Pain-Free Orthodontic Treatment with the Dental Pain Eraser
Pain is among the most frequently mentioned negative effects of orthodontic treatment and one of the most common concerns for patients. Several studies cite pain as the main reason for avoiding or stopping orthodontic treatment.1,2 About 8% of all orthodontic patients discontinue treatment because of pain.3
Many procedures, including separator placement, archwire insertion and activation, elastic wear, application of orthopedic forces, and debonding, can produce pain. Patients generally describe the sensation as a feeling of pressure, tension, or tooth soreness. Removable appliances are more comfortable than fixed appliances but are still associated with periods of significant discomfort.
Methods of controlling pain include oral analgesics,4 chewing gum, plastic bite wafers,5 vibratory forces,6 laser therapy,7 and transcutaneous electrical nerve stimulation (TENS).8-12 Administration of oral analgesics prior to separator placement can significantly reduce pain levels,4 but the side effects associated with nonsteroidal anti-inflammatory drugs are an issue for some patients. Chewing gum, plastic wafers, or vibration may also reduce the discomfort associated with separator placement and orthodontic tooth movement,6 but all three require patient cooperation. Low-level laser therapy has been shown to reduce pain perception after separator placement,7 but additional research is needed and the cost of a laser device can be prohibitive.
Roth and Thrash found the nonpharmacological, noninvasive TENS technique to be effective in reducing periodontal pain after separator placement, although they utilized large external sponge-pad electrodes or internal probe electrodes with an Alpha-Stim Model 2000,* which at the time was relatively large and expensive.8 Portable and less expensive TENS devices have since been engineered, yet no subsequent studies have tested the effectiveness of TENS in relieving pain related to orthodontic treatment.
Similar articles from the archive:
The present study was designed to evaluate whether a new portable TENS device can control orthodontic pain in a timely manner, as well as to determine the duration of pain relief following TENS application, identify the optimal locations of intraoral TENS application, and assess the reaction of patients and orthodontists to the use of TENS therapy.
Materials and Methods
Sixty-five patients with moderate to severe crowding, ranging in age from 10 to 57 (mean age 21), were selected from three private orthodontic practices in Cranston and Newport, Rhode Island, and Vancouver, British Columbia. All subjects had undergone routine dental examination and were in good dental health. Subjects were excluded if they were pregnant; had a history of seizures, cardiac arrhythmia, or pacemaker treatment; or were taking any over-the-counter or prescription pain medication during the testing period.
The selected patients were all in the leveling and alignment phase (first six months) of orthodontic treatment. Patients who were experiencing immediate pain following orthodontic adjustment were also selected. Of the 65 subjects, 45 were randomly assigned to the active treatment group and 20 to the control group. After consent forms were signed, patients in both groups were informed that they would be evaluating a pain-reduction device that would deliver a mild electric current. They were told that the intensity of the stimulation could range from sub-sensory to a very slight tingling.
The portable TENS device used in this study, the Dental Pain Eraser,** was designed for one-button operation, with one output for a safe and stable range of stimulation (Fig. 1).

Fig. 1 A. Dental Pain Eraser** model used in study. B. Production model.
It generated a biphasic, symmetrical pulse with a net neutral charge and a maximum current of 10mA, in accordance with the amplitudes and waveforms tested in various other dental applications.9-11 Control patients received the same mechanical application of the device with no current.
The TENS device was applied in each patient immediately after orthodontic wire activation or adjustment. Each application was administered in a clinical setting by a dental provider who had been trained to use the probe endings of the device. The provider followed a prescribed flow chart (Fig. 2), using a digital or paper survey system for data entry.
