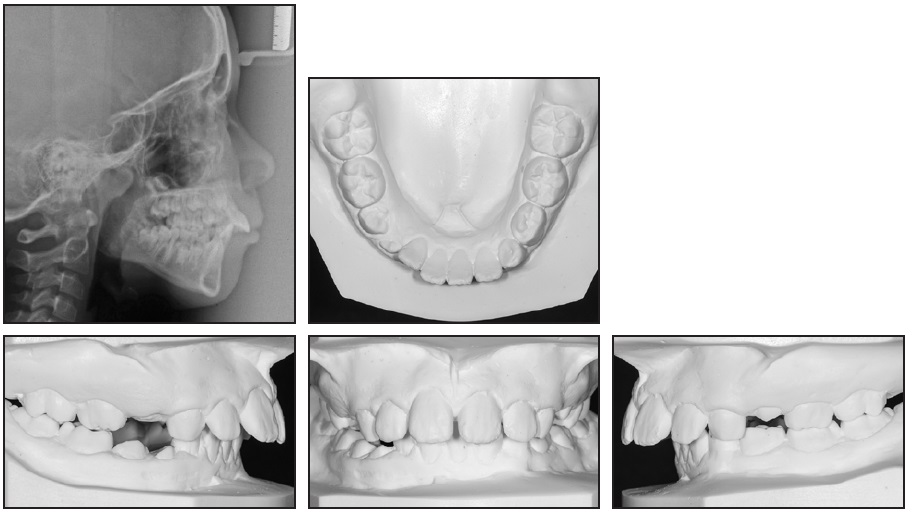
Fig. 2 9-year-old patient with Class II, division 1 malocclusion, strained lip closure, skeletal Class II relationship, and hyperdivergent jaw relationship before treatment.
At that time, she displayed habitual mouthbreathing, along with a low resting position of the tongue. The lateral cephalogram showed adenoid hypertrophy and strained lip closure. Cephalometric analysis indicated a skeletal Class II relationship and a hyper-divergent jaw relationship (Table 1).
Treatment Progress
Orthodontic treatment had been performed with a removable upper appliance for maxillary expansion, followed by an Andreasen activator and then full fixed Tip Edge* preadjusted appliances. The proclined upper incisors were retruded, while the lower incisors showed a slight proclination during treatment. The hyperdivergent jaw relation-ship persisted (Fig. 3).
An .024" stainless steel retainer wire was bonded only to the two lower canines.
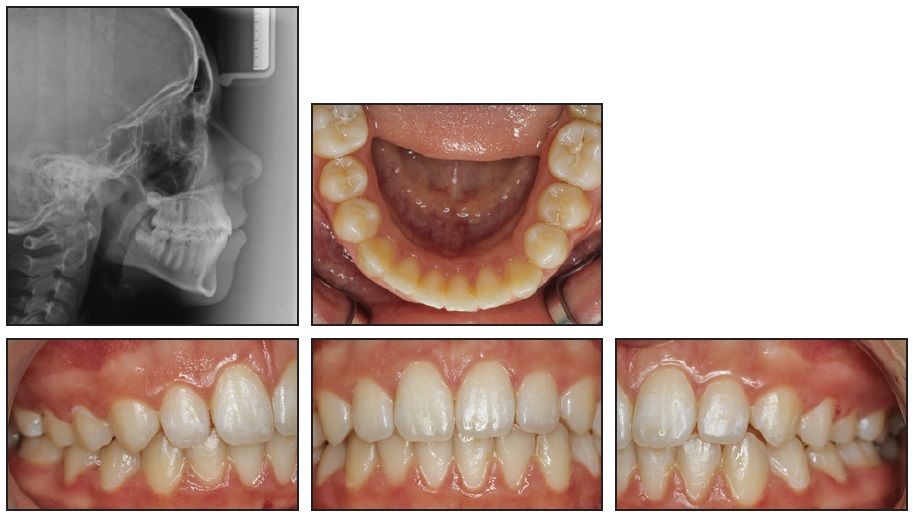
Fig. 3 Patient after three and one-half years of treatment.
