JCO Interviews Dr. Homer W. Phillips on Bonding, Part 2
Open bite is a common malocclusion in the deciduous and mixed dentition that can, if not corrected, evolve into a skeletal open bite in the permanent dentition.1 Its etiology is multifactorial, involving morphofunctional deviation of the masticatory system, tongue interposition, and deleterious habits, among other factors.2
The morphology of skeletal open bite may extend beyond the anterior region to the premolars and molars. Cephalometrically, it is characterized by an open mandibular plane angle, negative overbite, mesial angulation of the posterior teeth, divergence of the occlusal planes, maxillary arch atresia, disproportional relationship of total anterior and posterior facial heights (with a short mandibular ramus), excessive lower anterior facial height, counter-clockwise rotation of the palatal plane, clockwise rotation of the mandible, and increased alveolar height in the posterior region of the maxilla.1 Skeletal open bite often results in a vertical maxillomandibular imbalance called long-face syndrome.3-6
Diagnosis and treatment planning for anterior open bite depend mainly on the severity and degree of facial involvement. In non-growing young adult patients with severe skeletal open bite, the options are limited to compensatory orthodontics or surgical-orthodontic treatment.7,8 When the open bite affects facial esthetics, the patient’s chief complaint should be the decisive factor.1 Compensatory treatment of a hyperdivergent patient may require extraction of the first permanent molars, especially if the patient exhibits crowding or missing teeth.9-11
This article demonstrates effective strategies for compensatory fixed-appliance treatment of hyperdivergent adult patients with severe skeletal anterior open bites, including first-molar extractions and the use of lingual spurs and intermaxillary elastics.
Case Report
An 18-year-old male presented with the chief complaints of dental malpositions, speech difficulties, and poor smile esthetics (Fig. 1). Clinical examination found a lack of passive lip seal and an imbalance of the facial thirds, indicating a hyperdivergent pattern. The profile was convex, with clockwise rotation of the mandible and excessive lower anterior facial height. The patient had a severe anterior open bite, anterior crowding in both arches, and coincident maxillary and mandibular midlines. The lower right first molar was missing, and there was a Class III molar relationship on the left side. Maxillary atresia and a partial posterior crossbite were also noted.
