CASE REPORT
Reverse Engineering for Post-Treatment Analysis of a Surgical-Orthodontic Case
Advances in technology, such as computer-aided design and manufacturing (CAD/CAM), have made virtual setup models a viable option for orthodontic diagnosis and treatment planning.1 Studies have confirmed that digital analysis and setup can accurately reproduce dental features and orthodontic treatment effects.2-6
An accurate prediction setup is particularly essential in planning complex surgical-orthodontic cases.7,8 This case report describes a virtual setup method and digital analysis of various presurgical orthodontic options 15 years after treatment, using reverse-engineering technology.9,10
Diagnosis and Treatment Planning
A 24-year-old female with a hyperdivergent facial profile, long lower facial third, lip incompetence, vertical maxillary excess, excessive nasolabial angle, and posteriorly positioned mandible presented for treatment (Fig. 1). She exhibited a Class II malocclusion with excessive overjet, anterior deep bite, coincident midlines, a deep curve of Spee in the lower arch, and crowding in both arches. Diagnosis and treatment planning were performed using traditional methods, including plaster casts. Cephalometric analysis indicated a narrow symphysis, retroclined upper incisors, proclined lower incisors, and an excessive mandibular-plane angle (Table 1). A panoramic radiograph revealed bilateral condylar remodeling and three impacted third molars.
Similar articles from the archive:
- Generating an Ideal Virtual Setup with Three-Dimensional Crowns and Roots November 2015
- CASE REPORT "Surgery First" Maxillary Segmental and Mandibular Osteotomies with Invisalign Therapy February 2022
- CASE REPORT Surgical-Orthodontic Treatment of Class II Malocclusion with Maxillary Vertical Excess June 2009
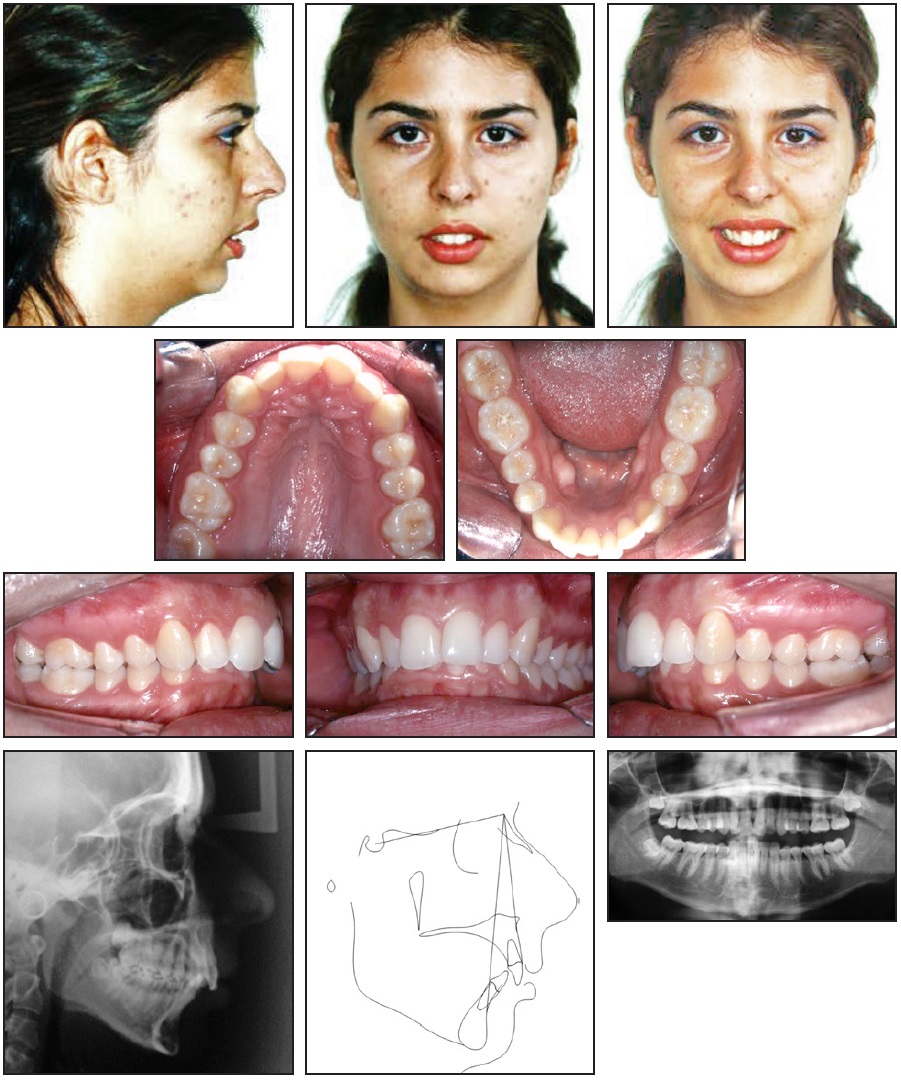
Fig. 1 24-year-old female patient with Class II malocclusion, hyperdivergent facial profile, excessive overjet, and anterior deep bite before treatment.