Treatment Results
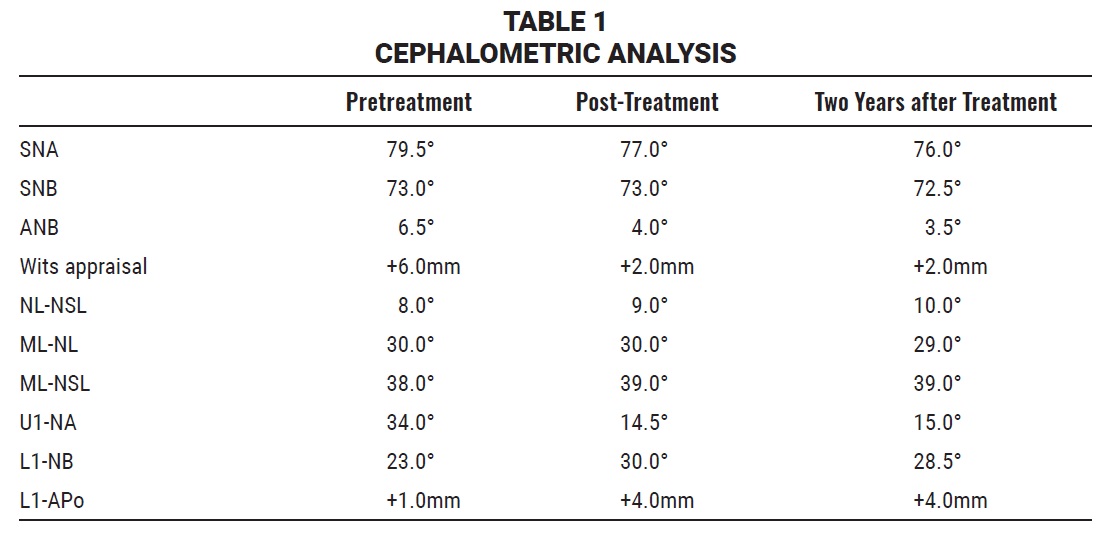
After 26 months of supervised retention, the patient was dismissed from regular appointments (Fig. 4).

Fig. 4 Patient after 26 months of retention. Note slight increase in buccal inclination of lower left canine despite good overall settling.
Cephalometric analysis showed that the skeletal Class I and the hyperdivergent jaw relationships, as well as the incisor inclination, remained stable during the retention period (Table 1).
Nine years later, the patient reported that after debonding of her initial stiff-wire retainer some years earlier, another dentist had bonded a new lower retainer to all six anterior teeth. Clinical examination found a flexible spiral-wire retainer with five out of six intact bonding sites, from the lower left canine to the right lateral incisor. The patient could not recall a particular time when the unwanted tooth movement had begun, but we removed the retainer to prevent any further progression. New diagnostic records were taken.
During retreatment planning, all previous plaster casts and photographs were carefully analyzed. A comparison of intraoral photographs from the initial debonding appointment and the end of the supervised retention period indicated not only a minor proclination of the central incisors, but a slight tendency of the lower left canine toward buccal inclination (Fig. 4). The plaster casts from these time points were then digitized using a desk-top scanner** to create standard tessellation lan-guage (STL) files. A 3D superimposition was per-formed with Viewbox 4*** software, using a protocol previously reported for the superimposition of maxillary dental casts.16,17 In our case, because of the lack of stable anatomical landmarks in the mandible, the crowns of the premolars and first molars were used as reference points (Fig. 5A).15,18 After superimposition, a color-coded distance map was created to indicate deviations of the superimposed models from 1.5mm to –1.5mm, highlighting the movement tendency of the lower left canine (Fig. 5B).