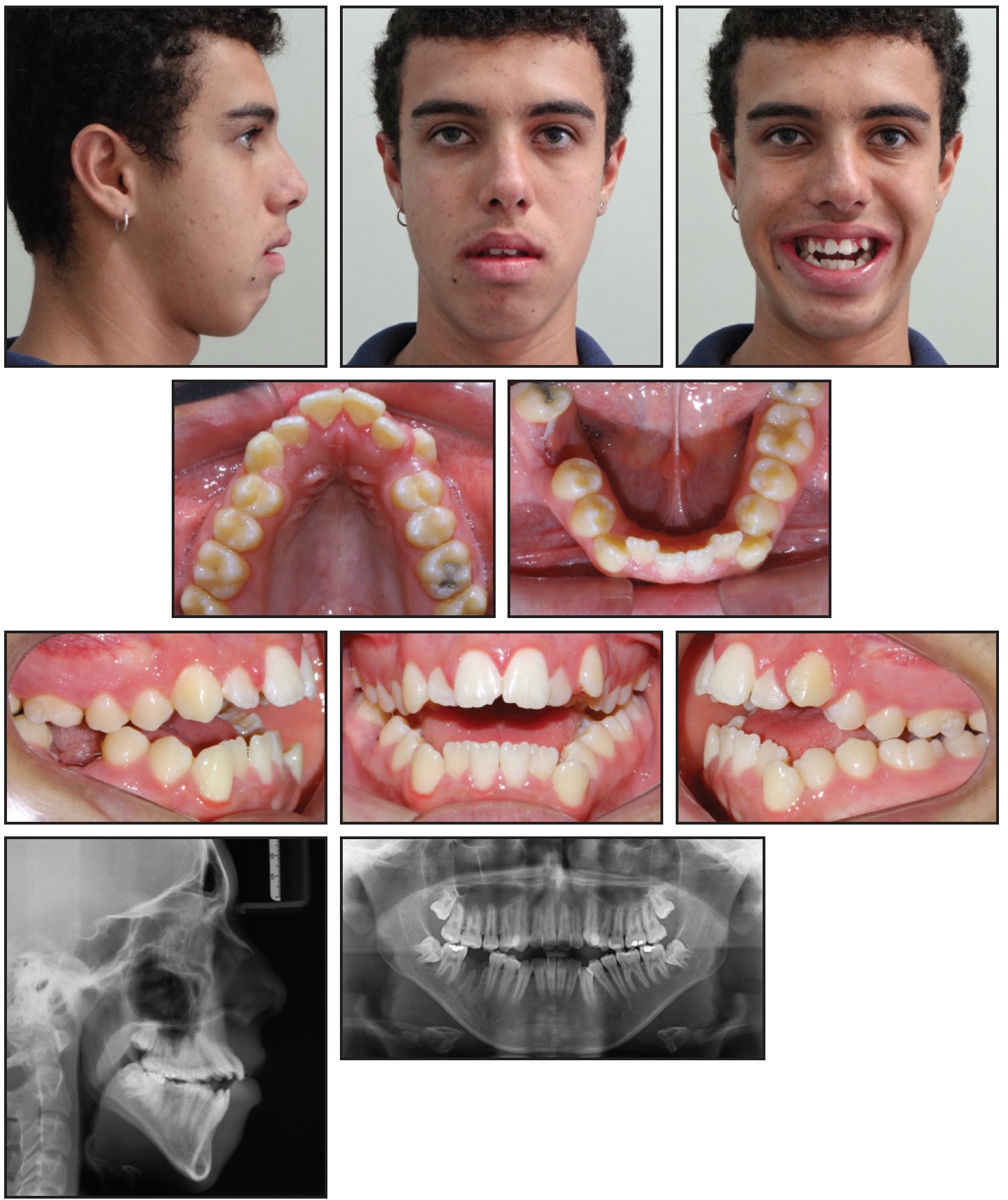
Fig. 1 18-year-old male patient with severe anterior open bite, Class III molar relationship on left side, and upper and lower anterior crowding before treatment.
A panoramic radiograph confirmed the recent extraction of the lower right first molar. All third molars were present, but the maxillary third molars had not erupted and the mandibular third molars were slightly impacted. Cephalometric analysis showed a mandibular clockwise rotation, anterior open bite (negative overbite) of −5.8mm, excessive overjet, protrusive maxillary and mandibular incisors, and buccally inclined maxillary incisors (Table 1). The anterior facial height and all vertical components measured above normal.
Treatment objectives were to close the open bite, correct the overjet and crowding, and obtain an ideal occlusion, while improving the smile esthetics. Because of the severe skeletal open bite and the vertical discrepancy, our first recommendation was for surgical-orthodontic treatment. When the patient refused orthognathic surgery, compensatory orthodontic treatment was planned. This would include rapid maxillary expansion, followed by extraction of the remaining three first permanent molars and the use of fixed appliances for leveling and alignment, lingual spurs on the maxillary incisors to promote proper tongue posture, and intermaxillary elastics to close the anterior open bite.
A Hyrax* rapid maxillary expander was inserted and activated one-quarter turn twice per day for 14 days (Fig. 2).

Fig. 2 Hyrax* rapid maxillary expander in place.
After five months of treatment, the lower left first molar was extracted. Another month later, the Hyrax appliance was removed, the upper first molars were extracted, and Biofunctional** Class III fixed appliances were bonded (Fig. 3). With the lower left first molar already removed, initial retraction of the lower left premolars could be performed with elastic chains.
