ORTHODONTICS IN THE COVID-19
The Way Forward Part 2: Orthodontic Treatment Considerations
The material contained in this communication is subject to change based upon federal, state, and local regulations; guidance from agencies; and additional knowledge that will come to light throughout the COVID-19 crisis. This information was organized to provide assistance and not specific direction; further due diligence is still required. Decisions for any specific orthodontic practice should be based on your own considerations and requirements, after consulting with professional advisers who are involved in all aspects of your practice.
Part 1 in this pair of articles provided background on the current coronavirus pandemic and suggestions for implementing new office environmental and infection controls. (Part 1 has been published only at www.jco-online.com.) This second part will discuss orthodontic treatment considerations in the COVID-19 era.
We must anticipate and be prepared for the effects of unsupervised orthodontic treatment in case a future lockdown is imposed in the wake of a COVID-19 resurgence. Therefore, we should reconsider the use of any orthodontic mechanism that, if left unattended, could create unintended detrimental effects—especially devices that are not self-limiting, such as Pendulum* springs, canine traction or eruption springs (Kilroy,** ballista), reverse-curve wires, torquing auxiliaries, and fixed functional appliances (Forsus,*** Herbst†). The following are some specific orthodontic procedures and appliances that may have to be modified, at least in the short term.
Similar articles from the archive:
- OVERVIEW Sterilization and Instrument Compatibility in a Digital World September 2012
- Optimizing Orthodontic Sterilization Techniques August 1997
- Efficient and Effective Infection Control January 1992
Bonding
The need to polish the enamel surface with pumice and the constant use of a three-way syringe for rinsing make conventional bonding an aerosol-generating procedure (AGP). Many non-AGP options for bonding are available (although it must be emphasized that these can compromise bond strengths58,59):
- Light-cured resin-modified glass ionomer cement can be used without any prior enamel preparation such as polishing, etching, or drying. This option reduces the need for an absolutely dry field, in turn reducing the need for any AGP.60
- Self-etch primers can also be used without prior enamel preparation and etching, but they require the smear layer to be removed prior to use, usually by pumicing or polishing teeth, which would be unnecessary with an AGP.
- The need for a three-way syringe before or after polishing and etching can be avoided by using a dry cotton roll to clean the enamel surface. Suction can still be used because it is non-AGP. Paul Gange Jr. of Reliance Orthodontic Products has shared similar interim recommendations for non-aerosol bonding.61
Indirect bonding may be another alternative to conventional direct-bonding techniques because it reduces patient exposure. It should be kept in mind that flash removal for indirect bonding is an AGP and must be performed with utmost caution.62
Leveling and Alignment
