CASE REPORT
Surgical-Orthodontic Treatment of a Patient with Severely Asymmetrical Skeletal Class III Dentofacial Deformity
Compared with a typical skeletal Class III mandibular protrusion, an asymmetrical skeletal Class III is a more complex three-dimensional craniomaxillary deformity, involving unilateral excessive mandibular growth or deficient maxillary growth in the sagittal dimension, bilateral inconsistency of maxillary and mandibular height in the vertical dimension, and inconsistency of the maxillary and mandibular widths in the transverse dimension.1,2 Comprehensive treatment including presurgical orthodontics, orthognathic surgery, and postsurgical orthodontics is required for these defects to be completely resolved.3
The long-term stability of conventional surgical-orthodontic treatment for a severely asymmetrical skeletal Class III dentofacial deformity has been considered problematic because of the possible inadequacy of dental decompensation before surgery, along with complications due to condylar changes, airway conditions, and muscle pull and function.4 Considering these factors, it is important to carefully evaluate such a skeletal deformity and the dental compensation mechanisms to plan presurgical orthodontics that can achieve the desired goals and ensure stability. The magnitude and amount of surgical correction will largely depend on the efficacy of the presurgical orthodontic decompensation, which should be planned in all three planes of space.5,6 In the sagittal dimension, the proclined upper incisors and retroclined lower incisors must be decompensated to place them in ideal positions with respect to the jaw; in the transverse dimension, the arches must be coordinated while controlling the torque of the posterior segments; in the vertical dimension, the overerupted teeth must be intruded to establish an appropriate vertical anterior tooth display after surgery.3,7
This case report demonstrates comprehensive surgical-orthodontic treatment of a patient with severe skeletal discrepancies in all three planes: sagittal (Class III malocclusion), transverse (facial asymmetry), and vertical (long face and open bite).
Similar articles from the archive:
- Surgical-Orthodontic Correction of Skeletal Class III Malocclusion with Vertical Maxillary Excess December 2016
- The "Surgery First" Approach with Passive Self-Ligating Brackets for Expedited Treatment of Skeletal Class III Malocclusion June 2015
- CASE REPORT Surgical-Orthodontic Correction of a Skeletal Class III Malocclusion with Severe Maxillary Constriction October 2013
Diagnosis and Treatment Plan
A 27-year-old male presented with an asymmetrical face, with the chin shifted to the left, a concave profile, and excessive lower facial height (Fig. 1A). He reported that a mild mandibular trauma had occurred a month earlier. Intraoral examination found a more-than-full-cusp Class III molar relationship, anterior and posterior crossbites, and an open bite. The patient also exhibited gingival swelling with bleeding and recession.
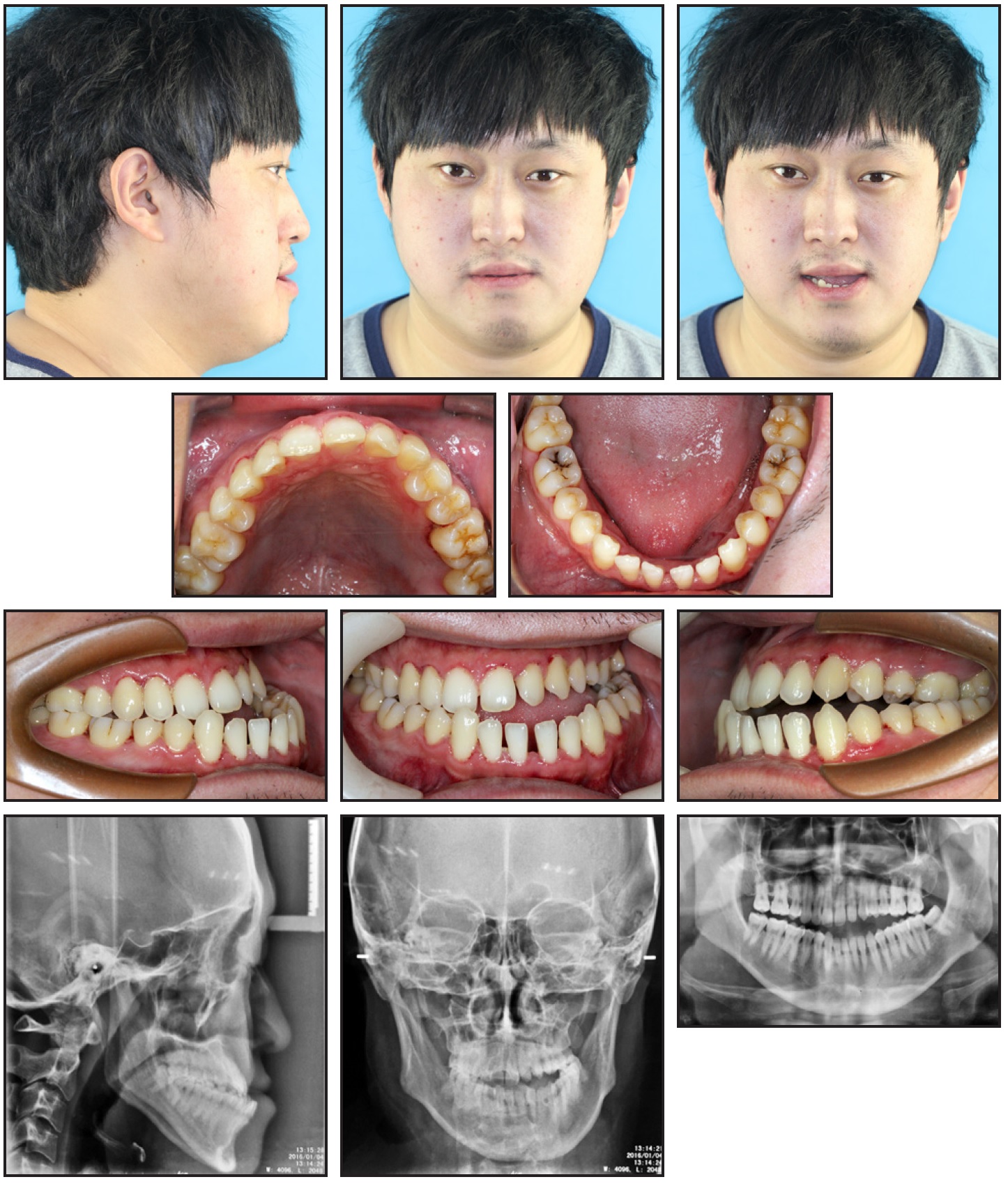
Fig. 1 27-year-old male patient with severe skeletal Class III dentofacial deformity, asymmetrical face, and concave profile before treatment (continued in next image).
Analysis of the study casts showed an overjet of −4.4mm to −8.07mm and generalized spacing in the upper and lower anterior segments (Table 1). The upper right first premolar was congenitally missing, and the upper left second molar was abnormal (Fig. 1B).
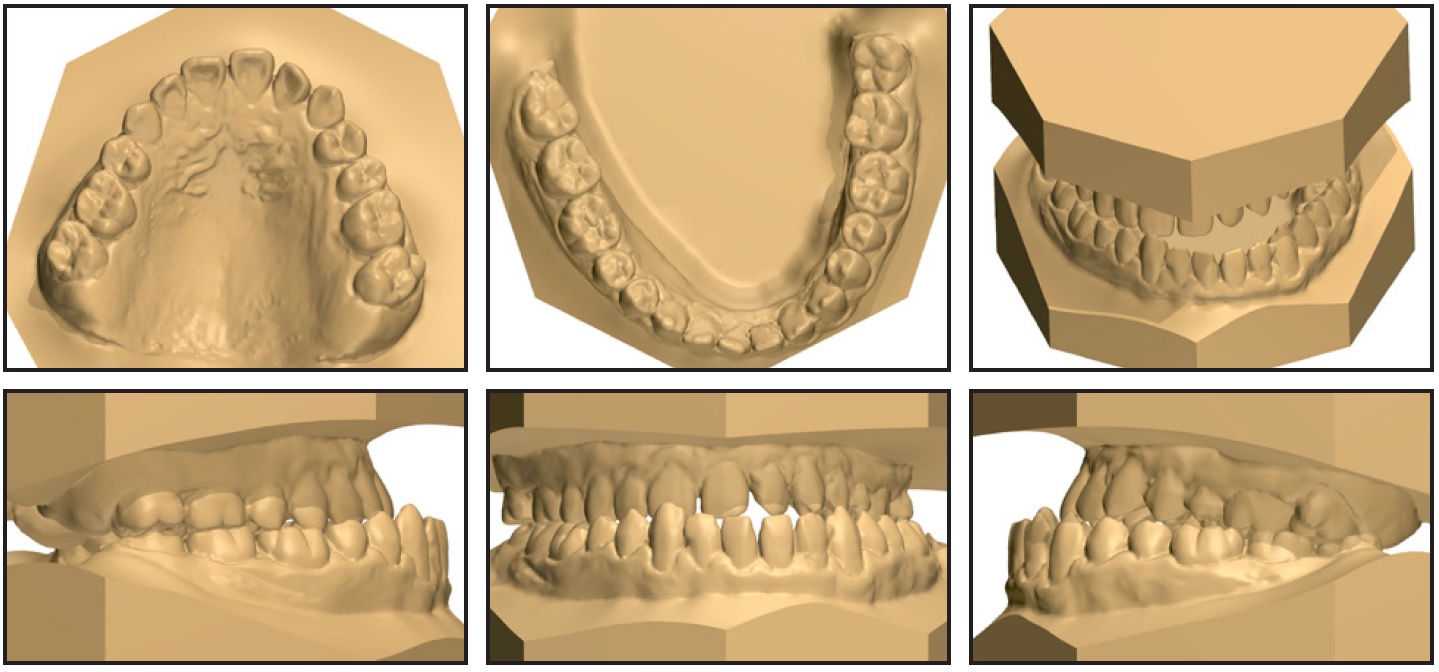
Fig. 1 (cont.) 27-year-old male patient with severe skeletal Class III dentofacial deformity, asymmetrical face, and concave profile before treatment.