Treatment objectives were to improve the facial appearance, achieve normal overbite and overjet, correct the upper and lower crowding, improve the chin projection, obtain lip competence, reduce the proclination of the lower incisors, procline the upper incisors, and establish a stable and functional occlusion. Considering the patient’s convex profile and Class II malocclusion, we recommended surgical-orthodontic treatment. The first option for the orthodontic phase was a nonextraction approach in which the dental arches would be leveled and aligned while the crowding, lower curve of Spee, and upper-incisor inclination were corrected. The second option involved extraction of the lower first premolars to allow retraction of the canines and incisors without loss of anchorage, thus providing enough overjet for the mandibular advancement surgery. The crowding, curve of Spee, and upper- and lower-incisor inclination would also be resolved. A third alternative was to extract the upper second premolars as well and to close the spaces with loss of anchorage, adding labial torque to the upper incisors to improve their inclination. This third option was selected.
Treatment Progress
After extraction of the upper second and lower first premolars, .022" Roth-prescription brackets and a lower lingual arch were placed. Wires in both arches progressed from .014" to .016" × .022" nickel titanium, followed by .017" × .025" stainless steel. In the upper arch, the spaces were closed with anchorage loss and labial torque of the upper incisors. Anterior retraction was finished with the insertion of nickel titanium closed-coil springs on a three-piece .017" × .025" stainless steel archwire. Posterior miniplates were inserted on both sides of the mandibular body and tied to the lower molars for anchorage control.11,12 The lower canines and incisors were intruded with three-piece mechanics, while side effects in the anchorage unit were controlled by the miniplates.
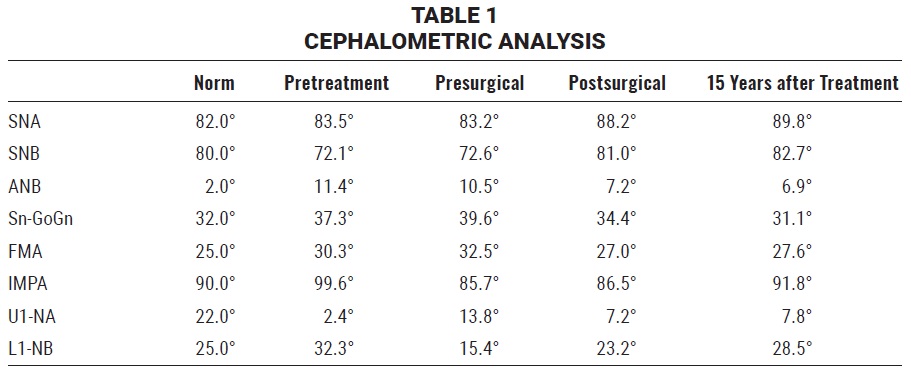
After 19 months, all spaces were closed and leveling and alignment were complete, resulting in a 13.9mm positive overjet (Fig. 2A). At this time, the .021" × .025" stainless steel surgical archwires were inserted. Spaces were left between the upper incisors for later cosmetic correction of a 4.23mm anterior tooth-size discrepancy. Comparison of the pretreatment and presurgical lateral cephalograms confirmed the upper and lower incisor decompensation.
A three-piece Le Fort I maxillary osteotomy was then performed to simultaneously correct the transverse, vertical, and sagittal discrepancies. Bilateral sagittal split osteotomies were used to provide mandibular advancement and counterclockwise rotation. The segments were fixated by rigid bone plates and screws.
