Interdisciplinary Treatment of Patients with Cleidocranial Dysplasia and Multiple Unerupted Permanent Teeth
Cleidocranial dysplasia (CCD) is a condition with an autosomal dominant inheritance pattern,1,2 a relatively low incidence (about 1 in 1 million), and no predilection for sex or race.3-5 It is caused by a mutation in the RUNX2 gene in band 1, region 2, of the short arm of chromosome 6 (6p21). This gene encodes the core binding factor A protein that controls the differentiation and growth of osteoblast precursor cells, which are essential for endochondral and intramembranous ossification.6
CCD was first mentioned in 1765 by Martin, who commented on rudimentary clavicles in a 30-year-old man whose father and brother had been diagnosed with a similar malformation.7 Scheuthauer wrote about the syndrome in 1871, followed by Marie and Sainton, who emphasized the association of hypoplasia or aplasia of one or both clavicles with an exaggerated transverse skull diameter and late fontanelle ossification.1,7
The main features of CCD are head and clavicle malformations.2,7 Among the craniofacial manifestations of this syndrome, the following radiographic aspects can be observed: brachycephalic head type, hypertelorism, depressed nasal bridge, deficiency of nasal and lacrimal bones, faulty development of the foramen magnum, prominent parietal and frontal bones, underdeveloped and narrow paranasal sinuses, parallel mandibular ascending branches, distally curved coronoid process, hypoplastic zygomatic bone, and discontinuous zygomatic arch in the zygomaticotemporal suture.8 Various clinical aspects may also be present, including maxillary retrusion and deficiency, which may lead to an incorrect diagnosis of mandibular prognathism; incomplete fusion of the mental symphysis; poor ossification of the hyoid bone; prolonged retention of deciduous teeth; presence of supernumerary teeth; ectopic eruption; and the delay or lack of eruption of permanent teeth with resultant impaction.2,9 Crown abnormalities in the form of enamel hypoplasia and other problems such as root dilaceration, hypodontia, and dentigerous cysts are also commonly found in CCD.7