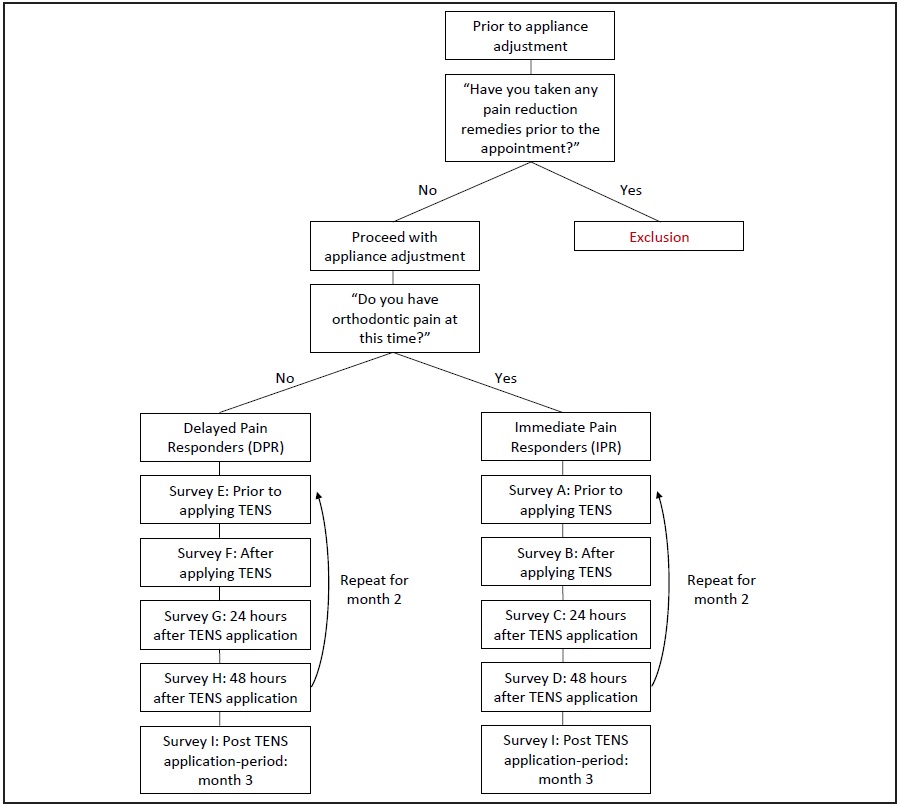
Fig. 2 Flow chart used by treatment providers.
After the stimulation, the provider recorded the time required to achieve comfort or when the subject no longer needed application. The patient was asked to rate the intensity of pain after TENS application and after 24 and 48 hours on a numeric rating scale (NRS), using whole numbers from 0 to 10 (Fig. 3).13,14
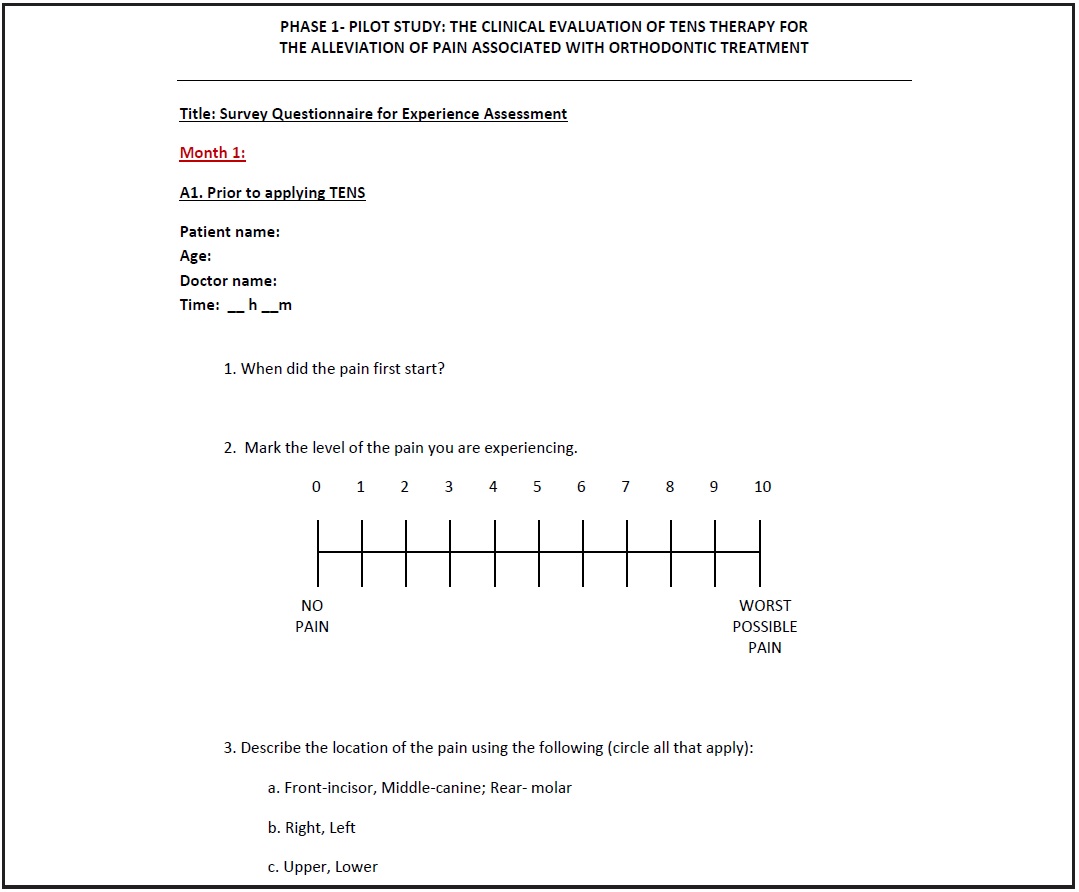
Fig. 3 Survey questionnaire for pain assessment, including numeric rating scale (NRS).