Immediately after surgery, bilateral Class I molar and canine relationships and a normal overbite and overjet could be observed (Fig. 2B). During the postoperative orthodontic phase, the occlusion was maintained using intermaxillary vertical elastics.
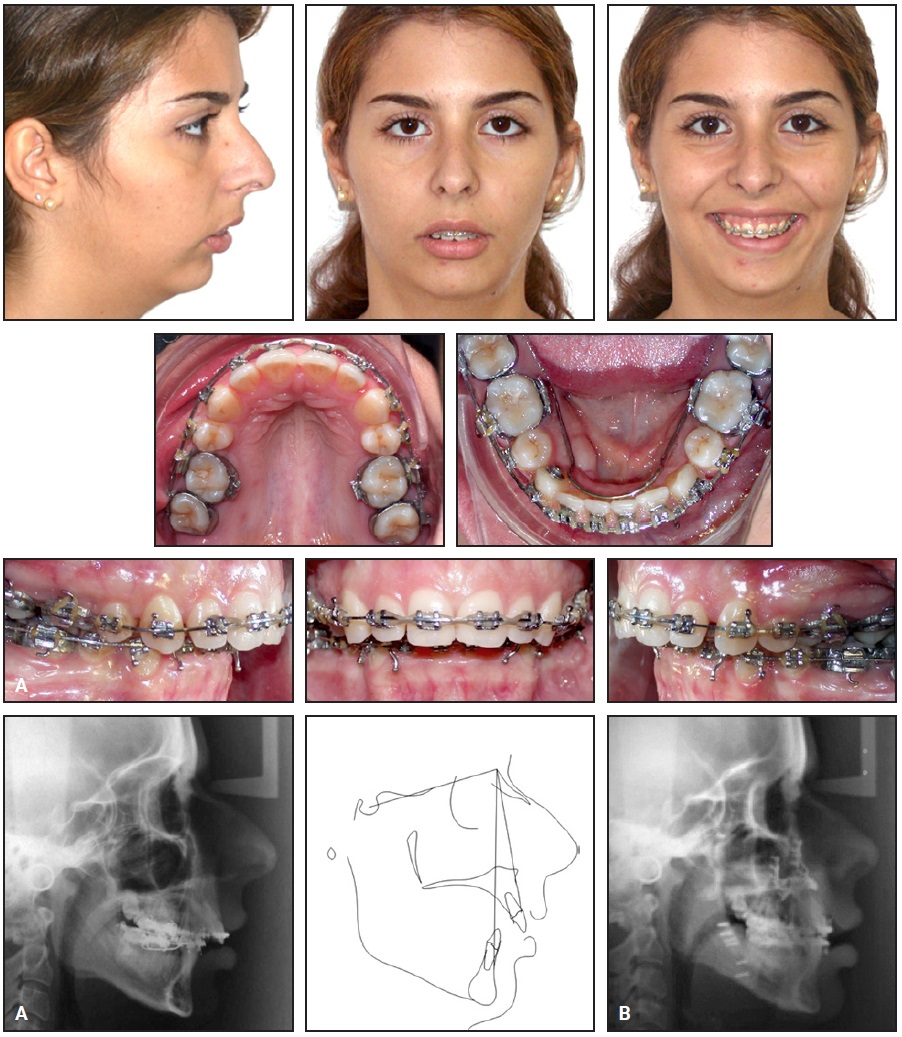
Fig. 2 A. After 19 months of orthodontic treatment, .021" × .025" stainless steel surgical archwires inserted. B. Lateral cephalogram taken immediately after surgery.
Seven months after surgery, the fixed appliances were removed. An .018" lingual 3-3 retainer wire was bonded, and an upper Hawley retainer was delivered.
Treatment Results
Post-treatment records showed an improvement in the facial profile (Fig. 3). The lip incompetence was corrected, and the upper-incisor display was adequate. A good occlusion was produced, with Class I molar and canine relationships on both sides. Normal overbite and overjet were achieved, and the upper and lower midlines remained coincident. Cephalometric assessment confirmed maxillomandibular advancement with counterclockwise rotation of the occlusal plane and an improvement in the incisor inclination (Table 1).