The panoramic radiograph indicated generalized horizontal bone loss in both arches, with the root of the upper left premolar shorter than normal. Cephalometric analysis (Table 2) confirmed a skeletal Class III relationship (ANB = −4.2°, Wits appraisal = −13.5mm, APDI = 96.4°), a hyperdivergent pattern (SN-MP = 4 4.9°, F MA = 2 9.1°, S-Go/N-Me = 58.3%, y-axis = 74.7°, ODI = 46.7°), and a skeletal open-bite tendency (ALFH/PLFH = 1.9).
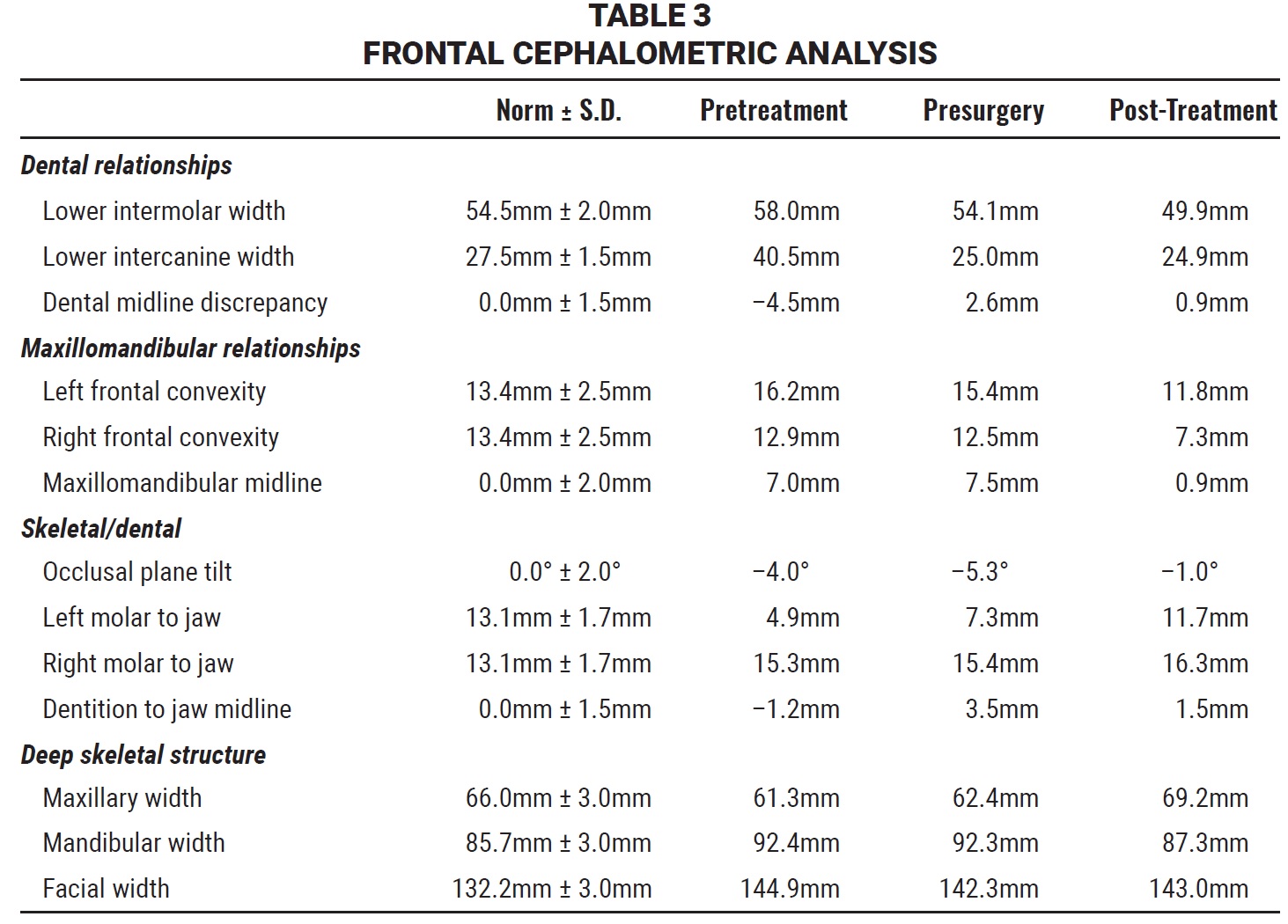
The Ricketts frontal cephalometric analysis indicated skeletal asymmetry of the mandible and dental asymmetry of the mandibular arch (Table 3).
Cone-beam computed tomography (CBCT) showed inconsistency in the morphology of the TMJ and widening of the anterior space on the left (Fig. 2). Functional examination found no signs of TMD, although the mandible deflected to the right when opening.
The diagnosis was a skeletal Class III dentofacial deformity with facial asymmetry, attributable to abnormal development of the maxilla and mandible in three dimensions; a congenitally missing upper right first premolar; an abnormality in the upper left second molar; and chronic generalized periodontitis.
Treatment objectives were to correct the asymmetrical skeletal Class III deformity, thus achieving a harmonious facial appearance; align the dental midlines with each other and with the facial midline; establish ideal overjet and overbite with proper interdigitation of the posterior teeth; improve the periodontal condition; and facilitate good oral hygiene.
Combined surgical-orthodontic treatment was the only viable approach to achieve these objectives. Presurgical orthodontics would decompensate the dentition to achieve a maximum skeletal correction and stable postsurgical occlusion. A Le Fort I osteotomy was planned to advance, slightly rotate, and center the maxilla, with the advancement more pronounced on the left and the impaction on the right and in the posterior regions. In addition, a bilateral sagittal split ramus osteotomy would set back and rotate the entire mandible counterclockwise, with more movement on the right to level the mandible with the maxilla. Postsurgical orthodontics would finish and detail the occlusion.
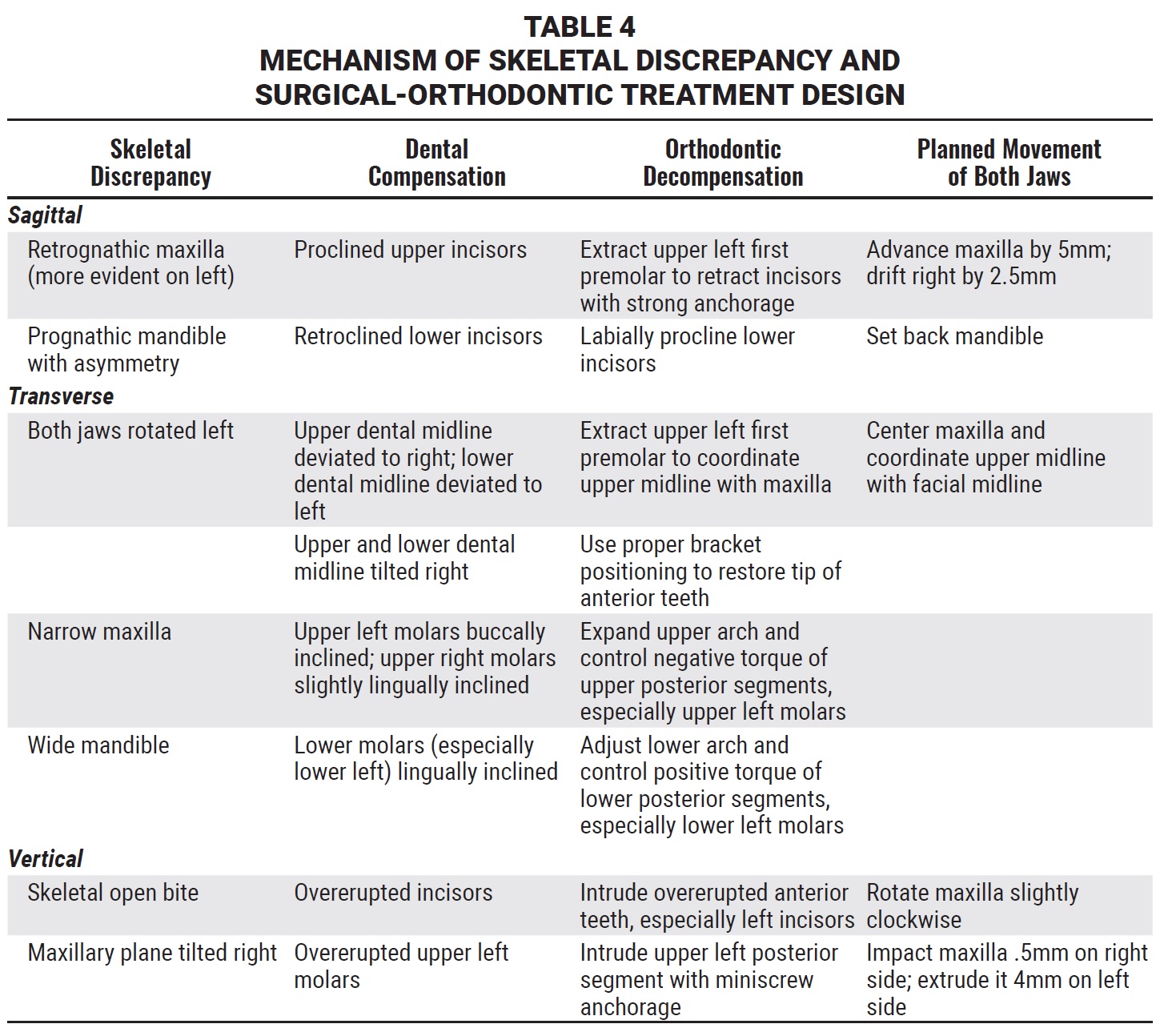
The presurgical orthodontic decompensation was carefully planned to coordinate with the planned surgical movements (Table 4). Maxillary premolars are commonly extracted to help decompensate proclined upper incisors and coordinate the midline between the upper dentition and the maxilla. In this patient, because of the missing maxillary right first premolar, the upper dental midline was deviated to the right compared with the maxillary midline. This was a challenging situation, since the upper dental midline and facial midline typically deviate to the same side. We decided to extract the upper left first premolar and to retract the upper left incisors with strong anchorage from a miniscrew in the left maxilla. The patient agreed to this plan and to extraction of the lower left and right third molars, followed by two-jaw surgery to correct his skeletal deformity.