The pain location was then noted as being in the incisor, canine, or posterior region of a particular quadrant.
This study used a repeated-measures experimental design involving five factors:
1. Randomized treatment modality (TENS or placebo group).
2. Stimulation time required for pain relief.
3. Pain location (incisor, canine, or posterior).
4. Measurement period (0, 24, or 48 hours).
5. Practice location.
Results
NRS scores before and after TENS stimulation were analyzed using Wilcoxon’s signed-rank test and paired t-tests, with a significance level of p < .05 (Table 1). The consolidated scores indicated a significant reduction in pain after initial application of the Dental Pain Eraser (Mann-Whitney U test).
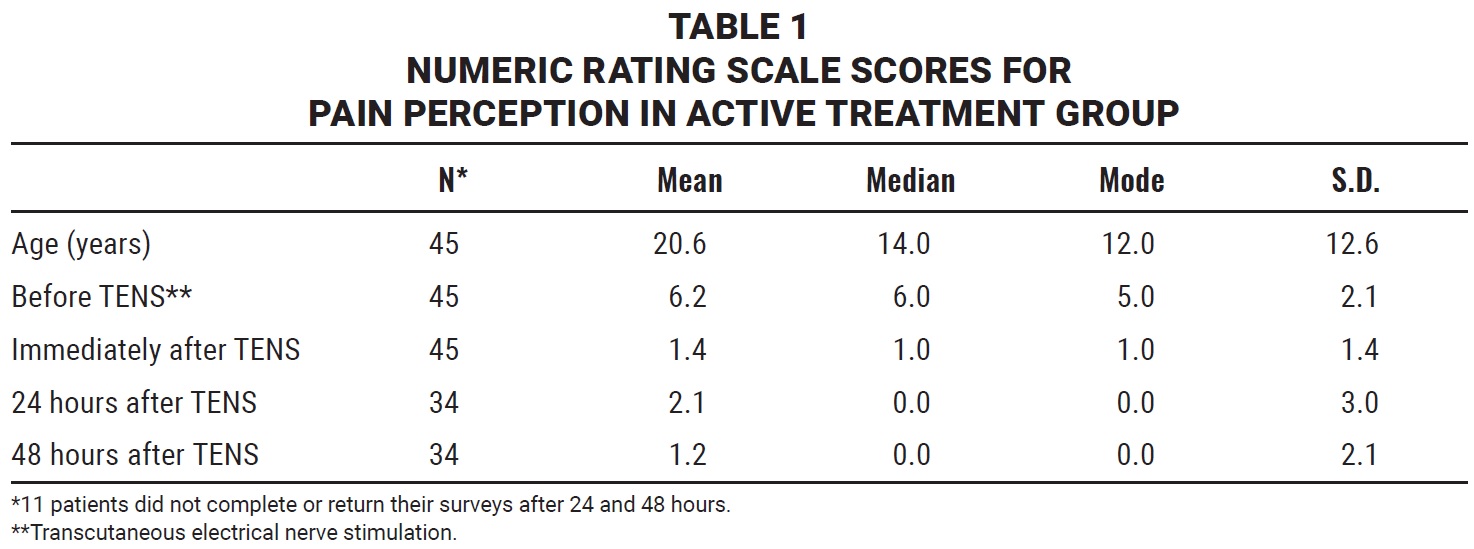
The mean patient age differed significantly among the three offices: 27 in Cranston, 13 in Newport, and 17 in Vancouver (Mann-Whitney U test, independent t-test). Although no significant difference was noted in overall NRS scores among the three offices, patients in the Cranston office reported higher levels of pain before stimulation compared with the other two locations (independent t-test). All three practices, independently and combined, reported significant pain reduction compared with pre-stimulation pain levels at 0, 24, and 48 hours (Kruskal-Wallis test). These results indicated that one TENS stimulation reduced discomfort immediately, and that the relief continued for as long as 48 hours.
