Functional Class II Treatment with a Miniplate-Anchored Herbst Appliance
Numerous functional orthopedic appliances have been developed over the past century for the correction of skeletal Class II malocclusions.1,2 Among the fixed bite-jumping appliances, the Herbst* system is the best known.3,4
In addition to the advantage of not requiring patient compliance, the Herbst offers the potential to improve the facial soft tissues, particularly in a patient with a convex profile, retrusive lower lip, and prominent sublabial fold.5 The ideal treatment timing is in the permanent dentition, at or just after the pubertal growth peak.4 Because mandibular growth stimulation is also possible in post-adolescent young adults, however, a new concept of Class II therapy has been proposed, in which the Herbst appliance provides an alternative to orthognathic surgery.6 The main disadvantage of the Herbst is in its dental side effects; in particular, lower incisor proclination due to loss of anchorage is almost unavoidable with conventional mechanics.7
Over the past 15 years, the use of skeletal anchorage in orthodontics and dentofacial orthopedics has increased exponentially. Miniplates have been incorporated in several methods of Class II and Class III orthopedic treatment.8 The following case report illustrates the use of a modified Herbst appliance with miniplate anchorage, taking advantage of the Herbst’s effectiveness in correcting mandibular retrusion9 while avoiding buccal tipping of the mandibular incisors.
Case Report
A 13-year-old male presented with the chief complaint that his upper teeth were too prominent (Fig. 1).
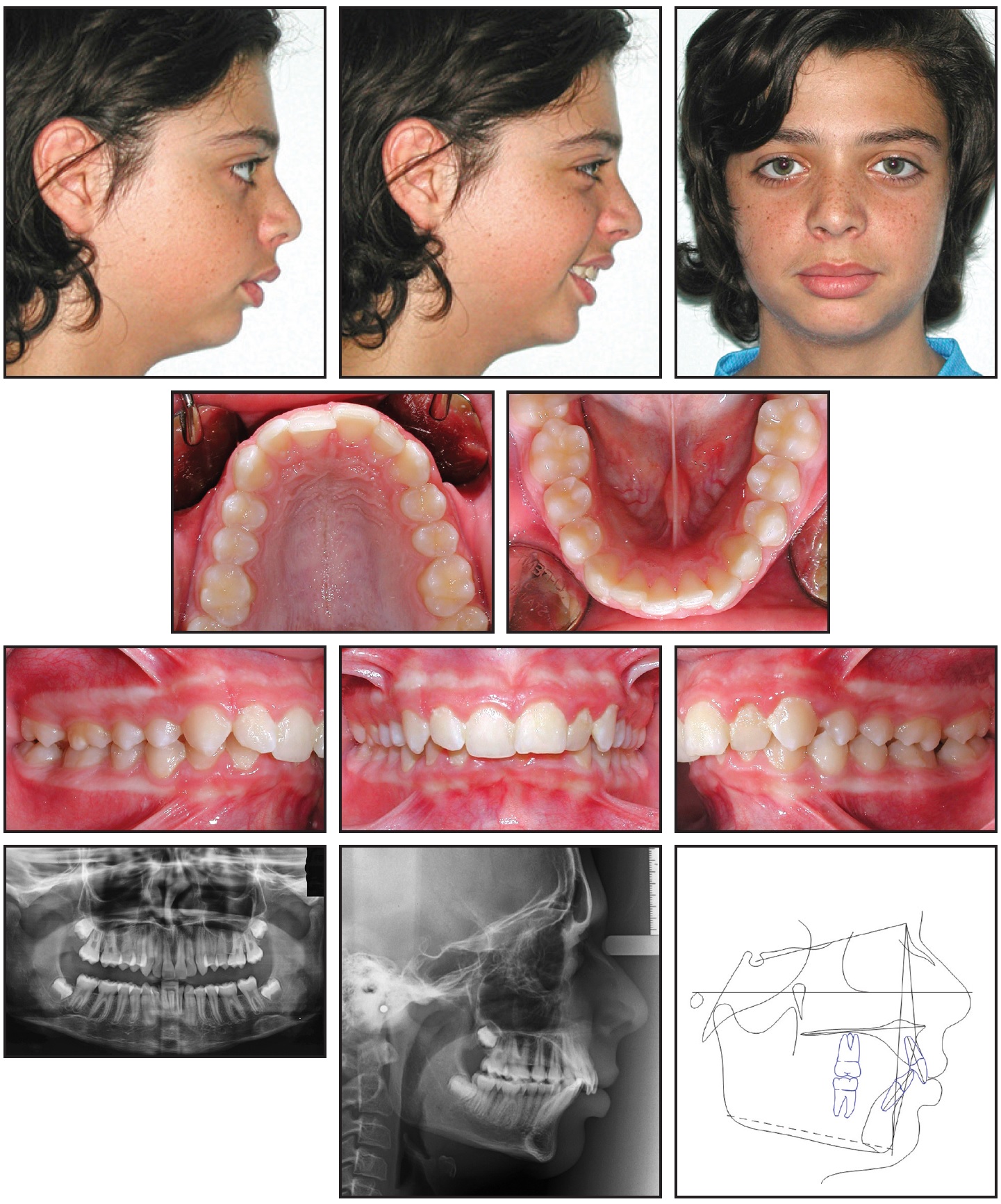
Fig. 1 13-year-old male patient with skeletal and dental Class II malocclusion and retrusive mandible before treatment.
He had skeletal and dental Class II relationships, with a retrusive mandible, a convex profile, and severely buccally inclined lower incisors (Table 1). Mild crowding was evident in the lower arch, and the dental midline was deviated to the right.