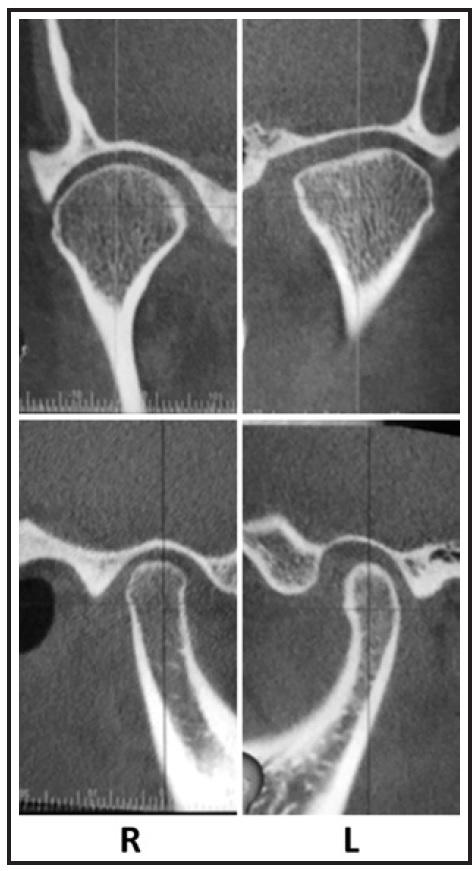
Fig. 2 Cone-beam computed tomography (CBCT) images of TMJs before treatment.
Treatment Progress
Before orthodontic treatment, the patient underwent periodontal therapy, including scaling and root planing, to control plaque and eliminate inflammation. Periodic periodontal maintenance visits were scheduled during orthodontic treatment.
Presurgical orthodontics began with direct bonding of .022" × .028" Victory Series brackets* in both arches; the lower anterior brackets were rotated 180° to effectively procline the retroclined lower incisors. A customized orthodontic band was used to control the abnormal upper left second molar.
After leveling and alignment of both arches, the diastema was closed with sliding mechanics on .019" × .025" stainless steel archwires. Self-tapping miniscrews** were placed buccally between the roots of the upper first and second molars to provide strong anchorage for retraction of the upper left incisors and midline alignment. To expand the upper arch and coordinate it with the lower arch, irrespective of the occlusal plane inclination, the inclinations of the upper posterior teeth (especially on the left side) were corrected by individual lingual root-torquing bends in the stainless steel archwires, and the inclinations of the lower posterior teeth were corrected by buccal root-torquing bends. Occlusal interferences were removed by grinding the lingual marginal ridges of the upper canines.
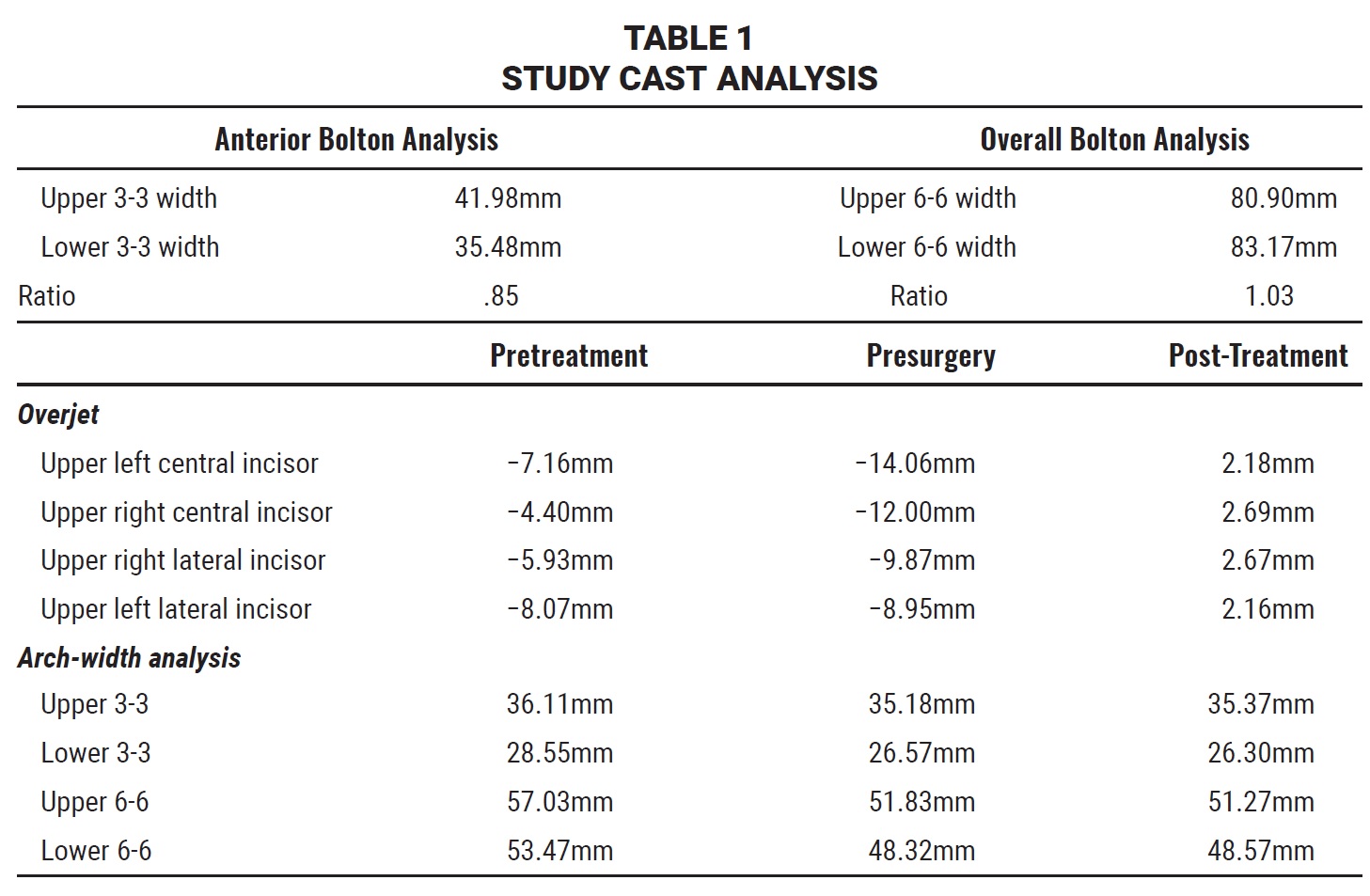
After 24 months of presurgical preparation, the teeth were properly positioned relative to the jaws, and the upper arch was coordinated with the lower arch (Fig. 3A and 3B).

Fig. 3 After 24 months of presurgical orthodontic treatment (continued in next image).
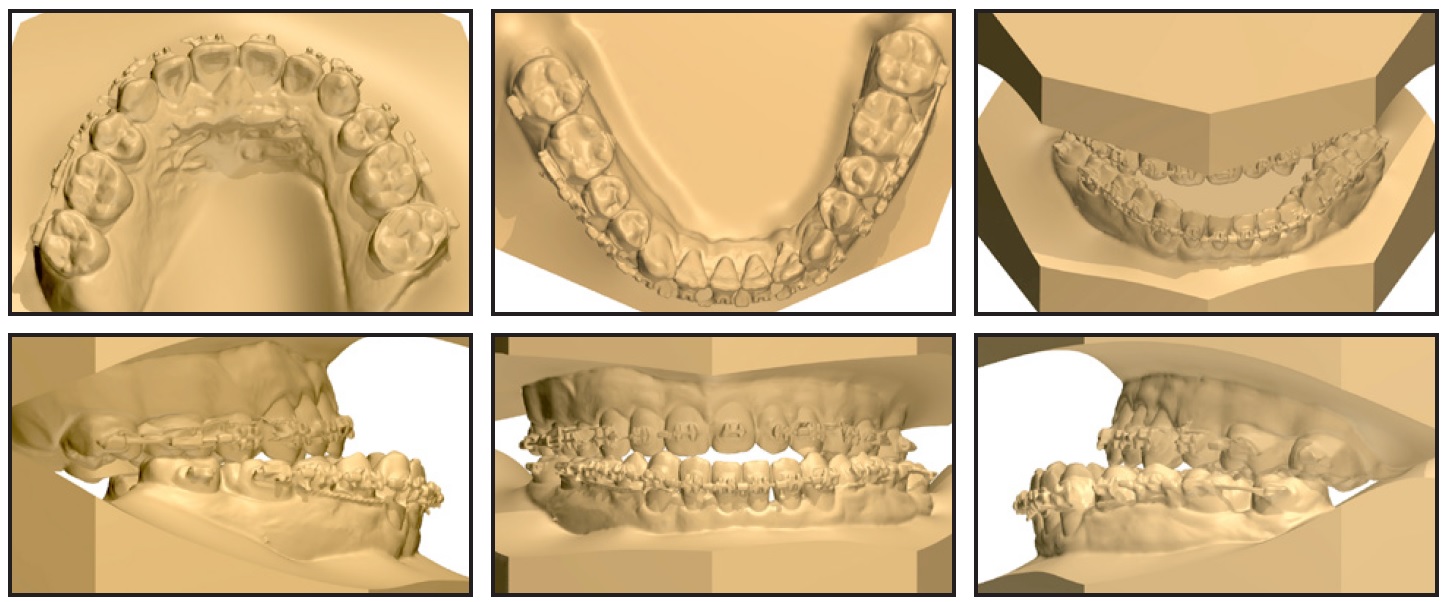
Fig. 3 (cont.) After 24 months of presurgical orthodontic treatment.