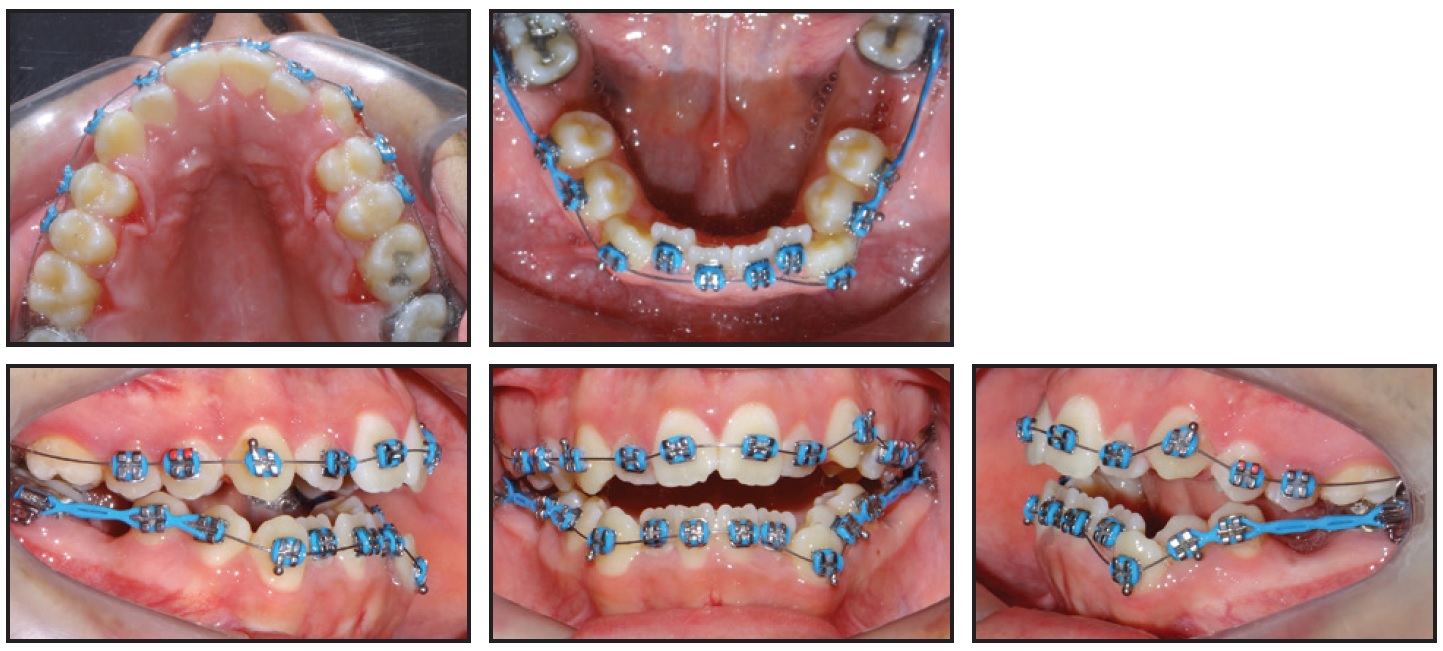
Fig. 3 After six months of treatment, Biofunctional** Class III fixed appliances placed for initial retraction of mandibular premolars.
Three months later, leveling and alignment were initiated on .012" nickel titanium archwires (Fig. 4), followed by wires of increasing thickness.

Fig. 4 Initiation of leveling and alignment after three months of retraction.
Another four months later, anterior retraction for extraction space closure was started using .019" × .025" stainless steel archwires and elastic chains from the upper left second molar to right second molar (Fig. 5). Lingual spurs were bonded to the maxillary incisors to avoid tongue interpositioning and thus help correct the anterior open bite.