Patients given the active TENS treatment reported significantly lower NRS scores (Mann-Whitney U test, independent t-test) compared with the control group (Fig. 4).
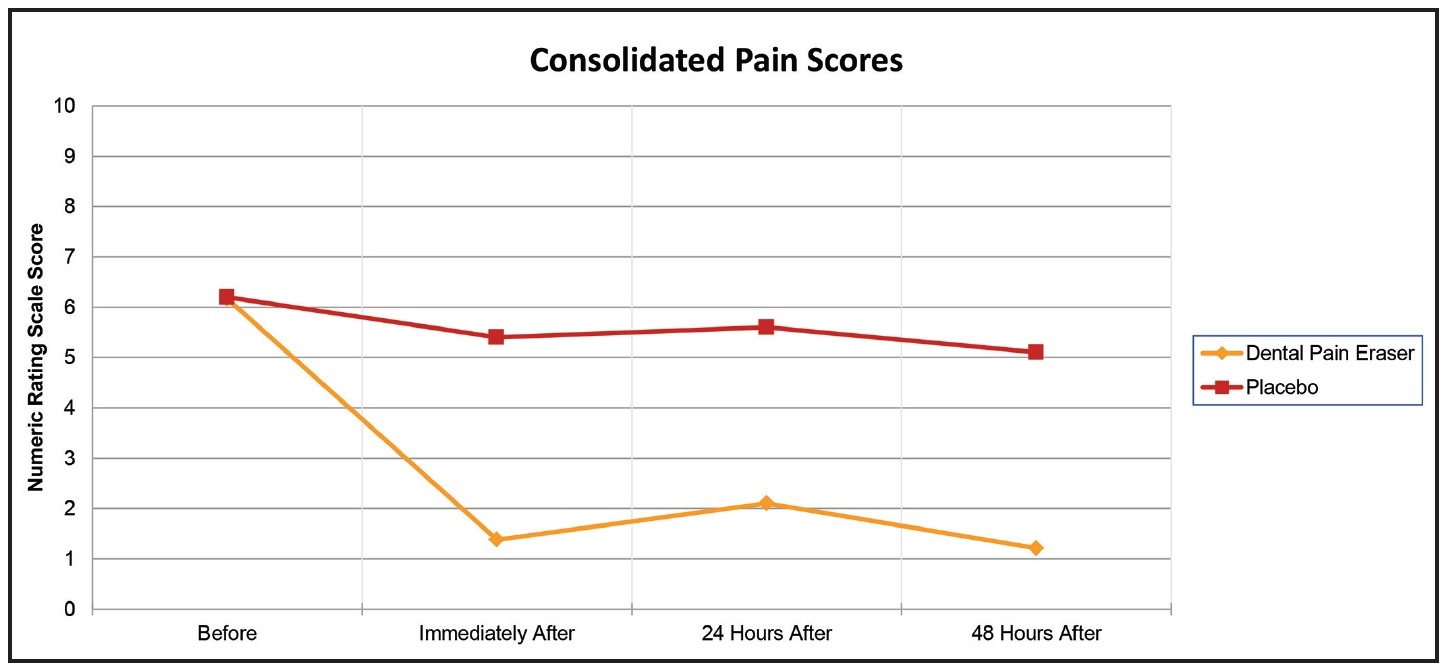
Fig. 4 Significantly lower mean NRS scores among active transcutaneous electrical nerve stimulation (TENS) treatment patients compared with controls at all post-application time points.
A slight but nonsignificant placebo effect was noted as an initial pain reduction in the control group, but there was no significant decline in pain in the control group after 24 or 48 hours.
Pain was diminished within one minute after application in 55% of the active TENS patients, and 29% experienced a reduction in one to two minutes (Fig. 5). Fully 96% of the patients said they received relief in an expected amount of time (less than a few minutes). Most subjects reported orthodontic pain in areas containing multiple teeth, primarily the incisor (49%) and canine (38%) regions, with roughly equal proportions in each quadrant (Fig. 6). If pain relief was reported over an entire area in less than one minute, it look less than 30 seconds for each individual tooth to experience significant pain reduction.