Leveling and alignment are complex processes during which all teeth move in different directions at the same time. As the teeth level and align, reciprocal forces develop between them and help guide the teeth to the correct positions. Practitioners usually start with light forces and round, light-gauge nickel titanium wires, which have a considerable amount of play that can cause slippage of the wire from brackets, especially on the terminal molars. Square or rectangular nickel titanium wires are preferable to avoid emergencies caused by slippage. Additionally, the archwires can be cinched back to prevent the sharp ends from impinging on the gums. The use of flowable composite is also recommended. To avoid slippage, it is wise not to include the second molars during the first few visits; they can be incorporated during the stages employing flexible rectangular wires.
Deep Bites
It is a common practice to use a reverse-curve nickel titanium wire to correct a deep bite caused by a deep curve of Spee in the lower arch. It usually takes about three months to flatten the curve with a constant force of approximately 300g generated by the wire itself. Note that such high forces from non-self-limiting mechanisms, if left unmitigated or not regularly attended, may yield untoward iatrogenic effects such as excessive bite opening or proclination of the lower incisors (Fig. 16).63
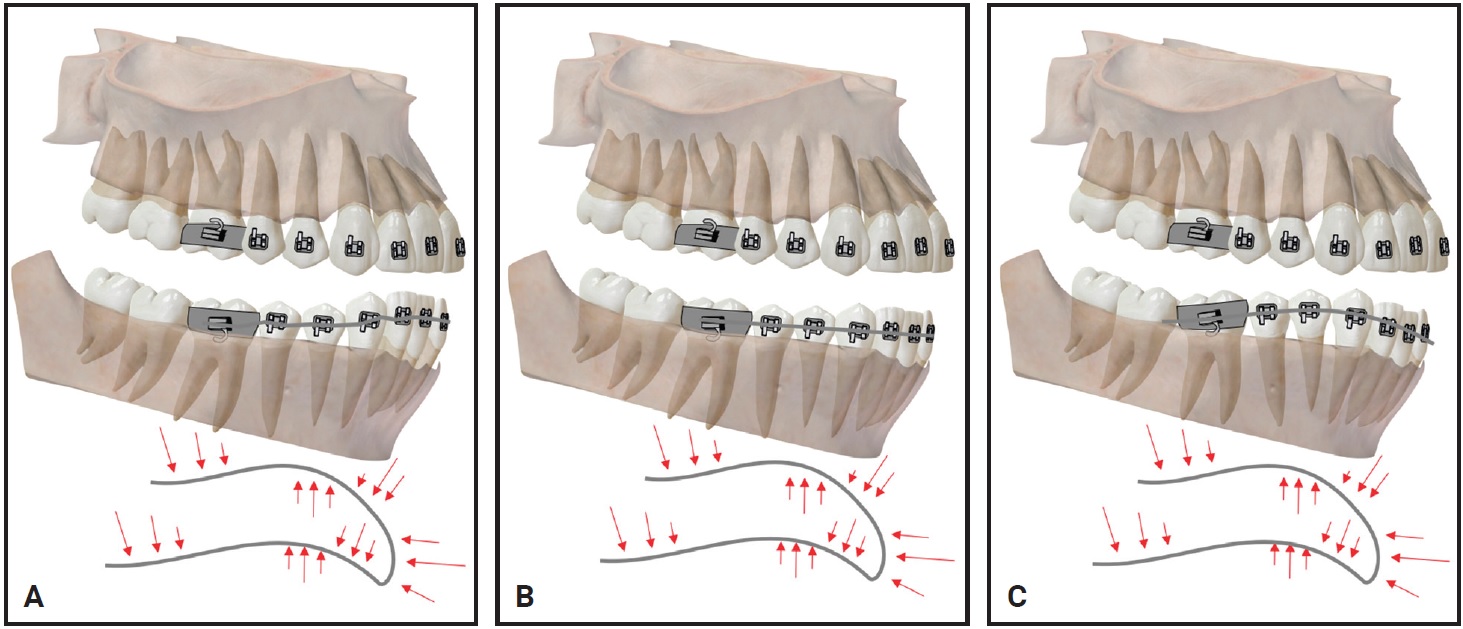
Fig. 16 A. Intended effect of reverse curve of Spee archwire. B. Reverse-curve archwire after reaching its objective. C. Inadvertent tooth movement produced by unmonitored reverse-curve archwire.
Space Opening
It is also common to use open-coil springs to create space during alignment and derotation. These should be prescribed with caution and require constant monitoring. Measure the exact amount of space needed and calibrate the coil length to avoid excessive space opening, root convergence, or proclination of anterior teeth in case of missed appointments (Fig. 17). Fail-safe alternatives such as opening loops on rectangular stainless steel wires can be adapted to create space as the forces diminish or dissipate, once the measured activation is reached.
Interproximal reduction should be delayed because it requires close monitoring and absolute control to utilize the space for its desired intent. Long delays in appointments may lead to a loss of anchorage and subsequent loss of space gained.
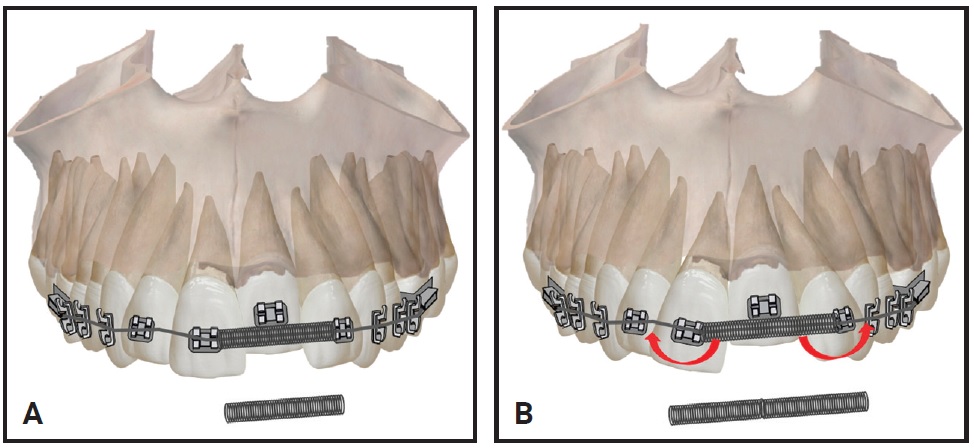
Fig. 17 A. Passive open-coil spring after reaching its objective. B. Inadvertent tooth movement caused by activation of open-coil spring beyond its objective.
Ligation and Bite Blocks
Archwires should be tied to the brackets with stainless steel ligatures instead of elastomeric rings, since the metal ligatures are more hygienic and offer more robust ligation. Passive self-ligating brackets offer advantages in delayed appointment situations, including fewer emergencies associated with torn or loose elastomeric rings or oral hygiene concerns caused by food and plaque accumulation around elastomeric rings.64 The first few appointments for patients during the leveling and alignment phase can therefore be scheduled about 10 weeks apart to reduce patient exposure and risks.