A visual treatment objective and model surgery were used to plan a Le Fort I osteotomy, bilateral sagittal split ramus osteotomy, and genioplasty (Fig. 4). The maxilla was advanced by 5mm and drifted to the right by 2.5mm, with a .5mm impaction on the right side and 4mm extrusion on the left, as well as a slight clockwise rotation to correct the open bite. The mandible was set back by 2mm on the left and 9mm on the right, and pogonion was advanced by 4mm. Rigid fixation was used in both the maxilla and the mandible, with no intermaxillary fixation.
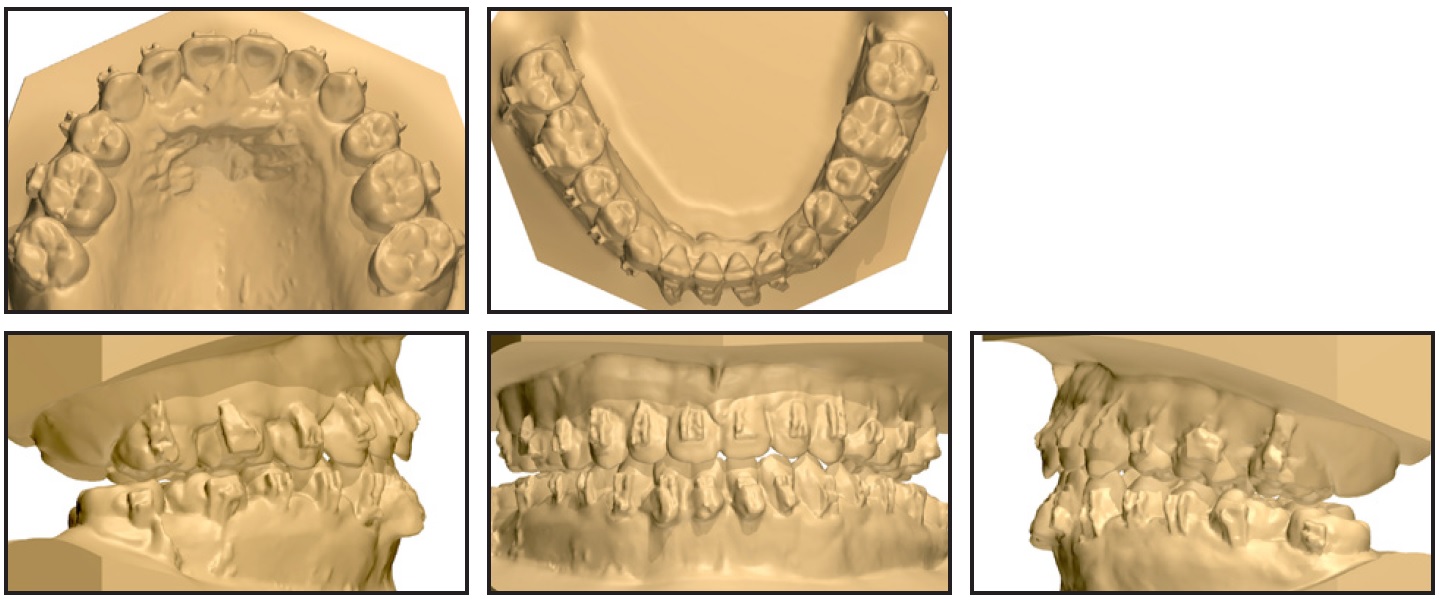
Fig. 4 Model surgery.
The patient was closely monitored for two months after surgery. Postsurgical orthodontic treatment was then initiated, using .019" × .025" stainless steel archwires to finish and detail the occlusion.
After a total 31 months of treatment, all appliances were removed. Considering the typical bilateral discrepancy in masticatory muscle tension in a patient with asymmetrical skeletal Class III dentofacial deformity, we designed special removable acrylic retainers for nighttime wear to help prevent relapse (Fig. 5).
Treatment Results
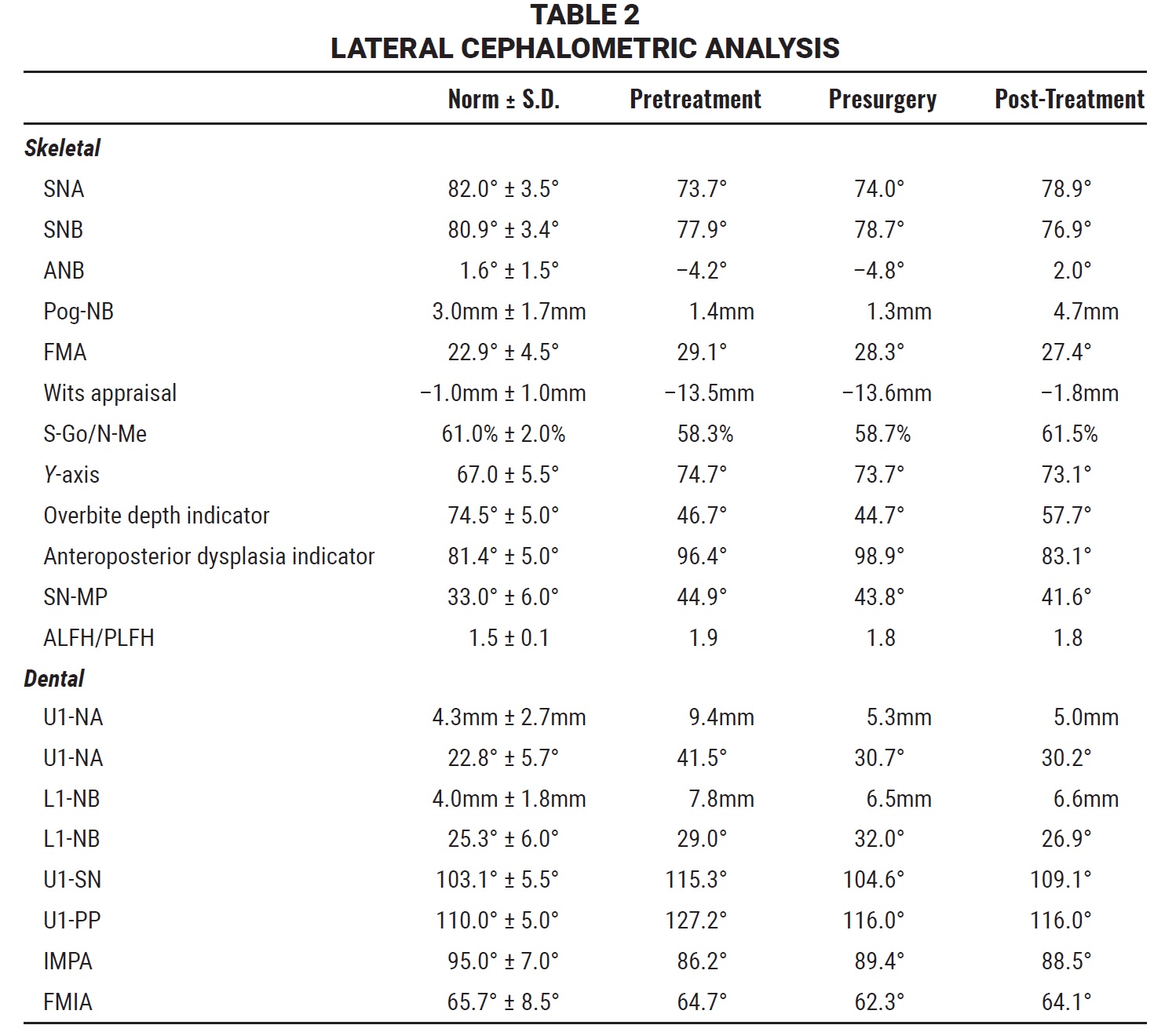
Post-treatment records confirmed good esthetic and occlusal results (Fig. 6A and 6B).

Fig. 5 Special retainers designed for nighttime wear.