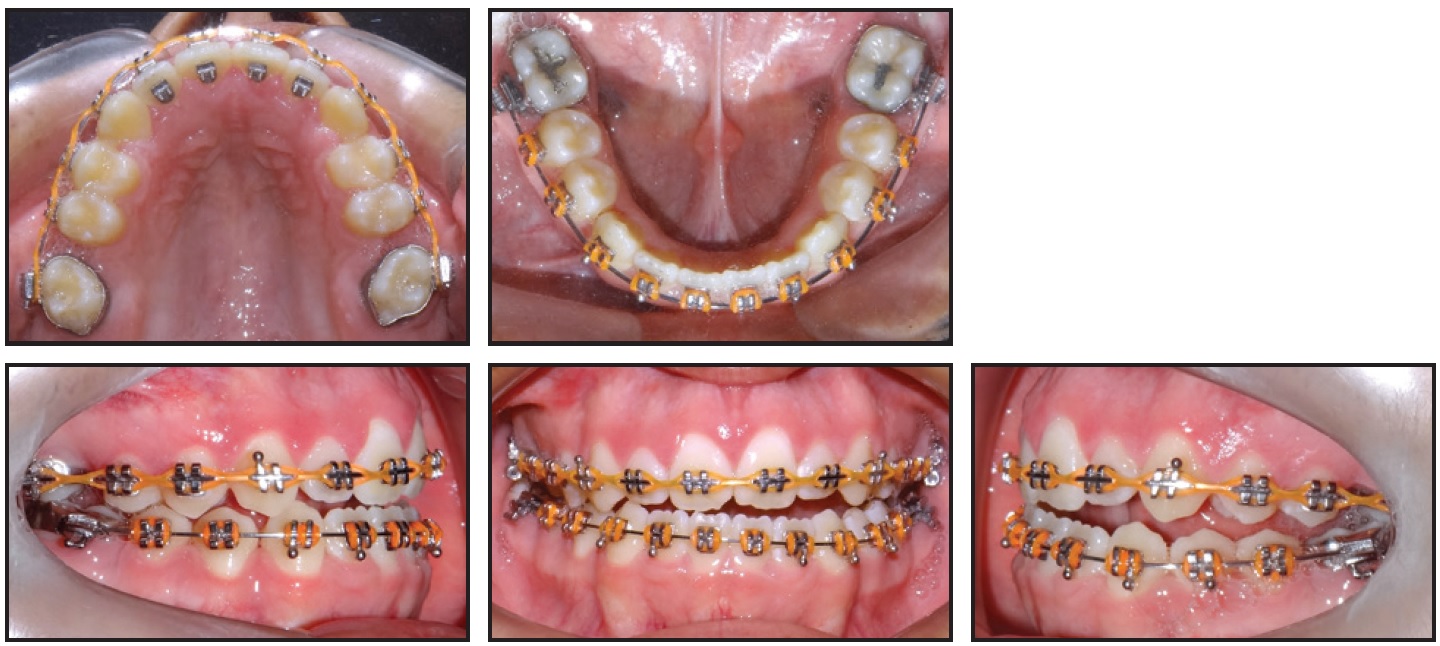
Fig. 5 After 13 months of treatment, anterior retraction started with elastic chains; lingual spurs bonded to maxillary incisors.
During these 13 months of fixed-appliance treatment, the anterior retraction without anchorage allowed mesialization of the second molars and spontaneous eruption of all four third molars (Fig. 6).
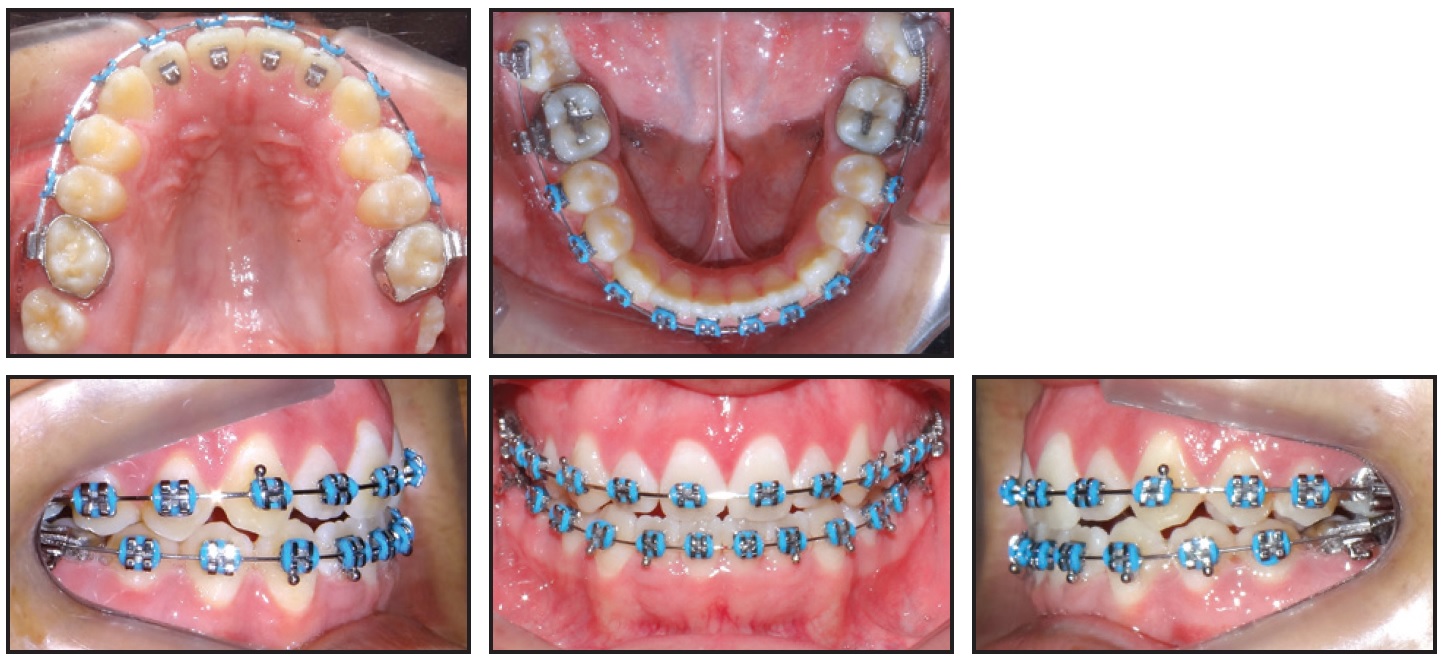
Fig. 6 After 19 months of treatment, mandibular third molars bonded.
The mandibular third molars were then bonded and leveled with nickel titanium archwires and open-coil springs as needed.
Three months later, ³⁄16" Class III intermaxillary elastics were prescribed to be worn 24 hours per day for overjet correction (Fig. 7). In addition, 1⁄8" triangle elastics were attached between the maxillary and mandibular canines and the mandibular first premolars on both sides to bring the canines into a Class I relationship and to act as active retention for maintaining the bite closure. After five months of this protocol, the elastic wear was gradually reduced over the next six months, until the fixed appliances were removed.

Fig. 7 After 22 months of treatment, Class III and triangle intermaxillary elastic wear initiated.
After 27 months of fixed-appliance treatment, a removable upper Hawley retainer was delivered to be worn 24 hours per day for one year, and a lower 3-3 lingual retainer was bonded.