The use of anterior and posterior bite blocks to avoid premature contact of brackets during the initial stages must be carefully monitored. Such bite raisers are generally used for one to two months, until the teeth are marginally aligned and there is no premature contact that could lead to bracket “pop-outs.” If a patient fails to return for an appointment, however, there is a chance that the occlusal plane could be altered by reciprocal extrusion of the non-contacting teeth or intrusion of the contacting teeth (Fig. 18).
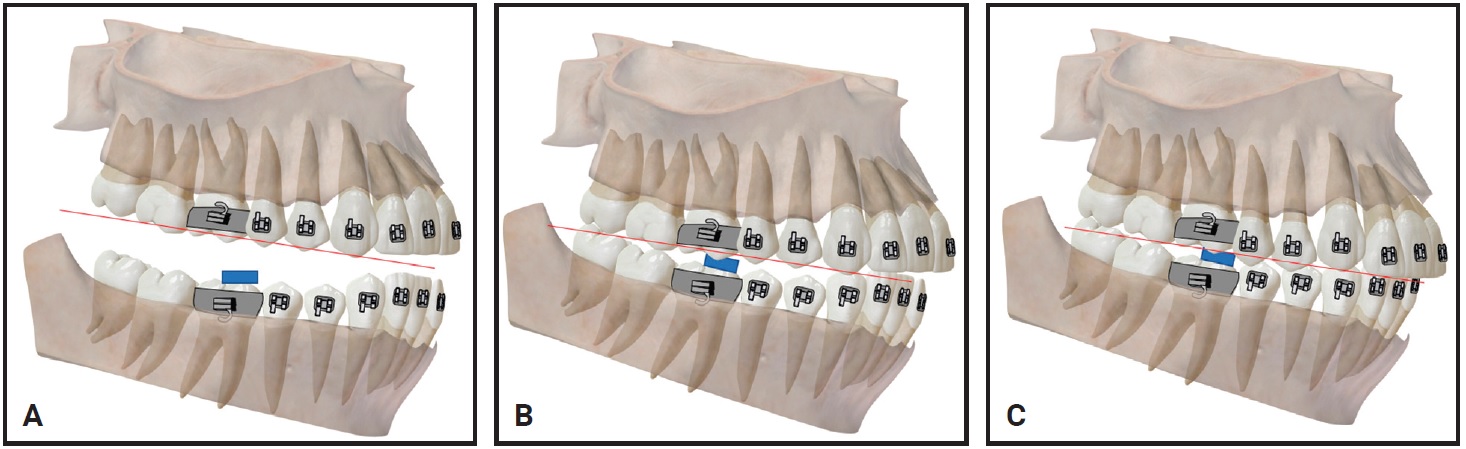
Fig. 18 A. Typical placement of posterior bite block. B. Bite block in occlusion. C. Inadvertent tooth movement caused by unmonitored bite block.
Extractions and Expansion
Orthodontic extractions may be carried out with standard precautions, but they should be planned for a single visit to reduce patient exposure. Meticulous planning for orthodontic anchorage is essential prior to extractions. Be aware that if there is a COVID-19 return and a lockdown is reimposed, further measures may be required to avoid undesirable anchorage loss.
Expansion treatment is still possible, but only with close monitoring after the practice reopens. Patients must be clearly instructed regarding the objectives of expansion. Once rapid palatal expansion is complete, it is essential to retain the achieved results by recalling the patient as soon as possible in case of a future lockdown. Overactivation can cause undesirable buccal tipping of posterior teeth, potentially necessitating “round-
tripping” and creating delays in finishing (Fig. 19).
Alternative methods of slow expansion are preferable during this period because they are more fail-safe and do not create abrupt changes over short intervals, thus reducing the chance of emergencies.