Although early extraction of deciduous teeth to promote spontaneous eruption of the succedaneous teeth is a reasonable approach, it is not always successful10 because the problem seems to arise from lack of bone resorption11 rather than a blockage of the eruption pathway. Because of the systemic alteration of bone ossification, several clinical conditions can coexist in this syndrome, including the presence of Wormian bones around the lambdoid suture, delayed ossification of the pelvic bones, and stunting of long bones leading to short stature, valgus knees, flat feet, scoliosis, short fingers, small hands and feet, hypoplastic nails, or bone fragility.12
This article describes the comprehensive orofacial treatment and long-term follow-up of a female patient with CCD.
Case Report
A 13-year-old female with multiple unerupted permanent teeth, multiple supernumerary teeth, and an anteroposterior maxillomandibular discrepancy was referred by her general dentist (Fig. 1). With the exception of the first permanent molars, all deciduous teeth were retained, with no evidence of eruption of the succedaneous teeth. The maxilla was deficient in both the sagittal and transverse dimensions, resulting in a posterior bilateral crossbite compensated by buccal tipping of the metallic crowns.
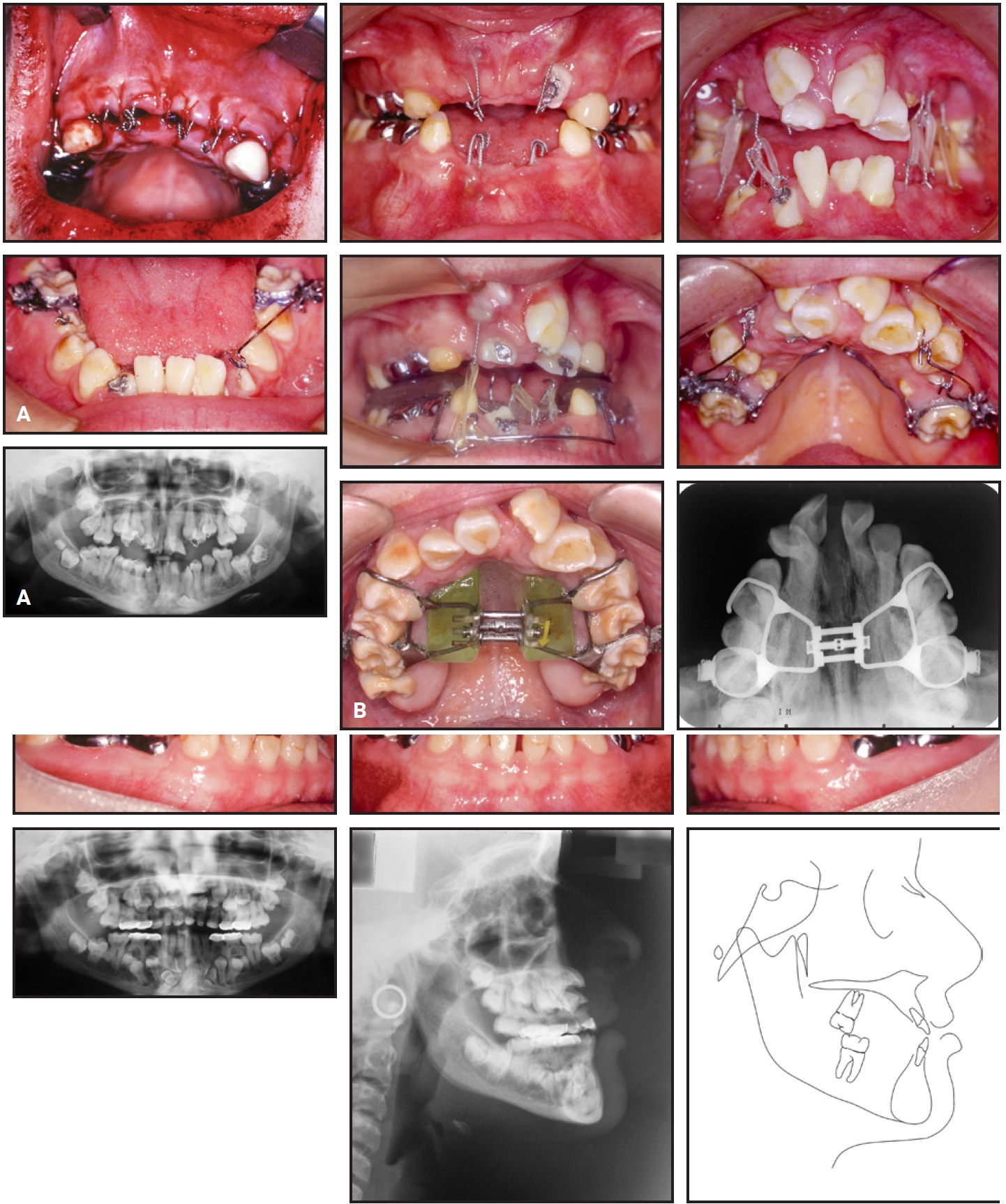
Fig. 1 13-year-old female patient with multiple unerupted permanent teeth, supernumerary teeth, and anteroposterior maxillomandibular discrepancy before treatment.
The patient’s family reported that all maxillary anterior deciduous teeth had been restored with pure porcelain crowns, and the mandibular anterior deciduous teeth with composite resin, at age 10 while awaiting spontaneous or forced eruption. Eight metal crowns had been cemented to the deciduous molars to improve masticatory function.
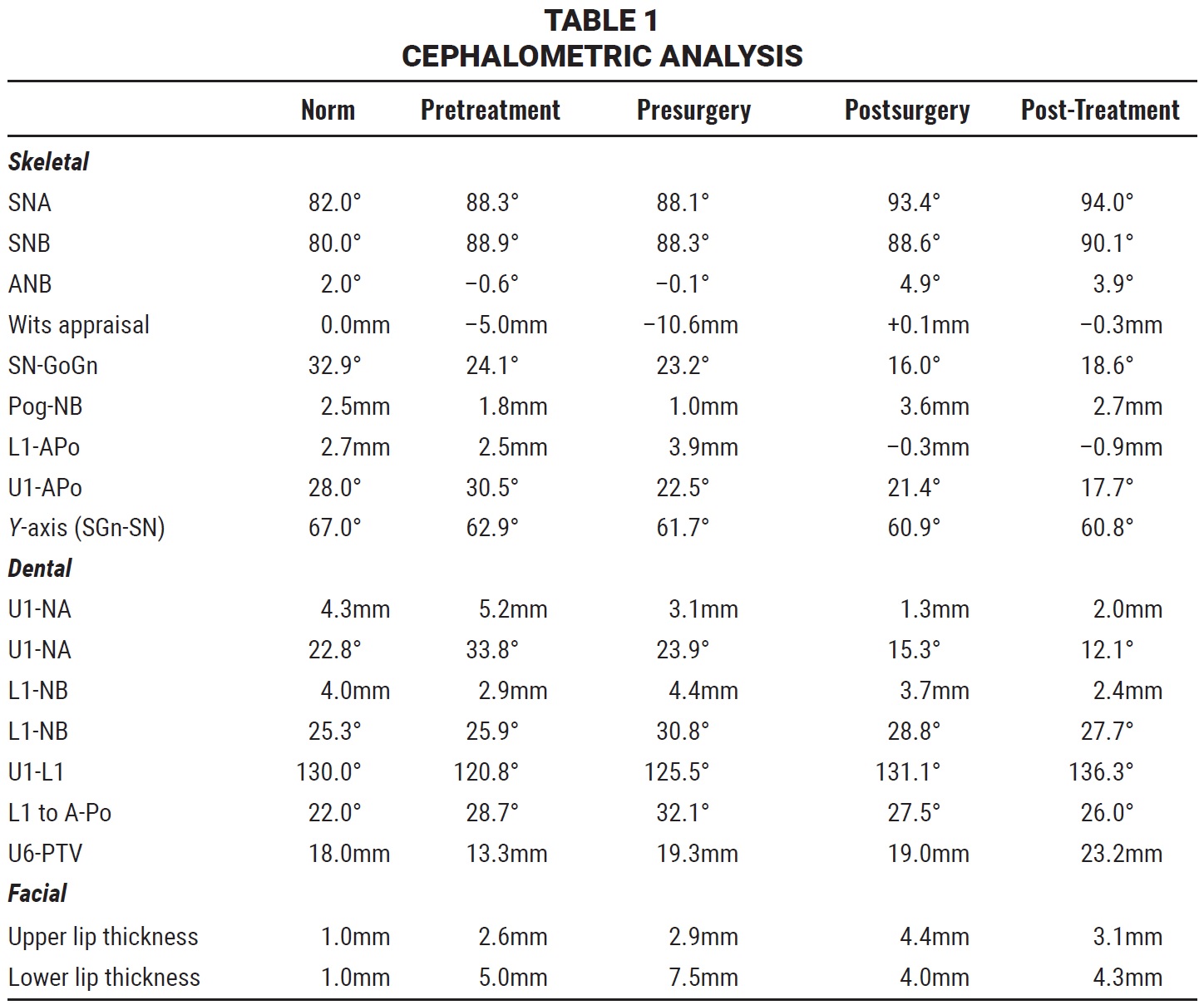
The panoramic radiograph revealed two supernumerary teeth in the maxillary arch and six in the mandibular arch, contributing to atypical intraosseous dental crowding and ectopic eruption pathways for the incisors and canines. A lateral cephalometric radiograph confirmed a midfacial growth deficiency and skeletal Class III malocclusion (Table 1).