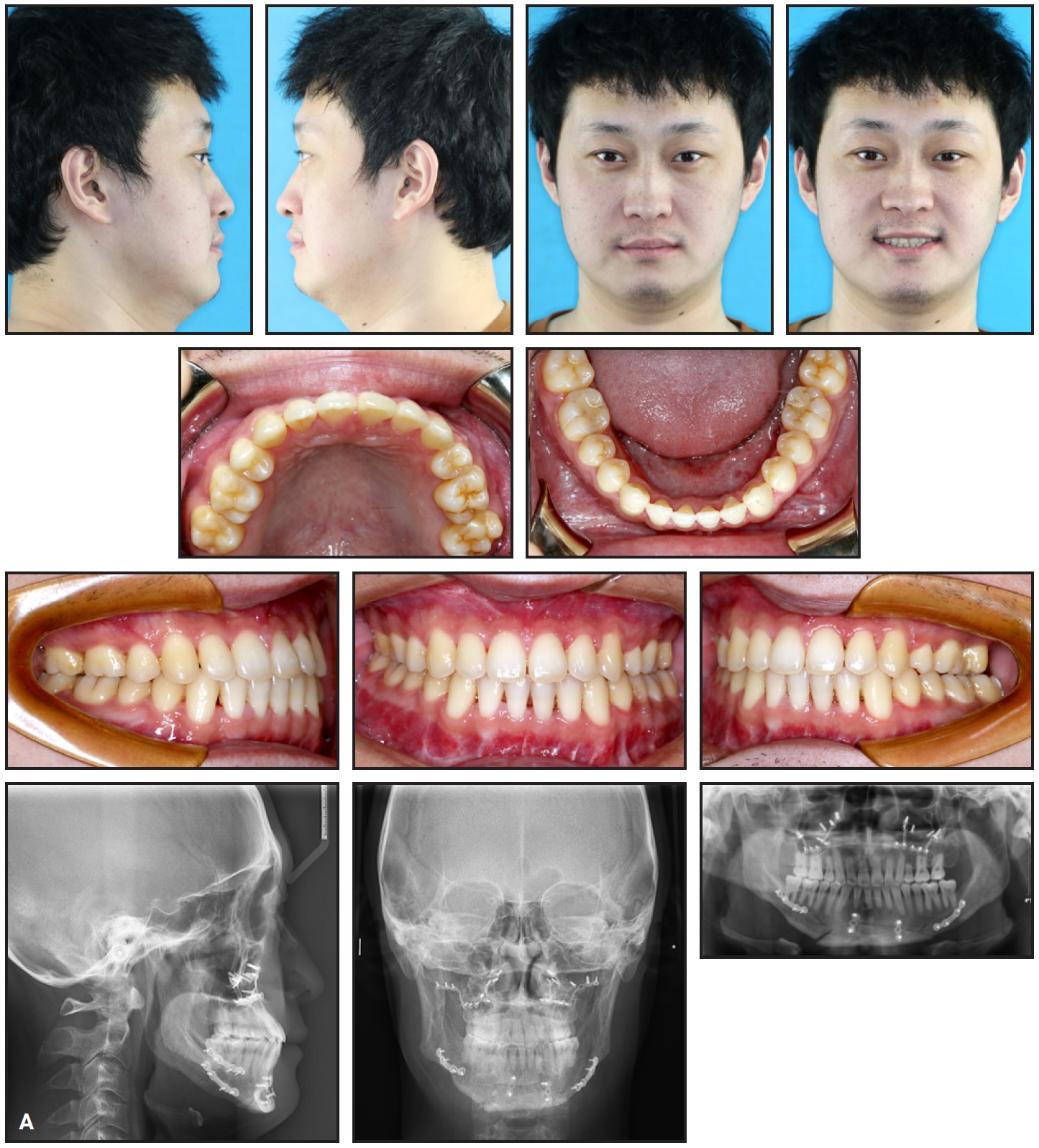
Fig. 6 A. Patient after 31 months of surgical-orthodontic treatment (continued in next image).
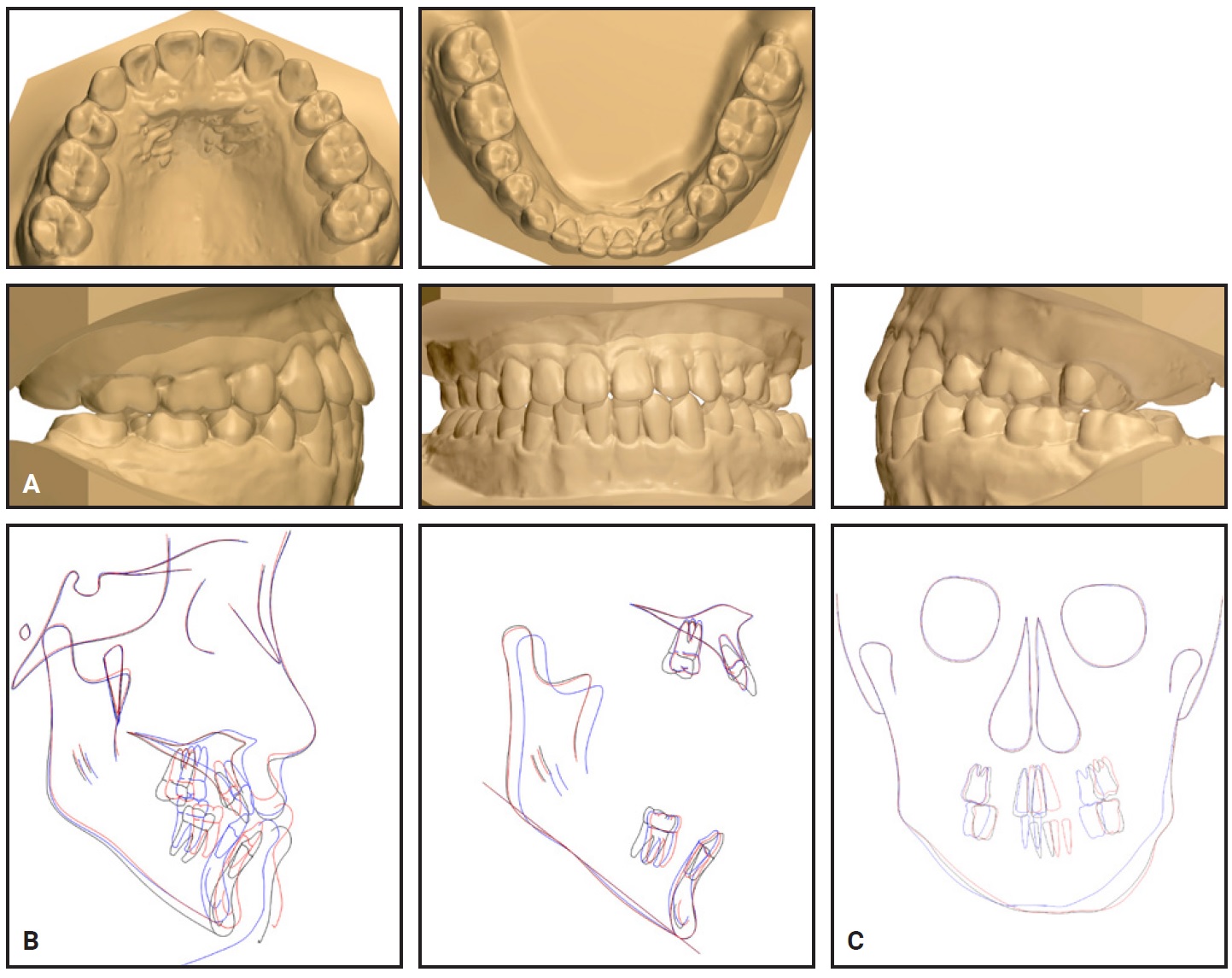
Fig. 6 (cont.) A. Patient after 31 months of surgical-orthodontic treatment. B. Superimposition of lateral cephalometric tracings before treatment (black), before surgery (red), and after treatment (blue). C. Superimposition of posteroanterior cephalometric tracings before treatment (black), before surgery (red), and after treatment (blue).