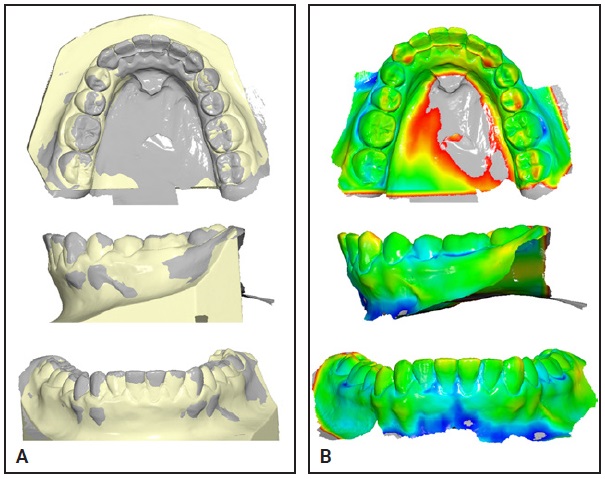
Fig. 5 A. Superimposition of digitized post-treatment (yellow) and post-retention (gray) models, according to best fit of premolar and first-molar crowns. B. Color map indicating deviations from 1.5mm (red) to –1.5mm (blue), based on postretention model; gray areas fall outside this range.
The plaster casts from the retreatment records were digitized and super-imposed on the postretention casts in the same manner. That superimposition and color map emphasized the worsening inclination of the left lower canine, as well as the resulting retrusion of the central incisors (Fig. 6).
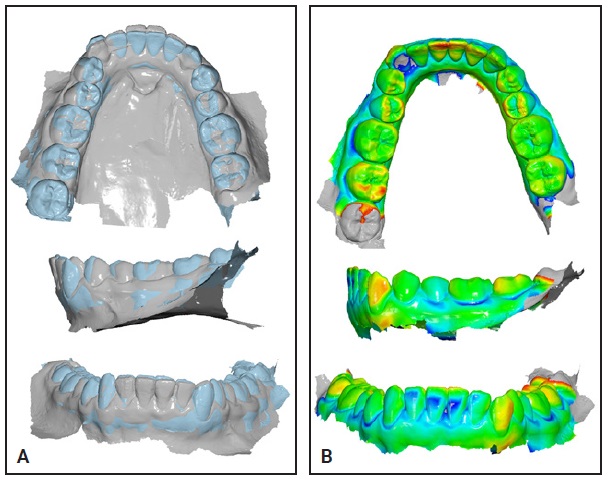
Fig. 6 A. Superimposition of digitized postretention (gray) and current (blue) models, according to best fit of premolars and first molars. B. Color map indicating deviations from 1.5mm (red) to –1.5mm (blue), based on current model; gray areas fall outside this range.
Discussion
At first glance, this case seemed to be a typical incidence of unintended tooth movement under a fixed flexible spiral-wire retainer. Careful analysis of all available records, however—with the added advantage of 3D superimposition—revealed the movement tendency of the lower left canine during retention with the initial stiff retainer wire. The flexible spiral-wire replacement retainer seemed to intensify, rather than limit, this inclination tendency.
Although the etiology of such complications is not yet known, some potential factors have been discussed. Iatrogenic activation during bonding has been assumed by some authors and cannot be completely ruled out in the present case.7-9,13,14 The patient reported, however, that her new retainer had been bonded some years earlier; any undesirable effects of an active retainer should occur within a few weeks of bonding. Wire fatigue or deformation from masticatory forces,8,9,11,14 as described by several in vitro studies,19,20 could also have been involved. Our patient’s flexible spiral- wire retainer did show some signs of wire fatigue—at the time she presented in our clinic, it was bonded to only five teeth, with an assumed wire fracture between the lower right lateral incisor and canine.