Treatment objectives consisted of extracting the remaining deciduous teeth, exposing and extruding the unerupted and ectopic permanent teeth, extracting the supernumerary teeth, correcting the transverse discrepancy, aligning the dental arches, correcting the skeletal Class III malocclusion with orthognathic surgery, achieving a functional occlusion, and enhancing the esthetics of the anterior teeth.
Based on the clinical and radiographic findings, three treatment options were offered: forced eruption of all unerupted and impacted teeth and correction of the malocclusion and skeletal sagittal discrepancy; forced eruption of strategic permanent teeth to serve as prosthetic abutments, extraction of the remaining teeth, and delivery of either removable partial dentures or bridges; or extraction of all unerupted teeth, followed by the placement of implants in the anterior region and an implant-supported denture. The patient and her parents chose the first option despite its projected long treatment time.
Multiple surgeries were performed to extract deciduous and supernumerary teeth, bond orthodontic attachments such as auxiliary buttons, and in some cases perforate the crowns of the unerupted teeth in preparation for orthodontic forced eruption (Fig. 2A). Eruption was performed using intermaxillary elastics, then .019" × .025" TMA* cantilever wires anchored to either a transpalatal arch or a lower lingual holding arch.
In the anterior region, forced eruption was performed by reciprocal toothborne anchorage and cemented or removable appliances. It was decided that in the maxillary arch, the tooth farthest from the alveolar ridge would be extracted, regardless of its crown anatomy.
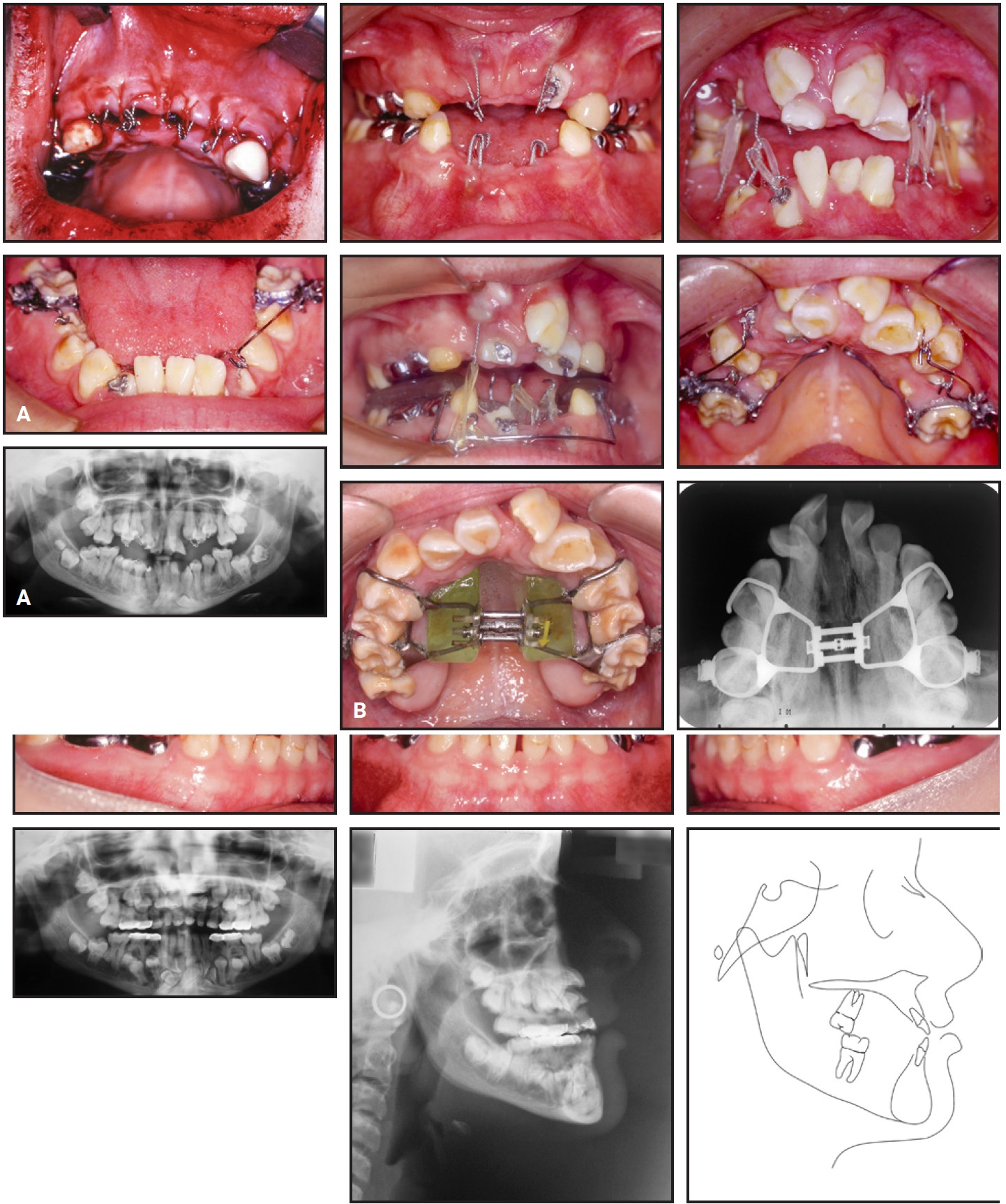
Fig. 2 A. Forced eruption with fixed appliances and reciprocal anchorage. B. Transverse changes after surgically assisted rapid palatal expansion.