The patient exhibited poor plaque control and reported previous unsuccessful treatment with a removable plate that he did not wear. The lateral cephalogram indicated that his skeletal maturation was between cervical stages 3 and 4.
Four treatment options were evaluated. The first called for extraction of the upper first premolars, and the second involved the use of headgear. Both of these approaches were rejected because of the need to enhance mandibular growth without affecting the maxillary anterior limit of the dentition. Waiting until the end of growth to plan surgical-orthodontic treatment was unacceptable to the patient and parents. A fourth option was to stimulate mandibular growth by means of orthopedic treatment, thus improving the profile while correcting the dental Class II malocclusion. This option was considered feasible because of the patient’s remaining growth.
Given this patient’s lack of compliance with the previous therapy, a MiniScope Herbst was chosen as the functional appliance. To maximize the skeletal effects and minimize the typical dental side effects—buccal inclination of the lower incisors and palatal inclination of the upper incisors—the appliance would be anchored by modified Bollard** miniplates with laser-soldered nuts.
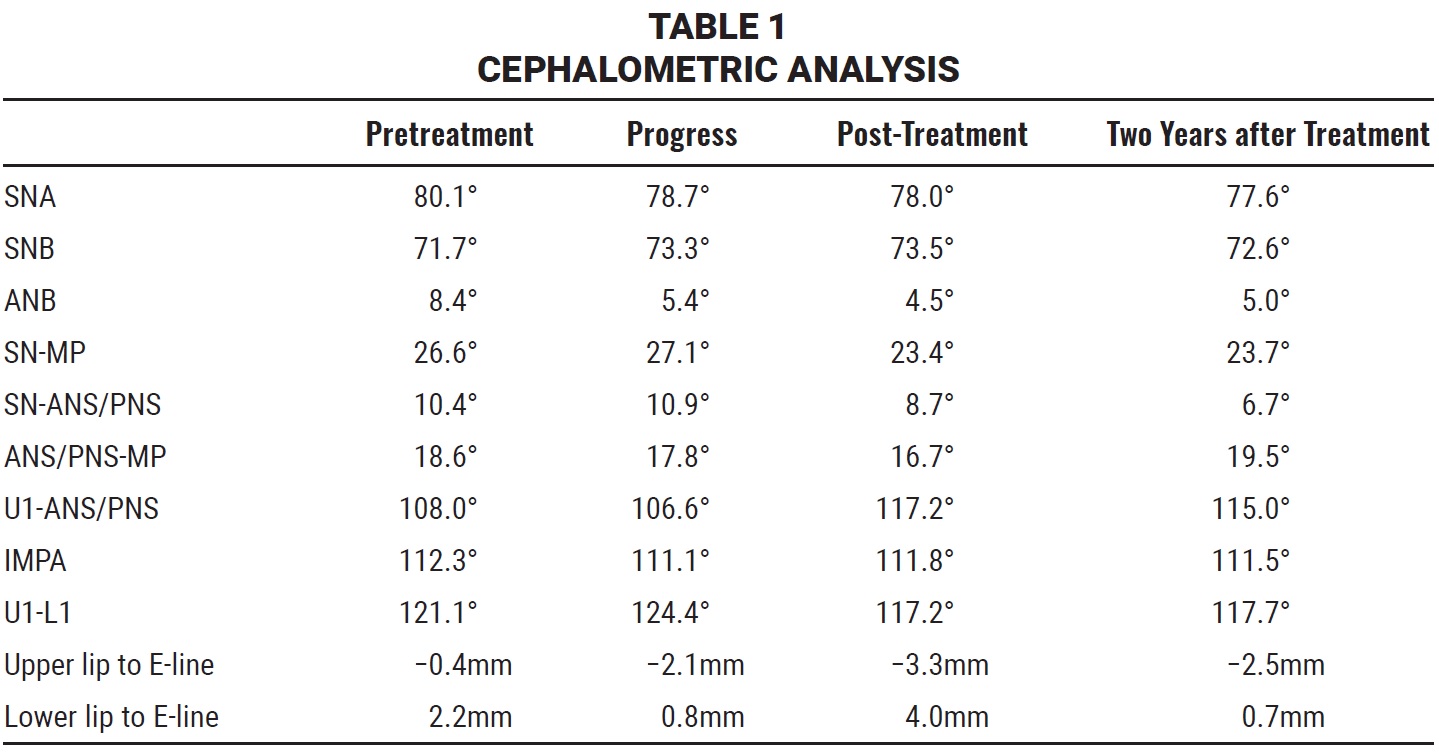
A minimally invasive flap was raised under local anesthesia, and the miniplate anchorage system was placed as described in previous reports.10 In the upper arch, the Bollard miniplates were inserted in the right and left infrazygomatic crests; in the mandible, they were placed between the canines and first premolars (Fig. 2).
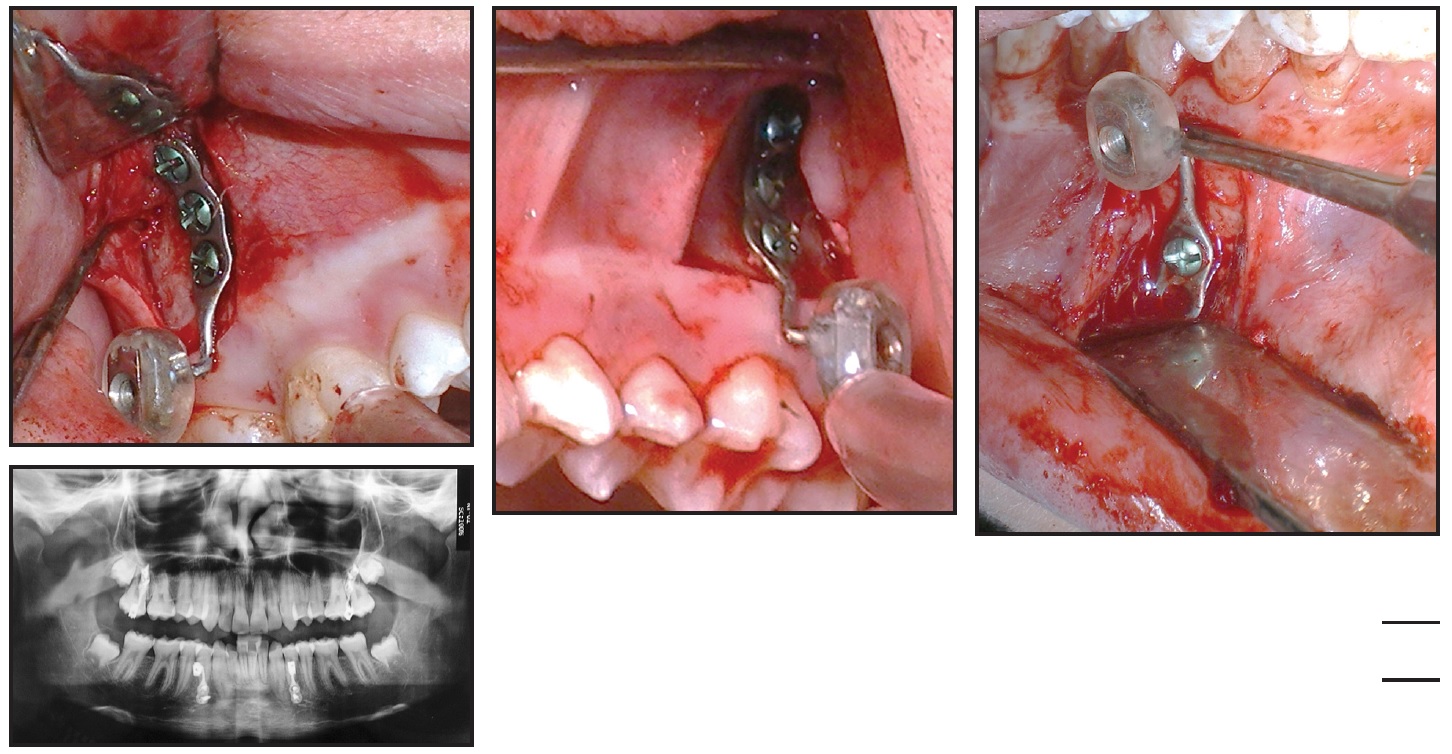
Fig. 2 Surgical placement of Bollard** miniplates.
Two weeks later, the Herbst arms were attached to the laser-soldered nuts of the miniplates (Fig. 3).

Fig. 3 A. Before attachment of MiniScope Herbst* arms. B. After Herbst placement.
The appliance did not cause any ulceration during treatment. The left MiniScope was removed after seven months to help resolve the dental midline discrepancy. The right MiniScope was removed three months later, when the profile had improved and a dental Class I relationship had been achieved (Fig. 4). The lower incisor inclination was unchanged.