To date, only three systematic retrospective studies have examined unwanted tooth movements despite fixed retention with multistranded retainer wires. Kucera and Marek, in an analysis of 3,500 retention patients, found 1.1% of the sample to be affected by a twist effect, an “X” effect, or other unprescribed tooth movements.9 This group was associated with a lower average age at debonding, a proclined position of the lower incisor relative to APo, and a greater mandibular-plane angle. Wolf and colleagues, in a study of 30 consecutively treated patients using 3D superimposition of dental casts, reported that 30% were moderately affected and 13.32% severely affected by the twist effect, noting an association with intercanine expansion or excessive overjet correction during orthodontic treatment.7 Klaus and colleagues found 14.1% of the lower fixed retainers in 163 patients to be affected by unwanted tooth movements.15 Compared to a control group, the affected patients were more likely to present with oral dysfunctions or habits prior to orthodontic treatment. These patients were also more likely to display an incisal overlap without interincisal contact—attributable to an abnormal resting position of the tongue or a tongue-thrust swallowing habit—resulting in orovestibular forces on the retained segments.15 Although Shaughnessy and colleagues have suggested that the magnitude and duration of tongue pressure are less than the force needed to bend a wire,8 the unwanted tooth movement may have been caused not by the wire itself, but by the altered biomechanical properties of the retained teeth. Because of the fixed wire, the retained segment works like a cantilever arm, transmitting the forces exerted on single teeth to the entire segment.
Several of these pretreatment- or treatment-related factors were present in our case: although the patient initially had normally positioned lower incisors (L1-APo = +1mm), she exhibited an excessive mandibular-plane angle (ML-NSL = 38°) and habitual mouthbreathing, along with a low resting position of the tongue. Additionally, her overjet was reduced by 8mm during orthodontic treatment.
The increasing digitization of dental records offers the opportunity to use serial model super-imposition, based on either digitized plaster casts or intraoral scans, for assessment of orthodontic tooth movement. While the hard palate around the third rugae provides acceptable stability for digital superimposition in the maxilla, however, there is no stable structure available for mandibular super-imposition.21 Three retrospective studies used dental superimpositions on the molars and premolars to analyze unwanted tooth movements during retention.7,15,18 Of course, a dental superimposition has limitations, which increase over time—for example, changes in tooth positions can be caused by post-orthodontic settling or eruption and dento-facial growth, and minor changes in tooth morphology can occur due to abrasion, attrition, and erosion. Although a more precise method may be needed for research purposes, the dental superimposition should be accurate enough for clinical purposes; in the present case, it proved its superiority over the visual inspections performed during the patient’s supervised retention period.
Within the limitations of a case report, no solid conclusions can be drawn regarding the risks of and reasons for unexpected tooth movements during fixed retention. Further research is needed to elucidate the underlying principles and causes of this complication. Because the present superimposition technique is time-consuming, further development of automated serial superimpositions of digital casts or intraoral scans could help in the detection of tooth movement tendencies before they become clinically visible, thus reducing the number of severe cases requiring retreatment, as the present one did.
In clinical practice, any type of bonded retainer must be carefully supervised as long as it is in place. Orthodontists, patients, and general dentists all need to pay attention to even minor signs of unwanted tooth movement. Clinicians may also want to consider the addition of removable appliances to avoid overreliance on bonded retainers.
FOOTNOTES
- *Registered trademark of TP Orthodontics, Inc., La Porte, IN; www.tportho.com.
- **OrthoX, registered trademark of Dentaurum GmbH & Co., Ispringen, Germany; www.dentaurum.de.
- ***Registered trademark of dHAL Software, Kifissia, Greece; www.dhal.com.
REFERENCES
- 1. Littlewood, S.J.: Evidence-based retention: Where are we now? Semin. Orthod. 23:229-236, 2017.
- 2. Pratt, M.C.; Kluemper, G.T.; Hartsfield, J.K. Jr.; Fardo, D.; and Nash, D.A.: Evaluation of retention protocols among members of the American Association of Orthodontists in the United States, Am. J. Orthod. 140:520-526, 2011.
- 3. Padmos, J.A.D.; Fudalej, P.S.; and Renkema, A.M.: Epidemiologic study of orthodontic retention procedures, Am. J. Orthod. 153:496 504, 2018.
- 4. Pizarro, K. and Jones, M.L.: Crown inclination relapse with multiflex retainers, J. Clin. Orthod. 26:780-782, 1992.