No tooth was considered ankylosed. Maxillary constriction became more evident after eruption of the permanent teeth, requiring alignment of the posterior teeth prior to delivery of an expansion appliance. Surgically assisted rapid palatal expansion (SARPE) was performed when the patient was 19 (Fig. 2B).
Roth-prescription .022" brackets** were bonded in both arches in preparation for orthognathic surgery (Fig. 3).
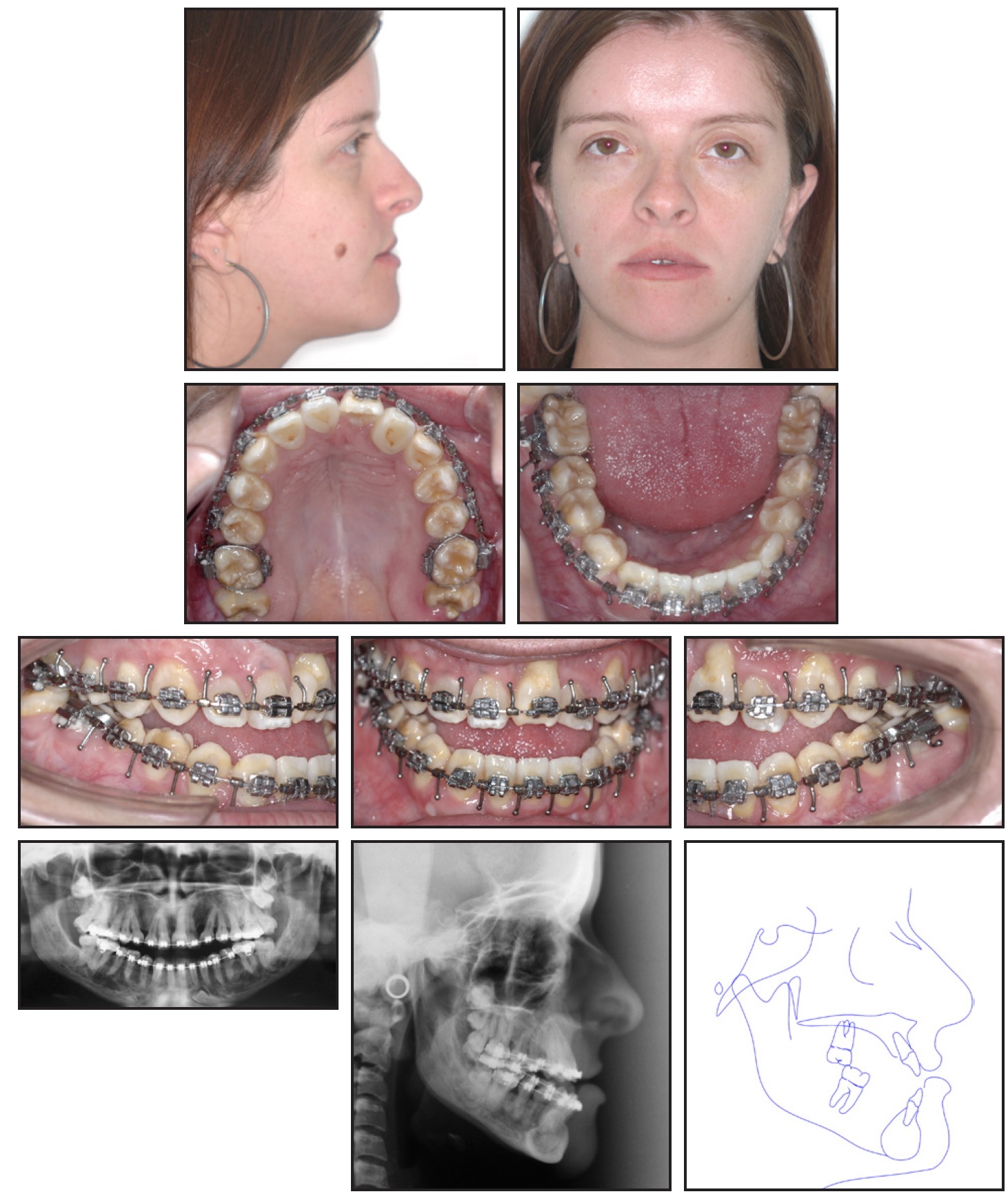
Fig. 3 Patient at age 23, before orthognathic surgery.
