MASTER CLINICIAN
David B. Kennedy, BDS, MSD, FRCD(C)
Associate Editor Peter Sinclair conceived this department devoted to recognizing the Master Clinicians who have made the orthodontic specialty what it is today. Every few months, Dr. Sinclair will delve into the career story and treatment principles of one of these seminal figures. We welcome your nominees for future Master Clinicians.
Dr. David Kennedy of the University of British Columbia (UBC) is our featured Master Clinician this month. He addresses an issue that has been a point of contention among orthodontists throughout the history of the specialty: early treatment. There are valid arguments regarding early treatment, both pro and con, with highly respected practitioners on each side of the debate. In this article, Dr. Kennedy presents a number of treated cases as excellent examples of what can be accomplished.
RGK
DR. SINCLAIR Who were your mentors?
DR. KENNEDY I attended two outstanding graduate programs where the department chairs—Drs. Jim Roche, pediatric dentistry at Indiana University, and Don Joondeph, orthodontics at the University of Washington School of Dentistry—respected the students, held the highest standards, and led by example. Both served as directors on their respective American boards. They encouraged their students to become board-certified, something that I did for both specialties and would highly recommend; it helped me be more critical of my work. They were my mentors, along with selected faculty from the University of Washington, including Bob Little, Vince Kokich, and Peter Shapiro.
Similar articles from the archive:
- MASTER CLINICIAN David M. Sarver, DMD, MS March 2021
- MASTER CLINICIAN Anoop Sondhi, DDS, MS May 2019
- MASTER CLINICIAN Mauro Cozzani, DMD, MScD January 2017
DR. SINCLAIR What is your philosophy, and how does it guide you?
DR. KENNEDY When I do a clinical exam, I ask myself the following three questions:
- What do you see? Are the occlusion, dental development, and eruption sequence normal?
- What should you see? This requires a comprehensive knowledge of growth and development. The clinician must be able to recognize normal and abnormal development at various stages of the mixed dentition.
- What is the difference? Usually you treat the difference, based upon the scientific evidence of treatment success.
I ask and answer three philosophical questions when considering early treatment, and I use evidence-based research to determine my decision-making.1
1. Can I treat this permanently? Examples are anterior and posterior crossbite correction. For nonskeletal anterior crossbite correction, a maxillary removable appliance can often be used, unless significant incisor rotational and torque control are needed (Fig. 1A and 1B).

Fig. 1 Case 1. A. 7½-year-old male patient with anterior crossbite and forward mandibular shift before treatment (continued in next image).

Fig. 1 (cont.) Case 1. B. Anterior crossbite corrected after nine months of treatment with removable maxillary appliance; mandibular incisors show spontaneous improvement in alignment.
Correction is usually accomplished in four months of full-time wear. A posterior biteplane is used when the vertical overbite exceeds 2-3mm, to allow bite opening for anterior crossbite correction; the biteplane is reduced after the crossbite is corrected to prevent deepening of the overbite. Space must be available for tooth movement to occur; therefore, maxillary expansion may sometimes be needed (Fig. 2).

Retention is not needed when the overbite is complete. Any gingival retreat on the mandibular incisors will improve after crossbite correction2 (Fig. 3). Mandibular incisor irregularity often improves secondary to maxillary incisor alignment, provided adequate space is available.
Bilateral posterior crossbites represent only 10% of mixed-dentition crossbites, with the unilateral presentation being more common. Unilateral mixed-dentition posterior crossbites often show a Class II tendency on the crossbite side, with the non-crossbite side being Class I (Fig. 4).