Total treatment time was 33 months (Fig. 8). There was a slight improvement in the facial profile because of the retraction of the upper and lower lips and achievement of passive lip seal, but there were no visible changes in the hyperdivergent pattern. An acceptable occlusion was obtained, with Class I molar and canine relationships, ideal overjet and overbite, and coincident midlines. The final panoramic radiograph showed good root parallelism and excellent positioning of the second and third molars.
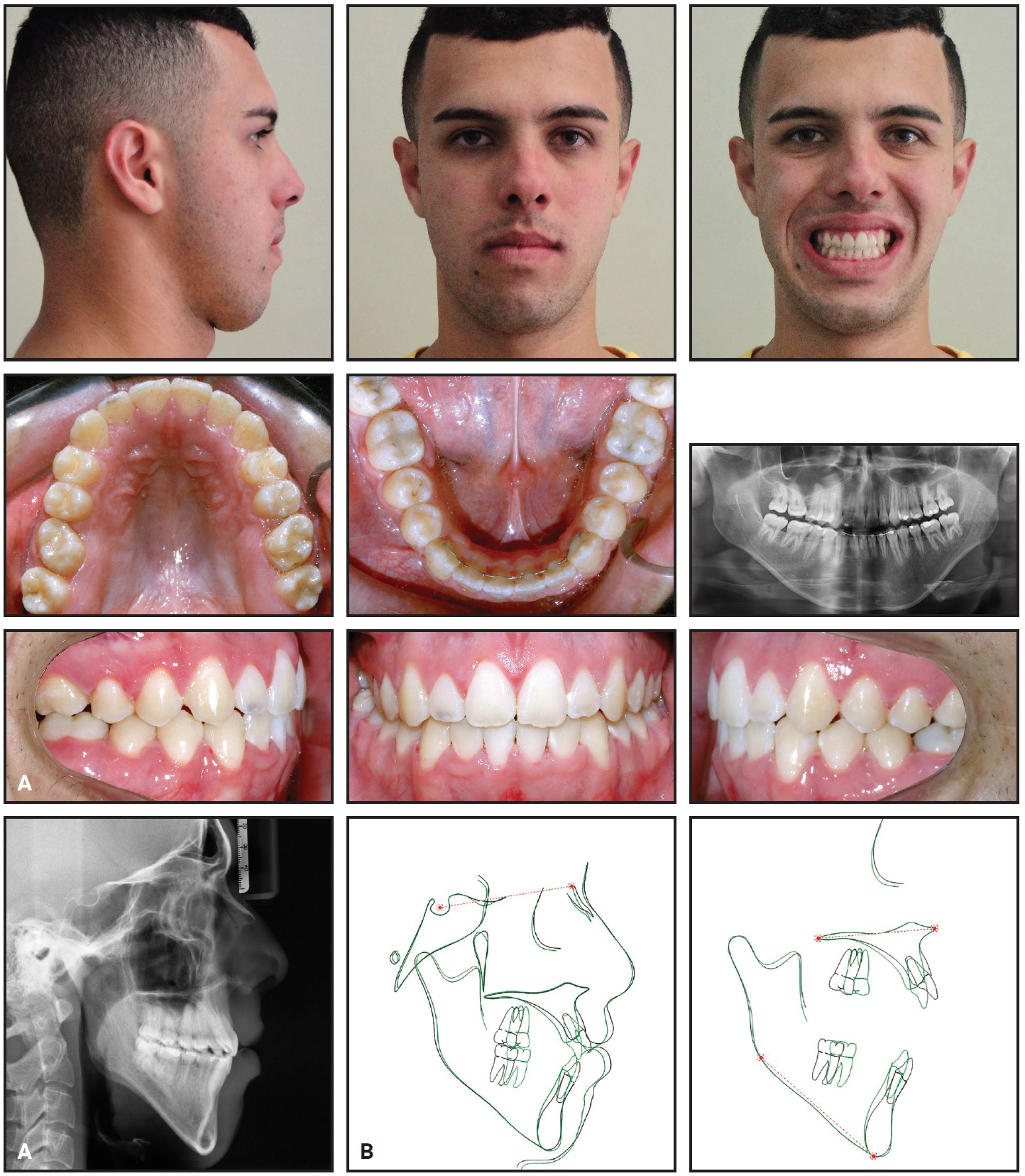
Fig. 8 A. Patient after 33 months of treatment. B. Superimposition of pre- and post-treatment cephalometric tracings.
Cephalometric analysis confirmed the retraction, uprighting, and extrusion of the maxillary and mandibular incisors; mesialization of the maxillary and mandibular molars; reduction in overjet and increase in overbite; opening of the nasolabial angle; and slight retrusion of the upper and lower lips (Table 1). Superimpositions illustrated the dental changes achieved through compensatory orthodontic treatment, with only minor changes in the facial profile.
The results remained stable one year after treatment (Fig. 9).

Fig. 9 Patient one year after treatment.
Discussion
Although etiological factors may be environmental or genetic, the causes of malocclusions are generally multifactorial.12 In the case shown here, genetics certainly contributed more than environmental factors, but the patient also had an airway problem—as confirmed by the large opening of the upper airway in the initial lateral cephalogram. He reported having his adenoids removed in early adolescence.