A Le Fort I osteotomy combined with bilateral sagittal split osteotomy (BSSO) was performed when the patient was 23 (Fig. 4).
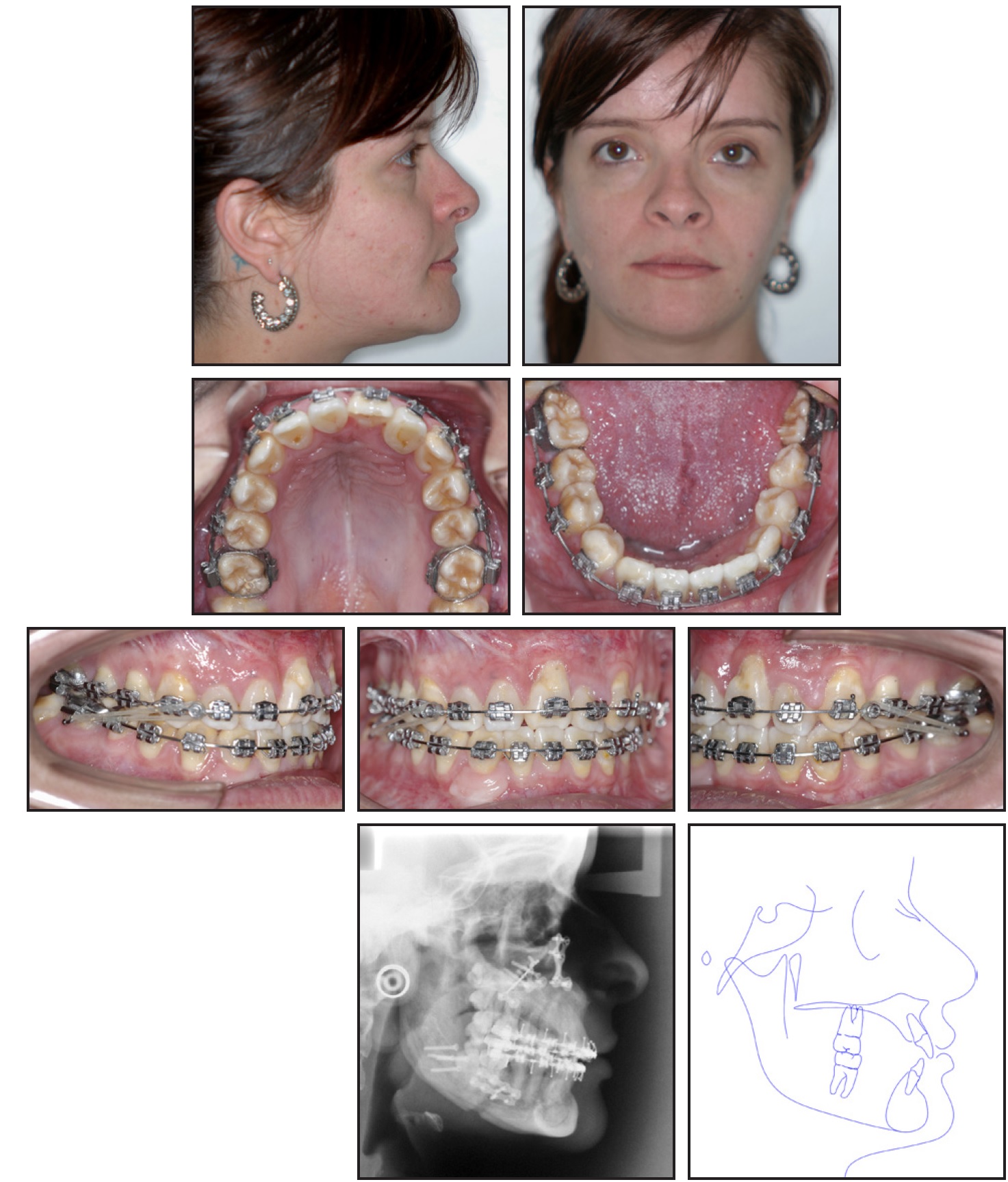
Fig. 4 After orthognathic surgery.
The maxilla was advanced 5mm and the mandible 2.4mm, with counterclockwise rotation of the occlusal plane. Pre- and postsurgical fixed appliances were used for a total of 43 months, with an archwire sequence of .014", .016", .018", .020", .017" × .025", and .018" × .025" nickel titanium and .018" × .025" and .019" × .025" stainless steel.
Due to its proximity to the mental foramen and the roots of both the lower left canine and first premolar, it was not possible to extract the supernumerary tooth in the lower left quadrant. The lower right lateral incisor was extracted and replaced by the lower right canine, which was adjusted to resemble the lower right lateral incisor, leaving the patient with a group function disocclusion on the right. A supernumerary tooth was left between the lower right first and second premolars, which did not prove advantageous in terms of function. The lower left and right third molars were extracted prior to orthognathic surgery, whereas the upper right and left third molars and the distally located supernumerary were maintained because they were unfavorably positioned for extraction.
After debonding at age 24 (Fig. 5), the patient was referred for restoration of the teeth affected by enamel hypoplasia. A lower fixed retainer was bonded, and the patient was instructed to wear an upper Hawley retainer for at least 24 months.