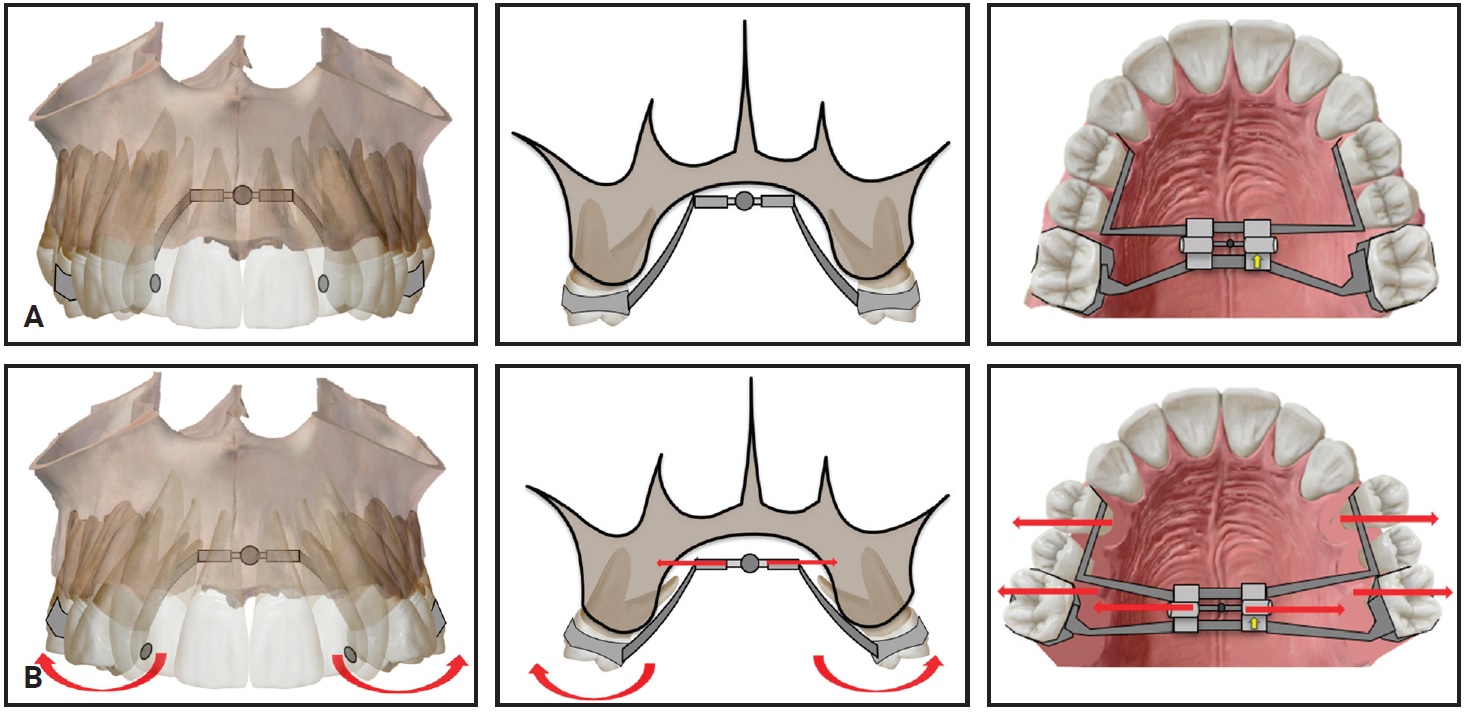
Fig. 19 A. Rapid palatal expander after achieving its objectives. B. Inadvertent tooth movement caused by overactivation of expander.
Space Closure
Space closure is generally considered the most crucial phase of orthodontic treatment. The magnitude of space closure is determined by the preexisting malocclusion, space requirements, extraction decisions, anchorage demands, types of tooth movement, and forces used. While closed-coil springs are commonly used to exert continuous forces during space closure, this raises the concern of overclosure or unnecessary tipping by the continuous forces if the patient does not report for a long time. In case of an unforeseen future lockdown, it is wiser to employ power chain or elastic thread for space closure, since their forces decay over a shorter period. It is of paramount importance to measure the applied forces with a Dontrix‡ or Correx†† gauge to ensure they are not excessive (Fig. 20).
Space closure can be accomplished by either friction or frictionless mechanics. Sliding or archwire-guided mechanics are preferable over frictionless mechanics for the popular preadjusted edgewise appliance systems, considering that segmental or loop mechanics produce higher differential moments and require timely monitoring and greater dexterity in placement. When not monitored closely, frictionless mechanics can produce such deleterious effects as excessive tipping, unwanted intrusion or extrusion, and occlusal canting. These effects would then require round-tripping and make the dentition more prone to root resorption. Because auxiliary wires and cantilevers can cause soft-tissue impingement if dislodged, it is best to avoid them for a few months.