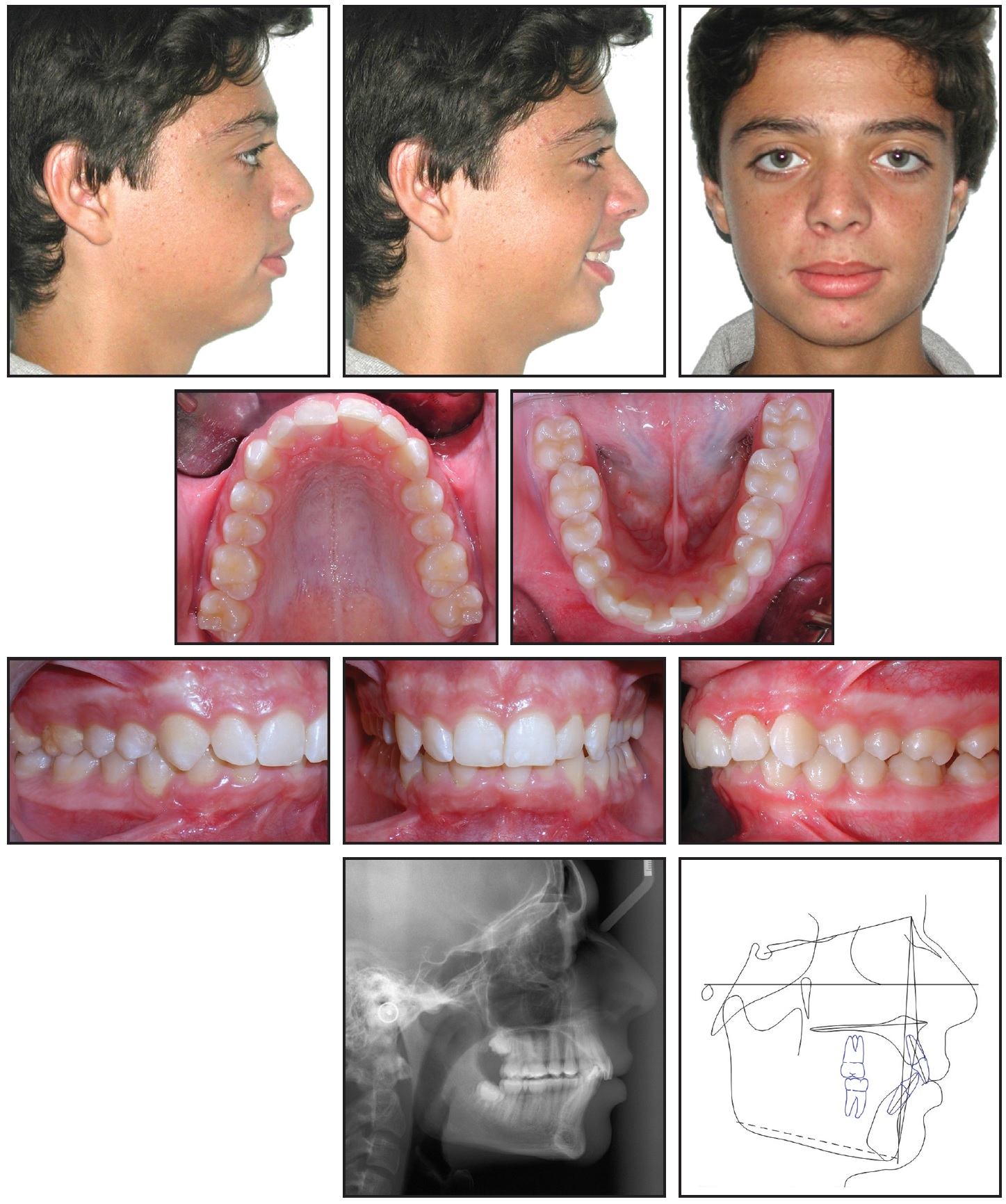
Fig. 4 After 10 months of orthopedic treatment (seven months on left side).
Upper and lower multibracket appliance therapy was then initiated, using .022" MBT*** appliances with archwires progressing from .016" nickel titanium to .019" × .025" stainless steel. Nineteen months later, the overbite had been corrected and the Class I relationship had fully settled (Fig. 5). A lower 3-3 .0195" stainless steel twisted lingual wire was bonded for retention, and an upper Hawley retainer was delivered.
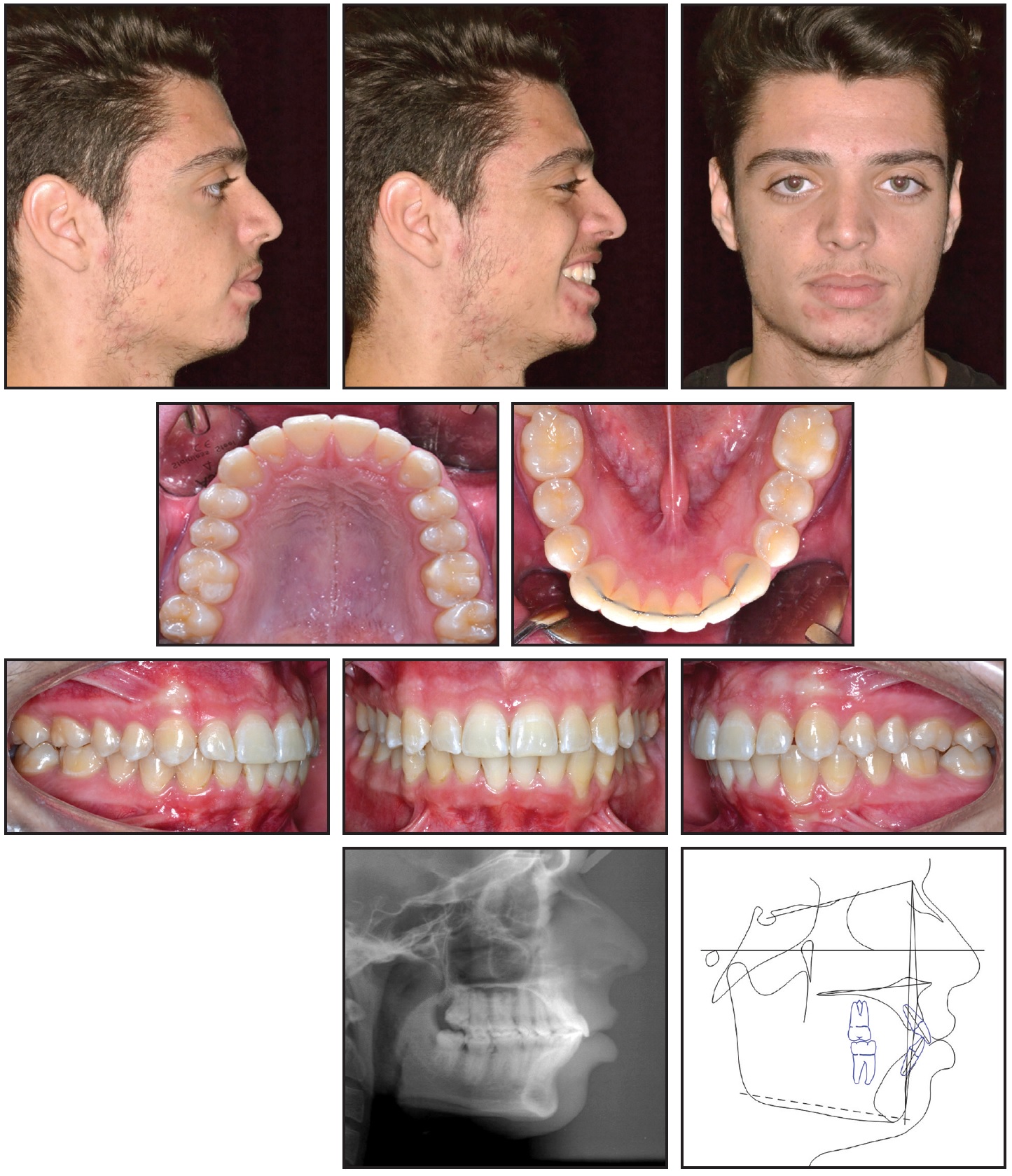
Fig. 5 Patient after 29 months of treatment.
Total treatment time was 29 months. Cephalometric analysis indicated a stable skeletal intermaxillary relationship and an improved profile, with adequate control of the lower incisor positions.
Two years later, the facial and occlusal relationships remained stable (Fig. 6).
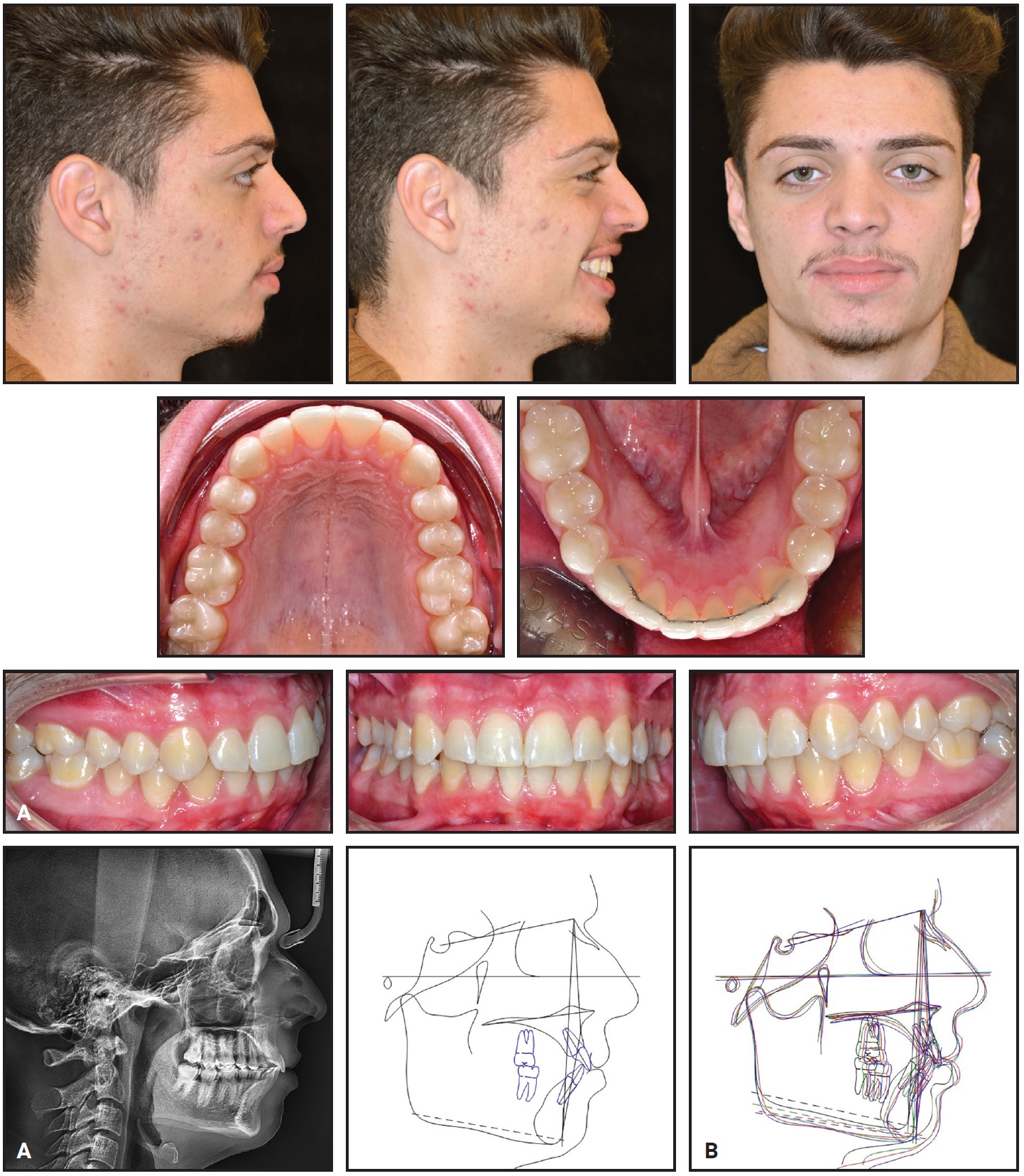