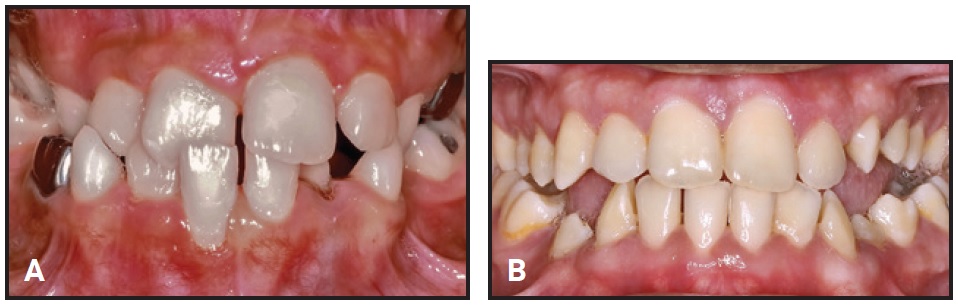
Fig. 3 Case 3. A. 9-year-old patient with crossbite before treatment. B. Two years later, showing improvement in gingival retreat after crossbite correction (six months of active treatment). Deciduous canines extracted to relieve crowding; no retention needed.

Fig. 4 Case 4. 8½-year-old female patient with unilateral left posterior crossbite, mandible shifted to crossbite side, and chin and mandibular dental midlines deflected to left before treatment. Crossbite side shows Class II tendency.
The mandibular dental and skeletal midlines are deflected toward the crossbite side, with asymmetry in the condyle position before treatment owing to the shift of the mandible toward the crossbite side. These asymmetries improve secondary to maxillary expansion, which eliminates the shift of the mandible (Fig. 5).

Fig. 5 Case 4. After Phase I treatment involving four months of slow maxillary expansion with fixed Hyrax* expander, followed by six months of retention with same passive appliance. Left Class II tendency improved, with chin and midlines corrected and mandibular shift eliminated.
A diagnostic tip relative to the need for maxillary expansion is that the maxilla shows more crowding than the mandible. Both bilateral and unilateral posterior crossbites with functional shifts require maxillary expansion, but the bilateral crossbite presentation requires more expansion.
In the early mixed dentition, slow maxillary expansion can be used with one-quarter turn every two to three days. Because the suture is immature, lower force levels are required to obtain skeletal expansion. Rapid maxillary expansion in the young child may widen the nasal base, hence the recommendation for slow expansion. Fixed expanders, such as a Haas-type, Hyrax,* or Quad-Helix,** are recommended. About 5-6mm of expansion is usually required for correction of unilaterally presenting crossbites.3
Maxillary constriction is sometimes caused by prolonged digit habits; this can be treated simultaneously by incorporating a habit-breaking crib. Overexpansion of 2mm per side and a minimum six months of fixed retention yield excellent stability.3 When an open bite exists, retention with the crib should be continued until a positive overbite has been established.
2. Is there something damaging that I cannot leave? Examples are gingival retreat from an anterior crossbite, ectopic canines that can be guided into better positions, and unerupted incisors from mesiodens or trauma to the deciduous incisors.
Palatally displaced ectopic canines occur more often in females and those with small or missing lateral incisors, or with a family history of ectopic canines.4-8 Distal crown tipping of the maxillary lateral incisors is a normal development in the early mixed dentition, which is called the “ugly duckling” stage. When distal tipping of the lateral incisor persists as the maxillary canines should erupt, however, this hints that the maxillary permanent canines may be ectopic, which calls for radiographic assessment (Fig. 6). A panoramic radiograph or periapical films are warranted at age 10-11 to check the canine positions, especially when the deciduous canines are not mobile. The maxillary deciduous canines should be mobile six months after mandibular permanent canine eruption.
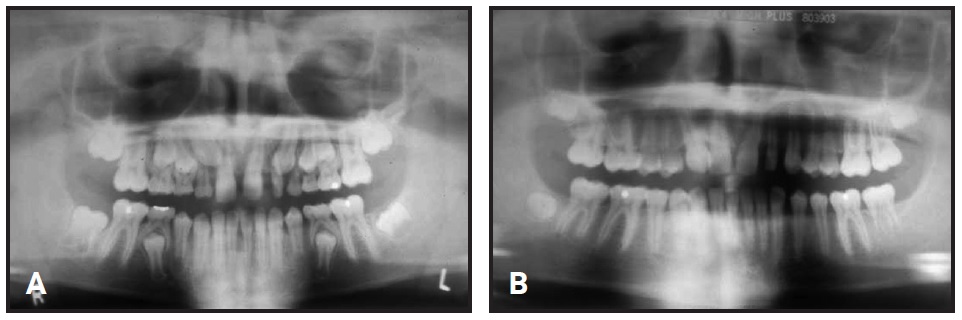
Fig. 6 Case 5. A. 11½-year-old patient with bilateral ectopic maxillary canines, missing maxillary right lateral incisor, and small left lateral incisor before extraction of maxillary deciduous canines. Late eruption for chronological age is common with ectopic teeth. B. One year later, positions of maxillary permanent canines improved after extraction of deciduous canines.