Fig. 3 Patient after 26 months of surgical-orthodontic treatment.
Fifteen years after treatment, the facial profile and the Class I molar and canine relationships remained stable (Fig. 4). Some relapse of the overbite and incisor crowding could be observed in the lower arch. Cephalometric assessment confirmed the maxillomandibular stability and increased overbite.
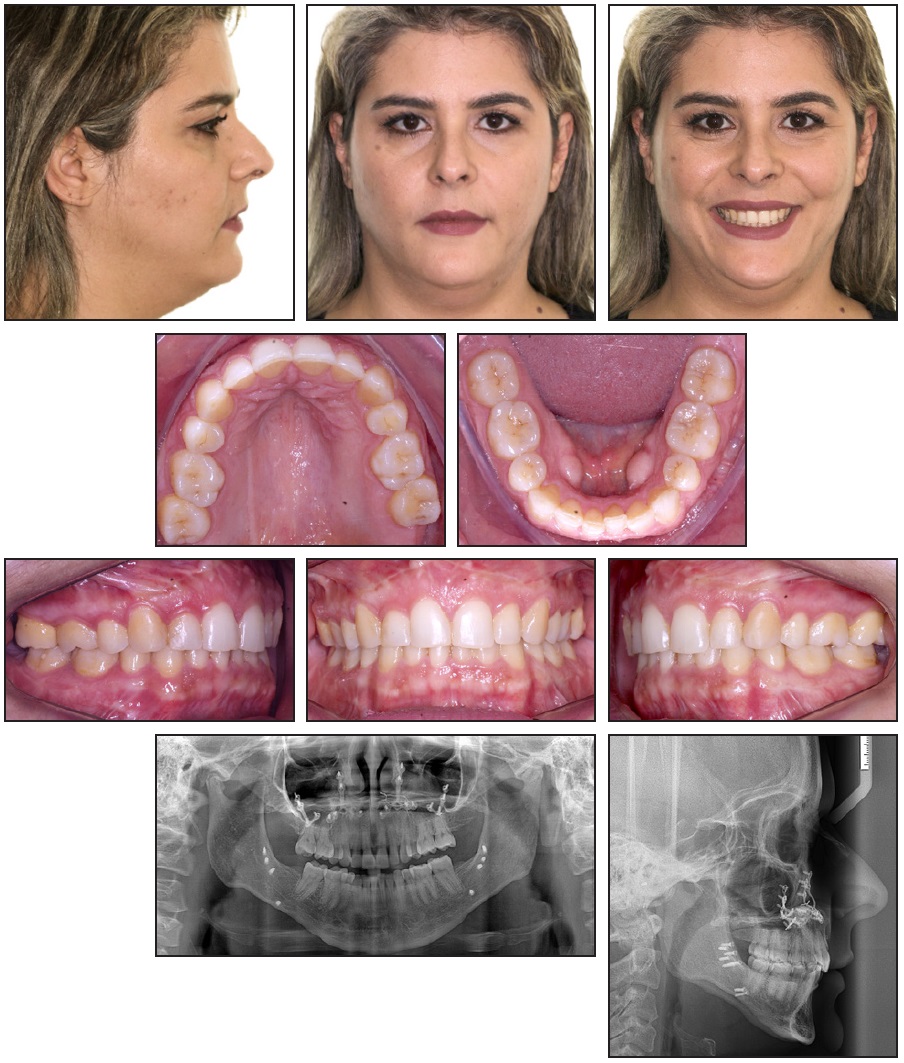
Fig. 4 Patient 15 years after treatment.
Virtual Treatment Simulation
After the 15-year follow-up records were taken, the original orthodontic plan was reanalyzed using a virtual setup. The original upper and lower presurgical plaster casts were scanned with Identica Light Scanner,* saved as STL files, and exported to 3D Slicer** version CMF 4.0. The patient’s initial pretreatment casts were also scanned, and a virtual presurgical orthodontic setup of the STL files was performed using SureSmile Elemetrix*** software and exported to 3D Slicer. The actual presurgical casts and the virtual setups were then superimposed using landmarks at the upper right canine, incisal papilla, and left canine and the mesial cusps of the lower first and second molars (Fig. 5).