Fig. 6 A. Patient two years after treatment. B. Superimposition of pretreatment, post-orthopedic, post-treatment, and two-year follow-up cephalometric tracings.
Discussion
The Herbst appliance has been shown to be the most efficient orthopedic device for treatment of a Class II malocclusion with mandibular deficiency.9 Anchorage loss is an issue with any fixed bite-jumping appliance, however, with the common side effects of lower incisor proclination and upper incisor retroclination. Any subsequent dental compensation of the overjet will inhibit mandibular advancement and thus reduce the potential for skeletal correction of the mandibular retrognathia.
Various approaches have been proposed to avoid this effect, including premolar anchorage, premolar-molar anchorage, Pelott anchorage, labiolingual anchorage, splint-type anchorage, and acrylic devices with occlusal coverage.7,11 Still, Weschler and Pancherz maintained that “mandibular anchorage loss in Herbst treatment is a reality with which the orthodontist has to live.”7
More recently, the miniscrew-anchored Herbst was introduced to take advantage of indirect skeletal anchorage.12,13 Bremen and colleagues demonstrated, however, that interradicular miniscrews could not prevent anchorage loss during Herbst treatment; consequently, the potential amount of incisor proclination and protrusion remained unpredictable.14 To preclude anchorage loss while avoiding the risk of miniscrew failure under an orthopedic load, we chose a direct anchorage system using miniplates. Al-Dumaini and colleagues have documented the success of a miniplate-anchored Class II protocol with elastics in producing maximum skeletal results with minimal dentoalveolar effects.15 Moreover, a miniplate-anchored Forsus device has been found effective in treatment of mandibular deficiency.16
In the case presented here, orthopedic treatment with the miniplate-anchored MiniScope Herbst appliance corrected a skeletal Class II malocclusion while improving the profile and soft-
tissue adaptation, without causing any buccal inclination of the mandibular incisors due to sagittal anchorage loss.