Extraction of the maxillary deciduous canines, maxillary expansion, and/or headgear treatment frequently improve the ectopic permanent canine positions and encourage normal eruption. Similarly, space opening improves the likelihood that the ectopic permanent canine will erupt without surgical intervention.9-11 When the tip of the maxillary canine has not crossed the midpoint of the lateral incisor, extraction of the deciduous canine alone results in an improved permanent canine position 91% of the time.12
3. Will early treatment help significantly with future Phase II treatment? Will early intervention move the case to nonextraction or make Phase II easier or shorter? Examples are early Class III treatment, leeway space management, and serial extraction.
Mild to moderate crowding can be resolved with leeway space management. In 66-70% of cases, 5mm of crowding can be resolved with a late-mixed-dentition mandibular lingual arch13 (Fig. 7A and 7B).

Fig. 7 Case 6. A. 9-year-old female patient with Class I malocclusion, mild mandibular crowding, and early loss of mandibular right second deciduous molar before treatment (continued in next image).

Fig. 7 (cont.) Case 6. B. After 15 months of treatment, with mandibular lingual arch in place.
The mandibular second deciduous molars may need to be removed to allow the crowding to resolve by distal drifting of the canines and first premolars into the edentulous space.13 The lingual arch is left in place until the permanent second molars erupt, with good long-term stability (Fig. 8A and 8B).14

Fig. 8 Case 6. A. Patient at age 12, showing mandibular premolar rotations prior to start of Phase II. Lingual arch removed previously, after second molar eruption (continued in next image).