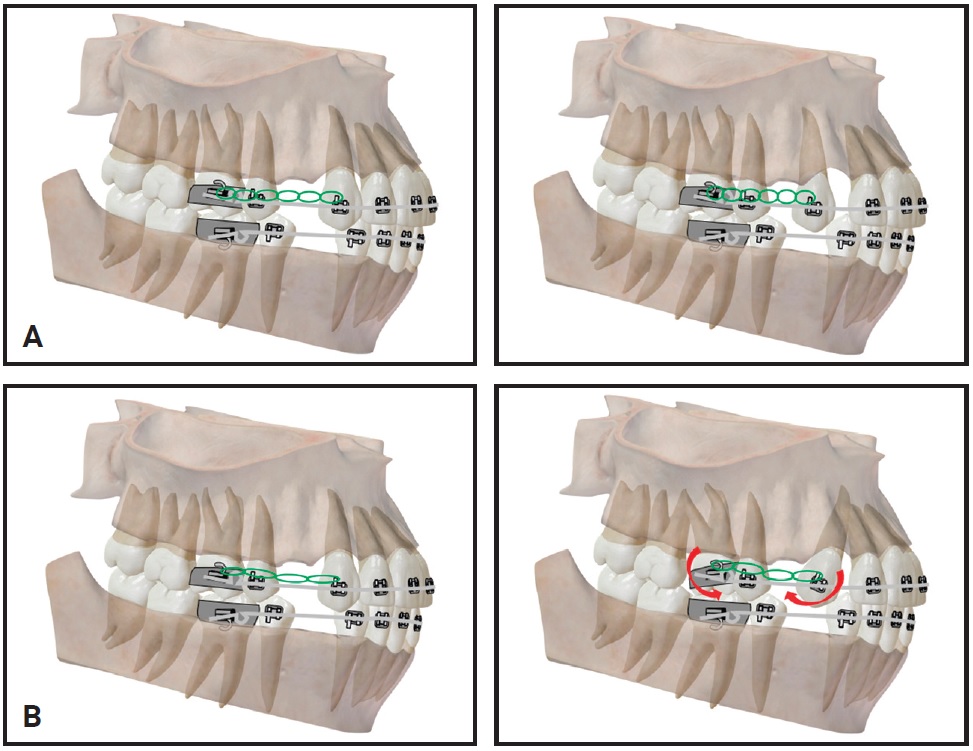
Fig. 20 A. Appropriate activation forces allow elastomeric chains to maintain retraction progress during force decay. B. Inadvertent tooth movement caused by improperly monitored elastomeric chains.
Tiebacks may be a useful method in cases with freshly extracted premolars where the intent is to alleviate anterior crowding.65 The tieback is a stainless steel ligature wire that is threaded through an elastomeric module and goes directly from the terminal molar to the canine bracket (Fig. 21). Although the initial force used to place tiebacks varies among clinicians,66 the force decay is almost 100% in 48 hours, with 63% of the decay occurring within the first 24 hours. The “trampoline effect” hypothesis speculates that intermittent movement or pumping action on the ligature wire during function and chewing will continue to stretch out the auxiliary, giving it a “pseudo-activation.” Therefore, if the patient misses appointments, space closure can continue with active tiebacks.
The use of intermaxillary elastics for space closure might well be avoided at this time, because they require continuous monitoring and can cause adverse effects in terms of tipping and bite deepening, leading to unexpected gummy smiles in Class II cases (Fig. 22).
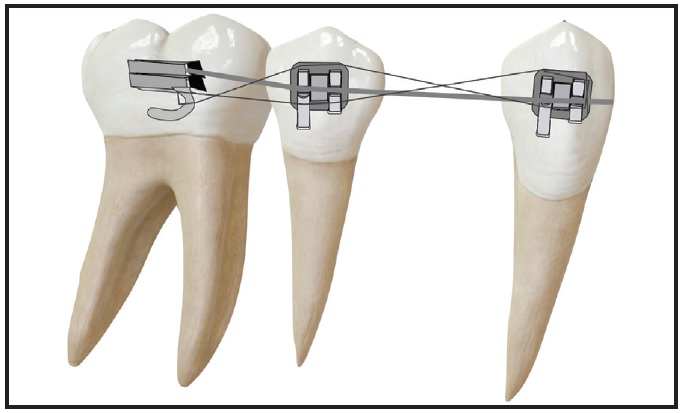
Fig. 21 Tiebacks in position.
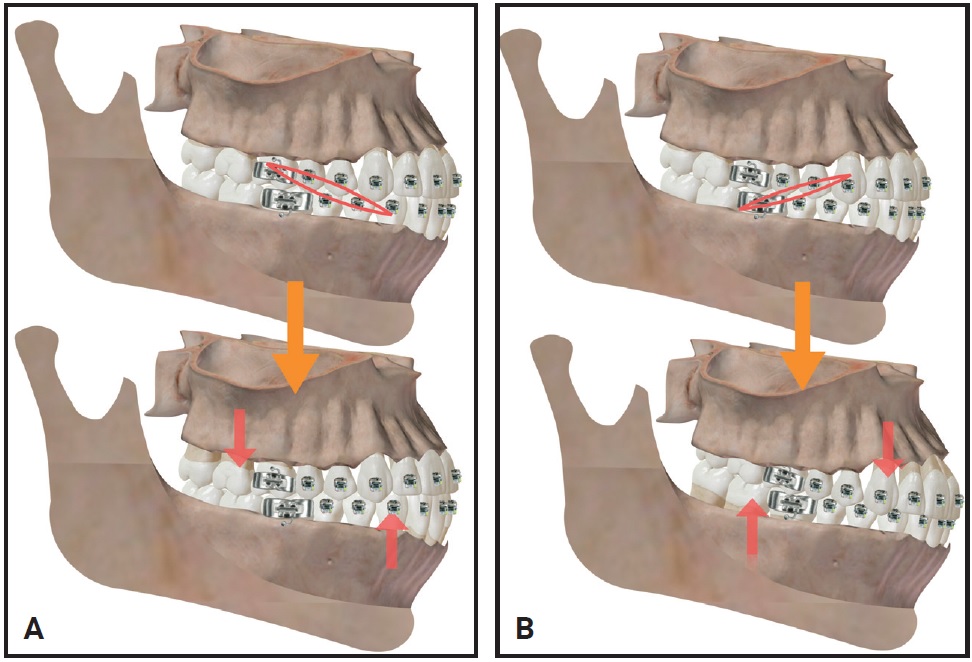
Fig. 22 Adverse effects of intermaxillary elastics. A. Tipping. B. Bite deepening.