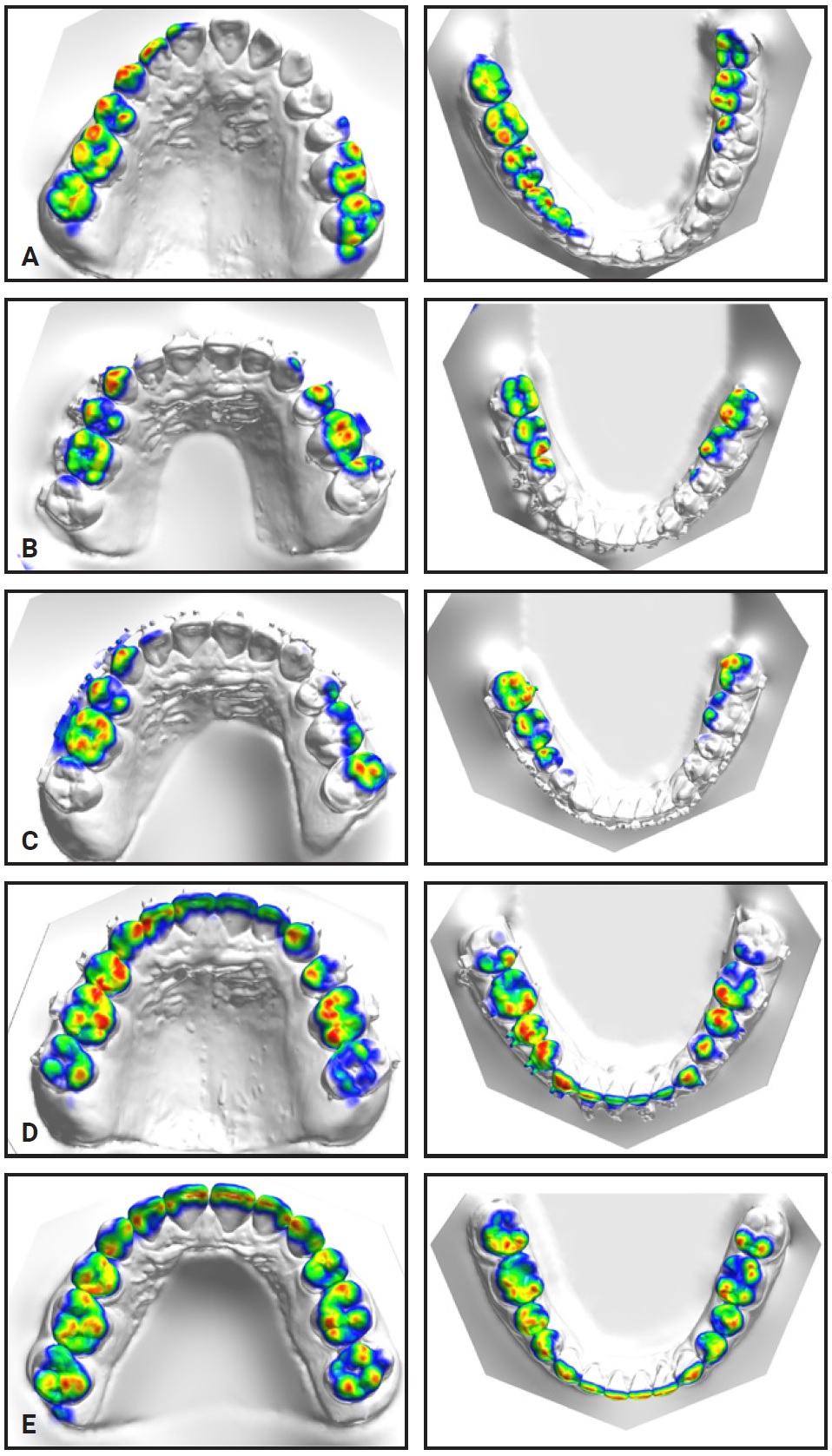
Fig. 7 Occlusal contacts (from OrthoAnalyzer*** 2017 x64). A. Before treatment. B. After 12 months of presurgical orthodontic treatment. C. Before surgery. D. After model surgery. E. After treatment.
The panoramic radiograph indicated parallel root positioning, minor root resorption in the anterior region, and more significant root resorption of the upper left premolar, perhaps related to the patient’s previous occlusal trauma or periodontitis. CBCT evaluation of facial asymmetry showed that both the source and magnitude of the deviations were corrected (Fig. 8, Table 5).
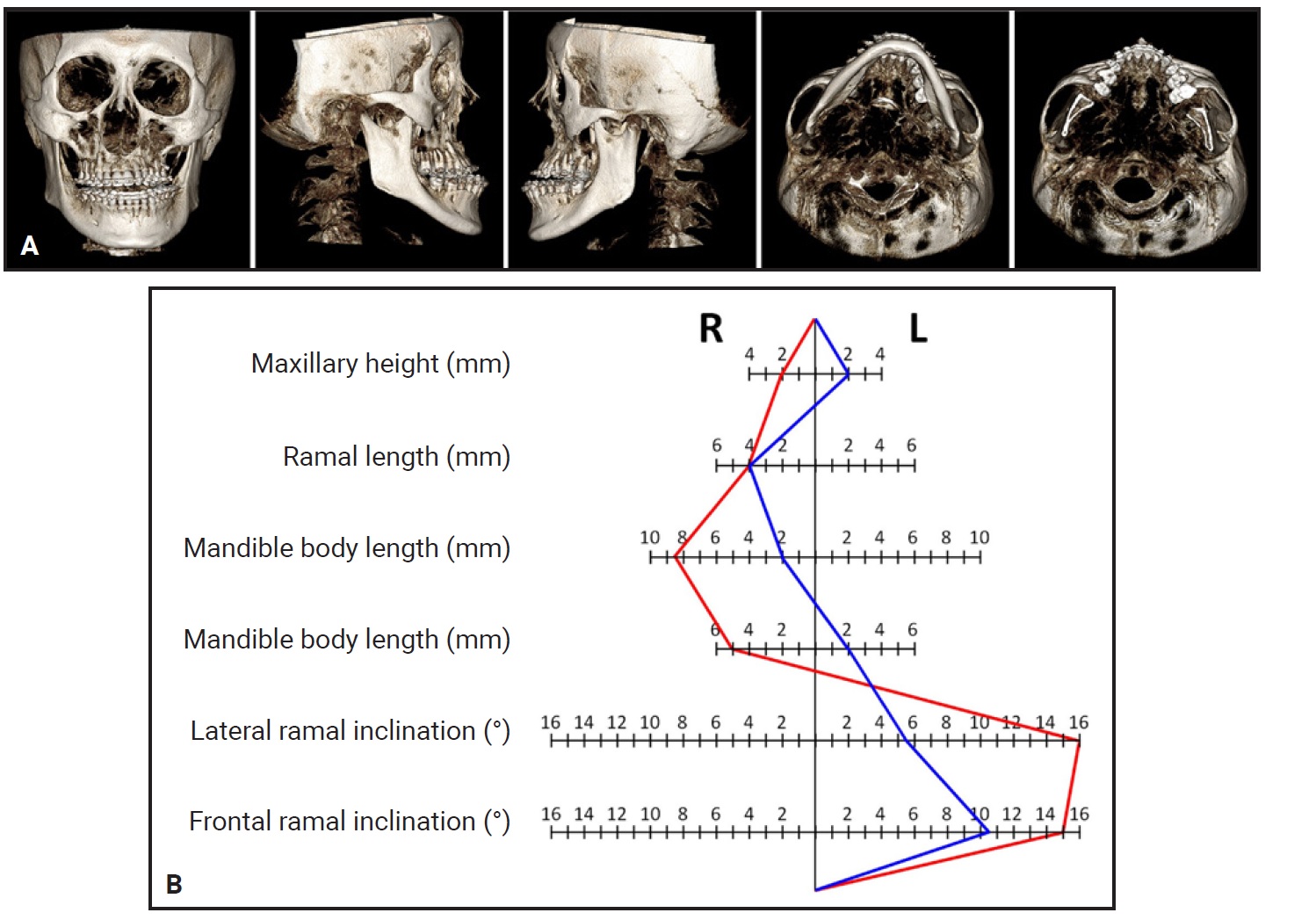
Fig. 8 A. Three-dimensional images of facial asymmetry generated from CBCT. B. Facial asymmetry analysis before surgery (red) and after treatment (blue).