Fig. 8 (cont.) Case 6. B. After 18 months of Phase II treatment with fixed appliances.
The intermolar angle between the first and second molars must be evaluated before lingual arch placement, because there is a more of a tendency for mandibular second permanent molar impaction when this angle exceeds 24°.15
Serial extraction is appropriate in 15% of cases—those that exhibit severe crowding of 8mm or more16 (Fig. 9).
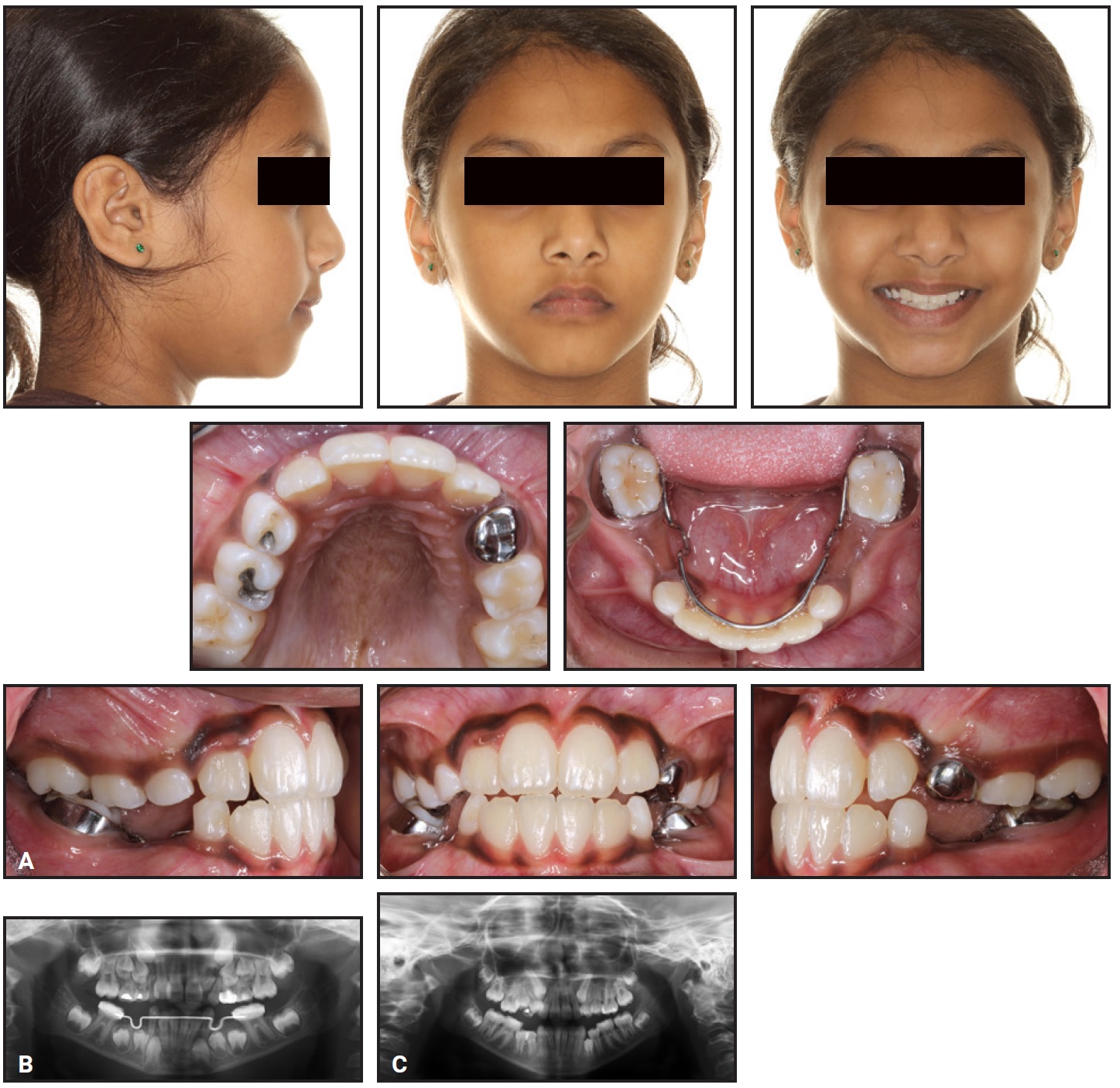
Fig. 9 Case 7. A. 9-year-old female Class I patient with mixed-dentition crowding before treatment. B. Panoramic radiograph taken 18 months earlier, before extraction of deciduous canines. C. Two years later, prior to first premolar extractions.
Indications for serial extraction are Class I occlusions with more than 7-8mm of crowding per arch. These patients should have protrusive dentitions, full faces, shallow overbites or open bites, and no missing or ectopic teeth. Serial extraction is contraindicated in patients with flat profiles, short lower faces, retrusive incisors, or minimal crowding. Severely bimaxillary protrusive patients, who require maximum retraction of the incisors, are not suitable candidates for serial extraction.
Serial extraction involves deciduous canine extractions as the lateral incisors erupt, allowing the crowded permanent incisors to spontaneously align. At age 9-10, the first deciduous molars are extracted. The purpose is to accelerate the eruption of the first premolars. Because normal maxillary eruption involves the first premolars erupting ahead of the canines, this is seldom needed in the maxilla. The first premolars are then extracted upon eruption, usually at age 11-12 (Fig. 10).