Miniscrews
Miniscrews have become popular in retraction and intrusion mechanics. In the current environment, miniscrews should not be placed in patients with poor oral hygiene or existing periodontal problems, since the chances of failure are higher.67 In addition, strict measures must be employed to keep the tissue around miniscrews clean and thus reduce infection- or inflammation-related emergencies. Avoid using direct cantilever mechanics from the miniscrews, because they may become dislodged and cause irritation to the soft tissues (Fig. 23). Reverse-threaded or counterclockwise-activated screws can be used on the left side to prevent an unwinding effect after activation and thus avoid loosening from torsional forces.68
Finishing and Detailing
Finishing and detailing is the most challenging phase of orthodontic treatment. Good intercuspation is normally achieved by using artistic archwire bends or settling elastics. Settling elastics may be preferable at this time because they produce lighter forces than the couples generated by artistic bends on thick finishing archwires, and they are less prone to debond attachments (Fig. 24).
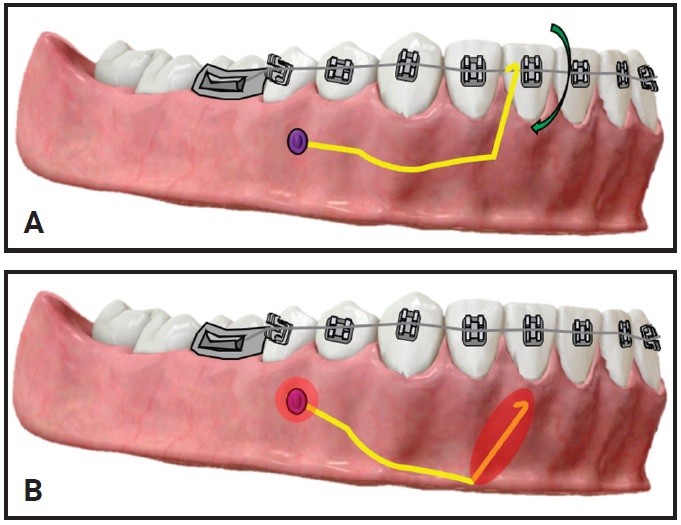
Fig. 23 A. Objective of cantilever mechanics with direct miniscrew anchorage. B. After dislodgement and subsequent soft-tissue irritation.
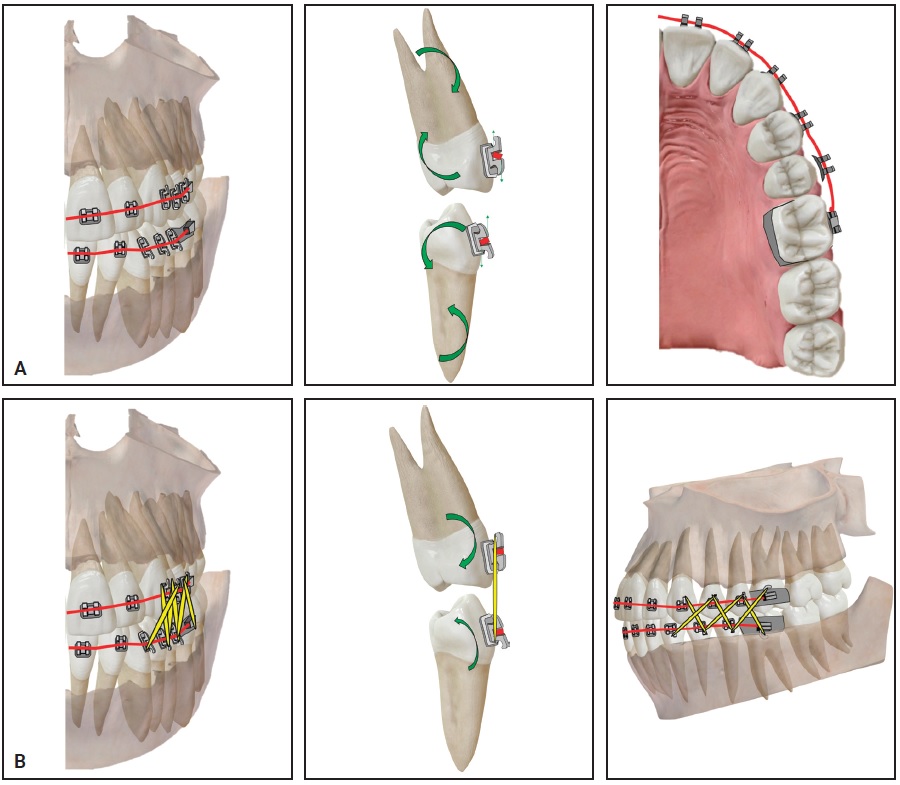
Fig. 24 A. During torquing mechanics, couples generated on finishing wire may create enough force to debond upper left second premolar bracket. B. Settling elastics may be preferable because they produce lighter forces and less risk of debonding attachments.