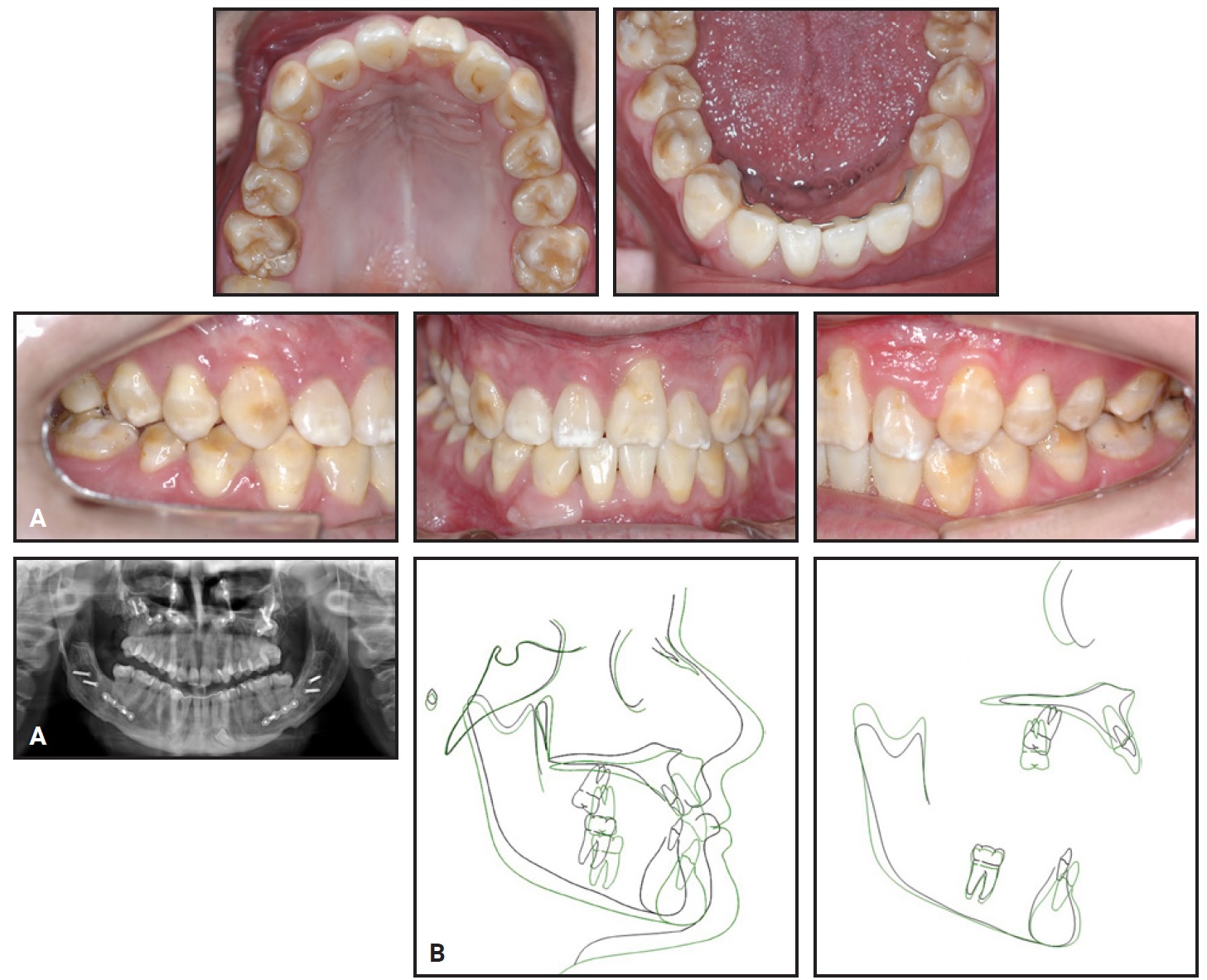
Fig. 5 A. Patient at age 24, after debonding of fixed orthodontic appliances. B. Superimposition of pretreatment (black) and post-treatment (green) cephalometric tracings.
Correction of the maxillomandibular discrepancy proved beneficial to the patient’s facial profile. Skeletal and dental changes were clinically stable except for the mandibular dental midline, which had shifted slightly to the left; the upper dental and facial midlines were coincident (Table 1).
The surgically corrected overjet remained unaltered two years after treatment (Fig. 6).