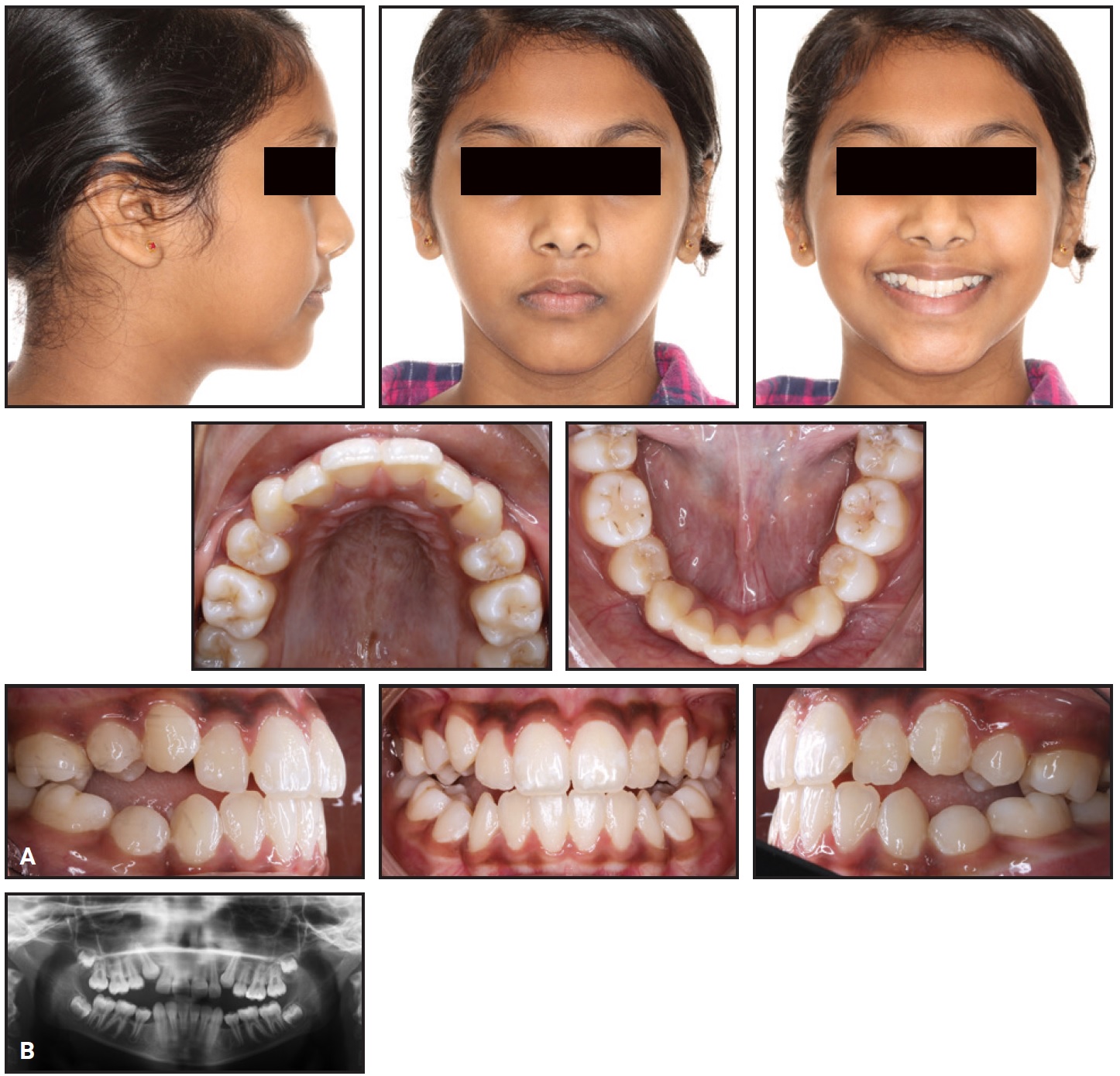
Fig. 10 Case 7. A. Patient at age 13, after extraction of first premolars, showing Class I relationship with poor interdigitation, but canines erupting into attached gingiva. B. After premolar extractions and drifting of teeth. Note tipping of teeth adjacent to mandibular extractions and difference between mandibular anterior and posterior occlusal planes, with deepening curve of Spee.
One modification to be considered is whether the premolars should be enucleated rather than extracted upon eruption. This is particularly indicated when the permanent canine is erupting ahead of the first premolar. Some children are apprehensive about extractions; as a result, serial extractions can become an adverse behavioral issue for needle-phobic children. After extractions and before braces, there is a period of what is commonly called “driftodontics,” in which spontaneous alignment occurs.17
A major advantage of serial extraction is that the crowded permanent canines are not displaced buccally from the arch, so they erupt into the attached gingiva. Crowding tends to improve because of the extractions,18 but we commonly see tipping of the mandibular teeth adjacent to the extraction sites. The mandibular curve of Spee also deepens, with a difference between the mandibular posterior and anterior occlusal planes. Comprehensive treatment to detail the alignment, close residual extraction spaces, and parallel the roots should be done in the early permanent dentition, with a reduced treatment time because of the spontaneous alignment18 (Fig. 11).