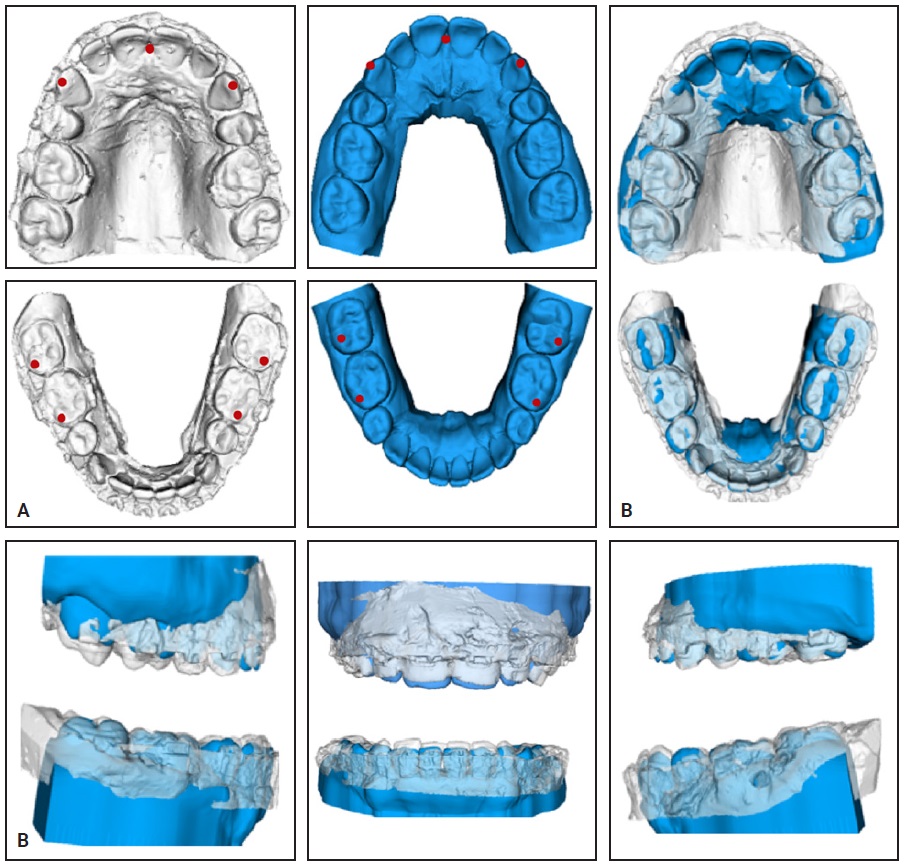
Fig. 5 A. Landmarks applied to upper right canine, incisal papilla, and left canine and to mesial cusps of lower first and second molars on scans of original presurgical casts (white) and virtual setups (blue). B. Superimposition of presurgical casts and virtual setups.
The superimpositions showed minor differences between the presurgical casts and the virtual setup. The upper right molars were more extruded and the upper arch was narrower on the original model. The lower arches differed in arch width (more constricted in the virtual setup) and in the vertical position of the canines and incisors (more extruded on the original model).
The three original treatment options were analyzed with SureSmile Elemetrix using the STL files of the patient’s pretreatment casts. The nonextraction simulation resulted in satisfactory leveling and alignment of both arches, as well as a curve of Spee correction due to incisor intrusion and proclination (Fig. 6A). The second approach, involving extraction of only the two lower first premolars, resulted in a larger overjet, which would have allowed more significant mandibular advancement than the nonextraction option (Fig. 6B). This simulation also showed, however, that the upper second molars would have had no opposing teeth after orthognathic surgery, which could have
led to their overeruption. The four-premolar extraction plan was clearly the most appropriate for this case because it allowed for correction of the curve of Spee, inclination of the incisors, and adequate mandibular advancement, and it established a stable and functional occlusion (Fig. 6C).