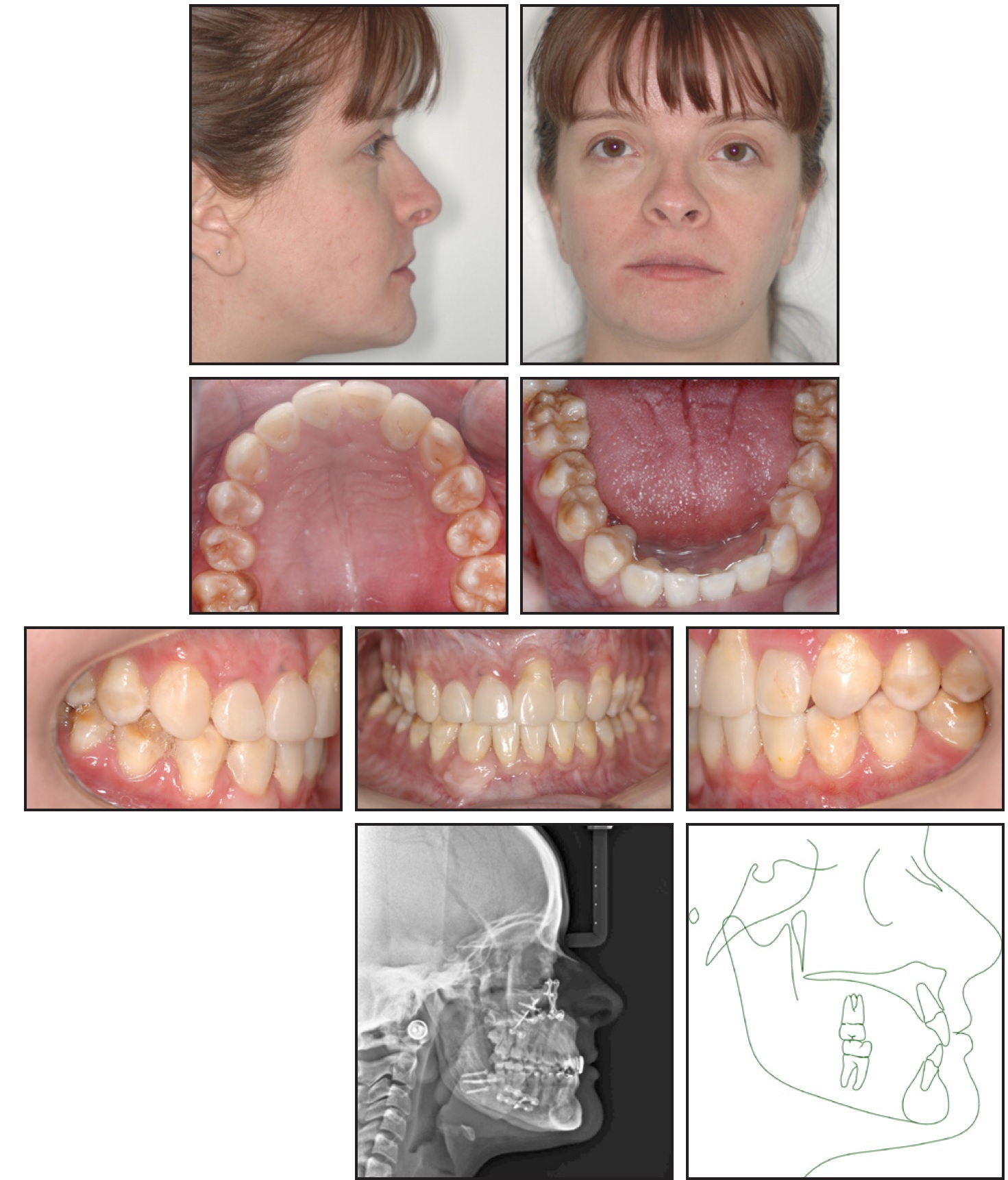
Fig. 6 Patient two years after treatment.
The smile was still pleasant, and the face was balanced. Eight years later, the upper right and left third molars and the remaining impacted supernumeraries showed no changes (Fig. 7).

Fig. 7 A. Patient 10 years after treatment. B. Periapical radiograph of lower left second molar after endodontic treatment and before extraction.
The lower left second molar required both endodontic and prosthodontic treatment due to an infection and a crown fracture, but the infection persisted, necessitating extraction. The patient underwent another cosmetic restorative treatment to further enhance her smile. The left side was finished in a quarter-cusp Class II malocclusion, which created some instability but did not compromise the overall outcome.
Discussion
There are two well-defined treatment protocols for CCD. The Toronto-Melbourne protocol recommends initiating treatment at an early age, starting with serial extraction of anterior deciduous teeth by age 5 or 6 and of posterior deciduous teeth at age 9 or 10.13,14 Permanent teeth are expected to erupt without the need for traction. The Jerusalem approach begins at a later age: anterior deciduous teeth are extracted at age 10-12, and posterior deciduous teeth at age 13; the permanent teeth are exposed before traction is begun.9,15 Because our patient was referred for orthodontic treatment at age 13, it was not possible to follow the Toronto-Melbourne protocol.13,14
Not all patients are eligible for such complex treatment, especially when intermaxillary elastics must be worn for a long period. Patient compliance is paramount because of the number of surgical procedures and forced eruptions, and excellent oral hygiene and frequent visits to a hygienist are indispensable.
Rapid palatal expansion is the most common method used to correct a maxillary transverse discrepancy. The ideal time for maxillary expansion is when the patient is still growing, since the midpalatal suture has not yet fused.16 Because our patient had already finished her growth spurt, however, a SARPE procedure was recommended. In some cases, the transverse discrepancy may be compensating for a sagittal maxillomandibular discrepancy.17,18 Skeletal Class III malocclusion is frequently observed in patients with CCD,9 for whom Le Fort I osteotomy, with or without BSSO, tends to be beneficial.
It is common to see young orthodontic patients with low self-esteem, especially in cases of syndromes that can negatively affect physical appearance.19 Despite the increased burden of care to which our patient was subjected, her self-esteem was high, especially after the satisfactory outcome. On the other hand, the long treatment time could have considerably reduced her quality of life, especially during the active phase. This raises doubts about the cost-benefit ratio of such treatment. Even longer follow-up studies are needed to confirm whether the actual benefits would be psychosocioeconomically significant in the long term. In the meantime, the burden of care can be minimized with an appropriately detailed treatment plan and with dedication from an interdisciplinary team. Patient selection also plays a decisive role.