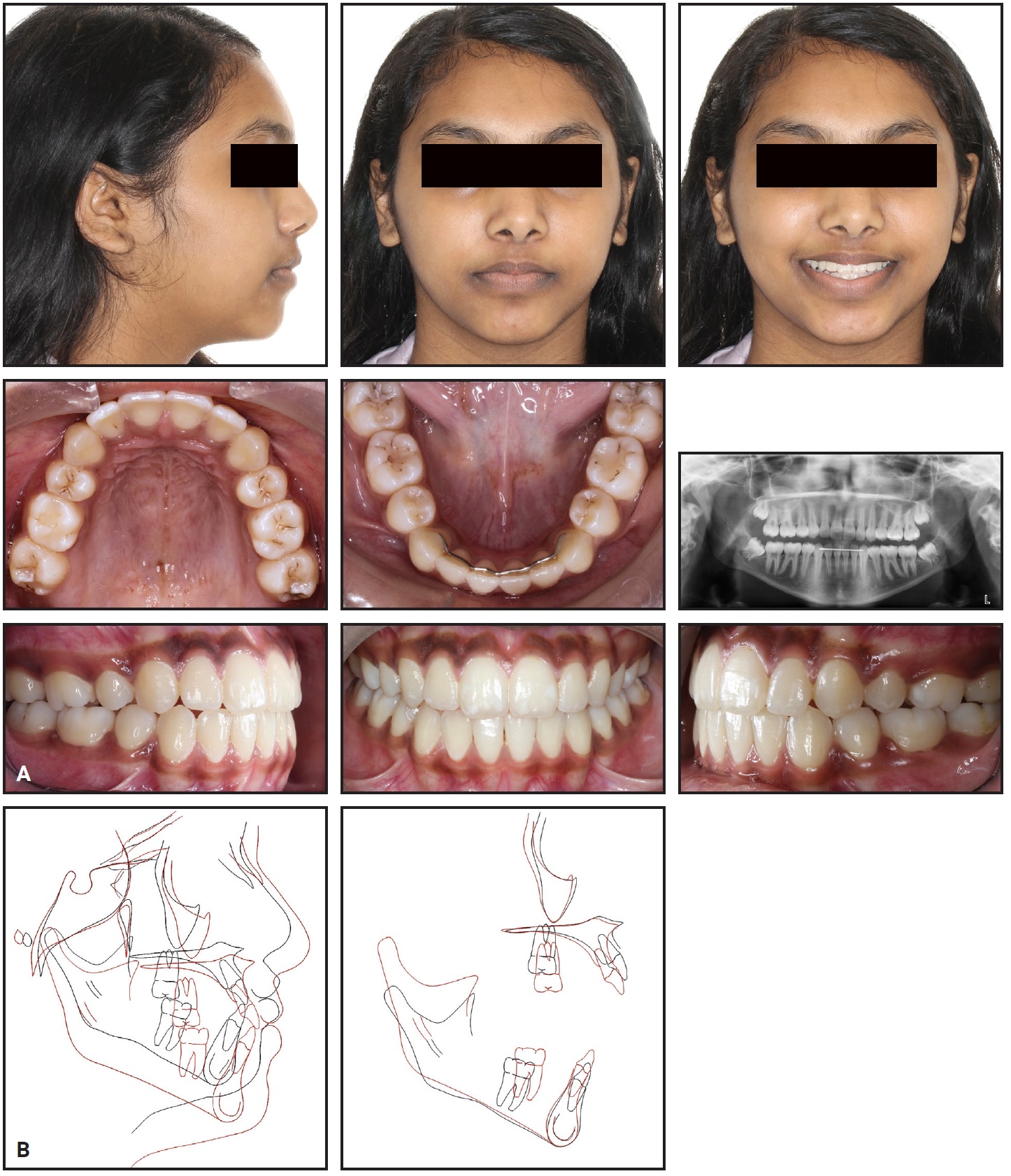
Fig. 11 Case 7. A. Two years later, after Phase II treatment with fixed appliances. Panoramic radiograph shows good root parallelism. B. Superimposition of pre- and post-treatment cephalometric tracings. Note excellent incisor torque and positioning.