Any movements that generate higher moments, such as 3rd-order twists, should be postponed for a few months. Unmonitored overexpression of these tooth movements can predispose to root resorption, fenestration, or dehiscence.
Retention
Finishing and polishing should be performed with caution during the debonding appointment because they are AGP. An Essix‡‡ or other removable retainer is preferable over a bonded retainer to avoid unnecessary aerosol contamination. Removable retainers can be worn for three to six months, after which fixed retainers can be bonded if indicated. Providing patients with additional sets of removable retainers may be a good policy in case one is lost or damaged during a potential COVID-19 resurgence.
Functional Appliances
Patients using removable functional appliances can be monitored remotely through video conferencing, and appliance use can be tapered once the objectives are met. In case of a second COVID-19 outbreak before the start of Phase II treatment, the fixed appliances can be delayed and the retentive phase extended by placing an upper anterior inclined plane to retain the corrected incisor relationship.69
Fixed bite correctors are associated with high rates of breakage and more emergency visits compared with removable functional appliances.70 Facial asymmetry, midline deviation, bite deepening, and occlusal cant changes are some of the detrimental effects of unmonitored therapy.
Aligners
Clear plastic aligners may offer some advantages in the COVID-19 era. A series of aligners is commonly provided to the patient for a set period (usually six to 12 weeks) before the patient returns for evaluation and additional aligners. Some orthodontists deliver all the aligners up front, saving storage space in the practice and reducing the number of in-office visits, and they may follow treatment progress online or with a remote monitoring system.
In the infrequent instance of loss or breakage of an aligner, the patient is usually advised to wear the previous aligner71 or, if unavailable, the next one in the series. If no aligner is available, a replacement “stage retainer” might be ordered from the manufacturer without a new digital scan. Fractured attachments can be replaced using one of the protocols described earlier to reduce aerosol generation during bonding.61
Virtual Tools
Given the unprecedented current situation, in which patient access to practices has been interrupted, virtual tools for dentistry72 and orthodontics have gained increasing popularity. Patients can use an array of available applications to take intraoral “selfies” with smartphones. These photos are automatically sorted, angulated, cropped, and organized by date. The orthodontist can access patient details at any time from any device through a common portal. Virtual prescreening or triage, as well as more immediate solutions to assess and monitor treatment and communicate with our patients, have been made possible by such digital tools.
A New Start
There is a good possibility that a future assault of COVID-19 would be even more difficult than the one we just went through. Hence, there is a need to develop clinical measures and guidelines for use in orthodontic practices during pandemics. As with any information in this continually evolving situation, it is most important that you do your own due diligence and carefully evaluate everything for yourself. We hope the measures and guidelines offered in this two-part series will stimulate thought and provide a rationale for:
- The need for more extensive COVID-19 testing, as well as guidelines for the personal protective equipment required for specific procedures in orthodontic practices.
- Potential changes in office environmental and infection controls.
- Comprehensive protocols for virtual consultations and appointments that can assure adequate patient care.
- Knowledge of and skill with orthodontic mechanics, with the intent of anticipating potentially adverse effects and offering more convenient and fail-safe methods to avoid emergencies in the immediate future.
It is true that it takes only one bad apple to spoil the whole bunch: one asymptomatic virus-spreading vector such as an insistent “helicopter” parent, a service vendor, or even a negligent employee may slip through and ruin our day. It is important, therefore, to note that despite our implementation of the most meticulous techniques, equipment, and practices, some people may still fall ill. Actions that need to be taken in that eventuality should also be formulated at this time. Our intent has been simply to offer options that can reduce those odds in an orthodontic practice for the benefit of our families, teams, and patients.