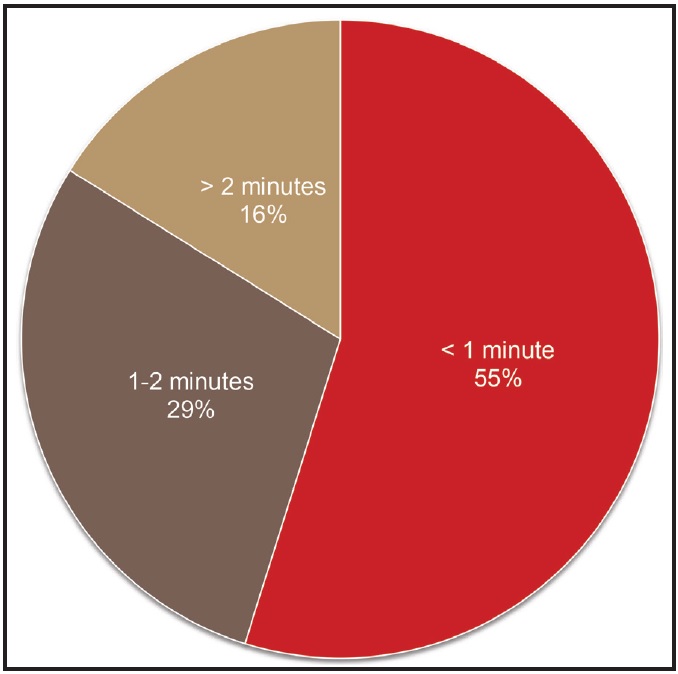
Fig. 5 Pain reduced in less than two minutes in 84% of active TENS patients.
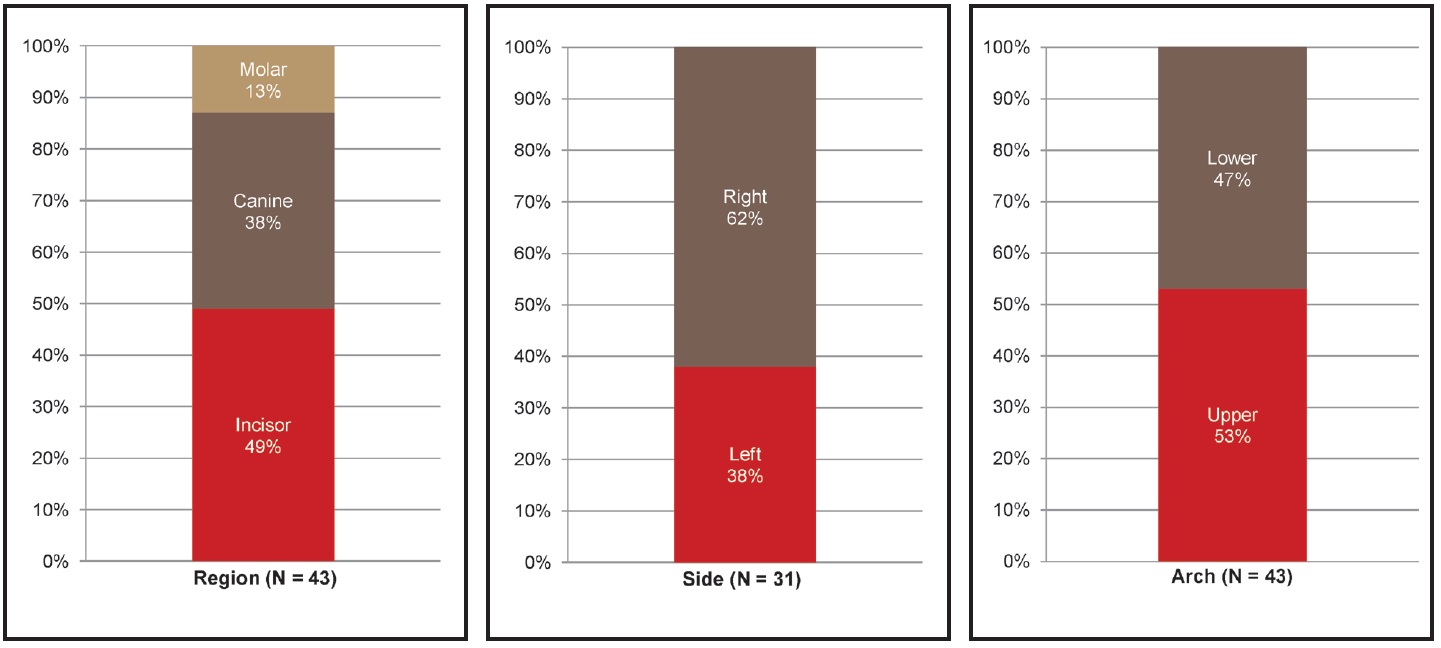
Fig. 6 Locations of intraoral pain after orthodontic wire activation or adjustment.