Serial extraction cases also have a lower Peer Assessment Rating score compared with late premolar extraction cases, making them easier to treat.18
DR. SINCLAIR What diagnostic principles do you follow?
DR. KENNEDY Diagnosis is the same for early and late treatment.19 This is best handled by looking at the face, followed by a “planes of space concept”—looking at the anteroposterior, transverse, vertical, and perimeter planes of space. A family history, especially as it relates to anteroposterior crowding, missing teeth, and parental treatment, is most helpful. Other information, such as the patient’s or parents’ chief complaint, anticipated child cooperation, and occlusal function, will be useful. Other factors to consider include TMJ, occlusion, and airway.
Full orthodontic records are necessary. Written diagnostic findings with objectives made from the problem list, based on the planes of space database, will lead the clinician to develop treatment alternatives.19 These alternatives should include the advantages and disadvantages, leading to informed consent. From there, the treatment goals are selected, and, lastly, the appliance is chosen—not the other way around. Too often, a clinician takes a continuing education course and wants to use a certain appliance. Treatment in the mixed dentition should be objective- and not appliance-driven.
“Objective-driven” treatment includes expanding the maxilla to correct a unilaterally presenting posterior crossbite by eliminating a functional shift, thus reducing asymmetry. I try to use a short duration, 12-15 months or less, to achieve the objectives. Patient fatigue is then reduced should future Phase II treatment be needed. Parents may have limited funds or insurance coverage for their children’s orthodontic treatment; responsible clinicians will factor this into their best short- and long-term decision-making. Extended, expensive Phase I treatment will unnecessarily increase patient costs and may reduce future insurance coverage if Phase II treatment is needed.
DR. SINCLAIR What important mechanical principles do you employ?
DR. KENNEDY Keep it simple. When using slow maxillary expansion, keep the expander in place as its own retainer. After active expansion, tie off the expansion screw with a ligature wire. Use slow maxillary expansion and limited fixed appliances with coils to open up space for crowded canines when needed. Avoid long spans in 2 × 4 appliances; deciduous molars can be bonded depending on their longevity and stability. This reduces the chance of wires coming out with the help of the child’s fingers! For retention, I use a Hawley with Adams clasps on the upper first molars and a soldered labial bow, and I keep the acrylic away from the erupting permanent premolars and canines (Fig. 12).

Fig. 12 Mixed-dentition maxillary Hawley retainer with Adams clasps on first molars, spurs to control incisors, and labial bow soldered to Adams clasps; acrylic cleared away from premolars and canines.
DR. SINCLAIR What is your best clinical tip?
DR. KENNEDY Use fixed appliances as much as possible to eliminate the need for patient compliance. When using partial fixed appliances, be mindful of the deciduous tooth’s longevity. Remember that the malocclusion is stable, so don’t move teeth beyond the alveolar housing. Maxillary expansion is quite stable, while mandibular expansion is often followed by a reduction in intercanine width and relapse. Therefore, try to avoid lower-arch expansion.20
DR. SINCLAIR What is your greatest clinical challenge?
DR. KENNEDY Choosing the best cases to treat early. A great place to start is to select mixed-dentition cases that present with good mandibular arches. The clinician is then faced with changing the maxillary arch to meet the good mandibular arch. The outcomes are usually best when this strategy is used. The earlier mixed-dentition treatment is started, the more extended will be the time available to evaluate its long-term success, since both relapse and normal growth can occur after the initial treatment. Comprehensive knowledge of the normal growth and development of the skeleton and dentition is essential.
There are many other instances of appropriate early orthodontic treatment that have been omitted from this article for space reasons. They will be covered in future articles.
DR. SINCLAIR Thank you for sharing your clinical experience with our readers.
ACKNOWLEDGMENTS: Dr. Kennedy gratefully acknowledges the assistance of Drs. James Andrews and Abdulraheem Alwafi (graduate orthodontic students at UBC), who handled the proofreading, illustrations, and references.