COVID-19 is undeniably here to stay for a long time; as a result, it may forever change the way we practice orthodontics. While providing our treatment, we must heighten our compassion for patients and enhance our sense of camaraderie and professionalism with staff and colleagues. With these factors in mind, we can get through this successfully, together.
FOOTNOTES
- *Ormco Corporation, Orange, CA; www.ormco.com.
- **Trademark of American Orthodontics, Sheboygan, WI; www.americanortho.com.
- ***Trademark of 3M, Monrovia, CA; www.3M.com.
- †Registered trademark of Dentaurum, Inc., Newtown, PA; www.dentaurum.com.
- ‡DentSply Sirona, Charlotte, NC; www.dentsplysirona.com.
- ††Haag-Streit Diagnostics, Köniz, Switzerland; www.haag-streit.com.
- ‡‡Registered trademark of Denstply Sirona Orthodontics Inc., Sarasota, FL; www.essix.com.
REFERENCES
- 58. Ireland, A.J.; Knight, H.; and Sherriff, M.: An in vivo investigation into bond failure rates with a new self-etching primer system, Am. J. Orthod. 124:323-326, 2003.
- 59. Aljubouri, Y.D.; Millett, D.T.; and Gilmour, W.H.: Six and 12 months’ evaluation of a self-etching primer versus two-stage etch and prime for orthodontic bonding: A randomized clinical trial, Eur. J. Orthod. 26:565-571, 2004.
- 60. Ireland, A.J. and Sherriff, M.: The effect of pumicing on the in vivo use of a resin modified glass poly (alkenoate) cement and a conventional no-mix composite for bonding orthodontic brackets, J. Orthod. 29:217-220, 2002.
- 61. Gange, P.: Bonding in the COVID-19 Era, J. Clin. Orthod., www.jco-online.com/covid19-resources/bonding-in-the-covid-19-era, published online, April 2020, accessed May 11, 2020.
- 62. Dalessandri, D.; Dalessandri, M.; Bonetti, S.; Visconti, L.; and Paganelli, C.: Effectiveness of an indirect bonding technique in reducing plaque accumulation around braces, Angle Orthod. 82:313-318, 2012.
- 63. Rodriguez Yanez, E.E.: 1,001 Tips for Orthodontics and Its Secrets, Medtech, New Delhi, India, 2013.
- 64. Pellegrini, P.; Sauerwein, R.; Finlayson, T.; McLeod, J.; Covell, D.A. Jr.; Maier, T.; and Machida, C.A.: Plaque retention by self-ligating vs elastomeric orthodontic brackets: Quantitative comparison of oral bacteria and detection with adenosine triphosphate-driven bioluminescence, Am. J. Orthod. 135:426.e1-9, 2009.
- 65. McLaughlin, R.P.; Bennett, J.C.; and Trevisi, H.J.: Systemized Orthodontic Treatment Mechanics, Mosby, Edinburgh, 2001.
- 66. Mohammadi, A. and Mahmoodi, F.: Evaluation of force degradation pattern of elastomeric ligatures and elastomeric separators in active tieback state, J. Dent. Res. Dent. Clin. Dent. Prospects 9:254-260, 2015.
- 67. Hergel, C.A.; Acar, Y.B.; Ates, M.; and Kucukkeles, N.: In-vitro evaluation of the effects of insertion and sterilization procedures on the mechanical and surface characteristics of mini screws, Eur. Oral Res. 53:25-31, 2019.
- 68. Venugopal, A.; Muthuchamy, N.; Tejani, H.; Gopalan, A.I.; Lee, K.P.; Lee, H.J.; and Kyung, H.M.: Incorporation of silver nanoparticles on the surface of orthodontic microimplants to achieve antimicrobial properties, Kor. J. Orthod. 47:3-10, 2017.
- 69. Clark, W.J.: Twin Block Functional Therapy, 3rd ed., Jaypee Brothers Medical Publishers, New Delhi, India, 2014.
- 70. O’Brien, K.; Wright, J.; Conboy, F.; Sanjie, Y.; Mandall, N.; Chadwick, S.; Connolly, I.; Cook, P.; Birnie, D.; Hammond, M.; and Harradine, N.: Effectiveness of treatment for Class II malocclusion with the Herbst or twin-block appliances: A randomized, controlled trial, Am. J. Orthod. 124:128-137, 2003.
- 71. Tai, S.: Clear Aligner Technique, Quintessence Publishing Co. Inc., Hanover Park, IL, 2018.
- 72. Jampani, N.D.; Nutalapati, R.; Dontula, B.S.; and Boyapati, R.: Applications of teledentistry: A literature review and update, J. Int. Soc. Prev. Comm. Dent. 1:37-44, 2011.









COMMENTS
.