If pain relief was reported over an entire area in less than one minute, it look less than 30 seconds for each individual tooth to experience significant pain reduction.
The vast majority of patients (80%) listed comfort in chewing as the quality-of-life component most affected by orthodontic pain, followed by a reduction in productivity (37%) and in sleep time and quality (37%).
Sixty-five percent of the TENS patients stated they did not feel any sensation during the application; 35% said they felt a vibration with mild tingling, but classified it as only a slight sensation not associated with pain. Nearly 80% said they would use the TENS device for relief of orthodontic pain, and most preferred it as the main method of relief.
Orthodontic staff members overwhelmingly stated that the Dental Pain Eraser was well received and effective in providing pain relief following orthodontic wire activation or adjustment. Other suggested clinical applications for the device included traction of impacted teeth, separator placement, clear-aligner adjustments, elastic wear, and debonding of appliances. Orthodontic providers said they would probably use the Dental Pain Eraser on patients 15-50 times per day, concluding that this would be a new standard of pain relief in their practices.
Discussion
Many clinical studies have found a positive relationship between TENS therapy and the behavior of pediatric patients, probably owing to a reduction in anxiety. Various authors have shown that 53-78% of children prefer TENS over local anesthesia.9-11 Dhindsa and colleagues noted no difference in pain reduction between TENS and 2% lidocaine during extraction, cavity preparation, pulpotomy, or pulpectomy of deciduous teeth in 180 pediatric patients.15
Roth and Thrash assessed the effects of TENS treatment on periodontal pain associated with orthodontic separators placed mesial and distal to the upper first molars in 45 adult patients.8 Patients using TENS reported a significant reduction in pain at the 24- and 36-hour assessment periods but did not experience pain relief immediately or during the first 12 hours. Because the pain caused by separator placement starts within four hours of insertion,3 the crucial first day of orthodontic treatment could still be painful. A major contribution of the present study is the demonstration of immediate pain relief following orthodontic adjustments.
Burstone described both immediate and delayed pain responses after orthodontic force application.16 The initial response was attributed to compression, and the delayed response to hyperalgesia of the periodontal ligament (PDL). This hyperalgesia has been related to the effects of prostaglandins (PGEs), which make the PDL sensitive to released algogenic substances such as histamine, bradykinin, serotonin, and substance P.17,18
Nerve-fiber bundles associated with the pain response to compression are highly concentrated around the bony support of root structures.19 Traditional explanations of pain-reduction pathways, such as the gate control theory of pain blockage20 or central nervous system activation and release of endorphins,21 have more recently been contravened by studies showing the importance of neuropeptide release from nerve fibers in the compressed and stretched zones of the PDLs. For example, substance P and calcitonin gene-related peptide (CGRP), the neuropeptides released by sensory peripheral nerve endings, are known to modify the secretion of other pro-inflammatory cytokines such as interleukin 1 beta, interleukin 6, and tumor necrosis factor from monocytes.22,23
When a periodontal nerve fiber is activated by a compressive stimulus, an action potential is propagated along the axon to the spinal cord. These action potentials also invade collaterals and travel along them back to the peripheral terminals, where substance P and CGRP are released. Neuropeptides dilate capillaries and trigger histamine release from mast cells. The histamine then further stimulates Class C nerve fibers, creating a positive feedback loop.24
Biomedical engineering research on TENS therapy has tested specific amplitudes, frequencies, and delivery types from direct and alternating currents, with an emphasis on blocking nerve depolarization.25 These concepts are employed in the Dental Pain Eraser to block nerve action potential and thus reduce both the initial neuropeptide response and the feedback loop. The additional mechanism of action can facilitate immediate and delayed pain relief following application of orthodontic compressive forces. In the present study, 55% of the TENS patients experienced significant pain reduction in less than one minute of localized stimulation, and 84% in less than two minutes. It is important to note that the provider attempted to relieve all areas of sensitivity; in most cases, stimulation was applied to both arches and to multiple teeth. A clinically important, though unmeasured, observation was that few individual teeth required more than 10 seconds of stimulation. This indicates a direct pattern of nerve block in which the probe application ran the height of the tooth and around the root surface.