FOOTNOTES
- *Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- **Rocky Mountain Orthodontics, Denver, CO; www.rmortho.com.
REFERENCES
- 1. Kennedy, D.B.: Early treatment options, PCSO Bull. 82:19-22, 2010.
- 2. Harrison, R.; Kennedy, D.; and Leggott, P.: Anterior dental crossbite: Relationship between incisor crown length and incisor irregularity before and after orthodontic treatment, Pediat. Dent. 15:394-397, 1993.
- 3. Huynh, T.; Kennedy, D.B.; Joondeph, D.R.; and Bollen, A.M.: Treatment response and stability of slow maxillary expansion using Haas, Hyrax, and Quad-Helix appliances: A retrospective study, Am. J. Orthod. 136:331-339, 2009.
- 4. Becker, A. and Chaushu, S.: Etiology of maxillary canine impaction: A review, Am. J. Orthod. 148:557-567, 2015.
- 5. Johnston, W.D.: Treatment of palatally impacted canine teeth, Am. J. Orthod. 56:589-596, 1969.
- 6. Becker, A.; Smith, P.; and Behar, R.: The incidence of anomalous maxillary lateral incisors in relation to palatally-displaced cuspids, Angle Orthod. 51:24-29, 1981.
- 7. Oliver, R.G.; Mannion, J.E.; and Robinson, J.M.: Morphology of the maxillary lateral incisor in cases of unilateral impaction of the maxillary canine, Br. J. Orthod. 16:9-16, 1989.
- 8. Sacerdoti, R. and Baccetti, T.: Dentoskeletal features associated with unilateral or bilateral palatal displacement of maxillary canines, Angle Orthod. 74:725-732, 2004.
- 9. Kokich, V.G.: Surgical and orthodontic management of impacted maxillary canines, Am. J. Orthod. 126:278-283, 2004.
- 10. Olive, R.J.: Orthodontic treatment of palatally impacted maxillary canines, Austral. Orthod. J. 18:64, 2002.
- 11. Armi, P.; Cozza, P.; and Baccetti, T.: Effect of RME and headgear treatment on the eruption of palatally displaced canines: A randomized clinical study, Angle Orthod. 81:370-374, 2011.
- 12. Ericson, S. and Kurol, J.: Early treatment of palatally erupting maxillary canines by extraction of the primary canines, Eur. J. Orthod. 10:283-295, 1988.
- 13. Gianelly, A.A.: Crowding: Timing of treatment, Angle Orthod. 64:415-418, 1994.
- 14. Dugoni, S.A.; Lee, J.S.; Varela, J.; and Dugoni, A.A.: Early mixed dentition treatment: Postretention evaluation of stability and relapse, Angle Orthod. 65:311-320, 1995.
- 15. Sonis, A. and Ackerman, M.: E-space preservation: Is there a relationship to mandibular second molar impaction? Angle Orthod. 81:1045-1049, 2011.
- 16. Proffit, W.R.; Fields, H.W. Jr.; Larson, B.; and Sarver, D.M.: Early (serial) extraction, in Contemporary Orthodontics, 6th ed., Mosby Elsevier, Philadelphia, 2018, p. 424.
- 17. Gönül, N.Y. and Sayinsu, K.: Treatment of a Class II patient with four premolar extractions and driftodontics in the lower jaw, Turk. J. Orthod. 30:89-100, 2017.
- 18. O’Shaughnessy, K.W.; Koroluk, L.D.; Phillips, C.; and Kennedy, D.B.: Efficiency of serial extraction and late premolar extraction cases treated with fixed appliances, Am. J. Orthod. 139:510-516, 2011.
- 19. Proffit, W.R.; Fields, H.W. Jr.; Larson, B.; and Sarver, D.M.: Diagnosis and treatment planning, in Contemporary Orthodontics, 6th ed., Mosby Elsevier, Philadelphia, 2018.
- 20. Little, R.M.; Riedel, R.A.; and Stein, A.: Mandibular arch length increase during the mixed dentition: Postretention evaluation of stability and relapse, Am. J. Orthod. 97:393-404, 1990.




COMMENTS
.