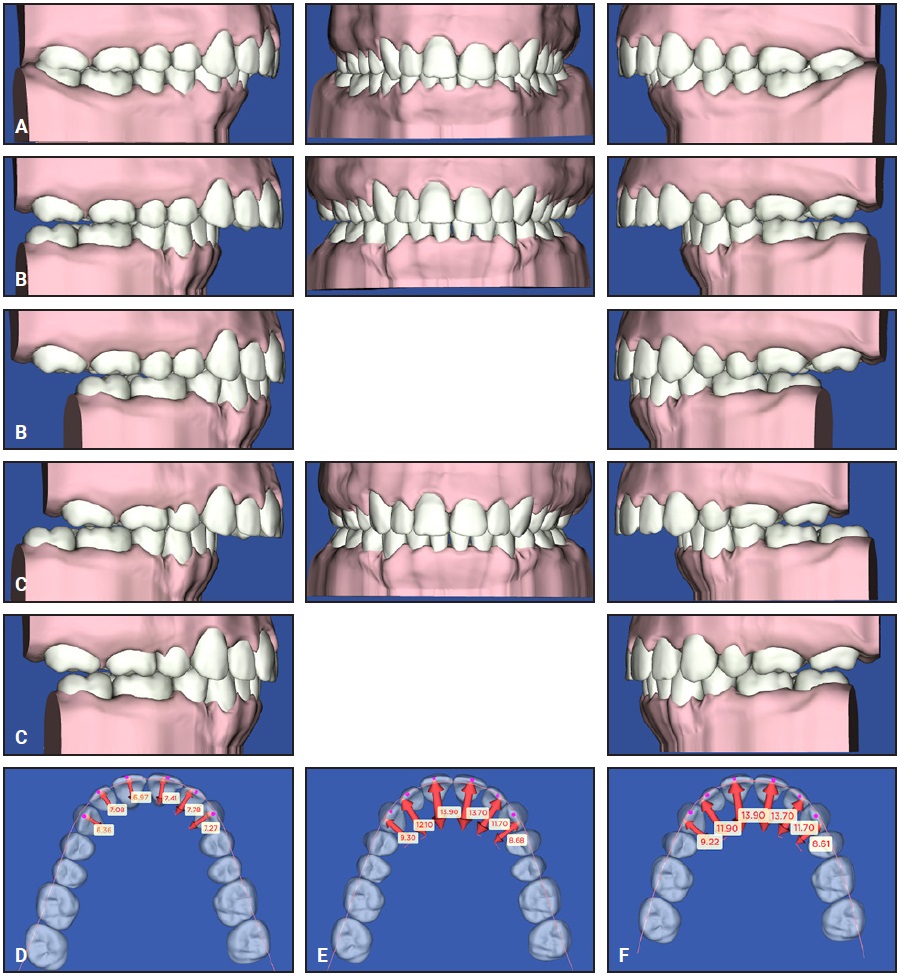
Fig. 6 A. Virtual setup of nonextraction treatment option prior to surgery. B. Virtual setup of lower first-premolar extraction treatment option prior to surgery and after simulation of surgical mandibular advancement. C. Virtual setup of four-premolar extraction treatment option and postsurgical simulation. D. Overjet after nonextraction simulation. E. Overjet after two-lower premolar extraction simulation. F. Overjet after four-premolar extraction simulation.
Discussion
Reverse engineering involves steps such as data acquisition, preprocessing (noise filtering and merging), triangulation, feature extraction, segmentation, and surface fitting.13 Already well established in the medical field, it has a number of potential applications for dentistry and orthodontics, including 3D model scanning and superimposition, digital diagnostic setups, volumetric evaluation of tooth wear, 3D soft-tissue facial analysis, and smile assessment.13,14
Digital setups are as useful and accurate as manual setups and can be reliably reproduced.6 There is a significant difference, however, in inter- and intraexaminer reliability of digital orthodontic setups.15 The virtual setups in the present report were performed by a single orthodontist.
Among the many advantages of digital models is the possibility of adding spatial registration at different points in time.16,17 The stability of the palatal rugae as a reference point has been confirmed using dental casts.18 Since neither external cranial references nor palatal rugae were visible in our setup models created with SureSmile Elemetrix, we had to devise a landmark method.
Decisions regarding the need for extractions in orthodontic therapy depend on more than the presence or absence of space in the dental arches.19 Factors such as the curve of Spee, incisor proclination, facial harmony, stability of results,19 and potential for surgical correction must be evaluated to ensure the best functional and esthetic results.