In terms of quality of life, our patients reported that the greatest negative effect of orthodontic treatment-related pain was on comfort in chewing, followed by a reduction in productivity and in sleep time and quality. This agrees with the results of other studies, which found that conditioned reflexes following archwire activation often lead to an avoidance of hard foods,26 and that pain from orthodontic treatment can have a marked influence on daily activities.27 Pain may be so bothersome that it causes wakeful nights and medication use.
Although an argument can be made that the lighter forces associated with advanced wires and self-ligating systems should cause less patient discomfort, Jones and Richmond found no statistical relationship among initial tooth positions, applied force levels, and pain.28 In the present study, where we used low-pressure, thermally activated nickel titanium wires and a self-ligating system to produce the lightest possible forces, 80% of the patients still experienced noticeable discomfort. Jones and Richmond observed that adults experienced more pain than children, which is also consistent with our findings.28
Feedback from the three independent private practices in the present study was highly supportive of chairside delivery of the Dental Pain Eraser to reduce orthodontic-related pain. Suggestions were made to improve the head shape of the Dental Pain Eraser to reach farther posteriorly, to improve the power and stimulation indicators, and to simplify the tip replacement method. These recommendations were incorporated into the commercially produced model (Fig. 1B).
Delayed onset of orthodontic pain can occur more frequently outside the clinical setting because of today’s advanced nickel titanium appliances and removable aligner systems. Orthodontists, staff members, and patients in this study all agreed that it would be beneficial for patients to be able to purchase portable Dental Pain Erasers for home use.
Conclusion
This study demonstrates that portable TENS delivery with the Dental Pain Eraser can be an effective method for reducing orthodontic pain. Every patient could benefit from an application of the Dental Pain Eraser immediately following any procedure that might cause discomfort. A Dental Pain Eraser could also be provided for home use during periods of hypersensitivity. Potential benefits include improved patient cooperation with oral hygiene because of the reduced pain of toothbrushing.4 Patients who would otherwise avoid orthodontics might accept treatment if they knew it would not be painful. Quality of life could be improved if pain did not interfere with eating, productivity, and sleep. The use of the Dental Pain Eraser might also result in less need for analgesics.
A subsequent study on the use of the Dental Pain Eraser to alleviate pain after separator placement in adolescents and adults was recently completed; findings included significantly reduced pain for as long as three days in patients who received TENS treatment, consistent with the results of the present study.29 Further investigations are currently being conducted to evaluate the effectiveness of the Dental Pain Eraser in blocking pain from such applications as cavity preparation, extractions, endodontic treatment, and soft-tissue procedures. Other studies are warranted to determine its utility in surgical treatment and as a take-home device to alleviate post-procedural sensitivity.
FOOTNOTES
- *Registered trademark of Electromedical Products International, Inc., Mineral Wells, TX; www.alpha-stim.com.
- **Synapse Dental LLC, Cranston, RI; www.synapsedental.com. The Dental Pain Eraser is an FDA-approved medical device.
REFERENCES
- 1. Kluemper, G.T.; Hiser, D.G.; Rayens, M.K.; and Jay, M.J.: Efficacy of a wax containing benzocaine in the relief of oral mucosal pain caused by orthodontic appliances, Am. J. Orthod. 122:359-365, 2002.
- 2. Keim, R.G.: The Editor’s Corner: Managing orthodontic pain, J. Clin. Orthod. 38:641-642, 2004.
- 3. Ngan, P.W.; Yiu, C.; Hägg, U.; Wei, S.H.Y.; and Bowley, J.: Masticatory muscle pain before, during, and after treatment with orthopedic protraction headgear: A pilot study, Angle Orthod. 67:433-437, 1997.
- 4. White, L.W.: Pain and cooperation in orthodontic treatment, J. Clin. Orthod. 18:572-575, 1984.
- 5. Marie, S.S.; Powers, M.; and Sheridan, J.J.: Vibratory stimulation as a method of reducing pain after orthodontic appliance adjustment, J. Clin. Orthod. 37:205-208, 2003.
- 6. Proffit, W.R. and Fields, H.W. Jr.: Contemporary Orthodontics, 3rd ed., Mosby, St. Louis, 2000.
- 7. Lim, H.M.; Lew, K.K.K.; and Tay, D.K.L.: A clinical investigation of the efficacy of low level laser therapy in reducing orthodontic postadjustment pain, Am. J. Orthod. 108:614-622, 1995.