FOOTNOTES
- *Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- **Registered trademark of Tita-Link, Brussels, Belgium; www.tita-link.com.
- ***Trademark of 3M, Monrovia, CA; www.3M.com.
REFERENCES
- 1. McNamara, J.A. Jr.: Components of class II malocclusion in children 8-10 years of age, Angle Orthod. 51:177-202, 1981.
- 2. Pancherz, H.; Zieber, K.; and Hoyer, B.: Cephalometric characteristics of Class II division 1 and Class II division 2 malocclusions: A comparative study in children, Angle Orthod. 67:111-120, 1997.
- 3. Pancherz, H.: Treatment of class II malocclusions by jumping the bite with the Herbst appliance: A cephalometric investigation, Am. J. Orthod. 76:423-442, 1979.
- 4. Pancherz, H.: The effects, limitations, and long-term dentofacial adaptations to treatment with the Herbst appliance, Semin. Orthod. 3:232-243, 1997.
- 5. Meyer-Marcotty, P.; Kochel, J.; Richter, U.; and Richter, F.: Reaction of facial soft tissues to treatment with a Herbst appliance, J. Orofac. Orthop. 73:116-125, 2012.
- 6. Pancherz, H.; Bjerklin, K.; and Hashemi, K.: Late adult skeletofacial growth after adolescent Herbst therapy: A 32-year longitudinal follow-up study, Am. J. Orthod. 147:19-28, 2015.
- 7. Weschler, D. and Pancherz, H.: Efficiency of three mandibular anchorage forms in Herbst treatment: A cephalometric investigation, Angle Orthod. 75:23-27, 2005.
- 8. Wehrbein, H. and Göllner, P.: Skeletal anchorage in orthodontics: Basics and clinical application, J. Orofac. Orthop. 68:443-461, 2007.
- 9. Cozza, P.; Baccetti, T.; Franchi, L.; De Toffol, L.; and McNamara, J.A. Jr.: Mandibular changes produced by functional appliances in Class II malocclusion: A systematic review, Am. J. Orthod. 129:599.e1-12, 2006.
- 10. Cornelis, M.A.; Scheffler, N.R.; Mahy, P.; Siciliano, S.; De Clerck, H.J.; and Tulloch, J.F.: Modified miniplates for temporary skeletal anchorage in orthodontics: Placement and removal surgeries, J. Oral Maxillofac. Surg. 66:1439-1445, 2008.
- 11. Pancherz, H. and Hansen, K.: Mandibular anchorage in Herbst treatment, Eur. J. Orthod. 10:149-164, 1988.
- 12. Luzi, C.; Luzi, V.; Carletti, P.; and Melsen, B.: The miniscrew Herbst, J. Clin. Orthod. 46:399-405, 2012.
- 13. Manni, A.; Mutinelli, S.; Pasini, M.; Mazzotta, L.; and Cozzani, M.: Herbst appliance anchored to miniscrews with 2 types of ligation: Effectiveness in skeletal Class II treatment, Am. J. Orthod. 149:871-880, 2016.
- 14. Bremen, J.V.; Ludwig, B.; and Ruf, S.: Anchorage loss due to Herbst mechanics: Preventable through miniscrews? Eur. J. Orthod. 37:462-466, 2015.
- 15. Al-Dumaini, A.A.; Halboub, E.; Alhammadi, M.S.; Ishaq, R.A.R.; and Youssef, M.: A novel approach for treatment of skeletal Class II malocclusion: Miniplates-based skeletal anchorage, Am. J. Orthod. 153:239-247, 2018.
- 16. Patil, H.A.; Kerudi, V.V.; Rudagi, B.M.; Sharan, J.S.; and Tekale, P.D.: Severe skeletal Class II Division 1 malocclusion in postpubertal girl treated using Forsus with miniplate anchorage, J. Orthod. Sci. 6:147-151, 2017.






COMMENTS
.