In a case as severe as this, with a skeletal open bite and hyperdivergent facial pattern, the best treatment option is usually a combined surgical-orthodontic approach.7 When our patient refused orthognathic surgery, however, compensatory orthodontic treatment was considered.1,13
Rapid maxillary expansion was performed because of the atresic maxilla and posterior crossbite. Since the patient was 18 years old at the beginning of treatment, the maxillary expansion was intended to achieve only dentoalveolar expansion and correction of the posterior crossbite. This could have been accomplished with other appliances or mechanics, such as a TMA*** auxiliary expansion arch, which is commonly used for dentoalveolar expansion in adults.14 Although an expander with occlusal coverage is indicated in anterior open-bite cases, previous studies suggest that Haas and Hyrax expanders can be safely used in hyperdivergent and open-bite cases because they do not open the bite over the long term,15 even in high-angle patients.16 Investigations of long-term skeletal changes produced by rapid maxillary expansion have found that the opening of the mandibular plane angle is a transient effect.16-18 In our case, some skeletal gain in the maxillary transverse dimension could be observed, with the opening of the midpalatal suture indicated by a diastema between the maxillary central incisors. We found increases of 4.3mm in the intercanine width, 6.4mm in the inter-first-premolar width, and 8.5mm in the intermolar width. A possible explanation for the discrepancy is that the canines did not support the Hyrax appliance, while both the first premolars and first molars anchored the device.