- 5. Kucera, J.; Streblov, J.; Marek, I.; and Hanzelka, T.: Treatment of complications associated with lower fixed retainers, J. Clin. Orthod. 50:54-59, 2016.
- 6. Laursen, M.G.; Rylev, M.; and Melsen, B.: Treatment of complications after unintentional tooth displacement by active bonded retainers, J. Clin. Orthod. 50:290-297, 2016.
- 7. Wolf, M.; Schulte, U.; Küpper, K.; Bourauel, C.; Keilig, L.; Papageorgiou, S.N.; Dirk, C.; Kirschneck, C.; Daratsianos, N.; and Jäger, A.: Post-treatment changes in permanent retention, J. Orofac. Orthop. 77:446-453, 2016.
- 8. Shaughnessy, T.G.; Proffit, W.R.; and Samara, S.A.: Inadvertent tooth movement with fixed lingual retainers, Am. J. Orthod. 149:277-286, 2016.
- 9. Kucera, J. and Marek, I.: Unexpected complications associated with mandibular fixed retainers: A retrospective study, Am. J. Orthod. 149:202-211, 2016.
- 10. Egli, F.; Bovali, E.; Kiliaridis, S.; and Cornelis, M.A.: Indirect vs direct bonding of mandibular fixed retainers in orthodontic patients: Comparison of retainer failures and posttreatment stability: A 2-year follow-up of a single-center randomized con-trolled trial, Am. J. Orthod. 151:15-27, 2017.
- 11. Katsaros, C.; Livas, C.; and Renkema, A.M.: Unexpected complications of bonded mandibular lingual retainers, Am. J. Orthod. 132:838-841, 2007.
- 12. Renkema, A.M.; Renkema, A.; Bronkhorst, E.; and Katsaros, C.: Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers, Am. J. Orthod. 139:614-621, 2011.
- 13. Abudiak, H.; Shelton, A.; Spencer, R.J.; Burns, L.; and Littlewood, S.J.: A complication with orthodontic fixed retainers: A case report, Orthod. Update 4:112-117, 2011.
- 14. Pazera, P.; Fudalej, P.S.; and Katsaros, C.: Severe complication of a bonded mandibular lingual retainer, Am. J. Orthod. 142:406-409, 2012.
- 15. Klaus, K.; Xirouchaki, F.; and Ruf, S.: 3D-analysis of unwanted tooth movements despite bonded orthodontic retainers: A pilot study, BMC Oral Health 20:308, 2020.
- 16. Vasilakos, G.; Koniaris, A.; Wolf, M.; Halazonetis, D.; and Gkantidis, N.: Early anterior crossbite correction through posterior bite opening: A 3D superimposition prospective cohort study, Eur. J. Orthod. 40:364-371, 2018.
- 17. Vasilakos, G.; Schilling, R.; Halazonetis, D.; and Gkantidis, N.: Assessment of different techniques for 3D superimposition of serial digital maxillary dental casts on palatal structures, Sci. Rep. 7:5838, 2017.
- 18. Knaup, I.; Bartz, J.R.; Schulze-Späte, U.; Craviero, R.B.; Kirschneck, C.; and Wolf, M.: Side effects of twistflex retainers: 3D evaluation of tooth movement after retainer debonding, J. Orofac. Orthop. 82:121-130, 2021.
- 19. Sifakakis, I.; Pandis, N.; Eliades, T.; Makou, M.; Katsaros, C.; and Bourauel, C.: In-vitro assessment of the forces generated by lingual fixed retainers, Am. J. Orthod. 139: 44-48, 2011.
- 20. Sifakakis, I.; Eliades, T.; and Bourauel; C.: Residual stress analysis of fixed retainer wires after in vitro loading: Can mastication- induced stresses produce an unfavorable effect? Biomed. Tech. (Berl.) 60:617-622, 2015.
- 21. Stucki, S. and Gkantidis, N.: Assessment of techniques used for superimposition of maxillary and mandibular 3D surface models to evaluate tooth movement: A systematic review, Eur. J. Orthod. 42:559-570, 2020.





COMMENTS
.