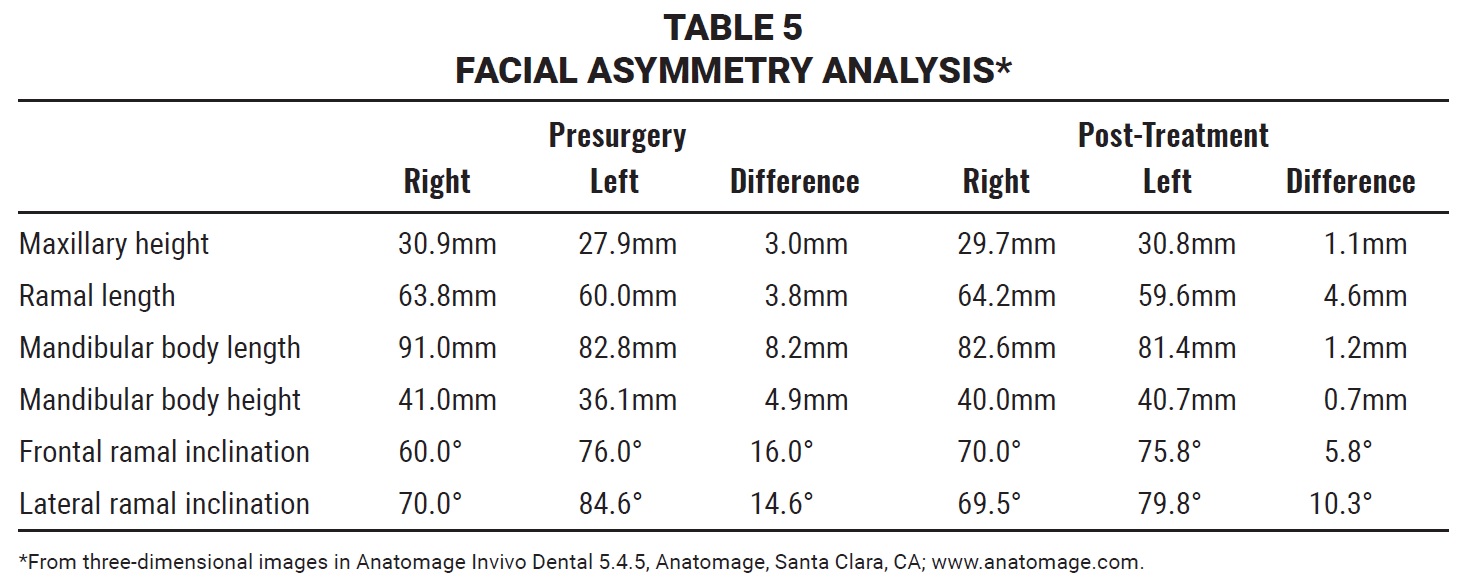
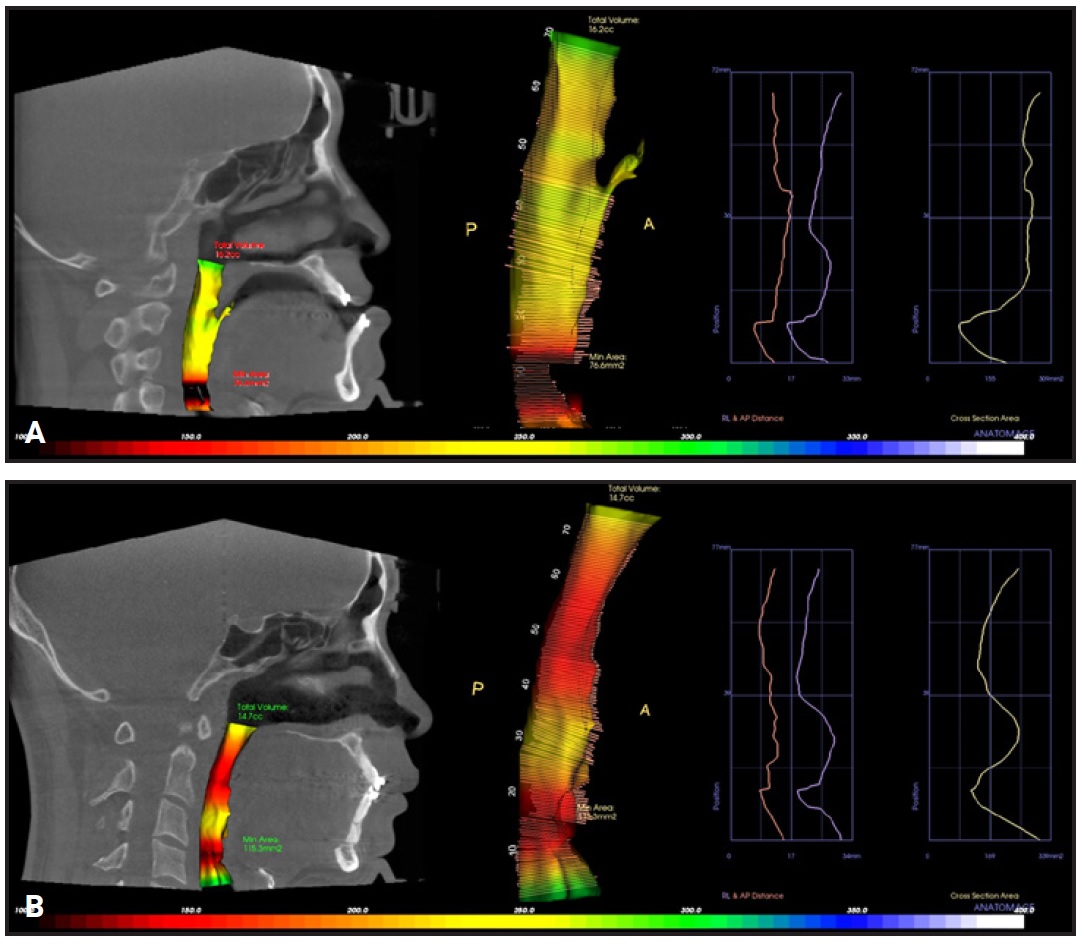
Fig. 9 3D airway images. A. Before surgery. B. After surgery.
The CBCT image of the TMJ showed slight growth of the right condyle during treatment (Fig. 10).
Discussion
Asymmetrical skeletal Class III dentofacial conditions with complex craniomaxillary deformities and dental compensation mechanisms in three dimensions are inevitably complex, usually requiring combined surgical-orthodontic treatment to achieve the best results in terms of occlusal function, facial esthetics, and long-term stability. An accurate evaluation of the facial soft tissues and skeleton, dental compensation mechanisms, TMJ function, and airway conditions is important in determining the appropriate treatment plan and achieving stable long-term results.8,9
Presurgical orthodontic mechanics should intentionally avoid any movements that might contribute to relapse. Kim and Baek maintained that adequate decompensation of the incisors is mandatory, so that mandibular setback surgery can retrude the mandible into a more ideal position with a more esthetic profile.10 In the case shown here, we used U1-PP rather than U1-SN to determine the inclination of the maxillary incisors for presurgical decompensation, since a proper U1-PP angle means the incisors are in normal positions with respect to the maxilla. Therefore, because the dentition and the maxilla are moved as a whole during surgery, the incisors will be in the right place when the maxilla is moved into the desired position, and a proper upper incisor display will be obtained. Presurgical objectives should also include decompensation of the extrusive teeth in an open bite; this promotes mandibular rotation in surgery while avoiding an increase in posterior facial height, thus contributing to stability.3 Without proper vertical control, especially in cases with intermaxillary occlusal interferences, the bite closure during postsurgical orthodontics would create a more forward chin projection.
Because patients with high-angle Class III malocclusions tend to have thin alveolar bone labial and lingual to the lower incisor apices,11 excessive labial proclination of the lower incisors can increase the risk of gingival recession. Troy and colleagues advised caution when decompensating the incisors in patients with severe skeletodental dysplasias.5 In our patient, considering the severe periodontal condition of his lower anterior teeth and his thin gingival biotype, it was crucial to protect the anterior teeth from tongue pressure during labial proclination of the lower incisors. In addition, thin alveolar bone brings the roots closer to cortical bone, with a consequent risk of orthodontically induced inflammatory root resorption (OIIRR) of the anterior teeth. Other potential contributors to OIIRR include treatment duration, magnitude of applied force, amount of tooth movement, and severity and type of malocclusion.12 Despite these risk factors, the post-treatment root resorption in our patient was minor to moderate except for the upper left second premolar. One study showed that a hypofunctionally nonoccluding tooth can accelerate the root destruction resulting from the mechanical stress of orthodontic force.13 Our patient’s pretreatment occlusal trauma and poor periodontal condition could also have contributed to the root resorption of the upper left second premolar.14
In recent years, several authors have expressed concern about the negative effects of a significant mandibular setback on the posterior airway space.15 This may result from the hyoid bone following the direction of the surgical movement as the mandible is displaced downward and backward.16 Studies have also demonstrated the constrictive effect of an insufficient maxilla on the upper airway in patients with skeletal Class III deformities.9,17 Hyperdivergent patients have a narrower anteroposterior pharyngeal dimension, and patients with long faces tend to have extremely narrow airways, both anteroposteriorly and coronally.18 Considering the risk of upper airway obstruction, it is essential to evaluate the upper airway morphology when formulating a treatment plan for an asymmetrical skeletal Class III dentofacial deformity. In our patient, to avoid deleterious positioning of the hyoid bone after the mandibular setback, we performed a genioplasty to advance pogonion by 4mm—not only for esthetic reasons, but to bring the genioglossal muscle forward, pulling the tongue away to avoid upper airway obstruction in the hypopharynx.19 Our 3D airway volume analysis demonstrated enlargement of the palatopharynx. Advancement of the maxilla and counterclockwise rotation of the maxillomandibular complex may also have helped reduce airway obstruction.20 Total airway volume did not change after surgery, and the patient showed no symptoms of obstructive sleep apnea. Considering his hypertrophy and low tongue position, however, we advised the patient to perform tongue exercises throughout treatment to promote adaptation to a reduced capacity of the oral cavity after surgery.
Asymmetrical growth of the condyle may continue in some cases after stabilization of a developmental mandibular deformity, leading to postsurgical relapse of mandibular asymmetry.21 In our patient, post-treatment CBCT imaging of the TMJ showed slight growth of the right condyle, which could have resulted either from asymmetrical growth of the condyle or from hyperplasia caused by the mild mandibular trauma before treatment. Technetium 99m-methyl diphosphonate (99mTc-MDP) is generally used to evaluate developmental characteristics of an asymmetrical mandibular condyle and to provide diagnostic guidance for treatment of these patients.22 Our patient declined a 99mTc-MDP examination because of the expense and inconvenience. To prevent a relapse of the mandibular asymmetry, we built in some overcorrection and designed special retainers that would adapt to the postsurgical jaw position.
Conclusion
In comprehensive surgical-orthodontic treatment of a patient with severely asymmetrical skeletal Class III discrepancies, accurate presurgical decompensation in all three dimensions is the key to success. Careful analysis and planning will determine the magnitude and type of surgical correction. U1-PP should be used rather than U1-SN to define the inclination of the maxillary incisors and ensure ideal positions after surgery. Periodontal and airway conditions and TMJ function are other important factors to consider in establishing an overall treatment plan.
ACKNOWLEDGMENTS: This work was supported by the National Natural Science Foundation of China (NSFC 81801005 and NSFC81870795) and the Jilin Provincial Development and Reform Commission (20181793146).
FOOTNOTES
- *Trademark of 3M, Monrovia, CA; www.3M.com.
- **Ningbo Cibei Medical Treatment Appliance Co. Ltd., Zhejiang, China.
- ***Trademark of 3Shape, Copenhagen, Denmark; www.3shape.com.