Extractions were needed to correct the severe crowding and bimaxillary protrusion in this case, as well as to promote the “drawbridge effect”—a useful strategy in open-bite treatment because it helps close the bite.1,19 With the patient’s lower right first molar already extracted, our decision was to remove the other three first permanent molars, which would relieve the severe crowding and facilitate retraction of the anterior teeth and closure of the anterior open bite. Although four premolars are more commonly extracted in orthodontic treatment plans, the four third molars are usually extracted as well in anterior open-bite cases. One study estimated that the extraction of four first premolars and four third molars would remove 25% of the total dental material, while extraction of only the four first molars would remove a more conservative 12.5%.20 The presence and size of the third molars must be confirmed radiographically and clinically before the latter option is chosen.20,21 In our case, the initial panoramic radiograph showed the presence of four third molars in good position to erupt and move anteriorly after extraction of the first molars and mesial movement of the second molars. The extraction mechanics can also incorporate some counterclockwise mandibular rotation along with the mesial movement of the posterior teeth, thus promoting open-bite closure.22
Cephalometric measurements showed that the anterior open-bite correction in this case resulted from the retraction, uprighting, and extrusion of the maxillary and mandibular incisors—the “drawbridge effect.” Maxillary anterior extrusion was not an issue in this case, since an increased maxillary incisor display would help achieve a more harmonious smile. No significant changes occurred in the skeletal components. Mesial movement of the second molars after first-molar extractions can change the fulcrum of contact, producing a counterclockwise rotation of the mandible and thus reducing the hyperdivergency of the mandibular plane.10,13 This effect did not occur in the present case, probably because the maxillary second molars were mesialized with slight extrusion, so that only the occlusal plane rotated counterclockwise, rather than the entire mandible.
The lingual spurs bonded to the maxillary incisors avoided tongue interpositioning and improved tongue posture, which certainly helped correct the anterior open bite.23 The only intercuspation elastics were worn between the maxillary and mandibular canines and the mandibular first premolars, as active retention to maintain the bite closure. Since no anterior elastics were used, the extrusion of the maxillary and mandibular incisors was attributable to the retraction and uprighting of these teeth, while normal physiological development of the incisors was minimized by the lingual spurs.23
The profile showed only minor changes. The nasolabial angle increased as a result of the molar extractions and subsequent retraction of the maxillary incisors, and a slight retrusion of the upper and lower lips was noted. These changes in the soft-tissue components were not enough to provide a significant esthetic improvement of the facial profile. Although the recommended orthognathic surgery would probably have produced such improvement,7 the patient was highly satisfied with the final outcome.
FOOTNOTES
- *Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- **Morelli Ortodontia, Sorocaba, São Paulo, Brazil; www.morelli.com.br.
- ***Trademark of Ormco Corporation, Orange, CA; www.ormco.com.
REFERENCES
- 1. Janson, G. and Valarelli, F.P.: Open Bite Malocclusion: Treatment and Stability, Wiley-Blackwell, Hoboken, NJ, 2014, p. 604.
- 2. Ngan, P. and Fields, H.W.: Open bite: A review of etiology and management, Pediat. Dent. 19:91-98, 1997.
- 3. Sassouni, V.: A classification of skeletal facial types, Am. J. Orthod. 55:109-123, 1969.
- 4. Fränkel, R. and Fränkel, C.: Functional aspects of molar extraction in skeletal open bite, in Orthodontics: State of the Art, Essence of the Science, ed. L.W. Graber, Mosby, St. Louis, 1987, pp. 184-199.