Natural physiological adaptation or previous orthodontic compensation may have reduced the dental discrepancy by worsening the skeletal discrepancy.20 Such a disparity needs to be corrected before orthognathic surgery is performed. In the case shown here, the presurgical orthodontic decompensation—uprighting of the lower incisors and proclination of the upper incisors—enabled the ideal mandibular advancement and reduced the degree of counterclockwise rotation.21
It is well documented that the type of force and duration of treatment have a greater impact on root resorption than the magnitude of force.22 Continuous forces can be more harmful than intermittent forces in some cases, and superelastic wires can cause greater root resorption than stainless steel wires.23 In the present case, we used heavy rectangular wires, filling the bracket slots, to control torque during the lower-arch retraction and to decompensate the upper arch.24 The primary risk of using heavy archwires occurs when they are placed too early in treatment, thus producing inordinate forces as well as root resorption. Another risk is that excessive torque may cause fenestration or dehiscence, especially in the lower incisors. This is particularly dangerous when the mandibular symphysis is thin.
In our case, the absence of a bonded lower lingual retainer may have contributed to a relapse of lower-incisor alignment. Craniofacial growth and development are continuous processes, however, and dimensional changes can occur naturally throughout life.20 A recent report showed a significant decrease (.69mm) in mandibular intercanine width between the ages of 17 and 60 in untreated patients.25 This effect may be associated with late incisor crowding as a result of mesial or lingual canine displacement.26 The dimensional changes found in our patient 15 years after treatment are consistent with those described in the literature.
A limitation of this case report is the lack of cephalometric superimpositions. The pretreatment images were taken under previous protocols, and we had access only to copies of x-rays without proper standardization for linear measurements (which is why Table 1 shows only angular values). Nevertheless, our post-treatment reverse engineering shows how simulation software can offer an alternative to physical setups in evaluating potential treatment outcomes and stability. In this case, we could have demonstrated to the patient the advantages of extracting four premolars instead of two or none.
FOOTNOTES
- *Registered trademark of Medit Corp, Seoul, Korea; www.medit.com.
- **3D Slicer is a free, open-source, multi-platform software package widely used for medical, biomedical, and related imaging research; www.slicer.org.
- ***Registered trademark of Dentsply Sirona, York, PA; www.dentsplysirona.com.
REFERENCES
- 1. Duret, F.; Blouin, J.L.; and Duret, B.: CAD-CAM in dentistry, J. Am. Dent. Assoc. 117:715-720, 1988.
- 2. Rossini, G.; Parrini, S.; Castroflorio, T.; Deregibus, A.; and Debernardi, C.L.: Diagnostic accuracy and measurement sensitivity of digital models for orthodontic purposes: A systematic review, Am. J. Orthod. 149:161-170, 2016.
- 3. Fleming, P.S.; Marinho, V.; and Johal, A.: Orthodontic measurements on digital study models compared with plaster models: A systematic review, Orthod. Craniofac. Res. 14:1-16, 2011.
- 4. Stevens, D.R.; Flores-Mir, C.; Nebbe, B.; Raboud, D.W.; Heo, G.; and Major, P.W.: Validity, reliability, and reproducibility of plaster vs digital study models: Comparison of peer assessment rating and Bolton analysis and their constituent measurements, Am. J. Orthod. 129:794-803, 2006.
- 5. Barreto, M.S.; Faber, J.; Vogel, C.J.; and Araujo, T.M.: Reliability of digital orthodontic setups, Angle Orthod. 86:255-259, 2016.
- 6. Bianchi, J.; Paniagua, B.; Oliveira Ruellas, A.C.; Fillion-Robin, J.C.; Prietro, J.C.; Gonçalves, J.R.; Hoctor, J.; Yatabe, M.; Styner, M.; Li, T.F.; Gurgel, M.L.; Chaves, C.M.; Massaro, C.; Garib, D.G.; Vilanova, L.; Castanha Henriques, J.F.; Aliaga-Del Castillo, A.; Janson, G.; Iwasaki, L.R.; Nickel, J.C.; Evangelista, K.; and Cevidanes, L.: 3D Slicer craniomaxillofacial modules support patient-specific decision-making for personalized healthcare in dental research, Multimodal Learn. Clin. Decis. Supp. Clin. Image Based Proc. 12445:44-53, 2020.