- 8. Roth, P.M. and Thrash, W.J.: Effect of transcutaneous electrical nerve stimulation for controlling pain associated with orthodontic tooth movement, Am. J. Orthod. 90:132-138, 1986.
- 9. Baghdadi, Z.D.: Evaluation of electronic dental anesthesia in children, Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 88:418-423, 1999.
- 10. TeDuits, E.; Goepferd, S.; Donly, K.; Pinkham, J.; and Jakobsen, J.: The effectiveness of electronic dental anesthesia in children, Pediat. Dent. 15:191-196, 1993.
- 11. Oztas, N.; Olmez, A.; and Yel, B.: Clinical evaluation of transcutaneous electronic nerve stimulation for pain control during tooth preparation, Quintess. Int. 28:603-608, 1997.
- 12. Yap, A.U. and Ho, H.C.: Electronic and local anesthesia: A clinical comparison for operative procedures, Quintess. Int. 27:549-553, 1996.
- 13. Rodriguez, C.S.: Pain measurement in the elderly: A review, Pain Manag. Nurs. 2:38-46, 2001.
- 14. Johnson, C.: Measuring pain: Visual analog scale versus numeric pain scale: What is the difference? J. Chirop. Med. 4:43-44, 2005.
- 15. Dhindsa, A.; Pandit, I.K.; Srivastava, N.; and Gugnani, N.: Comparative evaluation of the effectiveness of electronic dental anesthesia with 2% lignocaine in various minor pediatric dental procedures: A clinical study, Contemp. Clin. Dent. 2:27-30, 2011.
- 16. Burstone, C.J.: The biomechanics of tooth movement, in Vistas in Orthodontics, ed. B.S. Kraus and R.A. Riedel, Lea and Febiger, Philadelphia, 1962, pp. 197-213.
- 17. Ferreira, S.H.; Nakamura, M.; and de Abreu Castro, M.: The hyperalgesic effects of prostacyclin and prostaglandin E2, Prostaglandins 16:31-37, 1978.
- 18. Polat, O.; Kararam, A.I.; and Durmus, E.: Effects of preoperative ibuprofen and naproxen sodium on orthodontic pain, Angle Orthod. 75:791-796, 2005.
- 19. Huang, Y.; Corpas, L.S.; Martens, W.; Jacobs, R.; and Lambrichts, I.: Histomorphological study of myelinated nerve fibres in the periodontal ligament of human canine, Acta Odontol. Scand. 69:279-286, 2011.
- 20. Melzack, R. and Wall, P.D.: Pain mechanics: A new theory, Science 150:971-979, 1965.
- 21. Bennett, C.R.: Monheim’s Local Anesthesia and Pain Control In Dental Practice, 7th ed., CBS Publishers and Distributors, New Delhi, 1990.
- 22. Nicolay, O.F.; Davidovitch, Z.; Shanfeld, J.L.; and Alley, K.: Substance P immunoreactivity in periodontal tissues during orthodontic tooth movement, Bone Miner. 11:19-29, 1990.
- 23. Alhashimi, N.; Frithiof, L.; Brudvik, P.; and Bakhiet, M.: Orthodontic movement and de novo synthesis of proinflammatory cytokines, Am. J. Orthod. 119:307-312, 2001.
- 24. Vandevska-Radunovic, V.: Neural modulation of inflammatory reactions in dental tissues incident to orthodontic tooth movement: A review of the literature, Eur. J. Orthod. 21:231-247, 1999.
- 25. Weinberg, S.H.: High-frequency stimulation of excitable cells and networks, PLoS One 8:e81402, 2013.
- 26. Gianelly, A.A. and Goldman, H.M.: Tooth movement, in Biological Basis of Orthodontics, Lea and Febiger, Philadelphia, 1971, pp. 116-204.
- 27. Brown, D.F. and Moerenhout, R.G.: The pain experience and psychological adjustments to orthodontic treatment of preadolescents, adolescents, and adults, Am. J. Orthod. 100:349-356, 1991.
- 28. Jones, M.L. and Richmond, S.: Initial tooth movement: Force application and pain—A relationship? Am. J. Orthod. 88:111-116, 1985.
- 29. Noh, G.; Haralambidis, C.; Lee, M.; and Harewood, J.: The effect of the Dental Pain Eraser intraoral portable TENS device on periodontal pain relief due to orthodontic separator placement: A randomized controlled trial, unpublished data, St. Barnabas Hospital, Bronx, NY, 2019.




COMMENTS
.