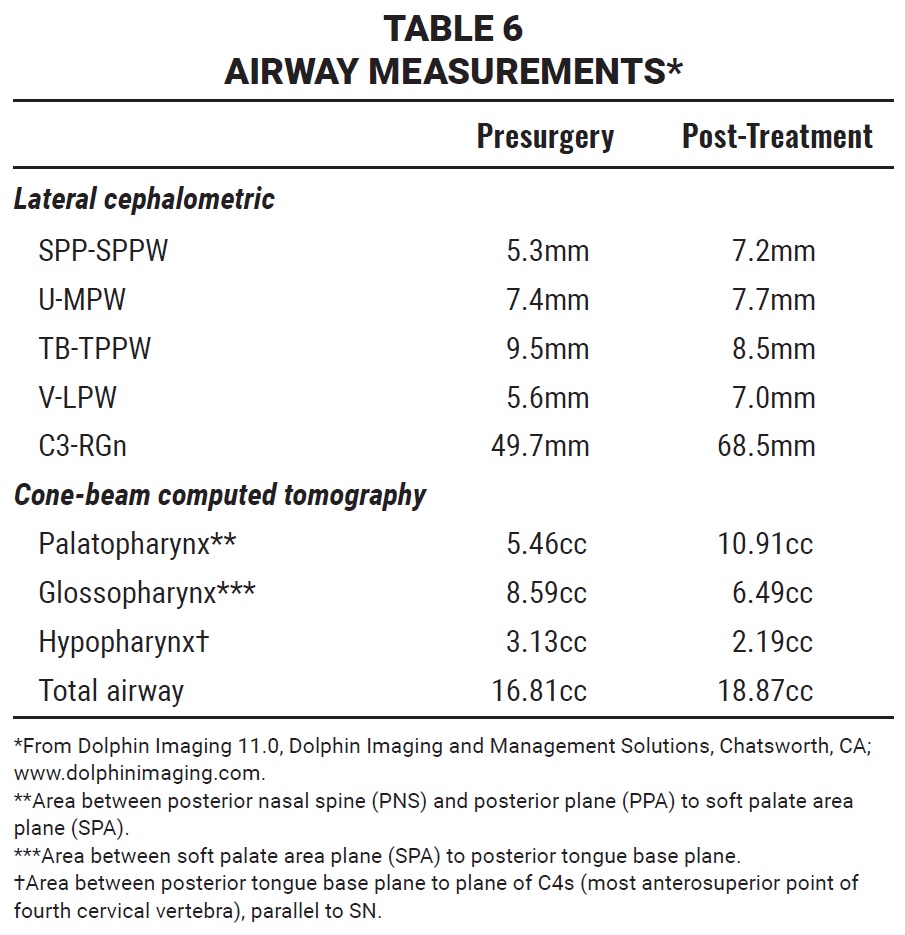
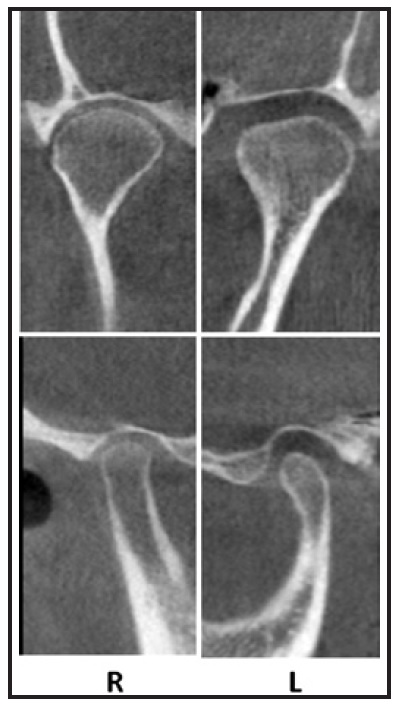
Fig. 10 CBCT images of TMJ after treatment.
REFERENCES
- 1. Hwang, H.S.; Hwang, C.H.; Lee, K.H.; and Kang B.C.: Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry, Am. J. Orthod. 130:779-785, 2006.
- 2. Thiesen, G.; Gribel, B.F.; Kim, K.B.; and Freitas, M.P.M.: Maxillofacial features related to mandibular asymmetries in skeletal Class III Patients, J. Oral Maxillofac. Surg. 75:1015-1025, 2017.
- 3. Proffit, W.R. and White, R.P.: Combined surgical-orthodontic treatment: How did it evolve and what are the best practices now? Am. J. Orthod. 147:205-215, 2015.
- 4. Chen, K.J.; Chen, Y.C.; Cheng, J.H.; Chen, C.M.; and Tseng, Y.C.: Factors related to skeletal relapse in the two-jaw surgery treatment of mandibular prognathism, J. Stomatol. Oral Maxillofac Surg. 119:113-117, 2018.
- 5. Troy, B.A.; Shanker, S.; Fields, H.W.; Vig, K.; and Johnston, W.: Comparison of incisor inclination in patients with Class III malocclusion treated with orthognathic surgery or orthodontic camouflage, Am. J. Orthod. 135:146-147, 2009.
- 6. Tyan, S.; Park, H.S.; Janchivdorj, M.; Han, S.H.; Kim, S.J.; and Ahn, H.W.: Three-dimensional analysis of molar compensation in patients with facial asymmetry and mandibular prognathism, Angle Orthod. 86:421-430, 2016.
- 7. Kim, J.W.; Lee, N.K.; Yun, P.Y.; Moon, S.W.; and Kim, Y.K.: Postsurgical stability after mandibular setback surgery with minimal orthodontic preparation following upper premolar extraction, J. Oral Maxillofac Surg. 71:1968.e1-1968.e11, 2013.
- 8. Lee, J.K.; Jung, P.K.; and Moon, C.H.: Three-dimensional cone beam computed tomographic image reorientation using soft tissues as reference for facial asymmetry diagnosis, Angle Orthod. 84:38-47, 2014.
- 9. Wen, X.; Wang, X.; Qin, S.; Franchi, L.; and Gu, Y.: Three-dimensional analysis of upper airway morphology in skeletal Class III patients with and without mandibular asymmetry, Angle Orthod. 87:526-533, 2017.
- 10. Kim, D.K. and Baek, S.H.: Change in maxillary incisor inclination during surgical-orthodontic treatment of skeletal Class III malocclusion: Comparison of extraction and nonextraction of the maxillary first premolars, Am. J. Orthod. 143:324-335, 2013.
- 11. Park, J.H.; Hong, J.Y.; Ahn, H.W.; and Kim, S.J.: Correlation between periodontal soft tissue and hard tissue surrounding incisors in skeletal Class III patients, Angle Orthod. 88:91-99, 2018.
- 12. Kim, K.W.; Kim, S.J.; Lee, J.Y.; Choi, Y.J.; Chung, C.J.; Lim, H.; and Kim, K.H.: Apical root displacement is a critical risk factor for apical root resorption after orthodontic treatment, Angle Orthod. 88:740-747, 2018.
- 13. Motokawa, M.; Terao, A.; Kaku, M.; Kawata, T.; Gonzales, C.; Darendeliler, M.A.; and Tanne, K.: Open bite as a risk factor for orthodontic root resorption, Eur. J. Orthod. 35:790-795, 2013.
- 14. Abbott, P.V.; Prevention and management of external inflammatory resorption following trauma to teeth, Austral. Dent. J. 61:82-94, 2016.
- 15. Yajima, Y.; Oshima, M.; Iwai, T.; Kitajima, H.; Omura, S.; and Tohnai, I.: Computational fluid dynamics study of the pharyngeal airway space before and after mandibular setback surgery in patients with mandibular prognathism, Int. J. Oral Maxillofac. Surg. 46:839-844, 2017.
- 16. Yamashita, A.L.; Iwaki Filho, L.; Leite, P.C.C.; Navarro, R.D.L.; Ramos, A.L.; Previdelli, I.T.S.; Ribeiro, M.H.D.M.; and Iwaki, L.C.V.: Three-dimensional analysis of the pharyngeal airway space and hyoid bone position after orthognathic surgery, J. Craniomaxillofac. Surg. 45:1408-1414, 2017.
- 17. Zhang, J.; Liu, W.; Li, W.; and Gao, X.: Three-dimensional evaluation of the upper airway in children of skeletal Class III, J. Craniofac. Surg. 28:394-400, 2017.
- 18. Wadhawan, N. and Kharbanda, O.P.: An airway study of different maxillary and mandibular sagittal positions, Eur. J. Orthod. 35:271, 2013.
- 19. Du, W.; He, D.; Wang, Y.; Liu, H.; Liao, C.; Fei, W.; and Luo, E.: Upper airway changes after mandibular setback and/or advancement genioplasty in obese patients, J. Oral Maxillofac. Surg. 75:2202-2210, 2017.
- 20. Torres, H.M.; Valladares-Neto, J.; Torres, E.M.; Freitas, R.Z.; and Silva, M.A.G.: Effect of genioplasty on the pharyngeal airway space following maxillomandibular advancement surgery, J. Oral Maxillofac. Surg. 75:1-12, 2017.
- 21. Ikeda, M.; Miyamoto, J.J.; Takada, J.I.; and Moriyama K.: Association between 3-dimensional mandibular morphology and condylar movement in subjects with mandibular asymmetry, Am. J. Orthod. 151:324-334, 2017.
- 22. Lima, G.M.; Diodato, S.; Costabile, E.; Cicoria, G.; Civollani, S.; Marchetti, C.; Guidalotti, P.L.; Pettinato, C.; Nanni, C.; and Fanti, S.: Low dose radiation 18F-fluoride PET/CT in the assessment of unilateral condylar hyperplasia of the mandible: Preliminary results of a single centre experience, Eur. J. Hybrid Imaging 2:7, 2018.




COMMENTS
.