ACKNOWLEDGMENTS: This study was authorized by the Ethics Committee at the Hospital for Rehabilitation of Craniofacial Anomalies of the University of São Paulo (HRCA-USP) under protocol No. 2.230.640. Informed consent was obtained.
FOOTNOTES
- *Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
- **Morelli, Sorocaba, Brazil; www.morelli.com.br.
REFERENCES
- 1. Kargul, B.; Salih, I.M.; Yilmaz, L.; and Dumlu, A.: Cleidocranial dysostosis: Report of a case, J. Clin. Pediat. Dent. 22:83-86, 1997.
- 2. Chen, S.; Santos, L.; Wu, Y.; Vuong, R.; Gay, I.; Schulze, J.; Chuang, H.H.; and MacDougall, M.: Altered gene expression in human cleidocranial dysplasia dental pulp cells, Arch. Oral Biol. 50:227-236, 2005.
- 3. Kelly, E. and Nakamoto, R.Y.: Cleidocranial dysostosis—a prosthodontic problem, J. Prosth. Dent. 31:518-526, 1974.
- 4. Mundlos, S.; Otto, F.; Mundlos, C.; Mulliken, J.B.; Aylsworth, A.S.; Albright, S.; Lindhout, D.; Cole, W.G.; Henn, W.; Knoll, J.H.; Owen, M.J.; Mertelsmann, R.; Zabel, B.U.; and Olsen, B.R.: Mutations involving the transcription factor CBFA1 cause cleidocranial dysplasia, Cell 89:773-779, 1997.
- 5. Kulkarni, M.L.; Vani, H.N.; Nagendra, K.; Mahesh, T.K.; Kumar, A.; Haneef, S.; Mohammed, Z.; and Kulkarni, P.M.: Yunis Varon syndrome, Ind. J. Pediat. 73:353-355, 2006.
- 6. D’Souza, R.N.; Aberg, T.; Gaikwad, J.; Cavender, A.; Owen, M.; Karsenty, G.; and Thesleff, I.: Cbfa1 is required for epithelialmesenchymal interactions regulating tooth development in mice, Develop. 126:2911-2920, 1999.
- 7. Richardson, A. and Deussen, F.F.: Facial and dental anomalies in cleidocranial dysplasia: A study of 17 cases, Int. J. Paediat. Dent. 4:225-231, 1994.
- 8. Furuuchi, T.; Kochi, S.; Sasano, T.; Iikubo, M.; Komai, S.; and Igari, K.: Morphologic characteristics of masseter muscle in cleidocranial dysplasia: A report of 3 cases, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 99:185-190, 2005.
- 9. Becker, A.; Lustmann, J.; and Shteyer, A.: Cleidocranial dysplasia: Part 1—General principles of the orthodontic and surgical treatment modality, Am. J. Orthod. 111:28-33, 1997.
- 10. Fukuta, Y.; Totsuka, M.; Fukuta, Y.; Takeda, Y.; Yoshida, Y.; Niitsu, J.; and Yamamoto, H.: Histological and analytical studies of a tooth in a patient with cleidocranial dysostosis, J. Oral Sci. 43:85-89, 2001.
- 11. Nayar, S. and Bishop, K.: Cleidocranial dysplasia—a late diagnosis, Dent. Update 33:221-226, 2006.
- 12. Cooper, S.C.; Flaitz, C.M.; Johnston, D.A.; Lee, B.; and Hecht, J.T.: A natural history of cleidocranial dysplasia, Am. J. Med. Genet. 104:1-6, 2001.
- 13. Smylski, P.T.; Woodside, D.G.; and Harnett, B.E.: Surgical and orthodontic treatment of cleidocranial dysostosis, Int. J. Oral Surg. 3:380-385, 1974.
- 14. Hall, R.K. and Hyland, A.L.: Combined surgical and orthodontic management of the oral abnormalities in children with cleidocranial dysplasia, Int. J. Oral Surg. 7:267-273, 1978.
- 15. Becker, A.; Shteyer, A.; Bimstein, E.; and Lustmann, J.: Cleidocranial dysplasia: Part 2—Treatment protocol for the orthodontic and surgical modality, Am. J. Orthod. 111:173-183, 1997.
- 16. Guest, S.S.; McNamara, J.A. Jr.; Baccetti, T.; and Franchi, L.: Improving Class II malocclusion as a side-effect of rapid maxillary expansion: A prospective clinical study, Am. J. Orthod. 138:582-591, 2010.
- 17. Baccetti, T.; Franchi, L.; Cameron, C.G.; and McNamara, J.A. Jr.: Treatment timing for rapid maxillary expansion, Angle Orthod. 71:343-350, 2001.
- 18. Franchi, L. and Baccetti, T.: Transverse maxillary deficiency in Class II and Class III malocclusions: A cephalometric and morphometric study on postero-anterior films, Orthod. Craniofac. Res. 8:21-28, 2005.
- 19. Kiyak, H.A.: Does orthodontic treatment affect patients’ quality of life? J. Dent. Ed. 72:886-894, 2008.







COMMENTS
.