- 7. Luther, F.; Morris, D.O.; and Hart, C.: Orthodontic preparation for orthognathic surgery: How long does it take and why? A restrospective study, Br. J. Oral Maxillofac. Surg. 41:401-406, 2003.
- 8. Camardella, L.T.; Rothier, E.K.; Vilella, O.V.; Ongkosuwito, E.M.; and Breuning, K.H.: Virtual setup: Application in orthodontic practice, J. Orofac. Orthop. 77:409-419, 2016.
- 9. Bradley, C. and Currie, B.: Advances in the field of reverse engineering, Comput. Aided Des. Appl. 2:697-706. 2005.
- 10. Chen, D.F. and Fang, M.L.: Reconstruction technique in reverse engineering, Proc. IEEE Int. Conf. Ind. Technol. (ICT 96) 37-41, 1996.
- 11. Sugawara, J.: JCO Interviews Dr. Junji Sugawara on the skeletal anchorage system, J. Clin. Orthod. 33:689-696, 1999.
- 12. Sugawara, J. and Nishimura, M.: Minibone plates: The skeletal anchorage system, Semin. Orthod. 11:47-56, 2005.
- 13. Ghafoor, H.: Reverse engineering in orthodontics, Turk. J. Orthod. 31:139-144, 2018.
- 14. Cha, B.K.: Clinical application of three-dimensional reverse engineering technology in orthodontic diagnosis, in Principles in Contemporary Orthodontics, IntechOpen, Rijeka, Croatia, 2011.
- 15. Fabels, L.N. and Nijkamp, P.G.: Interexaminer and intraexaminer reliabilities of 3-dimensional orthodontic digital setups, Am. J. Orthod. 146:806-811, 2014.
- 16. Grauer, D.; Cevidanes, L.H.; Tyndall, D.; Styner, M.A.; Flood, P.M.; and Proffit, W.R.: Registration of orthodontic digital models, Craniofac. Growth Ser. 48:377-391, 2011.
- 17. Anacleto, M.A. and Souki, B.Q.: Superimposition of 3D maxillary digital models using open-source software, Dent. Press J. Orthod. 24:81-91, 2019.
- 18. Hoggan, B.R. and Sadowsky, C.: The use of palatal rugae for the assessment of anteroposterior tooth movements, Am. J. Orthod. 119:482-488, 2001.
- 19. Ruellas, A.C.; Ruellas, R.M.; Romano, F.L.; Pithon, M.M.; and Santos, R.L.: Tooth extraction in orthodontics: An evaluation of diagnostic elements, Dent. Press J. Orthod. 15:134-157, 2010.
- 20. Bishara, S.E.; Treder, J.E.; and Jakobsen, J.R.: Facial and dental changes in adulthood, Am. J. Orthod. 106:175-186, 1994.
- 21. Larson, B.E.: Orthodontic preparation for orthognathic surgery, Oral Maxillofac. Surg. Clin. N. Am. 26:441-458, 2014.
- 22. Maltha, J.C.; Van Leeuwen, E.J.; Dijkman, G.E.; and Kuijpers-Jagtman, A.M.: Incidence and severity of root resorption in orthodontically moved premolars in dogs, Orthod. Craniofac. Res. 7:115-121, 2004.
- 23. Acar, A.; Canyürek, U.; Kocaaga, M.; and Erverdi, N.: Continuous vs. discontinuous force application and root resorption, Angle Orthod. 69:159-163, 1999.
- 24. Jacobs, J.D. and Sinclair, P.M.: Principles of orthodontic mechanics in orthognathic surgery cases, Am. J. Orthod. 84:399-407, 1983.
- 25. Massaro, C.; Miranda, F.; Janson, G.; Rodrigues de Almeida, R.; Pinzan, A.; Martins, D.R.; and Garib, D.: Maturational changes of the normal occlusion: A 40-year follow-up, Am. J. Orthod. 154:188-200, 2018.
- 26. Bondemark, L.; Holm, A.K.; Hansen, K.; Axelsson, S.; Mohlin, B.; Brattstrom, V.; Paulin, G.; and Pietila, T.: Long-term stability of orthodontic treatment and patient satisfaction, Angle Orthod. 77:181-191, 2007.







COMMENTS
.