- 5. Nahoum, H.I.: Vertical proportions and the palatal plane in anterior open-bite, Am. J. Orthod. 59:273-282, 1971.
- 6. Schendel, S.A.; Eisenfeld, J.; Bell, W.H.; Epker, B.N.; and Mishelevich, D.J.: The long face syndrome: Vertical maxillary excess, Am. J. Orthod. 70:398-408, 1976.
- 7. Epker, B.N. and Fish, L.: Surgical-orthodontic correction of open-bite deformity, Am. J. Orthod. 71:278-299, 1977.
- 8. Ribeiro, G.L.; Regis, S. Jr.; Da Cunha, T.M.; Sabatoski, M.A.; Guariza-Filho, O.; and Tanaka, O.M.: Multiloop edgewise archwire in the treatment of a patient with an anterior open bite and a long face, Am. J. Orthod. 138:89-95, 2010.
- 9. Klapper, L.; Navarro, S.F.; Bowman, D.; and Pawlowski, B.: The influence of extraction and nonextraction orthodontic treatment on brachyfacial and dolichofacial growth patterns, Am. J. Orthod. 101:425-430, 1992.
- 10. Aras, A.: Vertical changes following orthodontic extraction treatment in skeletal open bite subjects, Eur. J. Orthod. 24:407-416, 2002.
- 11. Oliveira, K.F.M.; Freitas, K.M.S.; Valarelli, F.P.; Cançado, R.H.; and Menezes, C.C.: Molar extraction in severe open bite treatment, J. Surg. Clin. Dent. 6:11-16, 2015.
- 12. Freitas, K. and Cançado, R.: Etiology of the open bite, in Open Bite Malocclusion: Treatment and Stability, ed. G. Janson and F.P. Valarelli, Wiley-Blackwell, Hoboken, NJ, 2014.
- 13. Martina, R.; Laino, A.; and Michelotti, A.: Class I malocclusion with severe open bite skeletal pattern treatment, Am. J. Orthod. 97:363-373, 1990.
- 14. Siécola, G.; Henriques, J.F.; Freitas, K.M.; and Janson, G.: Dentoalveolar changes in adults promoted by the use of auxiliary expansion arch: A CBCT study, J. Clin. Exp. Dent. 11:e898-e905, 2019.
- 15. Lineberger, M.W.; McNamara, J.A.; Baccetti, T.; Herberger, T.; and Franchi, L.: Effects of rapid maxillary expansion in hyperdivergent patients, Am. J. Orthod. 142:60-69, 2012.
- 16. Chang, J.Y.; McNamara, J.A. Jr.; and Herberger, T.A.: A longitudinal study of skeletal side effects induced by rapid maxillary expansion, Am. J. Orthod. 112:330-337, 1997.
- 17. Garib, D.G.; Henriques, J.F.; Carvalho, P.E.; and Gomes, S.C.: Longitudinal effects of rapid maxillary expansion, Angle Orthod. 77:442-448, 2007.
- 18. Velázquez, P.; Benito, E.; and Bravo, L.A.: Rapid maxillary expansion: A study of the long-term effects, Am. J. Orthod. 109:361-367, 1996.
- 19. Janson, G.; Valarelli, F.P.; Beltrão, R.T.S.; De Freitas, M.R.; and Henriques, J.F.C.: Stability of anterior open-bite extraction and nonextraction treatment in the permanent dentition, Am. J. Orthod. 129:768-774, 2006.
- 20. Jensen, I.D.: Extraction of the first molars in discrepancy cases, Am. J. Orthod. 64:115-136, 1973.
- 21. Williams, R.: Single arch extraction: Upper first molar or what to do when non-extraction treatment fails, Am. J. Orthod. 76:377-393, 1979.
- 22. Arat, M. and Iseri, H.: Orthodontic and orthopaedic approach in the treatment of skeletal open bite, Eur. J. Orthod. 14:207-215, 1992.
- 23. Canuto, L.F.; Janson, G.; De Lima, N.S.; De Almeida, R.R.; and Cançado, R.H.: Anterior open-bite treatment with bonded vs conventional lingual spurs: A comparative study, Am. J. Orthod. 149:847-855, 2016.









COMMENTS
.